Abstract
Purpose
The goal of the study was to evaluate the efficacy of additional axillary nerve block (ANB) with suprascapular nerve block (SSNB) and patient-controlled anaesthesia (PCA) with no device assistance after arthroscopic rotator cuff repair. The hypothesis is that patients with intravenous (IV) PCA and the blockade of the two main nerves (SSNB + ANB) experienced lesser pain than patients with IV PCA or IV PCA + SSNB.
Methods
The 114 patients undergoing arthroscopic rotator cuff repair were allocated randomly to three groups as follows: group I, intravenous PCA pumps (only PCA); group II, IV PCA + SSNB using a blind technique (PCA + SSNB); and group III, IV PCA + SSNB + ANB using a blind technique (PCA + SSNB + ANB). Pain visual analogue scale (VAS) scores were evaluated at 1, 6, 12, 24, 36, and 48 post-operative hours. Furthermore, the degree of pain was compared according to cuff tear size.
Results
The pain VAS score of group III was lower than that of the other two groups and was significantly lower at post-operative hours 1, 6, and 12. In addition, the larger cuff tear tended to be indicative of greater pain. However, all groups experienced rebound pain.
Conclusion
PCA + SSNB + ANB using a blind technique is a better pain control method than PCA + SSNB and only PCA during the initial 12 post-operative hours. PCA + SSNB + ANB is a cost-effective, time-saving, and easily performed method for post-operative pain control as an axis of multimodal pain control strategy.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopic shoulder surgery is a common procedure; although it is associated with reduced hospitalization time, the procedure could be associated with moderate and severe post-operative pain [15]. Severe pain within 48 post-operative hours is often observed after shoulder surgery [36]. Pain control remains a challenging aspect of shoulder arthroscopy. Various methods have been applied for post-operative pain control, including oral analgesics, regional nerve block [e.g. interscalene brachial plexus block, suprascapular nerve block (SSNB), C5 block], intravenous patient-controlled analgesia (IV PCA), and continuous intrabursal infusion pumps [17]. Underlying issues related to shoulder arthroscopy include determination of multimodal pain control strategies for increasing the effectiveness of pain control, as well as decreasing complications such as dizziness and nausea/vomiting. Interscalene brachial plexus block for blockade of almost all of the shoulder’s sensory function has been introduced as the most effective procedure [33]. However, interscalene brachial plexus blocks require increased performance time and costs related to the procedure, and the rate of success or complications can depend on the anaesthesiologist’s skill [3, 21, 22].
An alternative to interscalene brachial plexus block is PCA with SSNB, which provides excellent pain relief in shoulder disorders because the suprascapular nerve is the main sensory nerve to elicit pain in the shoulder joint [20]. However, the suprascapular nerve is not the only nerve affected [2]. The sensitive innervation of the shoulder is composed of the terminal branches of the axillary nerve and small branches of the cervical plexus as well as the suprascapular nerve [6]. The earlier studies were based on device-assistant technique using an ultrasound and/or a nerve stimulator [13, 20, 32, 34, 35]. These methods are too costly and time-consuming like interscalene brachial plexus block. Recently, blind techniques without device assistance for suprascapular nerve and axillary nerve block (ANB) have been introduced on the basis of this anatomical study [6, 28]. To our knowledge, no prospective studies have compared IV PCA + SSNB + ANB, IV PCA + SSNB, and only IV PCA through a blind technique as multimodal strategies of shoulder pain managements.
The purpose of this study was to evaluate the role of IV PCA + SSNB + ANB using blind techniques in decreasing post-operative pain with arthroscopic rotator cuff repair. The hypothesis is that patients with IV PCA and blockade of the two main nerves (SSNB + ANB) had lesser pain than patients with IV PCA or IV PCA + SSNB.
Materials and methods
This study is a prospective randomized cohort study from March 2012 to August 2012. After institutional review board approval, 114 consecutive patients with American Society of Anesthesiologists (ASA) physical status classifications I–II were enrolled and scheduled for elective arthroscopic repair of full-thickness rotator cuff tear under general anaesthesia, and all patients gave written informed consent for the study. The inclusion criteria included the following procedure for rotator cuff repair: (1) subacromial decompression for subacromial impingement, (2) arthroscopic capsulectomy for severe stiffness, (3) arthroscopic distal clavicle resection for AC joint arthrosis, or (4) biceps soft tissue tenodesis or tenotomy for long head biceps-related lesion. The exclusion criteria included the following: (1) preoperative opioid medication administered for >1 month before surgery, (2) pre-existing neuropathy, (3) known allergy to amide local anaesthetics, (4) subacromial impingement syndrome without rotator cuff tear, (5) osteoarthritis more than grade 3 Outerbridge classification, (6) biceps bony tenodesis, and (7) partial-thickness rotator cuff tear.
