Abstract
Objective
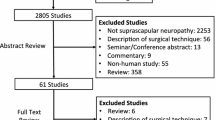
The objective of this study was to describe the suprascapular nerve block using CT guidance and to evaluate the short- and medium-term efficacy in a range of shoulder pathologies.
Design and patients
CT-guided infiltration around the suprascapular nerve was performed with bupivacaine and Celestone Chronodose on 40 consecutive patients presenting with chronic shoulder pathologies unresponsive to conventional treatment. Patients were interviewed using the Shoulder Pain and Disability Index (SPADI) before the procedure, 30 min after the procedure and at 3 days, 3 weeks and 6 weeks afterwards.
Results
Within 30 min of the block overall pain scores decreased from a mean (±SEM) pain score of 7.0 (±0.4) to 3.5 (±0.5) (n=39, P<0.001). At 3 days after the procedure, the mean overall improvement of the pain and disability scores were 20.4% (±4.9, P<0.001) and 16.8% (±4.8, P=0.004) respectively. Sustained pain relief and reduced disability were achieved in 10 of 35 (29%) patients at 3 weeks and longer. Patients suffering from soft tissue pathologies were the most likely patients to benefit from the injection. No serious side effects were noted.
Conclusions
In some patients with chronic soft tissue pathologies who do not respond to conventional treatment, a CT-guided suprascapular nerve block can provide safe short- and medium-term relief from pain and disability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
About 5% of all general practice consultations are related to painful shoulder pathologies [1, 2]. Fifty per cent of these resolve within 6 months following the initial consultation, but the remainder may persist for several years [3], resulting in significant disability and reduction in the quality of life of the patients affected. A number of management options, including steroid injections, are available to treat the pain and disability of shoulder pathologies, but to date there is little evidence to support their efficacy [4, 6].
Historically, all studies reporting nerve block injections into the shoulder were carried out in a blind fashion with the clinician using anatomical landmarks or the area of maximal pain to guide the injection. It has been suggested that inaccurate placement of the needle tip may be the cause of the variable effectiveness accorded to this technique [7, 10].
Thus, the objective of this study was to evaluate the efficacy and feasibility of image-guided suprascapular nerve block injections using CT for shoulder pain of various aetiologies. To the best of our knowledge, CT guidance for this procedure has not been previously reported.
Materials and methods
Subjects
Consecutive patients referred to our institution for suprascapular nerve block injections were considered for participation. The main inclusion criteria were a painful shoulder joint, the category of lesion being based on a previous clinical diagnosis, with a visual analogue pain score (VAS; score from 0 to 10, where 0 is no pain and 10 is severe pain) of at least 4/10 for pain at presentation, age 18 years or older, and previous unsuccessful conventional treatment such as analgesics, nonsteroidal anti-inflammatory drugs, physiotherapy, hydrodilatation, chiropractic treatment, steroid injections and surgery. Patients were excluded if they had previous allergic reactions to corticosteroids, contrast solution or local anaesthetic, if fractures or congenital disorders were present, if they were pregnant or if they were unable to comply with follow-up. The study protocol was approved by the Cabrini Hospital Human Research Ethics Committee and all patients gave informed consent.
The patients were recruited by an independent investigator at their initial presentation in the clinic. A detailed history of the shoulder discomfort was taken and baseline values of outcome measures were assessed prior to the injection. The baseline assessment included demographic details, as well as duration of current shoulder pain and precipitating cause.
No radiological categorization was undertaken.
CT-guided injection
The patients were placed prone on the CT table (GE High Speed Lx, Milwaukee, Wis., USA) and the affected arm positioned by their side. A scout scan was performed followed by contiguous 5 mm slices of the joint. A surface marker was placed over the injection site corresponding to the suprascapular notch (Fig. 1). The site was swabbed using chlorhexidine and a 25G spinal needle (Terumo, Leuven, Belgium) inserted through the deltoid muscle close to the neurovascular bundle (Fig. 2). A further image was taken to confirm accurate placement of the needle just above the neurovascular bundle (Fig. 3). Patients who were capable of rotating their arm above the head were positioned on the table with their arm raised above their head. This rotation brings the neurovascular bundle into a position that facilitates infiltration of the injectate around the suprascapular nerve (Fig. 3). The needle was then inserted into the superior and posterior aspect of the suprascapular notch. After aspiration to exclude intravascular injection, 3 ml of bupivacaine together with 1 ml of Celestone Chronodose were slowly injected into the soft tissues around the neurovascular bundle and the needle withdrawn. The patients were asked to sit up and were monitored for approximately 30 min. The investigator then evaluated the immediate post-procedural values of the outcome measures.
