Abstract
Purpose
We assessed long-term mortality and hospitalisation in patients with severe sepsis resuscitated with hydroxyethyl starch (HES) or Ringer’s acetate.
Methods
This was an investigator-initiated, parallel-grouped, blinded randomised trial using computer-generated allocation sequence and centralised allocation data that included 804 patients with severe sepsis needing fluid resuscitation in 26 general intensive care units (ICUs) in Scandinavia. Patients were allocated to fluid resuscitation using either 6 % HES 130/0.42 or Ringer’s acetate during ICU admission. We assessed mortality rates at 6 months, 1 year and at the time of longest follow-up and days alive and out of hospital at 1 year.
Results
The vital status of all patients was obtained at a median of 22 (range 13–36) months after randomisation. Mortality rates in the HES versus Ringer’s groups at 6 months were 53.3 (212/398 patients) versus 47.5 % (190/400) [relative risk 1.12; 95 % confidence interval (CI) 0.98–1.29; P = 0.10], respectively; at 1 year, 56.0 (223/398) versus 51.5 % (206/400) (1.09; 95 % CI 0.96–1.24; P = 0.20), respectively; at the time of longest follow-up, 59.8 (238/398) versus 56.3 % (225/400) (1.06; 95 % CI 0.94–1.20; P = 0.31), respectively. Percentage of days alive and out of hospital at 1 year in the HES versus Ringer’s groups was 24 (0–87 days) versus 63 % (0–90) (P = 0.07).
Conclusions
The long-term mortality rates did not differ in patients with severe sepsis assigned to HES 130/0.42 versus Ringer’s acetate, but we could not reject a 24 % relative increased or a 4 % relative decreased mortality at 1 year with HES at the 95 % confidence level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravenous fluids are very frequently used in the treatment of patients with severe sepsis. Hydroxyethyl starch (HES) solutions have been used to obtain rapid and lasting circulatory stabilisation, but data from recent trials and meta-analyses bring into question their efficacy and safety in patients with sepsis [1–6]. HES has been shown to increase 90-day mortality in a randomised trial of patients with severe sepsis [3], and the harmful effect appears to be independent of the interventions given prior to randomisation, timing of the randomisation and circulatory impairment at the time of randomisation [7]. In critically ill patients HES has been shown to impair kidney function [1, 8, 9], increase the use of renal replacement therapy [1, 3–6, 10, 11], impair liver function [4] and to cause itching [4]. One possible explanation for these effects is that HES is taken up and stored in tissues, a process which is cumulative, widespread and long-lasting [12]. In addition, HES has been shown to directly impair coagulation [13], which may explain the increased rates of bleeding and transfusion observed in trials of critically ill patients [1, 3, 4, 14].
The updated Surviving Sepsis Campaign (SSC) guidelines recommend the use of crystalloids for the initial resuscitation of a patient and not to use HES based on outcome differences observed at day 90 in the above-mentioned trials [15]. However, parts of the critical care community have questioned the trial data on HES [16], and new data have been published adding to the debate on colloid versus crystalloid resuscitation in sepsis [17].
Importantly, there are no data describing the effects of HES versus crystalloid on long-term mortality. In study reported here, we conducted a protocolised long-term follow-up in the Scandinavian Starch for Severe Sepsis/Septic Shock (6S) trial [3, 18], in which patients with severe sepsis were randomised to fluid resuscitation using either HES 130/0.42 [molecular weight/substitution ratio (hydroxyethyl groups per glucose molecule)] or Ringer’s acetate.
Methods
The trial protocol was approved by the relevant ethic committees and medicines agencies. The protocol, the statistical analysis plan and the primary report have all been published [3, 18].
Trial design and conduct
The 6S trial was investigator-initiated, blinded (including patients, clinical and research staff and outcome assessors) and parallel-grouped using computer-generated allocation sequence and centralised concealed allocation. The latter was achieved using an interactive voice-response system at the Copenhagen Trial Unit (Copenhagen, Denmark), which was changed to web-based system at Expertmaker (Lund, Sweden) halfway through the trial because of technical difficulties with dial-in at some sites.
