Abstract
Objective
To test whether assessing pulmonary permeability by transpulmonary thermodilution enables to differentiate increased permeability pulmonary edema (ALI/ARDS) from hydrostatic pulmonary edema.
Design
Retrospective review of cases.
Setting
A 24-bed medical intensive care unit of a university hospital.
Patients
Forty-eight critically ill patients ventilated for acute respiratory failure with bilateral infiltrates on chest radiograph, a PaO2/FiO2 ratio < 300 mmHg and extravascular lung water indexed for body weight ≥ 12 ml/kg.
Intervention
We assessed pulmonary permeability by two indexes obtained from transpulmonary thermodilution: extravascular lung water/pulmonary blood volume (PVPI) and the ratio of extravascular lung water index over global end-diastolic volume index. The cause of pulmonary edema was determined a posteriori by three experts, taking into account medical history, clinical features, echocardiographic left ventricular function, chest radiography findings, B-type natriuretic peptide serum concentration and the time-course of these findings with therapy. Experts were blind for pulmonary permeability indexes and for global end-diastolic volume.
Measurements and results
ALI/ARDS was diagnosed in 36 cases. The PVPI was 4.7 ± 1.8 and 2.1 ± 0.5 in patients with ALI/ARDS and hydrostatic pulmonary edema, respectively (p < 0.05). The extravascular lung water index/global end-diastolic volume index ratio was 3.0 × 10−2 ± 1.2 × 10−2 and 1.4 × 10−2 ± 0.4 × 10−2 in patients with ALI/ARDS and with hydrostatic pulmonary edema, respectively (p < 0.05). A PVPI ≥ 3 and an extravascular lung water index/global end-diastolic index ratio ≥ 1.8 × 10−2 allowed the diagnosis of ALI/ARDS with a sensitivity of 85% and specificity of 100%.
Conclusion
These results suggest that indexes of pulmonary permeability provided by transpulmonary thermodilution may be useful for determining the mechanism of pulmonary edema in the critically ill.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary edema is a common finding in the critically ill. However, it is a daily dilemma for the intensivist to determine which mechanism is responsible for the extravascular lung water (EVLW) increase: extravasation of fluid toward the interstitium due to increased hydrostatic pressure into the pulmonary capillary bed, or increased permeability of the lung capillary membrane due to its damage, as during acute lung injury (ALI) or acute respiratory distress syndrome (ARDS). Although the usual definition of ALI/ARDS requires ensuring that the filling pressures of the left ventricle are not elevated [1], the use of a pulmonary artery catheter for this purpose is questionable [2]. In this regard, determination of the pulmonary vascular permeability index could be helpful [3, 4].
The transpulmonary thermodilution technique provides an estimation of EVLW [5, 6] and of the pulmonary blood volume. The ratio between these two parameters, called “pulmonary vascular permeability index” (PVPI), is believed to reflect the permeability of the alveolo–capillary barrier [6]. PVPI should be elevated in ALI/ARDS (which simply means that the EVLW should be high compared with the pulmonary blood volume), while it should be normal in hydrostatic pulmonary edema. In the present study in mechanically ventilated patients, we tested whether PVPI was actually greater in ALI/ARDS than in hydrostatic pulmonary edema and whether a threshold value of PVPI could be determined for distinguishing between these two diagnoses. In addition, we tested the relevance of another index of pulmonary permeability for this purpose. This index, which is the simple ratio of EVLW indexed for body weight (EVLWi) to global end-diastolic volume (GEDV) indexed for body surface (GEDVi) [7], derives its advantage from being computed from two variables that are directly measured by the pulmonary thermodilution technique and displayed on any dedicated monitor.
Patients and methods
Patients
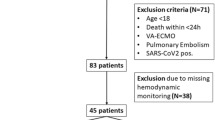
We studied 49 mechanically ventilated critically ill patients who were already monitored by transpulmonary thermodilution and for whom the diagnosis of pulmonary edema was established on (1) the presence of bilateral infiltrates on chest radiograph [8], (2) a PaO2/FiO2 (P/F) ratio ≤ 300 mmHg and (3) an increase in EVLWi ≥ 12 ml/kg. Patients for whom there was no consensus regarding the diagnosis were excluded from the study. The retrospective collection of data was approved by the institutional review board of our institution (Bicêtre Hospital).
