Abstract
Purpose
The purpose of this prospective study was to evaluate how early the bone plug was integrated into the rectangular femoral tunnel after anatomical ACL reconstruction using a bone-patellar tendon-bone (BTB) graft via a rectangular tunnel (RT BTB ACL-R).
Methods
Twenty consecutive patients who had undergone the reconstruction procedure were evaluated by CT scans at 4 and 8 weeks postoperatively. In each scan, 30 slices for multiplanar reconstruction were collected parallel to the long axis of the parallelepiped femoral tunnel and perpendicular to the tendinous plane of the bone plug. Each slice was classified as “complete,” indicating no visible gap between the plug and the tunnel wall or trabecular continuity or “incomplete,” showing a visible gap. Bone plug-tunnel integration was evaluated as “excellent,” “good,” “fair,” or “poor” for >20, 11–20, 5–10, and <4 “complete” slices, respectively.
Results
In this evaluation, 55% of the patients were rated as “excellent” on the first scan, and 80% were “excellent” on the second scan, showing healing over time. The CT values at the anterior interface between the bone plug and the tunnel wall were also measured on both scans. The mean changes in CT value at 8 weeks were significantly lower than those at 4 weeks.
Conclusion
This study shows that bone plug-femoral tunnel integration was almost complete by 8 weeks after surgery using RT BTB ACL-R.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Secure graft fixation with a proper femoral tunnel is an important factor in ACL reconstruction, especially in the early postoperative period [3, 13, 16]. Shino et al recently developed an innovative operative procedure in which a BTB graft is placed to mimic the natural fiber arrangement of the normal ACL following the concept of double-bundle reconstruction, with the additional goal of maximizing the graft-tunnel contact area [25, 26]. Thus, a parallelepiped femoral tunnel with a rectangular aperture is created in accordance with the rectangular cross section of the graft. This method seems to be beneficial for graft-bone integration in the femoral tunnel.
In principle, a wider interface and closer contact is likely to lead to earlier bone plug integration, but it is difficult to determine the period required for the grafted bone to integrate into the tunnel postoperatively. The time period for graft-tunnel integration has been examined in conventional round tunnel ACL reconstruction [7, 9, 14] but has not been studied in detail in rectangular tunnel ACL reconstruction. Our hypothesis was that the bone plug could be integrated into the rectangular femoral tunnel in early postoperative stage after RT BTB ACL reconstruction. Thus, this prospective study was to evaluate minute changes in bone plug integration using macroscopic analysis of slices from CT-MPR images and to examine macroscopically undetectable changes using CT values.
Materials and methods
Twenty consecutive patients (19 men; 1 woman) of the average age of 21 years old (range, 16–36) were included in the study. The average time from injury to surgery was 124 days (range, 7–376). All subjects gave informed consent prior to participating in the study.
Surgical technique and postoperative regimen
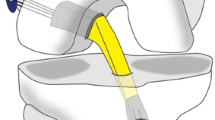
The details of the RT BTB ACL-R procedure have been described previously [25, 26] (Fig. 1). All patients underwent arthroscopic primary RT BTB ACL-R performed by one orthopedic surgeon (K.S.). Briefly, a 10-mm-wide BTB graft was harvested from the central portion of the patellar tendon with 15-mm-long bone plugs on both ends. The tibial bone plug was shaped to a size of 5 × 10 × 15 mm (thickness × width × length) and used for the femoral socket (Fig. 1).
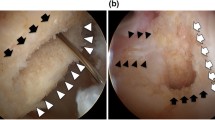
The surgical procedure of rectangular BPTB-ACL reconstruction under a clear view with an oblique arthroscope through the anteromedial portal with the knee in 90°C of flexion, the bony surface undulation around the ACL attachment area is clearly observed (a). The created 5-mm-wide, 10-mm-long, 20-mm-deep parallelepiped socket inside the attachment area. Note the “resident’s ridge” (solid arrows) (b)
Viewing the ACL femoral attachment area with a 45°C oblique arthroscope through the AM portal, the fibrous tissue is delicately removed using radiofrequency device with the knee flexed at 75–80°C by gravity. After cleaning, an almost linear “resident’s ridge” was consistently visualized on the wall (Fig. 1a). Since this ridge forms as the anterior border of the attachment area, the crescent-shaped attachment area is clearly delineated [8, 11, 27]. A 5 × 10 × 20 mm rectangular parallelepiped socket was created with an inside-out dilator posterior to the resident’s ridge [1] (Fig. 1b) (SNE#6901100 femoral dilator 5_10, Ref #6901100; Smith & Nephew Endoscopy).
