Abstract
Septic shock remains a global health challenge with millions of cases every year, high rates of mortality and morbidity, impaired quality of life among survivors and relatives, and high resource use both in developed and developing nations. Care and outcomes are improving through organisational initiatives and updated clinical practice guidelines based on clinical research mainly carried out by large collaborative networks. This progress is likely to continue through the collaborative work of the established and merging trials groups in many parts of the world and through refined trial methodology and translational work. In this review, international experts summarize the current position of clinical research in septic shock and propose a research agenda to advance this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis has been extensively researched over the last 50 years. We can better define the host immune response to infection and have made considerable progress in the provision of vital organ support. Today, many individuals with septic shock, who would previously have died, will survive a reflection of improved treatment of precipitating infections, better and safer organ support, less iatrogenic harm, and more co-ordinated and effective intensive care medicine. However, we still lack specific therapies to directly treat the dysregulated host response. All trials of interventions designed to manipulate the host’s immune response during sepsis have disappointed. The only therapy with initial encouraging results, activated protein C (APC) [1], was subsequently withdrawn due to neutral results in the confirmatory trial [2].
Important lessons can be learned from recent advances in the understanding and treatment of cancer. Targeted therapy is the result of a century of research in histological and anatomical classifications, understanding of global mechanisms of oncogenesis and anti-cancer immunity and, ultimately, the demonstration of highly specific immunological signatures. This has enabled the design of specific drugs and successful clinical trials. This process, only completed in a few cancer types and leading to approval of some very expensive new drugs, may serve as an example for sepsis research.
For more than 30 years, multiple editorials and reviews have emphasized that sepsis is a heterogeneous syndrome, depending on the infectious process (e.g., microorganism, focus and speed of evolution) and on the specific innate and adaptive immune response of an individual patient (Fig. 1). In hindsight, it was naive to believe that one drug would suit all cases, act on all the components of this complex phenomenon, and improve outcome for all patients.
It is now time to go back to the drawing board [3]. The classification of patients is still non-specific, even using the new definitions [4]. We thus need to better characterize the different types of sepsis by defining more homogeneous groups of patients, perhaps based on their biological profile rather than clinical criteria alone. Large epidemiological studies and classification analyses may help to identify classes of clinical phenotypes and genotypes that respond differently to therapies. We also need to develop and validate stratification tools that rapidly identify patients who will respond to a given intervention.
In this narrative review, invited by the editorial board of Intensive Care Medicine, we summarize the current position of the field of clinical research in sepsis and septic shock and propose a research agenda to advance this field.
What is the current standard of care for delivering the best possible sepsis care?
Arguably the most accepted international standard of care for the treatment of septic shock is the set of guidelines articulated by the Surviving Sepsis Campaign (SSC), the 2016 iteration of which has recently been published [5]. These guidelines emphasize the use of screening tools to allow early recognition of sepsis with prompt initiation of broad spectrum antimicrobial therapy guided by pharmacokinetic/pharmacodynamic principles, microbiological techniques aiming to identify the causative agents, and appropriate source control. All institutions should have strategies to promote awareness of sepsis-associated hypotension and severe hyperlactatemia as these are life-threatening conditions. Identification should be followed by appropriate fluid resuscitation using an empiric dose of 30 ml/kg of crystalloids over the first 3 h, while avoiding starches. Further fluid resuscitation should be guided by frequent reassessment of hemodynamic status using appropriate monitoring and evaluation of fluid responsiveness. Vasopressors should, in general, be initially titrated to a mean arterial pressure of 65 mmHg, with norepinephrine as the first-line therapy, and epinephrine and vasopressin as second-line agents. It is suggested that patients with severe hyperlactatemia receive hemodynamic optimization until lactate is normalized. Quality of care indicators include a second lactate sampling when the baseline is high, and re-assessment of fluid status and perfusion (http://www.survivingsepsis.org/Bundles/Pages/default.aspx).
Although these guidelines are based on the best available evidence as assessed by a group of experts, they are only rarely supported by high-quality evidence. Of the 93 statements in the 2016 iteration, only 7 are based on high-level evidence, 28 on moderate evidence, and 58 on low or very low evidence. Two interrelated questions arise when international standards are based on such paltry evidence. First, will the low evidence, and accompanying uncertainty, lead to physician disagreement and poor uptake of the guidelines? Second, if the guidelines are applied, will they improve outcomes accepting that the individual elements may not in fact work? Together, these issues underpin the larger question of whether we should promote and use guidelines at all.
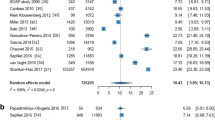
Increasing standardization, even in the absence of known efficacy, has the advantage of promoting reliability. This may facilitate quicker learning about good versus bad processes, simply because random noise is reduced (Fig. 2). The underlying principle of seeking to reduce variation in care has some rationale. Quality improvement initiatives based on SSC bundles have been associated with a reduction in sepsis mortality [6], even though the components of the bundle were not demonstrated to lower mortality in randomized trials. However, compliance is rarely high for any component of the bundle, and there is concern that forcing uniform management based on weak evidence may inadvertently cause harm. As such, one should be careful when converting guidelines into mandates [7].
The contribution of trial results (positive, negative or neutral) to the continued evolvement of clinical practice and new research questions to be tested in new trials (dark blue circles). In this process, explorative analyses of trial results, the harmonization of care and increased utilization of enrichment through improved geno- and phenotyping and novel trial designs (light blue circles) will all contribute to the conduct of better, more effective and more efficient trials
In addition, compliance with resuscitation measures in the 3- and 6-h SSC bundles is highly variable across studies [8,9,10,11], suggesting they are not standards of care across all settings or that the guidelines are in fact difficult to follow and comply with even in excellent centres. A multinational 1-day prevalence study also showed low compliance rates with all resuscitation items, including lactate sampling (56%), repeat lactate sampling (64%), administering 30 mL/kg of crystalloids for fluid resuscitation (57%), and vasopressors for hypotension (66%) [10].