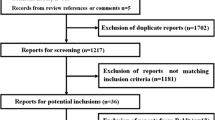
Patients were screened for enrolment between 23 December 2009 and 15 November 2011 in 26 general intensive care units (ICUs) in Scandinavia. Informed consent was obtained from the patient or a legal surrogate prior to enrolment. Enrolled patients were randomised 1:1 by clinicians or trial staff to fluid resuscitation with either HES 130/0.42 or Ringer’s acetate. Randomisation was stratified by the presence of shock, active haematological malignancy and inclusion in a University hospital as these characteristics may influence outcome [19, 20].
Trial patients
We screened patients aged 18 years or above who fulfilled the criteria for severe sepsis within the previous 24 h [21] and needed fluid resuscitation in the ICU as judged by the clinicians. The exclusion criteria and trial definitions are given in the Electronic Supplementary Material (ESM).
Intervention
Trial fluid [6 % HES 130/0.42 in Ringer’s acetate (6 % Tetraspan®, B Braun AG, Melsungen, Germany) or Ringer’s acetate (Sterofundin ISO®, B Braun)] was used when clinicians judged volume expansion to be needed in the ICU for a maximum of 90 days after randomisation. Trial fluids were masked using custom-made black, opaque, plastic bags, which were sealed by staff not involved in data registration or patient care. The maximum daily dose was 33 ml/kg ideal body weight; above this dose unmasked Ringer’s acetate was used for all patients. All other interventions were at the discretion of clinicians.
Long-term outcome measures
All-cause mortality at 6 months and 1 year after randomisation and at the time of longest follow-up were secondary outcome measures defined in the protocol and statistical analysis plan. These data were obtained from national registries using the unique national personal identification number of the patients. The final mortality follow-up of all patients was conducted in December 2012, 13 months after randomisation of the last patient. As the percentage of days alive and out of hospital at 90 days were lower in the HES versus the Ringer’s group [3], we did post hoc analyses of data on hospitalisation obtained from national registries using the personal identification numbers. In these registries all admissions to hospitals, including rehabilitation facilities, are linked to the personal identification numbers, so that all days in hospital can be assessed for each individual patient. Stays in nursing homes are not included. Days alive and out of hospital was calculated as the number of days spent out of hospital divided by the number of days alive in the 1-year period after randomisation for each individual patient and was expressed as a percentage.
Statistical analysis
All analyses were performed by the trial statistician (P.W.) according to the International Conference on Harmonisation-Good Clinical Practice guidelines E9 [22] and the statistical analysis plan in which the handling of missing data is also described. The analyses were done in the modified intention-to-treat population defined as all randomised patients (n = 804) except those who could be excluded post-randomisation without risk of bias [23] (n = 4; two were randomised without consent and we decided during the trial to exclude two other patients who were erroneously randomised and never received trial fluid) and those who withdrew consent for the use of data (n = 2). Ultimately, the data on 798 patients were used in the analyses.
Data were analysed by unadjusted chi-square testing for binary outcome measures and Wilcoxon’s rank for continuous measures. We used the log-rank-test to analyse time to death in the two intervention groups. We also compared 1-year mortality in the predefined subgroups (shock or acute kidney injury at time of randomisation) and conducted logistic regression analyses with adjustment for the following baseline variables: intervention group, the stratification variables (shock, active haematological malignancy and inclusion in a university hospital), age, diabetes, chronic kidney impairment, use of nephrotoxic drugs in hospital prior to randomisation, Simplified Acute Physiology Score (SAPS) II and Sepsis-related (=Sequential) Organ Failure Assessment (SOFA) scores [24, 25]. All analyses were done using SAS version 9.3 or SPSS version 17; P values (two-sided) of <0.05 were considered to be statistically significant.
