Abstract
Purpose
We assessed the predefined long-term outcomes in patients randomised in the Transfusion Requirements in Septic Shock (TRISS) trial.
Methods
In 32 Scandinavian ICUs, we randomised 1005 patients with septic shock and haemoglobin of 9 g/dl or less to receive single units of leuko-reduced red cells when haemoglobin level was 7 g/dl or less (lower threshold) or 9 g/dl or less (higher threshold) during ICU stay. We assessed mortality rates 1 year after randomisation and again in all patients at time of longest follow-up in the intention-to-treat population (n = 998) and health-related quality of life (HRQoL) 1 year after randomisation in the Danish patients only (n = 777).
Results
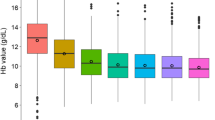
Mortality rates in the lower- versus higher-threshold group at 1 year were 53.5 % (268/501 patients) versus 54.6 % (271/496) [relative risk 0.97; 95 % confidence interval (CI) 0.85–1.09; P = 0.62]; at longest follow-up (median 21 months), they were 56.7 % (284/501) versus 61.0 % (302/495) (hazard ratio 0.88; 95 % CI 0.75–1.03; P = 0.12). We obtained HRQoL data at 1 year in 629 of the 777 (81 %) Danish patients, and mean differences between the lower- and higher-threshold group in scores of physical HRQoL were 0.4 (95 % CI −2.4 to 3.1; P = 0.79) and in mental HRQoL 0.5 (95 % CI −3.1 to 4.0; P = 0.79).
Conclusions
Long-term mortality rates and HRQoL did not differ in patients with septic shock and anaemia who were transfused at a haemoglobin threshold of 7 g/dl versus a threshold of 9 g/dl. We may reject a more than 3 % increased hazard of death in the lower- versus higher-threshold group at the time of longest follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blood transfusion is frequently given to patients with septic shock [1–4], including those who are not bleeding [5]. The most recent guidelines from the Surviving Sepsis Campaign recommended transfusion of patients with septic shock at a haemoglobin threshold of 7 g/dl aiming at levels between 7 and 9 g/dl after the initial resuscitation and in the absence of extenuating circumstances [6]. At the time of issuing, there were limited data supporting these recommendations [6] and many clinicians may not have followed them [4, 7].
Now the cumulative evidence suggests that a restrictive transfusion strategy is safe in critically ill patients [8, 9], and this may also hold for those with septic shock. At least no significant differences were observed in 90-day mortality, the use of life support or the occurrence of ischemic events between patients with septic shock and anaemia randomised to transfusion at a haemoglobin threshold of 7 g/dl versus 9 g/dl during their intensive care unit (ICU) stay in the Transfusion Requirements in Septic Shock (TRISS) trial [10]. And the restrictive strategy resulted in a marked reduction in the number of transfusions given and in the number of patients being transfused as compared to the more liberal strategy [10]. This has important implications for rational use of blood, but before stronger recommendations may be given, we need data on the effects of transfusion strategies on longer-term outcomes including survival and health-related quality of life (HRQoL) because patients with septic shock have ongoing decline in these outcomes [11–13]; in particular, because controversies remain regarding transfusion strategies in these patients [14–16].
Therefore, we present the results of predefined long-term follow-up of the TRISS trial describing the effects of transfusion at the lower versus higher haemoglobin threshold on long-term mortality and HRQoL in patients with septic shock [17].
Methods
Trial design
The TRISS trial was a multicentre, partially blinded, parallel-grouped, randomised trial using centralized computer-generated allocation sequence and stratification according to trial site and the presence or absence of active haematologic cancer, as these characteristics may influence outcome. Patients were enrolled between 3 December 2011 and 26 December 2013 in 32 general ICUs in Scandinavia. Informed consent was obtained from all patients or their legal surrogates.
Enrolled patients were randomised 1:1 to blood transfusion at a lower haemoglobin threshold or a higher haemoglobin threshold. Treatment assignments were concealed from the investigators assessing mortality and the trial statistician.