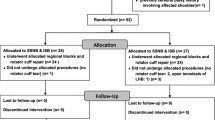
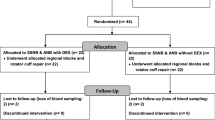
The 114 patients were allocated randomly to three groups as follows:
-
Group I with IV PCA pumps (only PCA)
-
Group II with IV PCA + blind SSNB (PCA + SSNB)
-
Group III with IV PCA + blind SSNB + blind ANB (PCA + SSNB + ANB)
Eight patients (5 in group I, 2 in group II, 1 in group III) of a total 114 patients were excluded because of nausea/vomiting. IV PCA was withheld and antiemetics were administered in these patients. Finally, group I had 33 patients, group II had 36 patients, and group III had 37 patients (Table 1). The mean age (±SD) of the 106 patients undergoing arthroscopic shoulder surgery was 60 ± 18 years. The mean body mass index (BMI) was 22.5 ± 4.5.
The previous night, all patients were pre-emptively administered pregabalin 75 mg, aceclofenac 100 mg, tramadol 37.5 mg, and acetaminophen 325 mg. The patients were positioned in the beach chair position after undergoing general anaesthesia. For all groups, the PCA contained a mixture of saline 80 mL, fentanyl 0.5 mg, ketorolac 180 mg, and ondansetron 12 mg in a time-release injection that persists up to 48 h. After marking the outlines of the clavicle, the scapular spine with the acromion, and the coracoid process, SSNB or SSNB + ANB was administered by a blind method using anatomical landmarks as described in the next paragraph. All surgical procedures were completed in a standardized manner in all patients and performed by one senior surgeon. Arthroscopic subacromial decompression with acromioplasty was performed in all patients. A suture bridge technique was used for the cuff tear. In addition, same-dose medication (zolpidem, tramadol, and pregabalin) was regularly prescribed during hospitalization. Passive pulley exercise with shrugging was started immediately for rehabilitation during the post-operative period.
Method of blind nerve block
The block method based on anatomical studies with no device assistance was called “blind block technique” in this article. The chosen technique was developed by Checcucci [6]. Instead of a mixture of 15 mL of lidocaine 2 % (5 mL) and levobupivacaine 0.5 % (10 mL) in the previous study, 10 mL of ropivacaine 0.75 % was used because lidocaine may lead to chondrotoxicity and levobupivacaine has been introduced into clinical practice recently, and as a consequence, experience of its use is more limited than with ropivacaine [4, 5, 11, 39]. Both nerve blocks were conducted by a senior surgeon and took 1 min after skin preparation and draping.
Suprascapular nerve block
After drawing a line connecting the medial area of the acromion and the medial end point of the spine of the scapula, a 25-gauge needle was inserted the parallel line to the vertebral column in 2 cm medial and 2 cm cephalad to the mid-point of the drawing line. The needle was advanced until it came into contact with the bone (scapular spine). Then the needle was moved back slightly, and 10 mL of ropivacaine 0.75 % was slowly injected, with repeated withdrawal to prevent the risk of unintended intravascular injection (Fig. 1).
Axillary nerve block
The point of ANB administration was approximately 2 cm cranial to the convergence of this line with the perpendicular line that started from the axillary fold after drawing the line between the lateral-posterior angle of the acromion and the olecranon tip of the elbow. After the 25-gauge needle was advanced with the perpendicular line from starting point until it came into contact with the humeral posterior cortex, 10 mL of 0.75 % ropivacaine was slowly injected in the same manner as for SSNB (Fig. 2).
Outcome assessment
One resident checked the post-operative pain VAS score. The pain VAS score of all patients was examined at 1, 6, 12, 24, 36, and 48 h post-operatively through the face to face survey. Pain was measured on a 10-cm VAS, with 0 indicating no pain and 10 indicating the worst pain.