Results
Characteristics at randomisation were comparable between the two groups, and none differed at the 5 % level of significance [3]. Vital status was obtained for all 798 patients in the modified intention-to-treat population [3] at a median of 22 (range 13–36) months after randomisation [in both the HES and Ringer’s groups, after 22 (13–36) months].
Long-term mortality
Six months after randomisation 212 of the 398 (53.3 %) patients in the HES group had died versus 190 of the 400 (47.5 %) in the Ringer’s group [relative risk (RR) 1.12; 95 % confidence interval (CI) 0.98–1.29; P = 0.10]. One year after randomisation 223 of the 398 (56.0 %) patients in the HES group had died versus 206 of the 400 (51.5 %) in the Ringer’s group (RR 1.09; 95 % CI 0.96–1.24; P = 0.20). At the time of the longest follow-up, 238 of the 398 (59.8 %) of the patients in the HES group had died versus 225 of the 400 (56.3 %) in the Ringer’s group (RR 1.06; 95 % CI 0.94–1.20; P = 0.31). Adjusting for potential risk factors at baseline did not noticeably change the point estimates for death [see Table 1 (analyses of the complete case dataset) and ESM Table S1 (analyses of the imputed dataset)]. The survival curves for the two intervention groups and 1-year mortality in the two predefined sub-groups are shown in Fig. 1.
Time to death and relative risks for 1-year mortality in the hydroxyethyl starch (HES) 130/0.42 and Ringer’s acetate groups, respectively. a Survival curves 1 year after randomisation for the two intervention groups in the modified intention-to-treat population. Kaplan–Meier analysis censored at 1 year showed that the survival time did not significantly differ between the two groups [intervention = HES: median survival 82 days, 95 % confidence interval (CI) 0–200 days; intervention = Ringer’s: median survival 328 days (no standard error, so 95 % CI cannot be calculated]. The P of the log rank test was 0.20; the reasoning for using log rank test is given in the ESM. b Relative risks with 95 % CI for 1-year mortality in the HES group compared with the Ringer’s acetate group in all patients and in the two pre-defined subgroups (shock defined as mean arterial pressure of <70 mmHg, ongoing treatment with vasopressor/inotropic agents or plasma lactate of >4.0 mmol/l in the hour prior to randomisation and acute kidney injury defined as renal Sepsis-related (=Sequential) Organ Failure Assessment score (SOFA) score of >2 [plasma creatinine of >170 µmol/l (1.92 mg/dl) or urinary output of <500 ml] in the 24 h prior to randomisation
Hospitalisation in the year after randomisation
At 1 year after randomisation, there were no differences between the intervention groups in terms of the numbers of days alive and out of hospital, in the number of patients being readmitted and in the length of hospitalisation (Table 2). More patients in the Ringer’s group than in the HES group appeared to be readmitted within 90 days (P = 0.03, Table 2).
Discussion
Here we report the long-term follow-up of an international, multicentre, randomised clinical trial in which HES 130/0.42 was compared with Ringer’s acetate for fluid resuscitation of patients with severe sepsis in terms of long-term mortality and hospitalisation. We did not find a statistically significant increased risk of death in the HES group at 6 months, 1 year or the longest follow-up. Comparable results were observed when potential risk factors were adjusted for and in the subgroups of patients with shock or acute kidney injury at randomisation. Also, the data on hospitalisation in the 1-year follow-up period were not markedly different between the two intervention groups.