The trial protocol was approved by the relevant ethic committees and data protection agencies and the trial was registered (ClinicalTrials.gov, No. NCT01485315). The protocol, statistical analysis plan and the primary report have all been published [10, 17]; the final protocol including summary of changes and the final statistical analysis plan for the long-term outcomes are presented in the Electronic Supplementary Material (ESM) 2.
Patients
Patients aged 18 years or older, who were in the ICU, fulfilled the criteria for septic shock [18] and had a blood haemoglobin concentration of 9 g/dl or less were screened for enrolment in the trial. The exclusion criteria and trial definitions are presented in the protocol (ESM 2) and in the primary publication [10]. There were no restrictions as to when patients could be included; inclusion occurred a median 21 (interquartile range 7–47) h after ICU admission [10].
Procedures
Patients were given single units of cross-matched, pre-storage leuko-reduced red cells suspended in a saline–adenine–glucose–mannitol (SAGM) solution when the blood haemoglobin had decreased to the assigned transfusion threshold—7 g/dl in the lower-threshold group and 9 g/dl in the higher-threshold group. Within 3 h after the end of each transfusion or before the initiation of another transfusion, the haemoglobin concentrations were re-evaluated. All other interventions were at the discretion of the treating clinicians except that the use of hydroxyethyl starch was discouraged [3, 19]. The intervention period was the entire ICU stay to a maximum of 90 days after randomisation.
Long-term outcome measures
All-cause mortality at 1 year after randomisation and at the time of longest follow-up (i.e. 1 year after randomisation of the last patients) and HRQoL at 1 year after randomisation were defined secondary outcome measures in the protocol (ESM 2) [17]. Early in 2015, data on mortality for all patients were obtained from national or regional registries or patient files using the unique national personal identification number of the patients.
The HRQoL study population comprised all the patients randomised in all the 19 Danish ICUs participating in the TRISS trial. One year after randomisation a printed copy of the Danish short form health survey questionnaire (SF-36) was sent to the patient if she/he was registered to be alive (version 1 before March 2014, which was changed to version 2 after March 2014 because of licensing issues).
The SF-36 is a multipurpose health survey tool constructed of 36 items, divided into eight health domain scales (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role emotional and mental health). The component summary scores [physical component summary (PCS), and mental component summary (MCS)] reflect the two main aspects of health, and both are scored using all of the eight health domain scales of the SF-36. The component summary scores are constructed as a scale of 0–100, with higher scores reflecting better physical or mental health status [20].
We predefined the PCS score and MCS score as the HRQoL outcome measures in the TRISS trial. Version 1 questionnaires were scored according to the manual (Quality Metrics Inc.) and version 2 by the use of the scoring software (Quality Metrics Inc.).
Statistical analysis
The statistician (P.W.) performed all the analyses blinded for the intervention and according to International Conference on Harmonization Good Clinical Practice guidelines [21] and the statistical analysis plan for the long-term outcomes (ESM 2).
The analyses were done in the intention-to-treat population defined as all randomised patients (n = 1005) except the seven patients who were excluded after randomisation, namely six withdrew consent and one was randomised in error and never received the intervention, leaving 998 patients in the intention-to-treat population. We did no power calculations for the long-term outcome measures and all primary analyses were adjusted for the stratification variables (modified trial site and the presence of haematological malignancy).
The landmark mortality at 1-year follow-up of every patient was analysed using logistic regression for differences in the binary outcome (alive/dead) and odds ratios were converted to relative risks [22]. The survival at the time of longest follow-up was analysed by using Cox regression analysis supplemented by Kaplan–Meier and log-rank test analyses.
The differences in means of PCS and MCS scores at 1 year after randomisation were analysed using a general linear univariate model. The primary analysis included the patients who were dead at 1 year after randomisation; they were assigned the worst possible score value (zero). The analyses were repeated in the population of 1-year survivors.