Randomized design
Each patient was distributed consecutively to groups I, II, and III according to tear size of rotator cuff because rotator cuff tear size is considered a main factor causing pain difference. Concretely, rotator cuff tear size of each patient was evaluated on MRI and belong to small (<1 cm), medium (1–3 cm), large (3–5 cm) or massive (>5 cm) by DeOrio and Cofield classification [10]. Each patient was belong to small to medium size (S group) and large to massive (L group). Each S group patient belongs to groups I, II, and III in serial order and each L group patient belongs in the same way.
The operation procedure and evaluation method were approved by the institutional review board of the Konkuk University Medical Center (IRB ID No. KUH1060074).
Statistical analysis
The sample size was determined based on clinical equivalence, as well as significance, which was considered a 20 % difference in the VAS pain score. A minimum of 32 patients were anticipated to provide a 5 % significance level and 80 % power. To allow for withdrawals with a total attrition rate of 15 %, a minimum of 114 participants were recruited. Statistical analyses were carried out using SPSS (version 18.0; SPSS Inc., Chicago, IL, USA). The independent t test was used to assess the significance of the VAS score difference among the three pain control methods. A p value of <0.05 was considered statistically significant.
Results
No significant differences were noted among the three injection groups regarding age, tear size, operative time, the number of used anchor, and other procedures. Specifically, the injection groups had no neurological complications.
The post-operative pain VAS scores of all groups are shown in Fig. 3. The VAS scores of group III were lower than those in the other two groups, and the VAS scores of group II were lower than those of group I for 48 h. The pain severity of all groups tended to lower over a period, but the pain VAS score rebounded at post-operative hours 12 and 36. Statistically, the VAS scores of group III were significantly lower than those in group I at post-operative hours 1, 6, 12, and 36 (p < 0.01) and significantly lower than those in group II at 48 h (p < 0.01). The VAS scores of group II were significantly lower than those of group I at post-operative hours 1, 6, 12, and 36 (p < 0.01).
There was no significant difference in demography according to cuff tear size (S group and L group), except for operation time. The operation time for the repair of small-to-medium-sized cuff tears was 49.8 ± 7.9 (min) and that for large-to-massive cuff tears was 84.6 ± 20.1 (min) (p < 0.01). The large-to-massive cuff tear group had significantly higher pain VAS scores than the small-to-medium-sized tear group at 1, 12, 24, 36, and 48 h (p < 0.01) (Table 2).
Discussion
The most important finding of the present study was that the mean VAS score of the PCA + SSNB + ANB group within 12 post-operative hours was significantly lower than that of the only PCA or PCA + SSNB group.
A major factor for successful shoulder surgery is the post-operative quality of pain management. Acute post-operative pain is responsible for 60 % of unplanned hospitalizations and rehabilitation in orthopaedic surgery, especially after shoulder surgery [8, 16]. Various methods for post-operative pain control exist, including oral analgesics, intravenous PCA, regional nerve block (e.g. interscalene brachial plexus block, SSNB, selective C5 nerve root block), and continuous intrabursal infusion pumps [27]. Intravenous PCA has been widely used, but could be associated with several side effects such as nausea, vomiting, and urinary retention. Interscalene brachial plexus block is the standard of care for shoulder arthroscopy at many institutions [1, 7, 26, 28, 35]. Faryniarz et al. [14] reported that successful surgical anaesthesia was achieved in 98 % of the 133 patients and an overall complication rate was 2.1 % when an experienced anaesthesiologist is involved. Shin et al. [34] reported that continuous and bolus interscalene block groups recorded the lower pain score than IV PCA group in total 99 patients. However, other study reported that this method has a failure rate of 5–13 % and a rebound phenomenon of increased pain 12 h after initial block [25]. Some authors hesitate to use interscalene block because it is associated with major complications such as cardiac arrest, central nervous system toxicity, pneumothorax, respiratory distress, Horner syndrome, phrenic nerve palsy, and remnant motor or sensory deficits [23, 31, 37]. Misamore et al. and Weber et al. reported a 13 % rate of interscalene block failure, a 16 % rate of immediate block side effects, and a 4.4 % rate of persistent neurological complications [23, 38]. Therefore, surgeons found this procedure challenging without the assistance of an anaesthesiologist.
