Abstract
Purpose
The aim of this prospective and randomized study was to compare the effects of general anesthesia to the combination of general anesthesia and continuous interscalene block on postoperative pain and functional outcomes in patients undergoing arthroscopic rotator cuff repair.
Methods
This study included a total of 85 patients aged 45–74 years, who were scheduled for elective arthroscopic rotator cuff repair. One group consists of patients who underwent only general anesthesia (GA, N = 43), and the other group consists of patients who underwent a combination of continuous interscalene brachial plexus block and general anesthesia (CISB + GA, N = 42). Pain levels of the patients were evaluated postoperatively by a visual analog scale. Shoulder function was evaluated preoperatively and postoperatively using the Constant score.
Results
Patients in the CISB + GA group had lower postoperative visual analog scores and less additional analgesic needs during the early postoperative period than those in the GA group. Constant scores of the patients in the CISB + GA group at postoperative week 6 were higher than those in the GA group. Evaluation of the functional outcomes at 6 months postoperatively showed that there were no significant differences between the two groups.
Conclusion
Although CISB significantly improved postoperative pain control and early (in the first 6 weeks) functional outcomes following arthroscopic rotator cuff repair, there was no significant difference between the CISB group and CISB + GA group at 6 months.
Level of evidence
Level II, Randomized Controlled Trial, Treatment Study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Shoulder pain is one of the common disorders of the musculoskeletal system, and its prevalence increases with age [1]. Although there are many structures that comprise the shoulder joint, shoulder pain is commonly caused by the rotator cuff (65–70%) [2]. In patients with symptomatic rotator cuff tears, the preferred treatment method to relieve pain and restore shoulder function is surgical repair [3]. Rotator cuff repair can be performed by open, arthroscopic, or combined techniques. However, the popularity of arthroscopic shoulder surgery is increasing owing to the advances in arthroscopic repair techniques [4]. Among the arthroscopic surgical procedures for the shoulder joint, rotator cuff repair is one of the procedures with the highest rate of postoperative pain [4]. Pain not only increases the duration of hospitalization but also negatively affects patient satisfaction and clinical outcomes [5]. Different approaches have been developed to reduce postoperative pain and opioid use, and one of the most effective of these is peripheral nerve blocks [6]. Our hypothesis in this study is that functional outcomes can be improved in patients undergoing arthroscopic rotator cuff repair (ARCR) by effective postoperative pain control. Based on this hypothesis, this study aimed to compare the functional outcomes of patients who underwent continuous interscalene brachial plexus block and general anesthesia (CISB + GA) and patients undergoing general anesthesia (GA) at 6 weeks and 6 months postoperatively.
Materials and methods
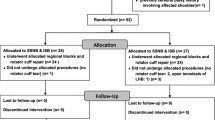
After obtaining approval from the institutional ethics committee review board (February 10, 2015/03-10) and informed patient consent, 122 patients aged ≥ 18 years with a body mass index of ≤ 35 kg/m2 and American Society of Anesthesiologists (ASA) physical status I or II and who had been scheduled for elective ARCR between February 2015 and January 2018 were identified as suitable for this study. “Block randomization method” was used for this prospective randomized study. Assignment of patients to groups was performed using computer-generated randomization numbers. After confirmation of inclusion and exclusion criteria, the method of treatment was assigned according to the randomization number obtained from a sealed envelope. A total of 85 patients (GA = 43 patients, CISB + GA = 42 patients) who met the inclusion criteria and completed the follow-up period were included in the study (Fig. 1).
Anesthesia and analgesia
After moving the patients to the operating room, standard procedures, including ECG, noninvasive blood pressure, pulse oximetry, bispectral monitoring, and intravenous infusion, were initiated. Midazolam (0.1 mg/kg IV) was administered to the patients in all groups for premedication. Intraoperative 1000 mg paracetamol IV was administered. Patients were monitored during surgery and recovery based on standard guidelines published by the American Society of Anesthesiologists.