We did supplementary analyses with (1) adjustment for the following predefined baseline variables: age, previous cardiovascular disease, surgery pre-randomisation during the index hospital admission, haemoglobin blood level, sequential organ failure assessment (SOFA) score and volume of transfused blood in the 24 h prior to randomisation, and (2) adjustment for the variables described above and simplified acute physiology score (SAPS) II in the 24 h prior to randomisation but without age and the stratification variable haematological malignancy, as they are included in SAPS II. We used SAS (v. 9.3) for the analyses and considered P values below 0.05 as statistically significant.
Missing data
The missing answers within the SF-36 domains were imputed using the missing data estimation (MDE) software (Quality Metrics Inc.). Because the number of missing total PCS and MCS scores (non-responders) was more than 5 % (20.7 % in the lower- and 17.4 % in the higher-threshold group of the total HRQoL cohort from the primary analysis) we searched for auxiliary variables in the full data set using the expectation maximization algorithm. No useful auxiliary variables could be identified and P of Little’s test was 0.69 indicating that the answers from non-responders were missing completely at random. Therefore, we did not impute values for the non-responders and analysed the PCS and MCS scores without the data of the non-responders. Missing SAPS II and SOFA score data were imputed by multiple imputations. A detailed description of the handling of the missing data is provided in the ESM 1.
Results
Baseline characteristics at randomisation were similar in the two intervention groups [10].
We obtained vital status 1 year after randomisation for 997 (99.9 %) of the 998 patients in the intention-to-treat population including 501 in the lower-threshold group and 496 in the higher-threshold group (Fig. 1). At the time of longest follow-up, which was 1 year after randomisation of the last patient, we obtained vital status for 996 (99.8 %) patients, 501 in the lower threshold-group and 495 in the higher-threshold group. At this time point, the median follow-up time among all patients was 21 months (range 12–37) (Table 1).
Patient flow including follow-up. Among the 1224 patients who fulfilled the inclusion criteria, 219 were excluded for the reasons presented in the main paper [10]; the three most frequent reasons for exclusion were blood transfusion in ICU prior to screening, consent not obtainable and ongoing acute coronary syndrome. Of the 1000 patients assigned to the two intervention groups, we obtained vital status on 996 patients on 26 December 2014, which was 1 year after randomisation of the last patient. All patients included in Denmark were followed up for health-related quality of life (HRQoL) 1 year after randomisation
HRQoL was assessed in all the 777 patients included in the 19 Danish sites (Table 1). The SF-36 questionnaire was sent out to the 321 patients who were alive at a median of 364 days (interquartile range 351–377) after randomisation; 208 (65 %) patients responded and returned the questionnaire, 108 from the lower-threshold group and 100 from the higher-threshold group (Fig. 1). The responders were older and more often had pulmonary source of sepsis as compared to those not responding (Table 1 in ESM 1). Among the responders, baseline characteristics and times to follow-up were similar in the two intervention groups (Tables 1, 2).
Long-term mortality
One year after randomisation 268 of the 501 (53 %) patients in the lower-threshold group had died as compared to 271 of the 496 (55 %) patients in the higher-threshold group [relative risk 0.97; 95 % confidence interval (CI) 0.85–1.09; P = 0.62] (Table 3). At the time of longest follow-up 284 of the 501 (57 %) patients in the lower-threshold group had died compared to 302 of the 495 (61 %) patients in the higher-threshold group (hazard ratio 0.88; 95 % CI 0.75–1.03; P = 0.12) (Table 3). The supplementary analyses adjusting for stratification variables and other potential risk factors did not change the results noticeably (Tables 2, 3 in ESM 1). There was no statistically significant difference in the probability of survival in the full observation period (log-rank test P = 0.22) (Fig. 2).