Transpulmonary thermodilution measurements
A thermistor placed into a femoral arterial catheter measures the downstream temperature changes induced by the injection of a cold saline solution bolus in the superior vena cava. The monitor (PiCCOplus®, version 6.0, Pulsion Medical System, Munich, Germany) calculates cardiac output from the thermodilution curve using the Stewart–Hamilton algorithm and also calculates the mean transit time and the exponential downslope time of the transpulmonary thermodilution curve. The product of cardiac output and mean transit time, i.e. the distribution volume of the thermal indicator [9], is the intrathoracic thermal volume (intrathoracic blood volume + EVLW). The product of cardiac output and exponential downslope time is the pulmonary thermal volume (pulmonary blood volume + EVLW) [10]. Therefore, the GEDV is calculated as the difference between the intrathoracic and the pulmonary thermal volume [5, 11]. The intrathoracic blood volume is calculated by multiplying the GEDV by 1.25, assuming a constant relationship between these parameters [5]. The EVLW value is deducted from the difference between the intrathoracic thermal volume and the estimated intrathoracic blood volume. The pulmonary blood volume is deducted from the difference between the pulmonary thermal volume and the EVLW. The PVPI is finally calculated as the ratio between EVLW and pulmonary blood volume.
In the present study, GEDVi, EVLWi, cardiac index (cardiac output indexed for body surface) and PVPI were collected at the time of the diagnosis of pulmonary edema. We also calculated the ratio of EVLWi to GEDVi [7]. This ratio is mathematically related to PVPI since with the transpulmonary thermodilution technique, the pulmonary blood volume that is used in calculating PVPI is simply one quarter of GEDV (EVLWi/GEDVi = PVPI × 0.25 × body surface/body weight).
Assessment of other variables
At the time of diagnosis, echocardiography had been performed in all patients to measure the left ventricular ejection fraction. A chest radiology score had been calculated by dividing each lung into two parts horizontally. The density of pulmonary infiltrate was proportionally scored from 1 to 3 in each part. The total score thus ranges from 0 to 12 [12]. The B-type natriuretic peptide serum concentration had been measured during the preceding hour in all but eight patients.
Diagnosis of the pulmonary edema mechanism
Three experts (two cardiologists and one lung specialist, all practitioners in intensive care), retrospectively determined the mechanism of pulmonary edema (i.e. hydrostatic or due to increased pulmonary microvascular permeability). For this purpose, they particularly took into account patient's past and present history, clinical presentation, chest radiograph, echocardiography features, cardiac index, EVLWi and serum concentration of B-type natriuretic peptide (when available) at the time when pulmonary edema was present. They also paid particular attention to the time course of all the preceding findings under therapy. Importantly, the experts were blind for PVPI, GEDVi and the EVLWi/GEDVi ratio.
Statistical analysis
The variables with a normal distribution (Kolmogorov–Smirnov test for normality) were expressed as mean value ± SD. The B-type natriuretic peptide serum concentration and the norepinephrine dosage were not normally distributed and were expressed as median values [25–75 interquartile range]. The comparison between patients with hydrostatic pulmonary edema and patients with ALI/ARDS was performed using a two-tailed Student t-test for the normally distributed variables and a Mann–Whitney U-test for the B-type natriuretic peptide concentration and the norepinephrine dosage. The mortality rate and the number of patients receiving norepinephrine were compared by a chi-square test. Receiver operating characteristic (ROC) curves were generated for PVPI, the EVLWi/GEDVi ratio and GEDVi, varying the discriminating threshold of each parameter. The area under the ROC curve (± SE) for each parameter was calculated and compared using a Hanley–McNeil test. The reproducibility of the PVPI measurement over a short time period was assessed in 10 patients after completion of the study. In these patients, hemodynamic monitoring required successive thermodilution measurements over a period of 15 min. The reproducibility between successive sets of PVPI measurements was expressed as the mean difference between measurements ± SD and as the mean percentage error (mean difference between measurements divided by the average of measurements). The repeatability of the PVPI measurement was expressed as 1.96 times the SD of the differences between repeated measurements. Statistical analysis was performed by means of the Statview 5.0 software (Abacus Concepts, Berkeley, CA) for all tests except the Hanley–McNeil test, which was performed with the MedCalc 8.1.0.0 software (Mariakerke, Belgium). A p value < 0.05 was considered statistically significant.