Patients in the CISB + GA group were administered blocks by an anesthesiologist with sufficient experience in the peripheral blocks. Blocks were administered using an ultrasound-guided stimulator [7]. Patients were in a supine position with the head facing the opposite side. A high-frequency (8–12 MHz) linear probe covered with sterile sheath was placed on the neck, on the side to be operated. Interscalene trunks were identified between the anterior and middle scalene muscles. After local anesthesia was administered to the skin with 1% lidocaine, the 50-mm 18-gauge insulated block needle (Contiplex® Tuohy, B. Braun Medical, Bethlehem, PA) was advanced from the lateral to the medial muscles so as to place the needle tip in the region between the upper and middle trunks (C5–C6) of the brachial plexus. A neurostimulator (Stimuplex® Dig RC; B Braun Medical, Bethlehem, PA) was used to monitor motor response (0.5 mA, 0.1 ms) in the deltoid and biceps muscles, and the location of the needle tip was confirmed. The catheter was then advanced until it passed the needle tip, and the needle was withdrawn. After negative aspiration, 30 ml of 0.25% bupivacaine (Bustesin® 0.5%) was administered to the brachial plexus nerve sheath. Sensorial changes and motor function following the injection of local anesthetics were measured every 5 min for the first 30 min. Complete loss of pinprick sensation and motor function was considered as the beginning of the interscalene block. GA was administered to the patients following interscalene block; 1.5–2.5 mg kg−1 propofol, 0.5 mg kg−1 rocuronium, and 3 μg kg−1 fentanyl were used in anesthesia induction, and 2–3% sevoflurane and 0.6 μg kg dk−1 remifentanil in 50% O2 + 50% air were used in anesthesia maintenance. At the end of the surgery, patients were antagonized with 4 mg kg−1 sugammadex to restore spontaneous breathing and then they were extubated. General anesthesia was administered to the patients in the general anesthesia (GA) group. After extubation, the patients were transferred to the post-anesthesia care unit (PACU). A total of 5 ml/h of 0.125% bupivacaine infusion was initiated in patients with interscalene catheter. An infusion pump was used for this. Pain intensity of the patients at 1, 6, 12, and 24 h was evaluated with a visual analog scale (VAS) (0: no pain and 10: worst possible pain). Interscalene catheter was removed 24 h after surgery.
Furthermore, 25 mg dexketoprofen (every 12 h) and 500 mg paracetamol (every 8 h) tablets were administered to all patients until they were discharged. Intravenous analgesics were given to patients with pain in spite of this treatment, based on the pain step protocol [8]. The protocol is as follows: by using an 11-point numeral rating scale (NRS; 0, no pain; 10, worst pain): step 0: NRS 0–2: no further analgesics, step 1: NRS 3–4: 1000 mg paracetamol IV, step 2: NRS 5–6: 1000 mg paracetamol IV and 30 mg ketorolac IV, and step 3: NRS 7–10: 1000 mg paracetamol IV and 30 mg ketorolac IV and 100 mg tramadol IV. Postoperative extra analgesic requirements of the patients in both groups were recorded.
Surgical technique
All patients were operated in lateral decubitus position and with 4–4.5 kg traction on the upper extremity. Normal saline was used as irrigation fluid in all patients, irrigation fluid pump was kept within previously defined limits so as to maintain the pressure between 40 and 80 mm/hg, and the flow rate was 50–150 mL/min [9]. In total, 3 or 4 portals were used for surgical procedures. The standard arthroscopic examination was performed. Bursectomy and limited acromioplasty were performed in all patients. The degree of biceps tendinopathy was intraoperatively evaluated, and the patients with delamination or partial rupture were treated with tenotomy. The extension and retraction of the rotator cuff rupture were intraoperatively determined according to the criteria defined by Boileau et al. [10]. The location where the rotator cuff was attached to the greater tuberosity was prepared by using a shaver. Single-row repair was performed using knotless suture anchors and nonabsorbable No. 2 sutures (Footprint PK, Smith & Nephew Endoscopy, Andover, MA, USA). A total of 1–3 anchors were used according to the size of the rotator cuff rupture.
Postoperative protocol
The operated shoulders were immobilized for 3 weeks using a sling immobilizer with abduction pad. Isometric cuff exercises and relaxation exercises for shoulder muscles were initiated on the first day after surgery. After 3 weeks of immobilization, passive and assisted-active exercises were initiated. After the sixth week, strengthening exercises for rotator cuff muscles and scapula stabilizers were initiated. Three months after the surgery, patients were allowed to engage in light sports activities. Full activity and heavy work were allowed based on the patients’ recovery at 6 months after the operation.