Time to death or censoring. Shown are the survival curves in the two intervention groups in the intention-to-treat population, with data censored at the time of longest follow-up, which was 1 year after randomisation of the last patient. The Kaplan–Meier analysis and log-rank test showed that the survival time did not differ between the two groups at the 5 % level of statistical significance
Health-related quality of life
We obtained PCS and MCS scores from 91 patients in each group after MDE imputation, and in the primary analysis, including the patients who had died at 1 year, we had 79.3 % complete scores in the lower-threshold group and 82.6 % complete scores in the higher-threshold group (Table 1). In the primary analysis the mean PCS scores and the mean MCS scores were similar in the lower-threshold group and the higher-threshold group (Table 3). The results did not change noticeably when the analyses were adjusted for the stratification and design variables and when the analyses were done in the data set of 1-year survivors only (Tables 4, 5 in ESM 1).
Discussion
In this large, international, randomised clinical trial of patients with septic shock and anaemia, we observed no statistically significant differences in long-term mortality rates among patients assigned to blood transfusion at a haemoglobin threshold of 7 g/dl versus a threshold of 9 g/dl during ICU stay. At the time of longest follow-up, we may reject a more than 3 % increased hazard ratio of death in the lower-threshold group versus the higher-threshold group. In the Danish patients, the quality of life did not differ between the two intervention groups 1 year after randomisation. Our results supplement those of trials with shorter follow-up times for mortality and systematic reviews of these trials suggesting that a restrictive transfusion strategy does not appear to increase mortality in critically ill patients including those with septic shock [8–10, 23–25]. As for other outcomes, results of systematic reviews of restrictive versus liberal transfusion strategies have associated restrictive transfusion decreased rates of severe infectious complications in hospitalized patients and increased risk of myocardial infarction in patient with cardiovascular disease [26, 27]. Together these apparent opposite results suggest that transfusions may have both beneficial and harmful effects, which may depend on the patient population. They also highlight the importance of assessing patient-important outcome measures whenever possible.
Our results are also in line with the long-term results of the FOCUS trial, which is the only large transfusion trial assessing long-term mortality [28]. In that trial, a liberal transfusion strategy (haemoglobin threshold 10 g/dl) was compared to a restrictive strategy (threshold 8 g/dl or symptoms of anaemia) among approximately 2000 elderly, high-risk patients who had undergone surgery for hip fracture. The 3-year follow-up showed no differences in mortality or causes of death between the two intervention groups [28].
Long-term mortality rates have also been assessed in observational studies of transfused versus non-transfused patients primarily in the perioperative setting [29, 30]. In these cohorts, blood transfusion was observed to be associated with increased long-term mortality. In spite of the use of adjusted analyses in these studies, it is unlikely that all the differences in risk factors were controlled for between groups of transfused and non-transfused patients. Therefore, these results were likely influenced by confounding by indication. On the other hand, the transfusion trials done in the perioperative setting may show differing results with some trials suggesting no effect on mortality of restrictive vs. liberal transfusion [9, 31], whereas the results of others have suggested increased mortality with restrictive transfusion strategies [9, 32]. Among these trials, long-term follow-up has only been done for the FOCUS trial, which found no effect on mortality of restrictive versus liberal transfusion as noted above.
We observed no significant differences in HRQoL scores at 1 year between the two intervention groups. Our primary analysis is influenced by the patients who had died at 1 year, whom we scored zero. The supplementary analyses done in the survivors only supported the primary analysis. It is less clear which difference in HRQoL scores represents a meaningful difference to ICU survivors, but studies have shown a minimal clinical important difference of 3 points of PCS and MCS scores across other, less severe disease states [20]. In the supplementary analysis done in the 1-year survivors only, we could not exclude a 4- to 5-point reduction in mean PCS and MCS scores in the lower- versus the higher-threshold group, but we cannot know if such differences are relevant to patients surviving septic shock. HRQoL appears to be rarely assessed in transfusion trials of critically ill patients; we only found one other transfusion trial assessing HRQoL [24]. In that pilot trial of elderly ICU patients, less than 50 patients had HRQoL assessments at 6 months, but the results were similar to ours [24]. ICU patients may have different trajectories for their recovery or continued decline in HRQoL [33], and the optimal time of follow-up remains to be established. For the assessment of landmark mortality similar challenges exists, but survival curves based on full follow-up of all patients at time of longest follow-up, as we obtained, display potential changes in risk of death over time. In some trials in sepsis, intervention effects observed at short-term follow-up have tended to diminish over time as observed in the PROWESS trial on activated protein C [34] and in the 6S trial on starch [11]. It is likely that mortality in patients with sepsis is influenced by baseline co-morbidity [35], so that late deaths from other causes than sepsis or any intervention effects may be reduced over time. The present data may show a different pattern with the highest numeric mortality difference observed between the two intervention groups at the time of longest follow-up (relative risks at 90 days, 0.94 [10]; at 1 year, 0.97; and hazard ratio at longest follow-up of 0.88 in the lower- versus the higher-threshold groups). This may, however, be a chance finding.