Recently, SSNB or SSNB with ANB, which has lower complication rates and can be performed easily, has been reported to be effective, and several block techniques have been introduced [19, 20, 29]. These methods include a blind, ultrasonography-guided, arthroscopic-guided, and electromyography-guided technique. A blind SSNB technique was first introduced by Moore [24]. Ritchie et al. [30] showed the methods’ effectiveness as comparing the blind injection group and placebo groups (25 patients in each group). Jerosch et al. [19] studied the blind SSNB’s effectiveness as a method of pre-emptive pain control in comparing of cohort group with nerve block and without nerve block (130 patients in each group). In addition, Lee et al. [21] reported that PCA with SSNB + ANB is a better anaesthetic choice than PCA with interscalene block without complication during the initial 24 h of the post-operative period in 61 patients. However, some authors insisted that the blind technique is less effective because of anatomical variations of the suprascapular nerve and the surgeon learning curve; therefore, they asserted that some image-guided methods should be used [25]. However, other authors advocated that a blind block technique based on the anatomical studies is very effective [6, 19, 25, 28]. Theoretically, SSNB alone has been less effective because the suprascapular nerve is not the only nerve in the shoulder sensory system [18]. The sensitive innervation of the shoulder is composed of the terminal branches of the axillary nerve and small branches of the cervical plexus (e.g. pectoral nerve) as well as the suprascapular nerve [6]. The best nerve block should include easy surgical access, less time, low cost, and effective pain control without time and cost wasting. Therefore, the blind technique, which does not require additional time, cost, and devices, was selected in this study. The pain VAS score was lower in the PCA + SSNB + ANB group than in the other two groups. The PCA + SSNB + ANB group had better post-operative pain control during the early phase of recovery, but no significant difference was noted after 24 post-operative hours. These results suggest that pain control was easier to achieve in the recovery room and that it was more difficult to obtain >12 h after the procedure. The median duration of action of 0.5 % ropivacaine 5 mL in the upper arm was reportedly 11.4–14.4 h [9]. The median onset time of sensory block produced by 0.5 % ropivacaine via axillary block was reportedly 10–45 min [12].
In our study, all groups showed rebound pain at 12 and 36 h after surgery, unlike previous studies [25, 28]. Because all operations were performed between 9 a.m. and 3 p.m., 12 and 36 h after surgery was equivalent to night-time. This rebound pain may have connection with night pain and attenuated block effect. Therefore, additional multimodal pain control factors such as sleep agent, pregabalin, opioid medication, and repeated nerve block may be required.
In addition, post-operative pain following arthroscopic rotator cuff repair may vary depending on the size of the cuff tear. Larger cuff tears indicate more pain. In shoulder arthroscopic surgery, the causative factor of post-operative pain was suspected swelling of the surgical site because of a longer operation time. Therefore, a larger tear would require more aggressive pain control. In our study, 1 and 6 h after the shoulder arthroscopic surgery, the mean pain VAS scores of 7.16 and 5.10 were relatively higher than those of 4.23 and 4.56 in other two studies [21, 25]. It is believed that the pain threshold was lowered, which lead patients to provide high scores for the pain because information about severe post-operative pain was obtained during provision of informed consent.
IV PCA + SSNB + ANB could not completely eliminate post-operative pain. However, it is a safe and easy procedure without severe complications and is associated with significantly reduced pain severity over several hours. Suprascapular nerve and axilla nerve are terminal branch of brachial plexus. So the potential complication may have lower than interscalene nerve block because of relative peripheral location. The complications are peripheral arteries (suprascapular artery and circumflex artery) injection and pneumothorax. The blind SSNB and ANB through the bony landmark could have lower complication rate. The bony block of scapular spine could diminish the possibility of pneumothorax and regurge during insertion needle could prevent intravascular injection. The blind injection can be easily performed by surgeons with short procedure time. The other advantages are that it requires no special device for block without further cost. Therefore, the blind injection could be useful in countries where the device-assisted blocks were not used due to the economic burden.
There are some limitations in this study. First, pain VAS score is a subjective tool. Second, all other possible methods of post-operative pain control were not included simultaneously. Third, potential subject bias can be existed since controls received no placebo injection. Fourth, the accuracy of blind injection is untested in each case. Further study is needed to evaluate the effect of issues with a larger population.
The blind SSNB and ANB based on anatomical studies with IV PCA were safe and time/cost saving in shoulder arthroscopy surgery.