Outcome assessment
Only one injection was given. The position of the arm during the injection was not included in the outcome assessment. The intervention outcome was assessed at 3 days, 3 weeks and 6 weeks after treatment. All assessments were by telephone with the exception of the baseline and the immediate post-procedural follow-up, which were conducted in the clinic. Patients remained in the study analysis unless further professional treatment was initiated or a repeat steroid injection given. Further treatment was identified as surgical intervention, physiotherapy, hydrodilatation, or alternative therapies such as acupuncture or manipulation.
Primary outcome measures
Patients were asked to score their pain levels, at rest with their arms by their side, using a 10-point visual analogue scale (VAS; 0=no pain, 10=unbearable pain) prior to and 30 min after the injection, as well as at each follow-up assessment. The pain associated with the procedure itself was assessed on a 5-point VAS scale (1=no pain, 2=mild pain, 3=moderate pain, 4=severe pain, 5=unbearable pain). Prior to the injection (baseline assessment) and during follow-ups, patients also completed the Shoulder Pain and Disability Index (SPADI) questionnaire [8, 9]. SPADI scores for pain index range from 0 to 50 (0=no pain, 50=unbearable pain) and for disability index from 0 to 80 (0=no disability, 80=maximal disability). The usefulness of the SPADI for telephone follow-up and as an accurate measure for clinical changes in shoulder disorders has previously been demonstrated [8]. At the 3 week follow-up patients were also asked whether the procedure had had a significant effect on their pain levels. A 30% or greater reduction in pain and/or disability SPADI scores was considered significant.
Statistical analysis
Normality of the data was evaluated using the Kolmogorov-Smirnov test. All outcome measures showed a non-Gaussian distribution. Differences between pre- and post-procedural pain VAS and SPADI scores were analysed using the Wilcoxon Signed-Rank test. Changes in outcome assessments at each follow-up (3 days, 3 weeks) compared with baseline values were calculated using the Wilcoxon Signed-Rank test. Differences in improvement over time for pain or disability were analysed using analysis of variance for repeated measures (Friedman test). All statistical analyses were carried out using SPSS, version 11.0 (Chicago, Ill., USA) and P values of <0.05 were considered statistically significant.
Results
Patient characteristics
A total of 40 consecutive suitable patients referred by their specialists were enrolled in the study. There were 16 men and 24 women with a mean age (±SD) of 44 years (10.5) and a mean duration of shoulder pain of 30.5 (range 1–180) months. Causes of shoulder pain in the study population were varied and are summarized in Table 1. The five trauma patients had previous soft tissue incidents involving the shoulder, such as falls and motor car accidents. In nine patients, the cause of pain was unknown.
Patient flow and follow-up
A total of five patients were lost to follow-up at 6 weeks. A further 12 had undergone supplementary treatment between 3 and 6 weeks after the injection (Table 2). Of those, repeat steroid injections were given to three patients, physiotherapy to five, hydrodilatation to one and two underwent surgical intervention. One patient presenting with shoulder pain was subsequently diagnosed as having referred pain from the cervical spine 3 weeks after the injection. This diagnosis was made using further clinical and imaging assessments.
Outcome
The overall (mean±SEM) pain rating of the procedure was 2.64 (±0.22). Eleven of 39 (28%) patients stated that the procedure caused no pain, 10 of 39 (26%) patients reported mild pain, and six of 39 (15%) each reported moderate, severe or unbearable pain. One patient did not provide an answer.