Other factors that decrease compliance with resuscitation guidelines include low awareness among healthcare workers, healthcare workforce shortages, overcrowding of emergency departments [11], and unfavorable nurse-to-patient ratios [12]. Low availability of resources can also limit the application of some interventions. For example, tools to assess fluid responsiveness may be unavailable in many low- and middle-income settings. Available strategies to improve implementation are continuous education programs, the use of multidisciplinary teams, reminders, checklists, and mechanisms of audit and feedback [13].
The best standard of care will be achieved by a balance between the best available evidence, identification of the population to which the recommendation may not apply and cause harm, and a capacity for well-trained and experienced physicians to weigh the balance between potential benefits and harms for a specific patient, given individual circumstances and the strength of the evidence.
Major recent advances in septic shock
Positive impact of negative trials
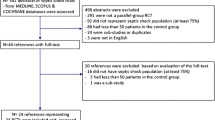
A popular critique of contemporary trials in critical care has been that these trials are mostly ‘negative’, in they have neither brought us new treatments nor shown those that can save lives. However, these so-called ‘negative’ trials have nonetheless generated considerable new knowledge, leading to both scientific advances and important changes in clinical practice [14, 15]. That said, individual trials continue to be under-powered to detect small but clinically important effects [16]. It is even more crucial to consider the comprehensive body of evidence to answer research questions. For example, it was the cumulative contribution of 31 trials, conducted between 1982 and 2012, that established the harm associated with hydroxyethyl starch (HES) [17].
Analyses of so-called ‘negative’ studies have informed practice in three ways. First, high-quality comparative effectiveness trials that do not report a statistically significant treatment effect in favor of the intervention can provide a strong rationale to guide restriction or withdrawal of ineffective or dangerous interventions (Fig. 2). This is exemplified by the HES and tight glycemic control trials that showed harm from the interventions. Second, ‘negative’ trials may identify important subgroup effects that support more individualized care to a heterogeneous patient population [18]. Third, they may reveal which factors are important in multifaceted interventions. The results of the original Early Goal-Directed Therapy (EGDT) trial [19] were not reproduced by three concurrent large clinical trials [20,21,22]. The pre-randomization resuscitation delivered to patients in these recent trials points to an evolution in usual care and suggests that clinician awareness and processes of care (i.e. prompt recognition and reaction to acute threats), rather than the specific aspects of resuscitation protocols, improve outcomes.
Large international collaborations
The need for adequate statistical power to demonstrate clinically relevant reductions in effect sizes, and the challenges imposed by heterogeneous patient populations, increase the already substantive direct and indirect costs of research. The establishment of successful research collaborations has provided exemplary high-quality trials. The emerging trend of other international research collaborations, particularly in middle-income countries, is also encouraging. From the perspective of research-funding agencies, these collaborations provide an efficient means of answering important clinical questions at a fraction of the usual cost. Trials of EGDT-directed resuscitation were designed to facilitate their harmonization in an individual patient data meta-analysis [23, 24]. This has further informed best practices and provided the power to explore important subgroup analyses. Answering the important questions in critical care research will hinge on such joint international efforts.
Less is more
A constant theme from research reported in recent years has been that less is often more. It is justified to challenge our prior beliefs about the risk–benefit balance of even the most standard critical care interventions. While potentially not applicable to septic shock in resource-rich environments, the increased mortality observed with fluid boluses in African children with severe febrile illnesses [25] is triggering a reassessment of the safety and overall effectiveness of aggressive fluid resuscitation beyond surrogate outcomes such as urine output and blood pressure. New data from Scandinavia in adults with septic shock support these observations [26]. More aggressive oxygen therapy may also be associated with increased mortality [27]. These findings require confirmation, but are consistent with the experiences and subsequent trials in blood transfusion, glycemic control, mechanical ventilation and sedation practices. Our patients are highly vulnerable to iatrogenic complications; there is an equal imperative that we systematically seek the lowest effective dose for any intervention.
Patient/family involvement
As ICU populations are becoming older and frailer [28], reducing short-term mortality may not translate into significant gains in quality-adjusted life-years. About 35% of patients are readmitted to hospital within 6 months, rising to 60% within the first year after ICU admission for sepsis [29, 30]. Cohort studies have confirmed that specific patient populations, particularly older patients who receive prolonged ICU care, experience an increased burden of chronic physical and psychological disabilities [31]. The toll of long-term ICU care sequelae on relatives is also increasingly recognized [32]. Despite expert recommendations to consider non-mortal outcomes in certain patient populations, most septic shock research continues to focus on short-term survival. Determined patient stakeholders have requested a more active role in critical care research [33], and system-level changes are taking place as a result of their engagement [34]. If septic shock research embraces these initiatives, increasing emphasis on patient-centered research may prove to be a significant advance in the field.
What are the commonly held beliefs that have been contradicted by recent trials in septic shock?
For the management of septic shock, several beliefs have been contradicted and guideline recommendations changed or challenged following the publication of RCTs and systematic reviews with a lower risk of bias. These changes represent progress within the field that should prompt caution among clinicians, guideline committee members and policy-makers, especially when assessing results of trials with high-risk of bias and low levels of external validity.
Early goal-directed therapy (EGDT) for patients with septic shock
The resuscitation bundles by the SSC guidelines were based on the concept of EGDT produced by the results of a small, single-centered, unblinded trial [19]. These characteristics may have overestimated the effect of EGDT [35,36,37]. This prompted the conduct of three RCTs and a systematic review, all having a lower risk of bias and greater real-world generalizability [20,21,22, 24, 38]. Together, these trials, alone and in combination, demonstrated no effect on mortality [24, 38].
Activated protein C for patients with septic shock and high risk of death
The use of APC was recommended in the first iteration of the SSC guidelines following the publication of an RCT (PROWESS) reporting reduced mortality in patients with sepsis with the use of APC [1]. A subsequent confirmatory RCT (PROWESS Shock), which was requested by medical regulatory authorities [39], reported no reduction in mortality in patients with septic shock [2], resulting in the withdrawal of APC from the market.