Imaging
Preoperative evaluations of all patients were performed with standard X-rays and MRI. Fatty infiltration was assessed by MRI (stage 0: completely normal muscle; stage 1: muscle contains striations of fatty degeneration; stage 2: marked fatty degeneration, but there is more muscle mass; stage 3: equal muscle mass and fatty degeneration; and stage 4: more fatty degeneration than muscle mass) [11].
Functional outcomes
Shoulder function of each patient was evaluated using the Constant score (CS) [12] at 6 weeks and 6 months postoperatively. CS is a validated outcome score commonly used to assess shoulder function [13, 14]. The CS system is a shoulder function scale with the highest score of 100 points in which high scores indicate good shoulder functions [12]. This scoring system consists of four separate subscales: subjective pain (15 points), function (20 points), objective clinical assessment of range of motion (40 points), and strength (25 points) [12]. Visual analog scale was used to assess the pain level of the patients.
Statistical analysis
Statistical package for the social sciences (SPSS 21, Chicago, IL, USA) was used for statistical analysis of the data. Categorical variables were described using relative frequency, and continuous variables were described using mean and standard deviation (SD). Distribution of continuous variables was investigated by Kolmogorov–Smirnov and Shapiro–Wilk normality tests. Mann–Whitney U-test was used in detecting the relationship between the dual groups not conforming to normal distribution. Chi-square test or Fisher’s exact test was used in the analysis of categorical variables. P < 0.05 was accepted as significant in all analyses.
Results
Preoperative and postoperative data of 85 patients who met the inclusion criteria of our study and completed their follow-up were analyzed (Fig. 1). There was no significant difference between the two groups in terms of preoperative shoulder functions and demographic characteristics (Table 1). Biceps tenotomy did not influence the functional outcomes at 6 weeks and 6 months postoperatively in both groups (GA group, P = 0.33 and P = 0.32; CISB + GA group, P = 0.22 and P = 0.27, respectively). There were no life-threatening complications in the intraoperative and postoperative period. The mean intraoperative heart rate, mean systolic blood pressure, mean duration of surgery, mean pressure, and mean flow rate of the irrigation fluid used in the CISB + GA group were significantly lower than the patients’ in the GA group (P < 0.05) (Table 2). In addition, the VAS scores of patients in the CISB + GA group at 1, 6, 12, and 24 h postoperatively and additional analgesic requirements in the early postoperative period were significantly lower than those in the GA group (P < 0.05) (Table 3). There was no significant difference between the groups in terms of hospitalization duration (Table 3). Comparison of the groups in terms of functional outcomes at 6 weeks postoperatively showed that the CS scores of the patients in the CISB + GA group were significantly higher than those of the patients in the GA group (P < 0.05) (Table 4). The evaluation of the functional outcomes at 6 months postoperatively revealed that there was no significant difference between the two groups (P > 0.05) (Table 4).
Discussion
Patients undergoing rotator cuff repair experience a higher level of pain than the other arthroscopic shoulder procedures [15]. Several techniques such as oral analgesia, cold therapy, local anesthetic infusion to the subacromial space, and the single or continuous interscalene brachial plexus blocks have been used for postoperative pain control after arthroscopic rotator cuff repairs [15]. Among these methods, one of the most effective ones is interscalene brachial plexus blocks [16]. The previous studies have shown that continuous interscalene brachial plexus block is more effective in reducing postoperative pain and opioid consumption than single-shot interscalene block [17, 18]. The reason for this is that the effect of single-shot interscalene block lasts a maximum of 12 h and then rebound pain occurs [18]. There are limited number of studies in the literature investigating the beneficial effects of CISB on postoperative pain management in terms of long-term functional outcomes after ARCR. From this perspective, we investigated the effect of CISB on the functional outcomes of patients after ARCR in this study. As it is known, early motion after surgical intervention on joints has been shown to lead to improved results [19]. One of the most important factors that restrain early mobility is pain [19]. Well management of pain in the postoperative period encourages the patient for early mobility, which positively affects functional outcomes [20, 21]. In our study, patients who underwent continuous interscalene brachial plexus block had improved postoperative analgesia than those who underwent only GA. Almost all of the patients in the GA group (93%) required opioid analgesic intervention in the PACU, whereas none of the patients in the CISB + GA group required any additional opioid analgesic intervention. Similarly, the VAS scores of the patients at 1, 6, 12, and 24 h postoperative and additional analgesic requirements were significantly lower in patients in the CISB + GA group than in the GA group. The results obtained in our study were consistent with those of the previous studies [17, 22]. Better postoperative pain management in the CISB + GA group resulted in better adaptation of these patients to routine exercise programs than those in the GA group.