Taken together we found a statistically significant increased mortality with HES at 90 days [3], but not 6 months or 1 year after randomisation. This result indicates that the harmful effects of HES occurred within the first months after randomisation. The reason for the lack of the difference in long-term mortality is unknown, but this was also observed in the long-term follow-up of the PROWESS trial on activated protein C [26]. It is likely that outcome in patients with severe sepsis is influenced by baseline co-morbidity [27], so that late deaths from causes other than sepsis and HES may have reduced the difference over time. On the other hand, the observed increased relative risk of the mortality rates with HES at 6 months, 1 year and at the time of the longest follow-up, even though not statistically significant, is in line with the pooled mortality estimate observed in the meta-analysis of trials with a low risk of bias on HES versus crystalloid/albumin in patients with sepsis (RR 1.11; 95 % CI 1.00–1.23) [5]. In contrast, the recently published data from the Colloids Versus Crystalloids for the Resuscitation of the Critically Ill (CRISTAL) trial suggested no short-term harm with colloid therapy, in this case mainly HES, and even an improved 90-day survival in ICU patients with septic shock [17]. Direct comparisons between the data of the two trials are difficult as the choice of both colloid and crystalloid solutions were made by clinicians in the CRISTAL trial. Also, the results of CRISTAL have a high risk of bias because the treatment was unblinded, allocation concealment was not 100 % ensured and marked baseline imbalance between the intervention groups was observed [28, 29]. In contrast, our trial had a low risk of bias in all domains and showed the opposite—that is, short-term harm from HES and no long-term benefits.
In our trial there appeared to be no major differences in hospitalisation data between the two groups, although the results should be interpreted with caution, as these analyses were planned post hoc. In addition, the trial was not powered to show differences in these endpoints. Taken together, the data indicate that the fewer days alive and out of hospital observed in the HES group at 90 days [3] and the lower point-estimate observed at 1 year were not due to more days spent in hospital but rather to the excess deaths which occurred between days 40 and 150 in this group. Significantly more patients in the Ringer group than in the HES group were readmitted within 90 days. The reason for this is unknown, but the higher number of 90-day survivors in the Ringer’s group may have contributed.
This is the first report on long-term mortality following resuscitation with HES. We have previously published data on health-related quality of life at 1 year in a post hoc analyses of the Danish survivors of the 6S trial [30]. In this population, patients in the HES group had a lower quality of life compared to that in the Ringer’s group. When all of the published outcome data from the 6S trial [3, 7, 14, 30] and the results of the meta-analysis of trials with a low risk of bias [5] are taken into account, it would appear unlikely that HES offers any benefit to patients with severe sepsis. On the contrary, the risk of harm is substantial.
The data on hospitalisation also reveal that there is a burden that severe sepsis inflicts on patients and society. The majority of the 1-year survivors were readmitted to hospital after the initial discharge, spending a total of 40 days in hospital with one-quarter of these spending more than 70 days in hospital in total. This may have contributed to the reduced quality of life observed in these patients [30]. In addition to the extra cost to society, there is also a financial burden on patients and families as a consequence of prolonged hospitalisation. Consequently, the full burden of severe sepsis is substantial.
The strengths of our trial include its high internal validity as the design ensured a low risk of bias in all domains [31]. In addition, the protocol and statistical analysis plan were published before the database was assessed, and we had 100 % follow-up of the modified intention-to-treat population. The latter was due to the use of national personal registration numbers, which enabled us to track patients in registries and include data from those patients who had transferred or been readmitted to other hospitals. We challenged the results in sub-group analyses and analyses adjusted for potential risk factors for death and found results comparable to the primary analyses. The external validity of the trial was presumably high because patients were recruited in many university and non-university hospitals in several countries, the majority of patients screened were included [3] and the protocol did not influence routine practice except for type of fluid used for resuscitation.
Our trial has a number of limitations. We did not protocolise haemodynamic monitoring or co-interventions. As the trial was relatively large and blinded and used stratified randomisation, it is less likely that imbalance in monitoring and concomitant interventions affected results. There were some protocol violations, but these were distributed equally between the two intervention groups, and the results of the per-protocol analyses supported those of the primary analyses presented in the original publication [3]. Also, the trial was not powered to show differences in mortality beyond day 90.