Results
Patients characteristics
Forty-nine patients were studied. For one patient, no consensus was achieved to discriminate between both mechanisms of pulmonary edema, and this patient was excluded from the further analysis. Considering the whole population of the remaining patients (30 men and 18 women, 57 ± 16 years of age), the chest radiograph score was 9 ± 3 and EVLWi was 22 ± 9 ml/kg. At the time of pulmonary edema occurrence, the presence of pneumonia was identified in 36 patients. A catecholamine was administered in 27 patients (norepinephrine in all cases). Six patients suffered from a non-pulmonary infection with septic shock. Two patients had an intra-alveolar hemorrhage. Pulmonary edema developed after drowning in one patient, during a trial of weaning from mechanical ventilation in one patient and in the context of myocarditis in the remaining patient.
Diagnosis of the mechanism of pulmonary edema
The experts attributed pulmonary edema to a hydrostatic mechanism in 12 patients and to a non-hydrostatic mechanism in 36 patients.
The patients' characteristics are summarized in Table 1, according to the causal diagnosis. Compared with the patients with hydrostatic pulmonary edema, the patients with ALI/ARDS exhibited significantly higher left ventricular ejection fraction and EVLWi, and significantly lower GEDVi and P/F ratio. In patients with ALI/ARDS, compared with patients with hydrostatic pulmonary edema, the level of the positive end-expiratory pressure was significantly higher and the tidal volume was significantly lower. The cardiac index was not statistically different between groups.
Pulmonary permeability indexes
The difference between successive measurements of PVPI was –0.02 ± 0.09 and the mean percentage error was –0.72 ± 4.23%. The repeatability of the PVPI was 0.25 ± 0.17.
The PVPI was 4.7 ± 1.8 in patients with ALI/ARDS and 2.1 ± 0.5 in patients with hydrostatic pulmonary edema (p < 0.05). In ALI/ARDS patients, PVPI was moderately although significantly correlated with the P/F ratio (r = 0.42). A PVPI value ≥ 3 allowed the diagnosis of ALI/ARDS to be established with sensitivity of 85% and specificity of 100%, i.e. only 5 out of 36 patients were misclassified since they had a PVPI value < 3 (Fig. 1). The five false-negative patients were characterized by a higher chest radiology score than the true-positive patients (12 ± 4 vs. 8 ± 4).
The EVLWi/GEDVi ratio was 3.0 × 10−2 ± 1.2 × 10−2 in patients with ALI/ARDS and 1.4 × 10−2 ± 0.4 × 10−2 in patients with hydrostatic pulmonary edema (p < 0.05). An EVLWi/GEDVi ratio ≥ 1.8 × 10−2 allowed establishing the diagnosis of ALI/ARDS with a sensitivity of 85% and specificity of 100%.
The areas under the ROC curve established for PVPI (0.92 ± 0.04) as well as the ROC curve established for the EVLWi/GEDVi ratio (0.92 ± 0.04) were significantly greater than the area under the ROC curve established for GEDVi (0.84 ± 0.08), i.e. the other variable that exhibited a significant difference between ALI/ARDS and hydrostatic pulmonary edema patients and that was unknown for the experts (Fig. 2).
The mortality rate was significantly higher in ALI/ARDS patients than in patients with hydrostatic pulmonary edema (56% vs. 33%). Considering the whole population, PVPI was significantly higher in patients who died (4.6 ± 2.1) than in survivors (3.5 ± 1.5). Similar findings were observed for the EVLWi/GEDVi ratio.
Discussion
This study demonstrates that in mechanically ventilated patients with pulmonary edema, PVPI assessed by transpulmonary thermodilution was greater in ALI/ARDS than in hydrostatic pulmonary edema, confirming its clinical relevance. Additionally, PVPI was able to discriminate between hydrostatic pulmonary edema and ALI/ARDS with acceptable accuracy. The same conclusions could be drawn if the EVLWi/GEDVi ratio was used for assessing pulmonary permeability.