Hydroxyethyl starches in patients with septic shock
For decades, HES solutions were used in the fluid management of patients with sepsis based on numerous industry-driven studies including some that was subsequently found to be fraudulent. When investigator-initiated RCTs with low risk of bias were conducted marked side effects and increased mortality were observed [40,41,42]. These studies have resulted in substantive changes to medical regulatory authorizations and guidelines that either prohibit or restrict the use of HES [5, 43].
Blood transfusion in patients with septic shock
The SSC guidelines have recommended a time- and biomarker-dependent protocol for blood transfusion based on the results of the initial EGDT trial [19] and on indirect evidence from a multicentre RCT (TRICC) in ICU patients [44]. A large high-quality confirmatory RCT showed no differences by time- and biomarker-independent blood transfusion at hemoglobin values of 7 versus 9 g/dl on patient-centered outcomes in patients with septic shock [45, 46].
These examples support the meta-epidemiological data indicating that results from RCTs with higher versus lower risk of bias overestimate intervention effects [35,36,37, 47, 48]. Similarly, observational studies are likely to overestimate intervention effects independent of the method of adjustment [49]. These effects may be amplified in septic shock trials where multiple, time-dependent exposures, competing risks and co-interventions are difficult to adjust for and thus will further hamper correct interpretation. The imperative for clinician researchers is to test as many as possible of the interventions, both current and novel, in large, multicenter RCTs with the lowest possible risk of bias.
What are remaining areas of uncertainties?
Look at those SSC Guideline recommendations based on low-quality evidence
The SSC Guidelines [50] use the GRADE approach to generate recommendations for clinical care [51]. While there are improvements in the 2016 iteration of the guidelines [5], few recommendations are based on high-quality evidence; in many areas, uncertainties remain.
Antibiotics
The 3- and 6-h resuscitation bundles focused on antibiotic therapy, fluid resuscitation and blood pressure targets (http://www.survivingsepsis.org/Bundles/Pages/default.aspx). The evidence pertaining to optimal antibiotic therapy is weak despite these agents being the cornerstone of treating infection, the trigger for sepsis [4, 52]. There is little equipoise for delayed or no antibiotics, raising practical and ethical issues over any efforts to generate new evidence where patients may be randomized to less antibiotic coverage. Nevertheless, the evidence base that ‘every hour counts’, that combination therapy is beneficial, and that long courses of therapy are needed to better eradicate microorganisms is weak and conflicting (e.g., [53, 54]). Emerging data suggest harm from antibiotic load, whether from longer courses and/or multiple agents. Studies of antimicrobial therapies seldom report mortality differences between patients treated with appropriate and inappropriate antibiotics, and also differ in how ‘appropriate’ is defined [55]. Even if the microorganism is susceptible, we are generally unaware whether or not the patient is receiving an adequate dose. Other than aminoglycosides and vancomycin, antibiotic dosing is seldom monitored. There is, therefore, great uncertainty whether individual patients are being under- or over-dosed with standard regimens, especially as drug excretion, metabolism, volumes of distribution, protein binding and augmented renal clearance will vary markedly in sepsis both temporally within patients and between patients [56, 57]. We are also uncertain whether monitoring of blood levels is appropriate to ensure adequate concentrations in the affected area (e.g., consolidated lung or soiled peritoneal cavity), and whether the minimal inhibitory concentration measured in vitro is applicable to in vivo cure or failure rates [58]. In the context of an increasing incidence of sepsis [59, 60] and fast-emerging antibiotic resistance [61], this weak evidence base is disappointing and arguably unacceptable. We must rapidly determine how to prescribe antibiotics optimally for both efficacy and safety [62].
Resuscitation
The ‘6-h resuscitation bundle’—based upon the original EGDT [19] targets—has also been shown to offer no advantage over standard of care [24, 38]. Surely we must re-evaluate the benefit of recommending rigid physiological targets in a heterogeneous population where one size cannot possibly fit all? This clearly applies to the volume needed to achieve ‘adequate’ fluid resuscitation, and the criteria upon which ‘adequate’ is determined. This is relevant in the light of a recent feasibility trial testing a more restrictive resuscitation strategy [26]. Similarly, the blood pressure target sufficient to achieve an adequate but not excessive organ perfusion pressure is likely to vary between individuals. Randomizing septic shock patients to two fairly fixed blood pressure targets failed to demonstrate overall improvements in outcome [63]; it may be that better pheno- or genotyping could stratify patients to the optimal blood pressure target?
New definitions and trigger tools
The new sepsis definitions [4, 52] have explicitly proposed criteria for sepsis and septic shock. Re-analyses of two existing trial databases have provided differing results regarding the potential interaction of the new definition and the intervention effect [64, 65]. We therefore need more such analyses to better estimate the potential of the new sepsis definitions to change the intervention effect estimates observed in previous trials. In addition, the new criteria include a simple physiology-based score to identify those patients with suspected infection at risk of bad outcomes [66]. Several track and trigger tools exist but differ in their performance and feasibility of implementation [67]. Determining the best tool to detect the at-risk patient with optimal sensitivity and specificity is key.
Mediator modulation
The SSC had previously abandoned the ‘24-h resuscitation bundle’ [50] as three (activated protein C, corticosteroids for shock, tight glycemic control) of the four components were shown in subsequent multicenter trials to confer no benefit. Similarly, other immunomodulatory drugs such as intravenous immunoglobulins have been discarded based on lack of overall outcome effect [68]. We should re-evaluate such treatment ‘failures’ by using predictive or prognostic enrichment [69]. Treatment-responsive sub-phenotypes have been suggested for ARDS [70] and sepsis [71], and these need to be explored further. We need to identify patients in whom therapies should be avoided. Immunosuppressive agents (such as steroids) should be withheld in patients found to be immunosuppressed, whereas immune-stimulatory agents (e.g., GM-CSF, IFN-gamma, or PD-1 inhibitors) would likely further aggravate a cytokine storm if given when a strong pro-inflammatory phenotype is being expressed [72].