The use of restrictive transfusion strategies has been shown to half the relative risk of being transfused and to reduce the number of transfusions by a mean of 1.4 units in the cohorts of trial patients pooled in a recent systematic review including all published randomised trials of restrictive versus liberal strategies [8]. These results are important, because blood is a limited and expensive resource.
There are several strengths to our trial. It was investigator-initiated, funded by a not-for-profit government agency, the design and conduct was to high methodological standards [17] and we had close to 100 % follow-up for mortality. By assessing mortality in all patients at the time of longest follow-up, and not just at 1 year for each specific patient, we obtained most of the possible information generated in the trial. The trial was pragmatic including patients in university and non-university hospitals in several countries, and the long-term outcomes were similar to those of some other recent trials in ICU patients with septic shock [11, 12]. In addition, the approximately 10 % absolute difference between 90-day and 1-year mortality observed in the TRISS trial is close to the differences observed in some other recent sepsis trials [3, 11, 13]. We assessed HRQoL by a generic scale, SF-36, which has been widely used in ICU patients [36] and validated in those with sepsis [37]. All these factors increase the generalizability of our results.
Our results come with some limitations. First, the primary outcome measure of the TRISS trial was 90-day mortality; the outcomes reported here were secondary outcomes. Second, the HRQoL was only assessed in the Danish patients and there were a number of non-responders. Even though we conducted analyses to investigate consequences of the data missing from the non-responders and performed the final analyses according to these, the generalizability of the HRQoL results is reduced. Third, we had wide 95 % confidence intervals in particular for mortality at the time of longest follow-up. Therefore, we could not reject a 25 % decreased or a 3 % increased hazard of death at this time point in the lower-threshold versus the higher-threshold group.
In conclusion, long-term mortality rates and HRQoL did not differ in patients with septic shock and anaemia who were transfused at a haemoglobin threshold of 7 g/dl versus a threshold of 9 g/dl during ICU stay. At the time of longest follow-up, we may reject a more than 3 % increased hazard of death in the lower- versus the higher-threshold group.
References
Zarychanski R, Doucette S, Fergusson D, Roberts D, Houston DS, Sharma S, Gulati H, Kumar A (2008) Early intravenous unfractionated heparin and mortality in septic shock. Crit Care Med 36:2973–2979
Labelle A, Juang P, Reichley R, Micek S, Hoffmann J, Hoban A, Hampton N, Kollef M (2012) The determinants of hospital mortality among patients with septic shock receiving appropriate initial antibiotic treatment. Crit Care Med 40:2016–2021
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Rosland RG, Hagen MU, Haase N, Holst LB, Plambech M, Madsen KR, Soe-Jensen P, Poulsen LM, Bestle M, Perner A (2014) Red blood cell transfusion in septic shock—clinical characteristics and outcome of unselected patients in a prospective, multicentre cohort. Scand J Trauma Resusc Emerg Med 22:14
Haase N, Wetterslev J, Winkel P, Perner A (2013) Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med 39:2126–2134
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Reade MC, Huang DT, Bell D, Coats TJ, Cross AM, Moran JL, Peake SL, Singer M, Yealy DM, Angus DC (2010) Variability in management of early severe sepsis. Emerg Med J 27:110–115
Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J (2015) Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ 350:h1354