With two leading sutures, the graft was passed from the tibial tunnel to the femoral socket with the parallelepiped bone plug kept on top and the cancellous bone surface maintained anteriorly (Fig. 2). Femoral graft fixation with a 6 mm × 20–30 mm interference screw was achieved in an outside-in fashion using a 7-mm skin protector (SNE#6901106) through an additional small lateral femoral incision. Tibial fixation was achieved with a modified pullout suture technique using the DSP (Double Spike Plate, made by Meira Co., Aichi, Japan, and distributed by SNE) system to fix the graft under a predetermined amount of tension [23].
The bone plug of the graft was introduced into the tunnel with its tendinous portion placed posteriorly and fixed with an 6-mm interference screw just posterior-superior to the bone plug (a). Oblique axial (b) multiplanar reconstruction computed tomography 30 images obtained parallel to the femoral rectangular tunnel and bone plug. Bony integration at the just anterior interface (ACL force direction) between the bone plug and the tunnel wall was evaluated (c arrow). Examples of “incomplete” slice (d) with visible hair line or gap and “complete” one (e) showing absence of a border or presence of trabecular continuity
Postoperatively, the knee was immobilized in 10–15°C for a week with a brace. Partial weight bearing was allowed at 2 weeks, followed by full weight bearing at 4 weeks.
Radiographic analysis
The patients underwent multi-detector computed tomography (MDCT) with multiplanar reconstruction (MPR) using an Asteion 4 Multislice CT System (Toshiba Medical Systems, Tochigi, Japan) at 3–5 weeks and 7–8 weeks postoperatively. Each CT scan was performed with the following parameters: 512 × 512 matrix, 1.00 mm slice thickness, 120 kVp, and 150 mA. Volume data were saved with a DICOM pattern and imaging software (Virtual Place-M; AZE Ltd., Tokyo Japan) was used to create MPR images. Since the bone plug and femoral tunnel are rectangular parallelepipeds of 5 × 10 × 15 mm, 30 slices were created parallel to the long axis of the parallelepiped bone plug and perpendicular to its tendinous plane (Fig. 2). Similar CT images for 4 patients were also taken at a mean of 3 days (range, 2–4 days) after surgery to examine the conditions prior to healing.
Morphological CT evaluation
For morphological CT evaluation, the 30 reconstructed slices were evaluated as “complete,” indicating no border between the plug and the tunnel wall or showing trabecular continuity or “incomplete,” indicating a visible gap of >1 mm [7]. To evaluate bone integration, cases in which >20 of the 30 slices were categorized as “complete” without bone absorption were determined to be “excellent” and those with 11–20, 5–10, and <5 “complete” slices were classified as “good,” “fair,” and “poor,” respectively. Data from these evaluations were compared at the two time points after surgery (Fig. 2).
CT value changes
For a more detailed quantitative analysis, the CT value was determined for a slice selected from the central portion (landmark of suture hall) of the 30 slices as a region of interest. In the selected slice, a straight line of 1.5 cm was drawn perpendicular to the long axis of the bone plug using image analysis software (virtual place M). This made it possible to visualize the CT value sequentially at each point on a graph (Fig. 3). Since the value changes from anterior to posterior according to the bone mineral density (BMD), the graph has a minimum at the point of the interface (point b in Fig. 3) at the anterior wall of the tunnel of dilated cancellous bone (point a in Fig. 3), reaches a peak at the cortex of the bone plug (point c in Fig. 3), and then decreases to the lowest value in the tendinous region. Since the BMD varies among patients, the change in the CT value at the interface and the depth of the minimum were normalized by dividing by the peak value for the cortex. In this manner, the relative drop in the CT value was calculated and expressed as a percentage.