Discriminating between hydrostatic pulmonary edema and ALI/ARDS is an important issue, since the appropriate therapy differs. The differential diagnosis is based on the assessment of the left atrial pressure, assumed to be normal in ALI/ARDS [1, 13]. However, this hemodynamic definition of ALI/ARDS is questionable [3]. First, the measurement of the pulmonary artery occlusion pressure, which is a reflection of left atrial pressure, is prone to numerous pitfalls [2] and is often misinterpreted [14, 15, 16]. Second, the pulmonary artery occlusion pressure may not reflect the hydrostatic pressure at the site of lung filtration (pulmonary microvessels) [17, 18]. Third, left ventricular preload can be elevated in ALI/ARDS, in particular in patients who have been already volume resuscitated and/or have some degree of cardiac failure, preexisting or related to sepsis. In this regard, the pulmonary artery occlusion pressure was recently found to be elevated in 30% of ARDS patients during the time-course of their disease [19]. Thus, the definition of ALI/ARDS should include the functional feature of lung injury, i.e. an increased pulmonary microvascular permeability [4, 13], and there is a need for a bedside measurement of this key parameter [3].
The transpulmonary thermodilution technique is a bedside method for assessing the distribution of fluids toward the intrathoracic compartment [5]. Particularly, by estimating EVLW and pulmonary blood volume, i.e. two well-defined intrathoracic volumes, and by simply calculating their ratio, the single indicator dilution method provides a bedside estimation of the pulmonary vascular permeability [6]. In a study in dogs, Katzenelson et al. found that PVPI was higher in increased permeability than in hydrostatic pulmonary edema, although no cut-off value was provided for distinguishing the two mechanisms [6]. Our study deals with the clinical setting, where the differential diagnosis between increased permeability and hydrostatic pulmonary edema may be difficult. In particular, PVPI may help to detect an increased pulmonary permeability even in patients with a high left ventricular filling pressure, i.e. patients with a pulmonary edema of “mixed” origin. Identifying such patients is difficult in the real world at the time when pulmonary edema occurs, but it was possible in our study, because the case analysis was retrospective and took into account not only the individual data but also their evolution during therapy.
Groeneveld and Verheij recently demonstrated that an index of pulmonary permeability assessed by the thermal-dye transpulmonary dilution technique was imperfect for measuring protein permeability in patients with sepsis-induced ALI/ARDS [7]. This suggests that such an index could be helpful for differentiating hydrostatic pulmonary edema and ALI/ARDS, i.e. two conditions with very different pulmonary permeability, but that it could be less accurate in distinguishing high from very high increased permeability in ALI/ARDS. In fact, in the latter condition, the inability of the thermal indicator to access pulmonary zones with severe lung insult [20, 21] could decrease the reliability of the technique. In this regard, the PVPI exhibited higher specificity than sensitivity for establishing the causal diagnosis of pulmonary edema in our study. In the false-negative cases of our study, EVLW and PVPI may have been underestimated due to difficult dilution of the thermal indicator towards the high-density condensed areas of the ARDS lung [20, 21]. In this regard, a higher chest radiology score was observed in the false-negative cases than in the true-positive ones.
In contrast to thermal-dye dilution, the transpulmonary thermodilution system does not directly measure the intrathoracic blood volume – and thus the pulmonary blood volume – but calculates it from GEDV. The present study logically confirms that, when the single thermodilution is used, the EVLWi/GEDVi ratio could be considered instead of PVPI for determining the mechanism of pulmonary edema. Since the EVLWi and the GEDVi are directly measured and displayed on the dedicated monitor, pulmonary permeability can be assessed at the bedside by simply dividing those two variables.