Trial design
We also need to be smarter in other aspects of trial design (Fig. 3). Many studies have been unrealistically powered to suit funding or time limitations; type II error is thus a concern. With the advent of ‘big data’ [73], we should be able to better characterize patients for study inclusion and exclusion, and to target more appropriate study endpoints instead of mortality, or to consider mortality with persisting organ failure [74]. However, choosing composite and/or non-mortality endpoints is complex [75]; improving a non-mortality endpoint may not necessarily translate into a survival benefit. Adaptive trial design can also increase trial efficiency by facilitating earlier discard of ineffective interventions or doses of drugs.
Enrichment and biomarker stratified designs. Enrichment designs could be either predictive enrichment or prognostic enrichment or combination of both [102]. Predictive enrichment refers to enriching patients based on greater likelihood of treatment response irrespective of illness severity (a). Prognostic enrichment identifies a patient population at high risk of outcome event and randomize them for interventions (b). Treatment response marker(s) negative population in predictive enrichment design, and the low risk of outcome population in prognostic enrichment design, are excluded from the trial. If a significant average treatment effect is observed, it recommended only for the tested population. Treatment response marker(s) stratified design randomizes both positive and negative population (c). Analyses are conducted in two stages. First, the treatment response marker(s) positive population is tested for difference in outcomes. If there is a difference in average treatment effect in the treatment response marker(s) positive population, then a second set of analyses are conducted. This could be carried out either in the treatment response marker(s) negative population or to the whole population to generate treatment recommendations
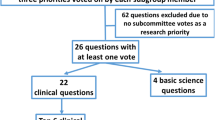
What are the top 10 topics to undergo clinical testing in septic shock in the next 10 years?
These range from those trials ready to be conducted now to more speculative programs for later study in the next decade. There are many other research questions to be answered, in particular in less resourced settings, but it is beyond the scope of the present paper to cover all of these.
Restrictive versus liberal fluid resuscitation
Although fluid therapy is a fundamental component of resuscitation, there is increasing evidence that excess fluid may be harmful [25, 76]. However, as this evidence comes from retrospective studies or different clinical settings, we need direct evidence from RCTs performed in the different phases of septic shock. A recent pilot trial demonstrated that a restrictive versus liberal fluid strategy trial is feasible after initial management of septic shock [26]. Similar trials of the fluid management of the post-resuscitation phase of septic shock are needed to complement existing evidence [77].
Rapid microbiology diagnostic and antibiotic measuring devices to guide therapy
Early appropriate antibiotic therapy in severely ill patients is critical for successful sepsis management. However, in less severely ill patients when the diagnosis of infection is less clear, there is evidence that waiting for positive microbiology results may be appropriate [78]. As antibiotic resistance rates continue to rise, avoiding unnecessary antibiotic use and optimizing the dosing of those used are high priorities. There are now several RCTs evaluating in different subsets of potentially infected patients whether procalcitonin, a marker of host response to infection, could be incorporated into antibiotic prescribing guidelines. Novel technology now allows a vast array of rapid assays of both microbial products and host response to infection as well as assessment of antibiotic pharmacokinetics and pharmacogenomics. We welcome the evaluation of these novel diagnostics in trial designs similar to those used to evaluate procalcitonin to help guide initiation, selection, dosing and duration of antibiotics.
Reducing catecholamine use in septic shock
The potentially favorable effects of reduced vasopressor dosing [79], adjunctive vasopressin [80, 81] or angiotensin-II [82], and/or beta-blocker(s) [83] support the notion that excess catecholamines be limited or avoided in septic shock. There is an imperative to conduct trials with low risk of bias to assess the effectiveness and safety of strategies aiming at reducing the effects of catecholamines in septic shock. These include lowering doses of noradrenaline and adjunctive vasopressin analogues, angiotensin-II and/or beta-blocking agents. For these strategies to be effective, more work should be carried out on the target populations; some patients may be harmed by broad application of these interventions to unselected populations. Such work should also include pharmacogenomic studies, as there are functional polymorphisms of both alpha and beta adrenoreceptor genes that affect vascular reactivity, response to catecholamines, and risk of sudden death [84, 85]. These and other polymorphisms in vasopressor pathway genes may be associated with vasopressor treatment response, serious adverse events and mortality [86].
Counteracting endocrine, metabolic and bioenergetic failure
The ADRENAL trial on hydrocortisone versus placebo will provide important information about the use of steroids in the total population of septic shock [87]. However, trials of steroids in potentially treatment-responsive subgroups [88] are also required. Potential interactions with vitamin C and thiamine need further investigation [89]. There is a general shift in energy substrate towards fat metabolism in sepsis; whether this is beneficial or should be modulated by, for instance, ultra-high-dose insulin or ketones warrants study. Mitochondrial dysfunction is well recognized in human sepsis [90] as well as multiple animal models. Bioenergetic failure is increasingly recognized as an important etiology of immune dysfunction. Protecting mitochondria (e.g., with targeted antioxidants [91]) or stimulating mitochondrial biogenesis [92] with regeneration of new, functioning mitochondria are strategies that may prove efficacious.
Stem cell therapies
Past attempts to modulate the immune response have been unsuccessful, perhaps because of the multiple redundant pathways in multiple cell types that are activated in any individual septic patient. Mesenchymal stromal stem cells target multiple pathways, interact with multiple cell types, and may be appropriately responsive to the inflammatory environment. Experimental and early clinical studies show promising results and now need to be tested in larger RCTs [93].
Biomarker-guided trials
Attempts to inhibit the systemic inflammatory response in sepsis have failed to reduce mortality and, in some cases, increased mortality [94]. Although the inflammatory response has important protective effects, an anti-inflammatory intervention likely only works if there is excessive inflammation. Initial attempts to target the most severely inflamed patients using a general marker of inflammation failed to improve outcomes [95]. Future RCTs that use specific predictive biomarkers [88] and pharmacogenomic biomarkers of response to drug(s) that are the target for the intervention, should be used to select patients for inclusion in many future trials.
Novel anti-inflammatory therapies
As detailed above, therapies targeting the host inflammatory response to sepsis have failed. An interesting alternative is to target the organism to reduce inflammation. Proprotein convertase subtilisin/kexin type-9 (PCSK9) inhibitors lower low-density lipoprotein (LDL) levels and may also increase clearance of pathogen lipids, such as LPS, transported in LDL [96]. This novel therapeutic strategy requires further basic and clinical trial investigations. As genetic PCSK9 variants affect PCSK9 function, a predictive pharmacogenetic strategy should be investigated in these trials.