In conclusion, the mortality difference observed at 90 days between patients with severe sepsis who were resuscitated with either HES 130/0.42 or Ringer’s acetate diminished over time, so that the difference was no longer statistically significant at 6 months and 1 year after randomisation. This disappearance of the difference may be due to a lack of statistical power or that the harmful effects of HES only occurred within the first months after randomisation. In any case, our trial showed short-term harm from HES and no long-term benefits.
References
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, Forceville X, Feissel M, Hasselmann M, Heininger A, van Aken H (2012) Assessment of hemodynamic efficacy and safety of 6 % hydroxyethylstarch 130/0.4 vs. 0.9 % NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care 16:R94
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SA (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
Haase N, Perner A, Hennings LI, Siegemund M, Lauridsen B, Wetterslev M, Wetterslev J (2013) Hydroxyethyl starch 130/0.38-0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ 346:f839
Patel A, Waheed U, Brett SJ (2013) Randomised trials of 6 % tetrastarch (hydroxyethyl starch 130/0.4 or 0.42) for severe sepsis reporting mortality: systematic review and meta-analysis. Intensive Care Med 39:811–822
Müller RG, Haase N, Wetterslev J, Perner A (2013) Effects of hydroxyethyl starch in subgroups of patients with severe sepsis: exploratory post hoc analyses of a randomised trial. Intensive Care Med 39:1963–1971
Mutter TC, Ruth CA, Dart AB (2013) Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 7: CD007594
Citerio G, Bakker J, Bassetti M, Benoit D, Cecconi M, Curtis JR, Hernandez G, Herridge M, Jaber S, Joannidis M, Papazian L, Peters M, Singer P, Smith M, Soares M, Torres A, Vieillard-Baron A, Timsit JF, Azoulay E (2014) Year in review in Intensive Care Medicine 2013: I. acute kidney injury, ultrasound, hemodynamics, cardiac arrest, transfusion, neurocritical care, and nutrition. Intensive Care Med 40:147–159
Gattas DJ, Dan A, Myburgh J, Billot L, Lo S, Finfer S (2013) Fluid resuscitation with 6 % hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Med 39:558–568
Zarychanski R, Bou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, Fergusson DA (2013) Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 309:678–688
Wiedermann CJ, Joannidis M (2014) Accumulation of hydroxyethyl starch in human and animal tissues: a systematic review. Intensive Care Med 40:160–170
Hartog CS, Reuter D, Loesche W, Hofmann M, Reinhart K (2011) Influence of hydroxyethyl starch (HES) 130/0.4 on hemostasis as measured by viscoelastic device analysis: a systematic review. Intensive Care Med 37:1725–1737
Haase N, Wetterslev J, Winkel P, Perner A (2013) Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med 39:2126–2134
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Meybohm P, van Aken H, Gasperi AD, Hert SD, Rocca GD, Girbes AR, Gombotz H, Guidet B, Hasibeder W, Hollmann MW, Ince C, Jacob M, Kranke P, Kozek-Langenecker S, Loer SA, Martin C, Siegemund M, Wunder C, Zacharowski K (2013) Re-evaluating currently available data and suggestions for planning randomised controlled studies regarding the use of hydroxyethyl starch in critically ill patients—a multidisciplinary statement. Crit Care 17:R166
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declere AD, Preiser JC, Outin H, Troche G, Charpentier C, Trouillet JL, Kimmoun A, Forceville X, Darmon M, Lesur O, Regnier J, Abroug F, Berger P, Clec’h C, Cousson J, Thibault L, Chevret S (2013) Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA 310:1809–1817