Within 30 min of the injection, overall shoulder pain scores decreased from a mean (±SEM) VAS of 7.0 (±0.4) to a mean of 3.5 (±0.5) (P<0.001, Wilcoxon Signed- Rank). Twenty-four of the 39 patients (62%) reported a mean pain reduction of 71% (±5.4%), including nine patients (23%) who reported complete resolution of pain by 30 min post-injection. These outcomes incorporated all those patients suffering from post-traumatic injuries or inflammatory changes (7/7), 7 of 10 (70%) with frozen shoulder, nine of 12 (75%) with rotator cuff tears and three of 9 (30%) with underlying idiopathic causes. A total of 13 patients (33%) noted a reduction of pain at 30 min post-injection, but this reduction did not reach statistical significance. These were patients who presented with degenerative changes (2/2), the majority of those with idiopathic pathologies (6/9, 67%), two of the ten patients with frozen shoulder (20%) and three of those with rotator cuff tears (25%). One patient (1/40, 3%) with frozen shoulder complained of increased pain after the procedure (55% increase since baseline).
At 3 days post-injection, the overall improvement in pain (mean±SEM) since baseline for all patients (n=35) was 20.4% (±4.9) (P<0.001), while the overall improvement in disability was 16.8% (±4.8) (P<0.004). Evaluation at 3 weeks demonstrated no further significant change in pain or disability since baseline (P=0.15 and 0.7 respectively) in the patient cohort (n=35).
The median (±interquartile range) pain and disability scores at each follow-up assessment, as well as the per cent improvement since baseline for those 23 patients who remained in the study until the 6 week follow-up are shown in Table 3 and Table 4 respectively. In these patients, significant improvements in pain scores were achieved by 3 days post-injection (24.2% (±6.9), P=0.005) with no further significant changes observed at the 3 and 6 week follow-ups (P=0.004, Table 3). By 3 days post-injection, disability scores had improved by 20.7% (±7.1) (P=0.02). However, disability did not improve significantly over the 6 week follow-up period (P=0.06, Table 4).
At 3 weeks, 10 of 35 (29%) patients stated that the procedure had had a noticeable effect on their pain levels. Six of the 12 (50%) patients with rotator cuff tears and three of the five patients (60%) presenting with post-traumatic shoulder injuries had improved as a result of the injection. The majority of patients with frozen shoulder (8/10, 80%) were unaffected by the injection. Only one of those patients (1/10, 10%) demonstrated an improvement as a result of the procedure, while another complained of increased pain (30.5% increase) 3 weeks post-injection. Disability scores in that patient, however, remained unchanged. Only two of the nine patients (22%) with unknown underlying pain and disability were improved during follow-up. None of the four patients with inflammatory or degenerative changes benefited from the procedure.
Five of the 23 patients (22%) who were still in the study at the 6 week follow-up maintained improvements in pain since the injection. Of those, the most dramatic improvement was seen in one patient with unknown pathology (68% reduction in pain) and one with a tendon tear (66% reduction in pain).
Adverse effects
Fifteen of the 40 patients reported mild side effects of the nerve block (Table 5). Five had slight pain at the injection site, five had mild to moderate headaches, two had mild nausea and one patient reported localized swelling at the injection site. Two patients noticed temporary numbness in the shoulder and arm. In 13 of the 15 patients, the reported side effects lasted a few hours, while two patients had side effects lasting 24–48 h (headache).
Discussion
The importance of accurate needle placement has been raised in most of the studies investigating the shoulder nerve block injection. However, only a few have assessed the accuracy of the technique by injecting radio-opaque contrast together with the steroid and evaluating the distribution of the contrast on radiography immediately post-injection within the joint space [10, 11, 12]. The demonstrated accuracy rates were reported to vary between 10% and 50%. Experience of the clinician and approach to the injection (anterior versus posterior) seemed to influence the outcomes. Similar observations have been made for epidural steroid injections [13]. Given these facts, it is surprising that an image-guided approach to this procedure has not been tested earlier. For painful conditions affecting the lower back, image-guided interventions have been carried out successfully for several years [14, 15, 16].
The suprascapular nerve supplies sensory fibres to about 70% of the shoulder joint, including the scapula, the acromioclavicular joint and the posterior and superior shoulder joint, but not the anterior or inferior portions of the shoulder. The supraspinatus and infraspinatus muscles are innervated by the suprascapular nerve. Injections of steroids together with an anaesthetic can inhibit the synthesis of inflammatory-mediating substances such as prostaglandins, have been shown to decrease calcification and reduce iron deposition of tissues adjacent to the injection site, increase vascularity and permeability of the synovial membrane, and reduce pain and provide temporary relief of symptoms associated with certain shoulder and other joint pathologies [16, 17, 18, 19].