Biomarker-guided immune stimulation trial
There is also an important anti-inflammatory host response in sepsis that may lead to secondary infection and poor outcomes. A recent study in patients with community-acquired pneumonia examining gene-expression profiles identified a subgroup of patients who had an immune-suppressed phenotype and higher mortality rate than patients without the immuno-suppression [97]. Such immuno-suppressed patients may benefit from treatment with immuno-stimulant therapies such as IL-7 (NCT02640807), anti-PDL1 and other immuno-stimulating interventions [98].
The use of machine learning algorithms/computer decision support systems
Growing use of electronic health records creates huge databases containing valuable information about demographics, altered pathophysiology and response to various treatments of sepsis. Machine-learning techniques embedded in clinical decision-support systems should be developed and tested to select “optimal” treatments in sepsis using data-driven models [99]. These offer the tantalising prospect of better precision-based decision making for the individual patient (characteristics and disease trajectories) to improve outcome.
Multi-arm, multi-stage trials of common sepsis therapies—“all in”
This review has highlighted several proposed trials of individual treatments in sepsis. Undoubtedly, there are other new therapies being developed. Furthermore, septic patients require multiple treatments in combination, and these interactions also require testing. Running separate RCTs for each therapy and each combination is a massive investment. The advent of long-term platform trials with multiple treatment arms and multiple stages, in which treatments may be dropped or added (optimally by using adaptive trial design), has provided multi-component successes within oncology [100]. Long-term platform trials should now be set up for sepsis [101] (Fig. 2).
References
Bernard GR, Vincent JL, Laterre PF et al (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709. doi:10.1056/NEJM200103083441001
Ranieri VM, Thompson BT, Barie PS et al (2012) Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med 366:2055–2064. doi:10.1056/NEJMoa1202290
Angus DC (2011) The search for effective therapy for sepsis: back to the drawing board? JAMA 306:2614–2615. doi:10.1001/jama.2011.1853
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:801–810. doi:10.1001/jama.2016.0287
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. doi:10.1007/s00134-017-4683-6
Levy MM, Rhodes A, Phillips GS et al (2014) Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med 40:1623–1633. doi:10.1007/s00134-014-3496-0
Aaronson EL, Filbin MR, Brown DFM et al (2016) New mandated centers for medicare and medicaid services requirements for sepsis reporting: caution from the field. J Emerg Med. doi:10.1016/j.jemermed.2016.08.009
Phua J, Koh Y, Du B et al (2011) Management of severe sepsis in patients admitted to Asian intensive care units: prospective cohort study. BMJ 342:d3245
Noritomi DT, Ranzani OT, Monteiro MB et al (2014) Implementation of a multifaceted sepsis education program in an emerging country setting: clinical outcomes and cost-effectiveness in a long-term follow-up study. Intensive Care Med 40:182–191. doi:10.1007/s00134-013-3131-5
Rhodes A, Phillips G, Beale R et al (2015) The Surviving Sepsis Campaign bundles and outcome: results from the International Multicentre Prevalence Study on Sepsis (the IMPreSS study). Intensive Care Med 41:1620–1628. doi:10.1007/s00134-015-3906-y
Shin TG, Jo IJ, Choi DJ et al (2013) The adverse effect of emergency department crowding on compliance with the resuscitation bundle in the management of severe sepsis and septic shock. Crit Care Lond Engl 17:R224. doi:10.1186/cc13047
Almeida M, Ribeiro O, Aragão I et al (2013) Differences in compliance with Surviving Sepsis Campaign recommendations according to hospital entrance time: day versus night. Crit Care Lond Engl 17:R79. doi:10.1186/cc12689
Borgert MJ, Goossens A, Dongelmans DA (2015) What are effective strategies for the implementation of care bundles on ICUs: a systematic review. Implement Sci IS 10:119. doi:10.1186/s13012-015-0306-1
Pocock SJ, Stone GW (2016) The primary outcome is positive—is that good enough? N Engl J Med 375:971–979. doi:10.1056/NEJMra1601511
Pocock SJ, Stone GW (2016) The primary outcome fails—what next? N Engl J Med 375:861–870. doi:10.1056/NEJMra1510064
Harhay MO, Wagner J, Ratcliffe SJ et al (2014) Outcomes and statistical power in adult critical care randomized trials. Am J Respir Crit Care Med 189:1469–1478. doi:10.1164/rccm.201401-0056CP
Zarychanski R, Abou-Setta AM, Turgeon AF et al (2013) Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 309:678–688. doi:10.1001/jama.2013.430
Iwashyna TJ, Burke JF, Sussman JB et al (2015) Implications of heterogeneity of treatment effect for reporting and analysis of randomized trials in critical care. Am J Respir Crit Care Med 192:1045–1051. doi:10.1164/rccm.201411-2125CP
Rivers E, Nguyen B, Havstad S et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377. doi:10.1056/NEJMoa010307
Investigators ProCESS, Yealy DM, Kellum JA et al (2014) A randomized trial of protocol-based care for early septic shock. N Engl J Med 370:1683–1693. doi:10.1056/NEJMoa1401602
Peake SL, ARISE Investigators, ANZICS Clinical Trials Group et al (2014) Goal-directed resuscitation for patients with early septic shock. N Engl J Med 371:1496–1506. doi:10.1056/NEJMoa1404380
Mouncey PR, Osborn TM, Power GS et al (2015) Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 372:1301–1311. doi:10.1056/NEJMoa1500896
ProCESS ARISE, Committee ProMISe Methodology Writing, Huang DT, Angus DC et al (2013) Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: methodology of ProCESS, ARISE, and ProMISe. Intensive Care Med 39:1760–1775. doi:10.1007/s00134-013-3024-7