Prolonged hospitalization in patients undergoing CISB is one of the major problems of this method. In fact, in a recent study, it was found that the duration of hospitalization in patients undergoing CISB was 1.6 times higher than in those who were treated with single-shot interscalene blocks [18]. In our study, the duration of CISB application was 24 h and there was no significant difference between the groups in terms of hospitalization duration (P > 0.05). In the previous studies, it was observed that the duration of CISB application ranged from 24 to 72 h [17, 23, 24].
One of the rare studies investigating the long-term functional outcomes in the patients who were treated with interscalene block is the study of Stevens et al. [25]. In this study, interscalene block was performed by using two different catheters, and the functional outcomes of the patients were evaluated at 6 weeks postoperatively. They found that the functional improvement at week 6 was better in the group treated with interscalene block by using a stimulating catheter [25]. Similarly, significant improvement was observed at 6 weeks postoperatively in the CS scores of patients who underwent CISB in our study. In addition, to determine the changes in functional improvement in the following periods, we evaluated the functional outcomes of the patients at 6 months postoperatively and found that there was no significant difference between the groups in this period (P > 0.05). The reason for this may be the decrease in the adverse effects of pain during the postoperative period and a delay in patients starting rehabilitation programs. In their study, Gallagher et al. [26] reported that early rehabilitation provided significant functional improvement, particularly in the first 3–6 months postoperatively in patients who underwent arthroscopic rotator cuff repair. In our study, we observed that the early functional improvement provided by early rehabilitation in the CISB + GA group was similar to that in the GA group at 6 months.
Intraoperative heart rate, systolic blood pressure, pressure, and flow rate of irrigation fluid were evaluated in patients who underwent arthroscopic rotator cuff repair. Patients in the CISB + GA group had lower intraoperative heart rate and lower systolic blood pressure than those in the GA group (P < 0.05). In shoulder arthroscopy, controlled hypotension is the most effective method that is used to reduce bleeding and improve arthroscopic visualization quality [27]. Therefore, it is recommended to maintain systolic blood pressure between 90 and 100 mmHg [27]. In our study, systolic blood pressure was more optimal in CISB + GA patients and intraoperative bleeding was minimal. As a result, a good arthroscopic visualization was obtained and the mean pressure and flow rate of the irrigation fluid were lower in the CISB + GA group than in the GA group. At the same time, mean duration of surgery was shorter in the CISB + GA group than in the GA group. Thus, keeping low irrigation fluid pressure and a short duration of surgery decreases fluid extravasation and also decreases the serious side effects associated with it [28].
In addition to these intraoperative and postoperative benefits of interscalene brachial plexus block, complications at a rate of 2–4% have been reported in the literature [29]. Complications such as brachial plexus injuries, respiratory system complications, central nervous system complications, and cardiovascular complications may be noted in association with interscalene brachial plexus block; however, almost all these complications are temporary [29]. In our study, transient ipsilateral hemidiaphragmatic paresis was observed in four patients. This complication recovered spontaneously within 12–24 h after catheter removal. It is also reported that this complication is frequently encountered and is observed almost in all patients [30]. Complications such as prolonged numbness, radiating pain in the distribution of the brachial plexus, and motor weakness were not noted in any of our patients.
Our study has some limitations. First, the total sample size is relatively small. Second, while we define our study as a prospective randomized controlled trial, patients and observers were not fully blinded. Last limitation of our study is the lack of radiological evaluation of the re-rupture at the final follow-up of the patients. Because, re-rupture is one of the most important factors affecting long-term results after the rotator cuff repair.