Fominskiy E, Putzu A, Monaco F, Scandroglio AM, Karaskov A, Galas FR, Hajjar LA, Zangrillo A, Landoni G (2015) Liberal transfusion strategy improves survival in perioperative but not in critically ill patients. A meta-analysis of randomised trials. Br J Anaesth 115:511–519
Holst LB, Haase N, Wetterslev J, Wernerman J, Guttormsen AB, Karlsson S, Johansson PI, Aneman A, Vang ML, Winding R, Nebrich L, Nibro HL, Rasmussen BS, Lauridsen JR, Nielsen JS, Oldner A, Pettila V, Cronhjort MB, Andersen LH, Pedersen UG, Reiter N, Wiis J, White JO, Russell L, Thornberg KJ, Hjortrup PB, Muller RG, Moller MH, Steensen M, Tjader I, Kilsand K, Odeberg-Wernerman S, Sjobo B, Bundgaard H, Thyo MA, Lodahl D, Maerkedahl R, Albeck C, Illum D, Kruse M, Winkel P, Perner A (2014) Lower versus higher hemoglobin threshold for transfusion in septic shock. N Engl J Med 371:1381–1391
Perner A, Haase N, Winkel P, Guttormsen AB, Tenhunen J, Klemenzson G, Muller RG, Aneman A, Wetterslev J (2014) Long-term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer’s acetate. Intensive Care Med 40:927–934
Wittbrodt P, Haase N, Butowska D, Winding R, Poulsen JB, Perner A (2013) Quality of life and pruritus in patients with severe sepsis resuscitated with hydroxyethyl starch long-term follow-up of a randomised trial. Crit Care 17:R58
Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC (2014) A randomized trial of protocol-based care for early septic shock. N Engl J Med 370:1683–1693
Holst LB, Carson JL, Perner A (2015) Should red blood cell transfusion be individualized? No. Intensive Care Med 41:1977–1979
Sakr Y, Vincent JL (2015) Should red cell transfusion be individualized? Yes. Intensive Care Med 41:1973–1976
Docherty A, Walsh TS (2015) Should blood transfusion be individualised? We are not sure. Intensive Care Med 41:1980–1982
Holst LB, Haase N, Wetterslev J, Wernerman J, Aneman A, Guttormsen AB, Johansson PI, Karlsson S, Klemenzson G, Winding R, Nebrich L, Albeck C, Vang ML, Bulow HH, Elkjaer JM, Nielsen JS, Kirkegaard P, Nibro H, Lindhardt A, Strange D, Thormar K, Poulsen LM, Berezowicz P, Badstolokken PM, Strand K, Cronhjort M, Haunstrup E, Rian O, Oldner A, Bendtsen A, Iversen S, Langva JA, Johansen RB, Nielsen N, Pettila V, Reinikainen M, Keld D, Leivdal S, Breider JM, Tjader I, Reiter N, Gottrup U, White J, Wiis J, Andersen LH, Steensen M, Perner A (2013) Transfusion Requirements in Septic Shock (TRISS) trial—comparing the effects and safety of liberal versus restrictive red blood cell transfusion in septic shock patients in the ICU: protocol for a randomised controlled trial. Trials 14:150
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Haase N, Perner A, Hennings LI, Siegemund M, Lauridsen B, Wetterslev M, Wetterslev J (2013) Hydroxyethyl starch 130/0.38–0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ 346:f839
Maruish ME (2011) User’s manual for the SF-36v2 health survey. QualityMetric, Lincoln
ICH Steering Committee (1998) International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use. ICH harmonised tripartite guideline for statistical principles for clinical trials, 3rd edn. Brookwood Medical Publications, Brookwood
Zhang J, Yu KF (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 340:409–417
Walsh TS, Boyd JA, Watson D, Hope D, Lewis S, Krishan A, Forbes JF, Ramsay P, Pearse R, Wallis C, Cairns C, Cole S, Wyncoll D (2013) Restrictive versus liberal transfusion strategies for older mechanically ventilated critically ill patients: a randomized pilot trial. Crit Care Med 41:2354–2363
Villanueva C, Colomo A, Bosch A, Concepcion M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santalo M, Muniz E, Guarner C (2013) Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med 368:11–21
Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, Hickner A, Rogers MA (2014) Health care-associated infection after red blood cell transfusion: a systematic review and meta-analysis. JAMA 311:1317–1326