PRISM Investigators (2017) Early, Goal-Directed Therapy for Septic Shock - A Patient-Level Meta-Analysis. N Engl J Med. doi:10.1056/NEJMoa1701380
Maitland K, Kiguli S, Opoka RO et al (2011) Mortality after fluid bolus in African children with severe infection. N Engl J Med 364:2483–2495. doi:10.1056/NEJMoa1101549
Hjortrup PB, Haase N, Bundgaard H et al (2016) Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med 42:1695–1705. doi:10.1007/s00134-016-4500-7
Girardis M, Busani S, Damiani E et al (2016) Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA 316:1583–1589. doi:10.1001/jama.2016.11993
Angus DC, Linde-Zwirble WT, Lidicker J et al (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Perner A, Haase N, Winkel P et al (2014) Long-term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer’s acetate. Intensive Care Med 40:927–934. doi:10.1007/s00134-014-3311-y
Mayr FB, Talisa VB, Balakumar V et al (2017) Proportion and cost of unplanned 30-day readmissions after sepsis compared with other medical conditions. JAMA 317:530–531. doi:10.1001/jama.2016.20468
Herridge MS, Chu LM, Matte A et al (2016) The RECOVER Program: disability risk groups and 1-year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med 194:831–844. doi:10.1164/rccm.201512-2343OC
Cameron JI, Wittenberg E, Prosser LA (2016) Caregivers and families of critically Ill patients. N Engl J Med 375:1000–1002. doi:10.1056/NEJMc1608225
Lamontagne F, Cohen D, Herridge M (2016) Understanding patient-centredness: contrasting expert versus patient perspectives on vasopressor therapy for shock. Intensive Care Med. doi:10.1007/s00134-016-4518-x
Selby JV, Forsythe L, Sox HC (2015) Stakeholder-driven comparative effectiveness research: an update from PCORI. JAMA 314:2235–2236. doi:10.1001/jama.2015.15139
Bafeta A, Dechartres A, Trinquart L et al (2012) Impact of single centre status on estimates of intervention effects in trials with continuous outcomes: meta-epidemiological study. BMJ 344:e813
Wiedermann CJ, Bellomo R, Perner A (2016) Is the literature inconclusive about the harm from HES? No. Intensive Care Med. doi:10.1007/s00134-016-4275-x
Landoni G, Comis M, Conte M et al (2015) Mortality in multicenter critical care trials: an analysis of interventions with a significant effect. Crit Care Med 43:1559–1568. doi:10.1097/CCM.0000000000000974
Angus DC, Barnato AE, Bell D et al (2015) A systematic review and meta-analysis of early goal-directed therapy for septic shock: the ARISE, ProCESS and ProMISe Investigators. Intensive Care Med 41:1549–1560. doi:10.1007/s00134-015-3822-1
Ranieri VM, Thompson BT, Finfer S et al (2011) Unblinding plan of PROWESS-SHOCK trial. Intensive Care Med 37:1384–1385. doi:10.1007/s00134-011-2272-7
Perner A, Haase N, Guttormsen AB et al (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134. doi:10.1056/NEJMoa1204242
Myburgh JA, Finfer S, Bellomo R et al (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911. doi:10.1056/NEJMoa1209759
Haase N, Wetterslev J, Winkel P, Perner A (2013) Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med 39:2126–2134. doi:10.1007/s00134-013-3111-9
Bion J, Bellomo R, Myburgh J et al (2014) Hydroxyethyl starch: putting patient safety first. Intensive Care Med 40:256–259. doi:10.1007/s00134-013-3167-6
Hébert PC, Wells G, Blajchman MA et al (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 340:409–417. doi:10.1056/NEJM199902113400601
Holst LB, Haase N, Wetterslev J et al (2014) Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med 371:1381–1391. doi:10.1056/NEJMoa1406617
Rygård SL, Holst LB, Wetterslev J et al (2016) Long-term outcomes in patients with septic shock transfused at a lower versus a higher haemoglobin threshold: the TRISS randomised, multicentre clinical trial. Intensive Care Med 42:1685–1694. doi:10.1007/s00134-016-4437-x
Lundh A, Sismondo S, Lexchin J, et al (2012) Industry sponsorship and research outcome. Cochrane Database Syst Rev 12: MR000033. doi: 10.1002/14651858.MR000033.pub2
Savović J, Jones HE, Altman DG et al (2012) Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Ann Intern Med 157:429–438. doi:10.7326/0003-4819-157-6-201209180-00537
Ziff OJ, Lane DA, Samra M et al (2015) Safety and efficacy of digoxin: systematic review and meta-analysis of observational and controlled trial data. BMJ 351:h4451
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228. doi:10.1007/s00134-012-2769-8
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. doi:10.1136/bmj.39489.470347.AD
Shankar-Hari M, Phillips GS, Levy ML et al (2016) Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:775–787. doi:10.1001/jama.2016.0289
Sterling SA, Miller WR, Pryor J et al (2015) The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med 43:1907–1915. doi:10.1097/CCM.0000000000001142
de Groot B, Ansems A, Gerling DH et al (2015) The association between time to antibiotics and relevant clinical outcomes in emergency department patients with various stages of sepsis: a prospective multi-center study. Crit Care Lond Engl 19:194. doi:10.1186/s13054-015-0936-3
McGregor JC, Rich SE, Harris AD et al (2007) A systematic review of the methods used to assess the association between appropriate antibiotic therapy and mortality in bacteremic patients. Clin Infect Dis 45:329–337. doi:10.1086/519283
Eyler RF, Mueller BA, Medscape (2011) Antibiotic dosing in critically ill patients with acute kidney injury. Nat Rev Nephrol 7:226–235. doi:10.1038/nrneph.2011.12
Abdul-Aziz MH, Sulaiman H, Mat-Nor M-B et al (2016) Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med 42:1535–1545. doi:10.1007/s00134-015-4188-0
Roberts JA, Taccone FS, Lipman J (2016) Understanding PK/PD. Intensive Care Med 42:1797–1800. doi:10.1007/s00134-015-4032-6
Shankar-Hari M, Harrison DA, Rowan KM (2016) Differences in impact of definitional elements on mortality precludes international comparisons of sepsis epidemiology-A cohort study illustrating the need for standardized reporting. Crit Care Med 44:2223–2230. doi:10.1097/CCM.0000000000001876