The CT value was measured sequentially from anterior to posterior through the bone plug along the transverse cutting. The anterior wall of the tunnel of dilated cancellous bone was defined as “point a,” a minimum at the point of the interface as “point b,” and a peak at the cortex of the bone plug as “point c,” after which the CT value decreased to the lowest level in the tendinous region
Reliability measurement
Reliability calculations were based on positioning the planes for the MPR and determine the ingrowth on each slice by the same observer (three time repeat) and by three different observers (T.S., H.O., and T.I.). The intra- and inter-observer intraclass correlation coefficient (ICC) and kappa coefficient were calculated, respectively. After assessing reliability measurement, one author determined the positioning the plane for MPR and the ingrowth on each slice.
Statistical analysis
The mean numbers of slices sorted into each category for the first and second CT scans were compared by paired t test. A P value of less than 0.05 was considered to indicate a significant difference.
Results
There were no intraoperative complications during fixation of the bone plug, including blow-out cortical fracture, bone plug fracture, bone plug dislocation, and graft failure.
Reliability measurement
The intra- and inter-observer intraclass correlation coefficient (ICC) concerning the measurements of radiographic assessment on positioning the planes for the MPR was 0.95 and 0.91. kappa coefficient was 0.83. The intra- and inter-observer reliabilities were substantial to excellent.
In the first postoperative week (days 2 and 4), all slices were macroscopically “incomplete” with a clear gap, leading to a classification of “poor” integration. The normalized change in the CT value at the border was 14.2 ± 4.3, and points a and b showed especially sharp angles in the graph (Tables 1, 2; Fig. 3).
In the first scan after 4 weeks (range 3–5 weeks), 19.3 ± 6.7 of the 30 slices were evaluated as macroscopically “complete” and 10.7 ± 5.4 slices were “incomplete.” Of the 20 cases, 55% were categorized as showing “excellent” integration (Tables 1, 2).
In the second scan after 8 weeks (range 7–9 weeks), 25.1 ± 5.4 of the 30 slices were macroscopically “complete,” showing a significant increase compared to 4 weeks (P = 0.004) and 4.9 ± 4.8 were “incomplete,” indicating a significant decrease over time (P = 0.00004) (Table 1). Of the 20 cases, 80% showed “excellent” integration (Fig. 4). The normalized change in the CT value at the border was 10.9 ± 7.2, which was significantly lower than this value at 4 weeks (P = 0.00305) (Tables 1, 2).
Discussion
The most important finding in this study was that the bone plug was integrated into femoral tunnel in early postoperative stage after RT BTB ACL reconstruction using macroscopic analysis of slices from CT-MPR images and to examine macroscopically undetectable changes using CT values.
One of the keys to success in ACL reconstruction is to restore the bone-tendon junction around the ACL femoral attachment [15, 29]. Since tremendous stress is exerted on the ACL femoral attachment in the functional position of the knee, and because the force direction in this area is dramatically changed by knee flexion and extension [10, 20], early re-establishment of the bone-tendon junction is desirable [3, 13, 16, 19, 21]. However, excessive gap space may be present around the interference screw used for fixing a parallelepiped or triangle pillar bone plug into a round tunnel in the traditional operation (Fig. 4) [13, 14, 22]. In contrast, the technique used in this study, in which the bone plug is first matched to the parallelepiped bone tunnel with subsequent screw fixation, may be better for earlier biological bone plug-tunnel integration and reestablishment of the bone-tendon junction by maximizing the interface of the graft and tunnel wall (Fig. 4) [4, 5, 17, 24].
This raises the question of the difference in time required for bone plug-tunnel integration between the conventional technique and our approach. Clancy et al. [6] found that the bone plug and a round bone tunnel established histological fixation at 8 weeks postoperatively in rhesus monkey. Among clinical studies, Lomasney used CT images to show fixation in 28.6% of cases at 8 weeks postoperatively after conventional surgery with a bone-patellar tendon-bone graft and a round bone tunnel [14]. The value of MDCT and MPR images for evaluation of bone fracture and bone integration after bone graft has been reported [2, 12, 18, 30], and imaging analysis is useful for clinical evaluation of bone integration postoperatively [14]. However, evaluation of bone plug integration after ACL reconstruction is uncommon since (1) analysis of the integration of a small bone plug with the femoral cancellous bone is much more difficult than for diaphyseal fracture healing and (2) evaluation is difficult since the surplus space between the bone plug and the tunnel is large and it takes a long time to fill the gap [7]. In this study, we used 30 slices in a plane parallel to an arbitrary long axis of the bone graft and the tunnel (a plane vertical to the anterior plane) in MPR images collected by MDCT [2, 12] at two postoperative time points [14]. A region of interest was established in the anterior surface of the evaluated site to detect slight changes; patterns of changes in CT values for the bone graft, bone tunnel and the surrounding area were observed, and the data were evaluated based on the difference in CT values at the boundary. This approach allowed the first detailed analysis of bone plug-tunnel integration after ACL reconstruction.