Conclusion
The blind SSNB and ANB with IV PCA is a cost-effective, time-saving, and easily performed method for post-operative pain control as an axis of multimodal pain control strategy. Orthopaedic surgeons can safely attempt repeated nerve block for rebound pain in the general ward or outpatient clinic. Additionally, supplementary pain control may be required for larger cuff tears.
References
Al-Nasser B (2012) Review of interscalene block for postoperative analgesia after shoulder surgery in obese patients. Acta Anaesthesiol Taiwan 50:29–34
Barber FA (2005) Suprascapular nerve block for shoulder arthroscopy. Arthroscopy 21(8):1015
Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone J, Flatow EL (2005) Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am 87(5):974–979
Borghi B, Facchini F, Agnoletti V, Adduci A, Lambertini A, Marini E, Gallerani P, Sassoli V, Luppi M, Casati A (2006) Pain relief and motor function during continuous interscalene analgesia after open shoulder surgery: a prospective, randomized, double-blind comparison between levobupivacaine 0.25 %, and ropivacaine 0.25 % or 0.4 %. Eur J Anaesthesiol 23(12):1005–1009
Casati A, Borghi B, Fanelli G, Montone N, Rotini R, Fraschini G, Vinciguerra F, Torri G, Chelly J (2003) Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: a randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg 96(1):253–259
Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G (2008) A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy 24(6):689–696
Cho CH, Song KS, Min BW, Jung GH, Lee YK, Shin HK (2015) Efficacy of interscalene block combined with multimodal pain control for postoperative analgesia after rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 23(2):542–547
Chung F, Ritchie E, Su J (1997) Postoperative pain in ambulatory surgery. Anesth Analg 85(4):808–816
Cummings KC 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, Sessler DI (2011) Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Brit J Anaesth 107(3):446–453
DeOrio JK, Cofield RH (1984) Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 66(4):563–567
Dragoo JL, Braun HJ, Kim HJ, Phan HD, Golish SR (2012) The in vitro chondrotoxicity of single-dose local anesthetics. Am J Sport Med 40(4):794–799
Dyhre H, Lang M, Wallin R, Renck H (1997) The duration of action of bupivacaine, levobupivacaine, ropivacaine and pethidine in peripheral nerve block in the rat. Acta Anaesth Scand 41(10):1346–1352
Elsharkawy HA, Abd-Elsayed AA, Cummings KC 3rd, Soliman LM (2014) Analgesic efficacy and technique of ultrasound-guided suprascapular nerve catheters after shoulder arthroscopy. Ochsner J 14(2):259–263
Faryniarz D, Morelli C, Coleman S, Holmes T, Allen A, Altchek D, Cordasco F, Warren RF, Urban MK, Gordon MA (2006) Interscalene block anesthesia at an ambulatory surgery center performing predominantly regional anesthesia: a prospective study of one hundred thirty-three patients undergoing shoulder surgery. J Shoulder Elbow Surg 15(6):686–690
Fontana C, Di Donato A, Di Giacomo G, Costantini A, De Vita A, Lancia F, Caricati A (2009) Postoperative analgesia for arthroscopic shoulder surgery: a prospective randomized controlled study of intraarticular, subacromial injection, interscalenic brachial plexus block and intraarticular plus subacromial injection efficacy. Eur J Anaesthesiol 26(8):689–693
Fortier J, Chung F, Su J (1998) Unanticipated admission after ambulatory surgery—a prospective study. Can J Anaesth 45(7):612–619
Fredrickson MJ, Krishnan S, Chen CY (2010) Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia 65(6):608–624
Han SS, Lee YH, Oh JH, Aminzai S, Kim SH (2013) Randomized, controlled trial of multimodal shoulder injection or intravenous patient-controlled analgesia after arthroscopic rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 21(12):2877–2883
Jerosch J, Saad M, Greig M, Filler T (2008) Suprascapular nerve block as a method of preemptive pain control in shoulder surgery. Knee Surg Sports Traumatol Arthrosc 16(6):602–607