Perner A, Haase N, Wetterslev J, Aneman A, Tenhunen J, Guttormsen AB, Klemenzson G, Pott F, Bodker KD, Badstolokken PM, Bendtsen A, Soe-Jensen P, Tousi H, Bestle M, Pawlowicz M, Winding R, Bulow HH, Kancir C, Steensen M, Nielsen J, Fogh B, Madsen KR, Larsen NH, Carlsson M, Wiis J, Petersen JA, Iversen S, Schoidt O, Leivdal S, Berezowicz P, Pettila V, Ruokonen E, Klepstad P, Karlsson S, Kaukonen M, Rutanen J, Karason S, Kjaeldgaard AL, Holst LB, Wernerman J (2011) Comparing the effect of hydroxyethyl starch 130/0.4 with balanced crystalloid solution on mortality and kidney failure in patients with severe sepsis (6S—Scandinavian Starch for Severe Sepsis/Septic Shock trial): study protocol, design and rationale for a double-blinded, randomised clinical trial. Trials 12:24
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le G Jr, Payen D (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344–353
Reinikainen M, Karlsson S, Varpula T, Parviainen I, Ruokonen E, Varpula M, Ala-Kokko T, Pettila V (2010) Are small hospitals with small intensive care units able to treat patients with severe sepsis? Intensive Care Med 36:673–679
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20: 864–74
ICH Steering Committee (1998) International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonised tripartite guideline for good clinical practice, 3rd edn. Brookwood Medical Publications Ltd, Richmond
Fergusson D, Aaron SD, Guyatt G, Hebert P (2002) Post-randomisation exclusions: the intention to treat principle and excluding patients from analysis. BMJ 325:652–654
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Angus DC, Laterre PF, Helterbrand J, Ely EW, Ball DE, Garg R, Weissfeld LA, Bernard GR (2004) The effect of drotrecogin alfa (activated) on long-term survival after severe sepsis. Crit Care Med 32:2199–2206
Clermont G, Angus DC, Linde-Zwirble WT, Griffin MF, Fine MJ, Pinsky MR (2002) Does acute organ dysfunction predict patient-centered outcomes? Chest 121:1963–1971
Bion J, Bellomo R, Myburgh J, Perner A, Reinhart K, Finfer S (2014) Hydroxyethyl starch: putting patient safety first. Intensive Care Med 40:256–259
Perner A, Haase N, Wetterslev J (2014) Mortality in patients with hypovolemic shock treated with colloids or crystalloids. JAMA 311:1067
Wittbrodt P, Haase N, Butowska D, Winding R, Poulsen JB, Perner A (2013) Quality of life and pruritus in patients with severe sepsis resuscitated with hydroxyethyl starch long-term follow-up of a randomised trial. Crit Care 17:R58
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration. Available at: http://www.cochrane.org/handbook. Accessed 25 April 2014
Conflicts of interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: The 6S trial was funded by the Danish Medical Research Council (271-08-0691 and 09-066938) and supported by Rigshospitalets Research Council and the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (the ACTA foundation) and endorsed by the European Clinical Research Infrastructures Network (ECRIN). B Braun AG delivered trial fluids to all trial sites free of charges. Neither the funding organisations nor B Braun had any influence on (1) the design and conduct of the study; (2) the collection, management, analysis and interpretation of the data; (3) the preparation, review or approval of the manuscript; (4) the decision to submit the manuscript for publication. AP is head of research in his ICU, which receives research funds from CSL Behring, Switzerland, Fresenius Kabi, Germany, COSMED, Italy and Bioporto Diagnostics A/S, Denmark and has received a speaker’s fee from LFP SA, France. B Braun AG has covered his travel expenses for presenting 6S-data at the German Anaesthetic Congress 2012.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message:
The long-term mortality rates did not differ in patients with severe sepsis assigned to HES 130/0.42 versus Ringer’s acetate, but the trial was not powered to show this. As 90-day mortality differed, the data indicate that the harmful effects of HES occurred within the first months after randomisation.
On behalf of the 6S trial group, and the Scandinavian Critical Care Trials Group.
Members of the Scandinavian Starch for Severe Sepsis/Septic Shock (6S) trial group are listed in the Appendix.