There are two types of healing processes for a bone plug with the tunnel [4, 5, 17]. In indirect healing, granulation tissue is generated between bone segments, callus develops, the gap between the bone segments increases, and neonatal bone finally fills the gap [4, 5]. In contrast, direct healing proceeds without generation of callus at the boundary or bone absorption at the bone edge at the interface, with no gap forming in a stable mechanical environment [15]. Our morphological CT evaluation indicated that direct healing occurs after the surgical technique used in this study. The clear boundary present after a few postoperative days gradually became unclear over time with no bone absorption observed. The number of “complete” slices on CT at 8 weeks postoperatively was significantly higher than that after 4 weeks, and the number of “incomplete” slices significantly decreased after 8 weeks. This indicates that early biological fixation is likely with this technique. If a gap was made at the interface, a postoperative period of 8 weeks would be insufficient to fill the gap.
The changes in CT values appear to support the macroscopic evaluations [2]. Slight changes that cannot be detected macroscopically were detectable by quantification of changes in the CT value in the region of interest. In addition, these changes gave an intuitive understanding of the healing process of the bone plug [2, 28]. The surrounding area of the bone tunnel and the graft had a slightly higher CT value than the surrounding cancellous bone, which might be caused by dilation, and a peak CT value that was probably due to pressure applied anteriorly was observed in all cases. A dip was also observed just anterior to that point. The CT value of the cancellous bone showed a general decrease over time, probably due to osteoporotic changes caused by non-weight bearing postoperatively. This change in the CT value decreased over time based on the values at 0, 4, and 8 weeks. Thus, the normalized change in the CT value at the border may be a useful marker for monitoring direct healing of the plug [4, 5, 17].
There is some limitation in this study. We did not include a control group of subjects treated by conventional techniques, while earlier bone plug integration was shown by CT [12, 18]. Thus, we still have to be cautious to accelerate postoperative rehabilitation, as it is still unclear how earlier the graft itself is remodeled postoperatively by accelerated healing of the bone plug to the tunnel wall.
However, we believe earlier integration of the bone plug to the tunnel accelerates the graft healing itself. Surgeons should pay attention to minimize extra space between the graft and the tunnel or to maximize contact area between them by adjusting the cross-sectional shape of the femoral tunnel aperture to that of the bone plug.
Conclusion
Because a snug fit is achieved at the bone plug-femoral tunnel interface, this method is beneficial for graft-bone integration in early postoperative stage after RT BTB ACL reconstruction.
In this technique of RT BTB ACL reconstruction, the bone plug integrated with the femoral tunnel in 55% of cases as early as 4 weeks postoperatively and in 80% of cases by 8 weeks postoperatively.