The results achieved with the CT-guided suprascapular steroid injection were variable and appeared to be associated with the type of pathology. A recent analysis of randomized controlled trials of steroid injections into the shoulder [6] has concluded that there is little evidence to date to provide guidelines on treatment, but that benefit may be dependent upon underlying disease. According to the analysis, patients with rotator cuff disease and adhesive capsulitis appeared to gain some benefit, but the overall effect of the treatment was small and short-lived [20, 21, 22, 23, 24] and the methodology between the studies too variable to allow a direct comparison of the outcomes achieved. The results of our study are similar in that patients with rotator cuff disease or post-traumatic injuries were most likely to benefit from the injection. However, among patients with frozen shoulder, no benefit was observed, with one exception. Nevertheless, clearly defined placement of the needle tip using CT guidance did not improve the outcomes of this technique overall.
It is noteworthy that the patients in our study were all refractory to previous conservative treatment and most had a long history of shoulder pain. However, immediately following the injection the majority of patients recorded complete or substantial pain relief, making this procedure potentially suitable as analgesia preceding painful manipulations such as physiotherapy or hydrodilatation. This technique could also be incorporated in the management of postoperative pain. Previous reports have already shown that the suprascapular nerve block can be successfully administered for pain relief associated with scapular fracture [25], shoulder dislocations [26], and as postoperative pain relief in arthroscopic surgery [27]. Image guidance can afford superior accuracy and safety under these circumstances. However, for long-term relief of pain and disability, different approaches to the suprascapular block may be necessary.
Lewis et al. [28] have shown that in patients suffering from rheumatoid arthritis or osteoarthritis, significant continuing pain relief can be attained by blocking the suprascapular nerve together with the circumflex nerve. The circumflex nerve provides sensory innervations to the anterior and inferior areas of the joint capsule. These authors showed that all 16 patients in the study had significant relief from their pain and disability at 13 weeks post-injection. However, controlled, randomized studies investigating the efficacy of combined nerve blocks are lacking at present.
Repeated steroid injections to the site of pathology may provide more effective relief from the pain of certain soft tissue injuries, but evidence to date is sparse. In patients with frozen shoulder, a series of three suprascapular nerve blocks, each 7 days apart, resulted in a 64% reduction in pain compared with 13% in the placebo group,2 weeks upon completion of the treatment.
It has been suggested that increasing the volume of the anaesthetic (10 ml) may improve the outcomes of the nerve block by facilitating “flooding” of the suprascapular notch, thereby reaching a greater proportion of the nerve and its branches [25]. This may obliterate the need for accuracy in needle positioning by allowing greater volumes to be injected more superficially into the joint, and avoiding close contact of the needle with the neurovascular bundle traversing the suprascapular fossa. It is questionable, however, given the inaccuracy rates reported above, whether increasing the volume of the anaesthetic will lead to continuing pain reduction, especially in the long term. To our knowledge, there are no published reports comparing volumes of injectate and outcomes.
This study has demonstrated that pain relief can be maintained for many hours or days in a few patients with soft tissue pathologies. However, one of the weaknesses of our study was the variety of shoulder pathologies treated in the study population, and hence, patient numbers in each pathology subgroup were too small for results to be conclusive. Furthermore, all our patients had long-term persistent pain and disability and had previously failed to respond to any other treatments. These results warrant further investigations of the technique in patients with more acute shoulder conditions.
References
Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis [?YEAR]; 54:959–964.
Miller H. Plan and operation of the health and nutrition examination survey: United States 1971–1973. Vital and Health Statistics series 1 no. 10. Public Health Service, US Department of Health
Van der Heijden GJMG, van der Windt DAWM, de Winter AF. Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomised clinical trials. BMJ 1997; 315:25–30.
Green S, Buchbinder R, Glazier R. Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessments, and efficacy. BMJ 1998; 316:354–360.
Green S, Buchbinder R, Glazier R Forbes A. Interventions for shoulder pain. Cochrane Database Syst Rev 2002; 2: CD001156.
Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003; 1: CV004016.
Stoker DJ. Intra-articular injections in capsulitis (letter). BMJ 1991; 303:123.
Williams JW, Holleman DR, Simel DL. Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol 1995; 22:727–732.
Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a Shoulder Pain and Disability Index. Arthritis Care Res 1991; 4:142–149.
Eustace JA, Brophy DP, Gibney RP, Bresnihan B, FitzGerald O. Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rheum Dis 1997; 56:59–63.
Jones A, Regan M, Hedingham J, Pattrick M, Manhire A, Doherty M. Importance of placement of intra-articular injections. BMJ 1993; 307:1329–1330.
White AET, Tuite JD. The accuracy and efficacy of shoulder injections in restrictive capsulitis. J Orthop Rheumatol 1996; 9:37–40.
Renfrew DL, Moore TE, Kathol MH, El Khoury GY, Lemke JH, Walker CW. Correct placement of epidural steroid injections: flouroscopic guidance and contrast administration. AJNR Am J Neuroradiol 1991; 12:1003–1007.
El-Khoury GY, Renfrew DL. Percutaneous procedures for the diagnosis and treatment of lower back pain: discography, facet-joint injection, and epidural injection. AJR Am J Roentgenol 1991; 157:685–691.
Gangi A, Kastler B, Klinkert A, Dieteman JL. Interventional radiology guided by a combination of CT and fluoroscopy: technique, indications, and advantages. Semin Interv Radiol 1995; 12:4–14.
Gray RG, Gottlieb NL. Intra-articular corticosteroids. An update assessment. Clin Orthop 1983; 177:235–263.
Goldie I. Local steroid therapy in painful orthopaedic conditions. Scott Med J 1972; 17:176–186.
van de Putte LBA, Joosten LAB, van den Berg WB. Corticosteroids: immediate and delayed risks of intra-articular administration. In: Mummenthaler M, van Zwieten PA, Farcor JM, eds. Treatment of chronic pain. Possibilities, limitations and long term follow up. Chur: Harwood Academic Publishers, 1990:72–75.
Gangi A, Dieteman JL, Mortazavi R, Pfleger D, Kauff C, Roy C. CT-guided interventional procedures for pain management in the lumbosacral spine. Radiographics 1998; 18:621–633.
Petri M, Dobrow R, Neiman R, Whiting-O’Keefe Q, Seaman W. Randomised double blind placebo controlled study of the treatment of the painful shoulder. Arthritis Rheum 1987; 30:1040–1045.
Adebajo A, Nash P, Hazleman B. A prospective double blind dummy placebo controlled study comparing triamcinolone hexacitonide injection with oral diclofenac in patients with rotator cuff tendonitis. J Rheumatol 1990; 17:1207–1210.
Blair B, Rokito AS, Cuomo F, Jarolem K, Zuckerman JD. Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am 1996; 78:1685–1689.
Van der Windt DA, Koes BW, Boeke AJ, Deville W, De Kong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996; 46:519–523.
Plafki C, Steffen R, Willburger RE, Wittenberg RH. Local anaesthetic injection with and without corticosteroids for subacromial impingement syndrome. Int Orthop 2000; 24:40–42.
Breen TW, Haigh JD. Continuous suprascapular nerve block for analgesia of scapular fracture. Can J Anaesth 1990; 37:786–788.
Gleeson AP, Graham CA, Jones I, Beggs I, Nutton RW. Comparison of intra-articular lignocaine and a suprascapular nerve block for acute anterior shoulder dislocation. Injury 1997; 28:141–142.
Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: A new modality? Anesth Analg 1997; 84:1306–1312.
Lewis RN. The use of combined suprascapular and circumflex (articular branches) nerve blocks in the management of chronic arthritis of the shoulder joint. Eur J Anaesthesiol 1991; 16:37–41.
Dahan THM, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomised clinical trial examining the efficacy of Bupivacaine in suprascapular nerve blocks in frozen shoulder. J Rheumatol 2000; 27:1464–1469.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider-Kolsky, M.E., Pike, J. & Connell, D.A. CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol 33, 277–282 (2004). https://doi.org/10.1007/s00256-003-0733-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-003-0733-y