Kaukonen K-M, Bailey M, Suzuki S et al (2014) Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA 311:1308–1316. doi:10.1001/jama.2014.2637
Spellberg B, Bartlett JG, Gilbert DN (2013) The future of antibiotics and resistance. N Engl J Med 368:299–302. doi:10.1056/NEJMp1215093
Perner A, Gordon AC, De Backer D et al (2016) Sepsis: frontiers in diagnosis, resuscitation and antibiotic therapy. Intensive Care Med 42:1958–1969. doi:10.1007/s00134-016-4577-z
Asfar P, Meziani F, Hamel J-F et al (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583–1593. doi:10.1056/NEJMoa1312173
Rygård SL, Holst LB, Wetterslev J et al (2017) Higher vs. lower haemoglobin threshold for transfusion in septic shock: subgroup analyses of the TRISS trial. Acta Anaesthesiol Scand 61:166–175. doi:10.1111/aas.12837
Russell JA, Lee T, Singer J et al (2017) The septic shock 3.0 definition and trials: a vasopressin and septic shock trial experience. Crit Care. doi:10.1097/CCM.0000000000002323
Seymour CW, Liu VX, Iwashyna TJ et al (2016) Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315:762–774. doi:10.1001/jama.2016.0288
Bhattacharjee P, Edelson DP, Churpek MM (2016) Identifying patients with sepsis on the hospital wards. Chest. doi:10.1016/j.chest.2016.06.020
Cohen J, Vincent J-L, Adhikari NKJ et al (2015) Sepsis: a roadmap for future research. Lancet Infect Dis 15:581–614. doi:10.1016/S1473-3099(15)70112-X
Prescott HC, Calfee CS, Thompson BT et al (2016) Toward smarter lumping and smarter splitting: rethinking strategies for sepsis and acute respiratory distress syndrome clinical trial design. Am J Respir Crit Care Med 194:147–155. doi:10.1164/rccm.201512-2544CP
Famous KR, Delucchi K, Ware LB et al (2016) ARDS subphenotypes respond differently to randomized fluid management strategy. Am J Respir Crit Care Med. doi:10.1164/rccm.201603-0645OC
Wong HR, Cvijanovich NZ, Anas N et al (2015) Developing a clinically feasible personalized medicine approach to pediatric septic shock. Am J Respir Crit Care Med 191:309–315. doi:10.1164/rccm.201410-1864OC
Hotchkiss RS, Sherwood ER (2015) Immunology. Getting sepsis therapy right. Science 347:1201–1202. doi:10.1126/science.aaa8334
Iwashyna TJ, Liu V (2014) What’s so different about big data?. A primer for clinicians trained to think epidemiologically. Ann Am Thorac Soc 11:1130–1135. doi:10.1513/AnnalsATS.201405-185AS
Heyland DK, Muscedere J, Drover J et al (2011) Persistent organ dysfunction plus death: a novel, composite outcome measure for critical care trials. Crit Care Lond Engl 15:R98. doi:10.1186/cc10110
Montori VM, Permanyer-Miralda G, Ferreira-González I et al (2005) Validity of composite end points in clinical trials. BMJ 330:594–596. doi:10.1136/bmj.330.7491.594
Boyd JH, Forbes J, Nakada T et al (2011) Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39:259–265. doi:10.1097/CCM.0b013e3181feeb15
Wiedemann HP, Wheeler AP, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network et al (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575. doi:10.1056/NEJMoa062200
Hranjec T, Rosenberger LH, Swenson B et al (2012) Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis 12:774–780. doi:10.1016/S1473-3099(12)70151-2
Lamontagne F, Meade MO, Hébert PC et al (2016) Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med 42:542–550. doi:10.1007/s00134-016-4237-3
Russell JA, Walley KR, Singer J et al (2008) Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 358:877–887. doi:10.1056/NEJMoa067373
Gordon AC, Mason AJ, Thirunavukkarasu N et al (2016) Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA 316:509–518. doi:10.1001/jama.2016.10485
Chawla LS, Busse L, Brasha-Mitchell E et al (2014) Intravenous angiotensin II for the treatment of high-output shock (ATHOS trial): a pilot study. Crit Care Lond Engl 18:534. doi:10.1186/s13054-014-0534-9
Morelli A, Ertmer C, Westphal M et al (2013) Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 310:1683–1691. doi:10.1001/jama.2013.278477
Dishy V, Sofowora GG, Xie HG et al (2001) The effect of common polymorphisms of the beta2-adrenergic receptor on agonist-mediated vascular desensitization. N Engl J Med 345:1030–1035. doi:10.1056/NEJMoa010819
Laukkanen JA, Mäkikallio TH, Kauhanen J, Kurl S (2009) Insertion/deletion polymorphism in alpha2-adrenergic receptor gene is a genetic risk factor for sudden cardiac death. Am Heart J 158:615–621. doi:10.1016/j.ahj.2009.07.023
Nakada T-A, Russell JA, Boyd JH et al (2010) beta2-Adrenergic receptor gene polymorphism is associated with mortality in septic shock. Am J Respir Crit Care Med 181:143–149. doi:10.1164/rccm.200903-0332OC
Venkatesh B, Myburgh J, Finfer S et al (2013) The ADRENAL study protocol: adjunctive corticosteroid treatment in critically ill patients with septic shock. Crit Care Resusc 15:83–88
Bentzer P, Fjell C, Walley KR et al (2016) Plasma cytokine levels predict response to corticosteroids in septic shock. Intensive Care Med 42:1970–1979. doi:10.1007/s00134-016-4338-z
Marik PE, Khangoora V, Rivera R et al (2016) Hydrocortisone, Vitamin C and Thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. doi:10.1016/j.chest.2016.11.036
Brealey D, Brand M, Hargreaves I et al (2002) Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 360:219–223. doi:10.1016/S0140-6736(02)09459-X
Lowes DA, Webster NR, Murphy MP, Galley HF (2013) Antioxidants that protect mitochondria reduce interleukin-6 and oxidative stress, improve mitochondrial function, and reduce biochemical markers of organ dysfunction in a rat model of acute sepsis. Br J Anaesth 110:472–480. doi:10.1093/bja/aes577
Lancel S, Hassoun SM, Favory R et al (2009) Carbon monoxide rescues mice from lethal sepsis by supporting mitochondrial energetic metabolism and activating mitochondrial biogenesis. J Pharmacol Exp Ther 329:641–648. doi:10.1124/jpet.108.148049