References
Arnold MP, Kooloos J, van Kampen A (2001) Single-incision technique misses the anatomical femoral anterior cruciate ligament insertion: a cadaver study. Knee Surg Sports Traumatol Arthrosc 9:194–199
Boer FC, Bramer JAM, Haarman HJTM (1998) Quantification of fracture healing with three-dimensional computed tomography. Arch Orthop Trauma Surg 117:345–350
Brand J Jr, Weiler A, Johnson DL (2000) Graft fixation in cruciate ligament reconstruction. Am J Sports Med 28:761–774
Claes L, Augat P, Wilke HJ (1997) Influence of size and stability of the osteotomy gap on the success of fracture healing. J Orthop Res 15:577–584
Claes LE, Heigele CA (1999) Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech 32:255–266
Clancy WG, Narechania RG, Lange TA (1981) Anterior and posterior cruciate ligament reconstruction in rhesus. J Bone Joint Surg Am 63:1270–1284
Drogset JO, Grøntvedt T, Myhr G (2006) Magnetic resonance imaging analysis of bioabsorbable interference screws used for fixation of bone–patellar tendon–bone autografts in endoscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 34:1164–1169
Feretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23:1218–1225
Fink C, Benedetto KP, Hackl W, Hoser C, Freund MC, Rieger M (2000) Bioabsorbable polygluconate interference screw fixation in anterior cruciate ligament reconstruction: A prospective computed tomography-controlled study. Arthroscopy 16:491–498
Hoher J, Livesay GA, Woo SL (1999) Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 7:215–219
Hutchinson MR, Ash SA (2003) Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy 19:931–935
Krestan CR, Noske H, Czerny C (2006) MDCT versus digital radiography in the evaluation of bone healing in orthopedic patients. Am J Roentgenol 186:1754–1760
Kurosaka M, Yoshiya S, Andrish JT (1987) A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 15:225–229
Lomasney LM, Tonino PM, Coan MR (2006) Evaluation of bone incorporation of patellar tendon autografts and allografts for ACL reconstruction using CT. Orthopedics 30:152–157
Malkolf KL, Burchfield DM, Shapiro MM, Davis BR, Finerman GAM, Slauterbeck JL (1996) Biomechanical consequences of replacement of the anterior cruciate ligament with patellar ligament allograft. Part 1: insertion of the graft and anterior-posterior testing. J Bone Joint Surg Am 78:1720–1727
Pavlik A, Hidas P, Berkes I (2006) Femoral press-fit fixation technique in anterior cruciate ligament reconstruction using bone–patellar tendon–bone graft: a prospective clinical evaluation of 285 patients. Am J Sports Med 34:220
Rahn BA, Gallinaro P, Perren SM (1971) Primary bone healing: an experimental study in the rabbit. J Bone Joint Surg Am 53:783–786
Reynolds DG, Hock C, Awad HA (2007) Micro-computed tomography prediction of biomechanical strength in murine structural bone grafts. J Biomech 40:3178–3186
Rupp S, Krauss PW, Fritsch EW (1997) Fixation strength of a biodegradable interference screw and a press-fit technique in anterior cruciate ligament reconstruction with a BPTB graft. Arthroscopy 13:61–65
Segawa H, Koga Y, Omori G, Sakamoto M, Hara T (2005) Contact pressure in anterior cruciate ligament bone tunnels: comparison of endoscopic and two-incision technique. Arthroscopy 21:439–444
Shapiro JD, Jackson DW, Aberman HM et al (1995) Comparison of pullout strength for seven- and nine-millimeter diameter interference screw size as used in anterior cruciate ligament reconstruction. Arthroscopy 11:596–599
Shino K, Kimura T, Ono K (1986) Reconstruction of the anterior cruciate ligament by allogeneic tendon graft an operation for chronic ligamentous insufficiency. J Bone Joint Surg Br 68:739–746
Shino K, Mae T, Maeda A, Miyama T, Shinjo H, Kawakami H (2002) Graft fixation under predetermined tension using a new device—double spike plate. Arthroscopy 18:908–911
Shino K, Nakata K, Nakamura N, Mae T et al (2005) Anatomical ACL reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop 15:130–134
Shino K, Nakata K, Nakamura N et al. (2005) Anatomically oriented anterior cruciate ligament reconstruction with a bone–patellar tendon–bone graft via rectangular socket and tunnel: a snug-fit and impingement-free grafting technique. Arthroscopy 21:1402.e1–1402.e5
Shino K, Nakata K, Nakamura N, Suzuki T (2008) Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft to mimic natural fiber arrangement. Arthroscopy 24:1178–1183
Shino K, Suzuki T, Nakagawa S (2010) The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1164–1168
Walton M (1999) Absorbable and metal interference screws: comparison of graft security during healing. Arthroscopy 15:818–826
Woo SL, Kanamori A, Zeminski J, Yagi M, Papageorgiou C, Fu FH (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. J Bone Joint Surg Am 84:907–914
Wright JM, Pellicci PM, Roberts MM, Koh JL et al (2001) Bone density adjacent to press-fit acetabular components: a prospective analysis with quantitative computed tomography. J Bone Joint Surg Am 83:529–536
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, T., Shino, K., Nakagawa, S. et al. Early integration of a bone plug in the femoral tunnel in rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: a prospective computed tomography analysis. Knee Surg Sports Traumatol Arthrosc 19 (Suppl 1), 29–35 (2011). https://doi.org/10.1007/s00167-011-1481-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1481-5