Lee JJ, Yoo YS, Hwang JT, Kim DY, Jeon SJ, Hwang SM, Jang JS (2013) Efficacy of direct arthroscopy-guided suprascapular nerve block after arthroscopic rotator cuff repair: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23:562–566
Lee SM, Park SE, Nam YS, Han SH, Lee KJ, Kwon MJ, Ji JH, Choi SK, Park JS (2012) Analgesic effectiveness of nerve block in shoulder arthroscopy: comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc 20:2573–2578
Lenters TR, Davies J, Matsen FA 3rd (2007) The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg 16:379–387
Misamore G, Webb B, McMurray S, Sallay P (2011) A prospective analysis of interscalene brachial plexus blocks performed under general anesthesia. J Shoulder Elbow Surg 20(2):308–314
Moore D (1979) Block of the suprascapular nerve. In: Thomas CC (ed) Regional nerve block 4th edn. Charles C Thomas, Springfield, Illinois, pp 300–303
Nam YS, Jeong JJ, Han SH, Park SE, Lee SM, Kwon MJ, Ji JH, Kim KS (2011) An anatomic and clinical study of the suprascapular and axillary nerve blocks for shoulder arthroscopy. J Shoulder Elbow Surg 20(7):1061–1068
Oh JH, Rhee KY, Kim SH, Lee PB, Lee JW, Lee SJ (2009) Comparison of analgesic efficacy between single interscalene block combined with a continuous intra-bursal infusion of ropivacaine and continuous interscalene block after arthroscopic rotator cuff repair. Clin Orthop Surg 1:48–53
Park JY, Lee GW, Kim Y, Yoo MJ (2002) The efficacy of continuous intrabursal infusion with morphine and bupivacaine for postoperative analgesia after subacromial arthroscopy. Reg Anesth Pain Med 27(2):145–149
Price DJ (2007) The shoulder block: a new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesth Intensive Care 35(4):575–581
Price DJ (2008) Axillary (circumflex) nerve block used in association with suprascapular nerve block for the control of pain following total shoulder joint replacement. Reg Anesth Pain Med 33(3):280–281
Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD (1997) Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg 84(6):1306–1312
Robaux S, Bouaziz H, Boisseau N, Raucoules-Aime M, Laxenaire MC, Service SOSRHL (2001) Persistent phrenic nerve paralysis following interscalene brachial plexus block. Anesthesiology 95(6):1519–1521
Rothe C, Steen-Hansen C, Lund J, Jenstrup MT, Lange KH (2014) Ultrasound-guided block of the suprascapular nerve—a volunteer study of a new proximal approach. Acta Anaesth Scand 58(10):1228–1232
Savoie FH, Field LD, Jenkins RN, Mallon WJ, Phelps RA 2nd (2000) The pain control infusion pump for postoperative pain control in shoulder surgery. Arthroscopy 16(4):339–342
Shin SW, Byeon GJ, Yoon JU, Ok YM, Baek SH, Kim KH, Lee SJ (2014) Effective analgesia with ultrasound-guided interscalene brachial plexus block for postoperative pain control after arthroscopic rotator cuff repair. J Anesth 28(1):64–69
Singh A, Kelly C, O’Brien T, Wilson J, Warner JJ (2012) Ultrasound-guided interscalene block anesthesia for shoulder arthroscopy: a prospective study of 1319 patients. J Bone Joint Surg Am 94(22):2040–2046
Tuominen M, Pitkanen M, Rosenberg PH (1987) Postoperative pain relief and bupivacaine plasma levels during continuous interscalene brachial plexus block. Acta Anaesth Scand 31(4):276–278
Turker G, Demirag B, Ozturk C, Uckunkaya N (2004) Cardiac arrest after interscalene brachial plexus block in the sitting position for shoulder arthroscopy: a case report. Acta Orthop Belg 70(1):84–86
Weber SC, Jain R (2002) Scalene regional anesthesia for shoulder surgery in a community setting: an assessment of risk. J Bone Joint Surg Am 84-A(5):775–779
Whiteside JB, Wildsmith JA (2001) Developments in local anaesthetic drugs. Brit J Anaesth 87(1):27–35
Acknowledgments
The authors appreciate Yoo-Kyung Hwang Ph.D. for providing assistance in performing statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Park, JY., Bang, JY. & Oh, KS. Blind suprascapular and axillary nerve block for post-operative pain in arthroscopic rotator cuff surgery. Knee Surg Sports Traumatol Arthrosc 24, 3877–3883 (2016). https://doi.org/10.1007/s00167-015-3902-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3902-3