Walter J, Ware LB, Matthay MA (2014) Mesenchymal stem cells: mechanisms of potential therapeutic benefit in ARDS and sepsis. Lancet Respir Med 2:1016–1026. doi:10.1016/S2213-2600(14)70217-6
Fisher CJ, Agosti JM, Opal SM et al (1996) Treatment of septic shock with the tumor necrosis factor receptor: Fc fusion protein. The Soluble TNF Receptor Sepsis Study Group. N Engl J Med 334:1697–1702. doi:10.1056/NEJM199606273342603
Reinhart K, Menges T, Gardlund B et al (2001) Randomized, placebo-controlled trial of the anti-tumor necrosis factor antibody fragment afelimomab in hyperinflammatory response during severe sepsis: the RAMSES Study. Crit Care Med 29:765–769
Walley KR, Thain KR, Russell JA et al (2014) PCSK9 is a critical regulator of the innate immune response and septic shock outcome. Sci Transl Med 6:258ra143. doi:10.1126/scitranslmed.3008782
Davenport EE, Burnham KL, Radhakrishnan J et al (2016) Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Respir Med 4:259–271. doi:10.1016/S2213-2600(16)00046-1
Hotchkiss RS, Monneret G, Payen D (2013) Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach. Lancet Infect Dis 13:260–268. doi:10.1016/S1473-3099(13)70001-X
Tsoukalas A, Albertson T, Tagkopoulos I (2015) From data to optimal decision making: a data-driven, probabilistic machine learning approach to decision support for patients with sepsis. JMIR Med Inform 3:e11. doi:10.2196/medinform.3445
James ND, Sydes MR, Clarke NW et al (2016) Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 387:1163–1177. doi:10.1016/S0140-6736(15)01037-5
Angus DC (2015) Fusing randomized trials with big data: the key to self-learning health care systems? JAMA 314:767–768. doi:10.1001/jama.2015.7762
Shankar-Hari M, Rubenfeld GD (2017) The use of enrichment to reduce statistically indeterminate or negative trials in critical care. Anaesthesia 72:560–565. doi:10.1111/anae.13870
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
AP is member of the steering committee and national investigator of a vasopressin trial in septic shock sponsored by Ferring Pharmaceuticals; his department is reimbursed for his time. The department also receives research funding from Fresenius Kabi and CSL Behring. ACG has received speaker fees from Orion Pharmaceuticals and Amomed. He has consulted for Ferring Pharmaceuticals, Tenax Therapeutics, GlaxoSmithKline and received grant support from Orion Pharmaceuticals, Tenax Therapeutics and HCA International with funds paid to his institution. He is the Chief Investigator for two NIHR funded trials in septic shock: VANISH—examining vasopressin and LeoPARDS—examining levosimendan. He is supported by an NIHR Research Professorship award. DCA has received consulting fees from Abbott, Bayer, Beckman-Coulter, Biocartis, GenMark, GlaxoSmithKline, and Sobi for advice on sepsis trial design and is paid by Ferring for his participation on the Trial Steering Committee of the Sepsis-ACT multicenter trial of selepressin for septic shock. JMa is the chair of InFACT, a DSMB member for AK Pharma and a consultant for Regeneron Therapeutics and Bristol-Myers Squibb. JMy was the principal investigator of the CHEST trial; his institution, the George Institute for Global Health, has received unrestricted grant funding from Fresenius Kabi and Baxter Healthcare in relation to fluid resuscitation research; he is supported by a Practitioner Fellowship from the National Health and Medical Research Council of Australia. JR reports patents owned by the University of British Columbia (UBC) that are related to PCSK9 inhibitor(s) and sepsis and related to the use of vasopressin in septic shock. JR is an inventor on these patents. JR is a founder, Director and shareholder in Cyon Therapeutics Inc. (developing a sepsis therapy). Dr. Russell has share options in Leading Biosciences Inc. JR is a shareholder in Molecular You Corp. JR reports receiving consulting fees from Cubist Pharmaceuticals (now owned by Merck; formerly Trius Pharmaceuticals; developing antibiotics), Ferring Pharmaceuticals (manufactures vasopressin and is developing selepressin), Grifols (sells albumin), La Jolla Pharmaceuticals (developing angiotensin II; JR chairs the DSMB of a trial of angiotensin II), CytoVale Inc. (developing a sepsis diagnostic), and Asahi Kesai Pharmaceuticals of America (AKPA) (developing recombinant thrombomodulin). JR reports having received grant support from Ferring Pharmaceuticals that was provided to and administered by UBC. MSH acknowledges the support from National Institute for Health Research Clinician Scientist Award (CS-2016-16-011). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. MS is a co-investigator of the UK Department of Health-funded LeoPARDs trial (levosimendan in septic shock), the ADAPT trial (comparing biomarkers) and the STRESS-L trial (beta-blockade in septic shock). He is Clinical PI of a multicenter sepsis biomarker study conducted by the UK Ministry of Defence (DSTL), and a multiplex biomarker panel study with Mologic UK. He has grants from MedCity to develop an antibiotic monitoring with Probe Scientific, and the Wellcome Trust/UK Department of Health to investigate a novel tissue perfusion monitor with Oxford Optronix. He is also Co-PI of a sub-study of the EU Innovative Medicines Initiative Combacte-Magnet Program. He sits on advisory boards for Biotest, Bayer, Bristol Myers Squibb, Deltex and La Jolla Pharmaceuticals. He chaired the Data Safety and Monitoring Committee for InflaRx’s Phase II trial of a novel C5a inhibitor.
Rights and permissions
About this article
Cite this article
Perner, A., Gordon, A.C., Angus, D.C. et al. The intensive care medicine research agenda on septic shock. Intensive Care Med 43, 1294–1305 (2017). https://doi.org/10.1007/s00134-017-4821-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-4821-1