Docherty AB, O’Donnell R, Brunskill S, Trivella M, Doree C, Holst L, Parker M, Gregersen M, de Pinheiro AJ, Walsh TS, Stanworth SJ (2016) Effect of restrictive versus liberal transfusion strategies on outcomes in patients with cardiovascular disease in a non-cardiac surgery setting: systematic review and meta-analysis. BMJ 352:i1351
Carson JL, Sieber F, Cook DR, Hoover DR, Noveck H, Chaitman BR, Fleisher L, Beaupre L, Macaulay W, Rhoads GG, Paris B, Zagorin A, Sanders DW, Zakriya KJ, Magaziner J (2015) Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet 385:1183–1189
van Straten AH, Bekker MW, Soliman Hamad MA, van Zundert AA, Martens EJ, Schonberger JP, de Wolf AM (2010) Transfusion of red blood cells: the impact on short-term and long-term survival after coronary artery bypass grafting, a 10-year follow-up. Interact Cardiovasc Thorac Surg 10:37–42
Shaw RE, Johnson CK, Ferrari G, Brizzio ME, Sayles K, Rioux N, Zapolanski A, Grau JB (2014) Blood transfusion in cardiac surgery does increase the risk of 5-year mortality: results from a contemporary series of 1714 propensity-matched patients. Transfusion 54:1106–1113
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K, Macaulay W, Lewis C, Cook DR, Dobbin G, Zakriya KJ, Apple FS, Horney RA, Magaziner J (2011) Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 365:2453–2462
Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, Reeves BC (2015) Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 372:997–1008
Iwashyna TJ (2012) Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med 186:302–304
Angus DC, Laterre PF, Helterbrand J, Ely EW, Ball DE, Garg R, Weissfeld LA, Bernard GR (2004) The effect of drotrecogin alfa (activated) on long-term survival after severe sepsis. Crit Care Med 32:2199–2206
Clermont G, Angus DC, Linde-Zwirble WT, Griffin MF, Fine MJ, Pinsky MR (2002) Does acute organ dysfunction predict patient-centered outcomes? Chest 121:1963–1971
Winters BD, Eberlein M, Leung J, Needham DM, Pronovost PJ, Sevransky JE (2010) Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med 38:1276–1283
Heyland DK, Hopman W, Coo H, Tranmer J, McColl MA (2000) Long-term health-related quality of life in survivors of sepsis. Short form 36: a valid and reliable measure of health-related quality of life. Crit Care Med 28:3599–3605
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The trial was funded by the Danish Strategic Research Council and supported by Copenhagen University Hospital, Rigshospitalet, the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (the ACTA Foundation) and Ehrenreich’s Foundation. The funders had no role in the design of the study, collection and analyses of data or the writing of the report. The TRISS trial was endorsed by the European Clinical Research Infrastructures Network (ECRIN).
Conflicts of interest
The Department of Intensive Care, Rigshospitalet receives support for research from CSL Behring, Fresenius Kabi and Ferring Pharmaceuticals. No other potential conflict of interest relevant to this article was reported.
Additional information
Members of the Transfusion Requirements in Septic Shock (TRISS) Trial Group are listed in the Electronic Supplementary Material 1.
Take-home message: In patients with septic shock, we may reject a more than 3 % increased long-term hazard of death with transfusion at a lower versus a higher haemoglobin threshold.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rygård, S.L., Holst, L.B., Wetterslev, J. et al. Long-term outcomes in patients with septic shock transfused at a lower versus a higher haemoglobin threshold: the TRISS randomised, multicentre clinical trial. Intensive Care Med 42, 1685–1694 (2016). https://doi.org/10.1007/s00134-016-4437-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4437-x