Conclusion
In conclusion, in our study, CISB significantly improved both postoperative pain control and early functional outcomes after ARCR. Functional improvement was more evident at 6 weeks postoperatively. At 6 months postoperatively, there was no difference in functional outcomes between patients who underwent CISB and patients who did not. Although CISB has had a positive effect on functional outcomes in the early period, the additional time and cost for CISB should be evaluated in terms of the effectiveness to consider it as a treatment option.
References
Luime JJ, Koes BW, Hendriksen IJ, Burdorf A, Verhagen AP, Miedema HS, Verhaar JA (2004) Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol 33(2):73–81
Jain NB, Fan R, Higgins LD, Kuhn JE, Ayers GD (2018) Does my patient with shoulder pain have a rotator cuff tear? A predictive model from the row cohort. Orthop J Sports Med 6(7):2325967118784897. https://doi.org/10.1177/2325967118784897
Plachel F, Traweger A, Vasvary I, Schanda JE, Resch H, Moroder P (2018) Long-term results after arthroscopic transosseous rotator cuff repair. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2018.09.003
Day M, Westermann R, Duchman K, Gao Y, Pugely A, Bollier M, Wolf B (2018) Comparison of short-term complications after rotator cuff repair: open versus arthroscopic. Arthroscopy 34(4):1130–1136. https://doi.org/10.1016/j.arthro.2017.10.027
Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone JN, Flatow EL (2006) Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elbow Surg 15(5):567–570. https://doi.org/10.1016/j.jse.2006.01.009
Wu CL, Rouse LM, Chen JM, Miller RJ (2002) Comparison of postoperative pain in patients receiving interscalene block or general anesthesia for shoulder surgery. Orthopedics 25(1):45–48
Perlas A, Chan VW (2004) Ultrasound-guided interscalene brachial plexus block. Tech Reg Anesth Pain Manag 8(4):143–148
Lehmann LJ, Loosen G, Weiss C, Schmittner MD (2015) Interscalene plexus block versus general anaesthesia for shoulder surgery: a randomized controlled study. Eur J Orthop Surg Traumatol 25(2):255–261. https://doi.org/10.1007/s00590-014-1483-3
Gupta S, Manjuladevi M, Vasudeva Upadhyaya KS, Kutappa AM, Amaravathi R, Arpana J (2016) Effects of irrigation fluid in shoulder arthroscopy. Indian J Anaesth 60(3):194–198. https://doi.org/10.4103/0019-5049.177866
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Jt Surg Am 87(6):1229–1240. https://doi.org/10.2106/JBJS.D.02035
Horiuchi S, Nozaki T, Tasaki A, Yamakawa A, Kaneko Y, Hara T, Yoshioka H (2017) Reliability of MR quantification of rotator cuff muscle fatty degeneration using a 2-point Dixon technique in comparison with the Goutallier classification: validation study by multiple readers. Acad Radiol 24(11):1343–1351. https://doi.org/10.1016/j.acra.2017.03.026
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Rocourt MH, Radlinger L, Kalberer F, Sanavi S, Schmid NS, Leunig M, Hertel R (2008) Evaluation of intratester and intertester reliability of the Constant–Murley shoulder assessment. J Shoulder Elbow Surg 17(2):364–369. https://doi.org/10.1016/j.jse.2007.06.024
Blonna D, Scelsi M, Marini E, Bellato E, Tellini A, Rossi R, Bonasia DE, Castoldi F (2012) Can we improve the reliability of the Constant–Murley score? J Shoulder Elbow Surg 21(1):4–12. https://doi.org/10.1016/j.jse.2011.07.014
Calvo E, Torres MD, Morcillo D, Leal V (2018) Rotator cuff repair is more painful than other arthroscopic shoulder procedures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-018-3100-0
Bowens C Jr, Sripada R (2012) Regional blockade of the shoulder: approaches and outcomes. Anesthesiol Res Pract 2012:971963. https://doi.org/10.1155/2012/971963