Trial registration: clinicaltrials.gov NCT00962156.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The 6S trial investigators
Steering Committee: Anders Perner (Chair), Nicolai Haase, Anne B. Guttormsen, Jyrki Tenhunen, Gudmundur Klemenzson, Anders Åneman and Jørn Wetterslev.
Management Committee: Anders Perner (Chair), Nicolai Haase and Jørn Wetterslev.
Scientific Committee: Simon Finfer, Andre Vercueil, Lars S. Rasmussen and Frank Brunkhorst.
Data Monitoring and Safety Committee: Daniel De Backer (Chair), Peter Dalgaard and Kathy Rowan.
Writing Committee: Anders Perner (Chair), Nicolai Haase and Jørn Wetterslev.
Trial site investigators (in Denmark unless otherwise specified): Rigshospitalet: A. Perner, N. Haase, M.N. Kjær, K.R. Uhre, V. Knudsen, V. Christiansen, A. Schulze, J. Wiis, J.O. White, K. Thornberg, L.Quist, F. Sjøvall, N. Wesche, N. Reiter, I.L. Jarnvig; Næstved Hospital: K.R. Madsen, A. L. Kjældgaard, M. L. Fabritius, F. Mondrup, K.F. Sommer, L. F. Pedersen; Bispebjerg Hospital: M.H. Møller, F.C. Pott, J.A. Petersen, A. Lindhardt, K. Møller, A. Haraldson, C. Pedersen; Holbæk Hospital: H.H. Bülow, J.M. Elkjær, T. P. Møller, L.H. Andersen, L.B. Holst, J.F. Schmidt, S.T. Nielsen, F.P. Treschow, M. Overgaard, H. Ahlstrøm, S. Grangaard, J.H. Bruun, S. Larsen; Køge Hospital: L.M. Poulsen, M.V. Madsen, B. Bang; Glostrup Hospital: A. Bendtsen, Herning Hospital R. Winding, K.V. Jepsen, S. Haubjerg, N. Dey, J. Hjørringsgaard; Hvidovre Hospital: M. Steensen, J. Nielsen, C. Albek, S. Petersen, A. Christensen, A. Kristensen; Vejle Hospital: P.Berezowicz; Herlev Hospital: P. Søe-Jensen, H. Tousi; Hillerød Hospital: M. Bestle, K. Nielsen, T. Kold, K. Grundahl; Stavanger University Hospital, Norway: K. Strand, O. Larsen; Slagelse Hospital: S. Iversen, O. Schøidt; Hjørring Hospital: M. Pawlowicz, M. Kruse, H.S. Rasmussen, L.O. Nielsen; Haukeland University Hospital, Bergen, Norway: A.B. Guttormsen, B. Sjøbø; Sønderborg Hospital: S. Leivdal; Tromsø University Hospital, Norway: L.M. Ytrebø; Tampere University Hospital, Finland: J. Tenhunen, S. Karlsson, A. Kukkurainen, S. Kortelainen, M.L. Peltola, S. Varila; Gentofte Hospital: K. Thormar, P.M. Bådstøløkken; Landspitali, Reykjavik, Iceland: G. Klemenzson, S. Karason; Helsinki University Hospital, Finland: V. Pettilä, M. Kaukonen, L. Pettilä, S. Sutinen; Odense University Hospital: M. Carlson, N.H. Lassen, U.L. Larsen, K.D. Jung; Holstebro Hospital: C. Kancir; Kuopio University Hospital, Finland: J. Rutanen, E. Ruokonen, S. Rissanen, K. Kontra; Trondheim University Hospital, Norway: P. Klepstad; Esbjerg Hospital: R.E. Berthelsen, K.D. Bødker, B. Dilling.
Rights and permissions
About this article
Cite this article
Perner, A., Haase, N., Winkel, P. et al. Long-term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer’s acetate. Intensive Care Med 40, 927–934 (2014). https://doi.org/10.1007/s00134-014-3311-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3311-y