Salviz EA, Xu D, Frulla A, Kwofie K, Shastri U, Chen J, Shariat AN, Littwin S, Lin E, Choi J, Hobeika P, Hadzic A (2013) Continuous interscalene block in patients having outpatient rotator cuff repair surgery: a prospective randomized trial. Anesth Analg 117(6):1485–1492. https://doi.org/10.1213/01.ane.0000436607.40643.0a
Kim JH, Koh HJ, Kim DK, Lee HJ, Kwon KH, Lee KY, Kim YS (2018) Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 27(7):1243–1250. https://doi.org/10.1016/j.jse.2018.02.048
Faryniarz D, Morelli C, Coleman S, Holmes T, Allen A, Altchek D, Cordasco F, Warren RF, Urban MK, Gordon MA (2006) Interscalene block anesthesia at an ambulatory surgery center performing predominantly regional anesthesia: a prospective study of one hundred thirty-three patients undergoing shoulder surgery. J Shoulder Elbow Surg 15(6):686–690. https://doi.org/10.1016/j.jse.2006.02.001
Chelly JE, Greger J, Gebhard R, Coupe K, Clyburn TA, Buckle R, Criswell A (2001) Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplast 16(4):436–445. https://doi.org/10.1054/arth.2001.23622
Hadzic A, Arliss J, Kerimoglu B, Karaca PE, Yufa M, Claudio RE, Vloka JD, Rosenquist R, Santos AC, Thys DM (2004) A comparison of infraclavicular nerve block versus general anesthesia for hand and wrist day-case surgeries. Anesthesiology 101(1):127–132
Yan S, Zhao Y, Zhang H (2018) Efficacy and safety of interscalene block combined with general anesthesia for arthroscopic shoulder surgery: a meta-analysis. J Clin Anesth 47:74–79. https://doi.org/10.1016/j.jclinane.2018.03.008
Malik T, Mass D, Cohn S (2016) Postoperative analgesia in a prolonged continuous interscalene block versus single-shot block in outpatient arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy 32(8):1544–1550. https://doi.org/10.1016/j.arthro.2016.01.044
Klein SM, Grant SA, Greengrass RA, Nielsen KC, Speer KP, White W, Warner DS, Steele SM (2000) Interscalene brachial plexus block with a continuous catheter insertion system and a disposable infusion pump. Anesth Analg 91(6):1473–1478
Stevens MF, Werdehausen R, Golla E, Braun S, Hermanns H, Ilg A, Willers R, Lipfert P (2007) Does interscalene catheter placement with stimulating catheters improve postoperative pain or functional outcome after shoulder surgery? A prospective, randomized and double-blinded trial. Anesth Analg 104(2):442–447. https://doi.org/10.1213/01.ane.0000253513.15336.25
Gallagher BP, Bishop ME, Tjoumakaris FP, Freedman KB (2015) Early versus delayed rehabilitation following arthroscopic rotator cuff repair: a systematic review. Phys Sportsmed 43(2):178–187. https://doi.org/10.1080/00913847.2015.1025683
Gillespie R, Shishani Y, Streit J, Wanner JP, McCrum C, Syed T, Haas A, Gobezie R (2012) The safety of controlled hypotension for shoulder arthroscopy in the beach-chair position. J Bone Jt Surg Am 94(14):1284–1290. https://doi.org/10.2106/JBJS.J.01550
Memon M, Kay J, Gholami A, Simunovic N, Ayeni OR (2018) Fluid extravasation in shoulder arthroscopic surgery: a systematic review. Orthop J Sports Med 6(5):2325967118771616. https://doi.org/10.1177/2325967118771616
Lenters TR, Davies J, Matsen FA 3rd (2007) The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg 16(4):379–387. https://doi.org/10.1016/j.jse.2006.10.007
Nickless JT, Waterman BR, Romeo AA (2018) Persistent diaphragmatic paralysis associated with interscalene nerve block after total shoulder arthroplasty: a case report. JSES Open Access 2(3):165. https://doi.org/10.1016/j.jses.2018.05.003
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gurger, M., Ozer, A.B. A comparison of continuous interscalene block versus general anesthesia alone on the functional outcomes of the patients undergoing arthroscopic rotator cuff repair. Eur J Orthop Surg Traumatol 29, 1659–1666 (2019). https://doi.org/10.1007/s00590-019-02482-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02482-8