Our study has some limitations. First, the mechanism of pulmonary edema was defined by experts, but this does not exclude some degree of arbitrariness. However, we selected only the cases where a total agreement between experts was obtained. Second, the number of patients of the study was small and these results require confirmation. In particular, many patients suffered from pneumonia, a condition known to influence the thermodilution technique, and our results should be confirmed in a larger and general population. By taking an EVLWi ≥ 12 ml/kg for inclusion, we specifically addressed the problem of severe pulmonary edema but we excluded an unknown number of patients with less severe pulmonary edema, particularly in patients with hydrostatic pulmonary edema. Considering a lower EVLW benchmark for inclusion could have lowered the diagnostic cut-off value of pulmonary permeability indexes. Third, we used the single indicator dilution technique for assessing pulmonary blood volume and EVLW. Using the thermal-dye dilution could have changed our findings. Finally, higher positive end-expiratory pressure in ALI/ARDS patients could have reduced the GEDV without altering the EVLW by the same proportion. This could have theoretically lowered PVPI and the EVLWi/GEDVi ratio values in ALI/ARDS patients compared with patients with hydrostatic pulmonary edema independently from differences in pulmonary permeability.
In conclusion, this study demonstrates that pulmonary permeability indexes obtained by transpulmonary thermodilution can be helpful for distinguishing between hydrostatic pulmonary edema and ALI/ARDS.
References
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Monnet X, Teboul JL (2006) Invasive measures of left ventricular preload. Curr Opin Crit Care 12:235–240
Isakow W, Schuster DP (2006) Extravascular lung water measurements and hemodynamic monitoring in the critically ill: bed-side alternatives to the pulmonary artery catheter. Am J Physiol Lung Cell Mol Physiol 291:L1118–1131
Schuster DP (1997) Identifying patients with ARDS: time for a different approach. Intensive Care Med 23:1197–1203
Sakka SG, Ruhl CC, Pfeiffer UJ, Beale R, McLuckie A, Reinhart K, Meier-Hellmann A (2000) Assessment of cardiac preload and extravascular lung water by single transpulmonary thermodilution. Intensive Care Med 26:180–187
Katzenelson R, Perel A, Berkenstadt H, Preisman S, Kogan S, Sternik L, Segal E (2004) Accuracy of transpulmonary thermodilution versus gravimetric measurement of extravascular lung water. Crit Care Med 32:1550–1554
Groeneveld AB, Verheij J (2006) Extravascular lung water to blood volume ratios as measures of permeability in sepsis-induced ALI/ARDS. Intensive Care Med 32:1315–1321
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138:720–723
Meier P, Zierler KL (1954) On the theory of the indicator-dilution method for measurement of blood flow and volume. J Appl Physiol 6:731–744
Newman EV, Merrell M, Genecin A, Monge C, Milnor WR, Mc Keever WP (1951) The dye dilution method for describing the central circulation. An analysis of factors shaping the time-concentration curves. Circulation 4:735–746
Neumann P (1999) Extravascular lung water and intrathoracic blood volume: double versus single indicator dilution technique. Intensive Care Med 25:216–219
Fagon JY, Chastre J, Vuagnat A, Trouillet JL, Novara A, Gibert C (1996) Nosocomial pneumonia and mortality among patients in intensive care units. JAMA 275:866–869
Abraham E, Matthay MA, Dinarello CA, Vincent JL, Cohen J, Opal SM, Glauser M, Parsons P, Fisher CJ Jr, Repine JE (2000) Consensus conference definitions for sepsis, septic shock, acute lung injury, and acute respiratory distress syndrome: time for a reevaluation. Crit Care Med 28:232–235
Gnaegi A, Feihl F, Perret C (1997) Intensive care physicians' insufficient knowledge of right-heart catheterization at the bedside: time to act? Crit Care Med 25:213–220
Iberti TJ, Fischer EP, Leibowitz AB, Panacek EA, Silverstein JH, Albertson TE (1990) A multicenter study of physicians' knowledge of the pulmonary artery catheter. Pulmonary Artery Catheter Study Group. JAMA 264:2928–2932
Iberti TJ, Daily EK, Leibowitz AB, Schecter CB, Fischer EP, Silverstein JH (1994) Assessment of critical care nurses' knowledge of the pulmonary artery catheter. The Pulmonary Artery Catheter Study Group. Crit Care Med 22:1674–1678
Nunes S, Ruokonen E, Takala J (2003) Pulmonary capillary pressures during the acute respiratory distress syndrome. Intensive Care Med 29:2174–2179
Teboul JL, Andrivet P, Ansquer M, Besbes M, Rekik N, Lemaire F, Brun-Buisson C (1992) Bedside evaluation of the resistance of large and medium pulmonary veins in various lung diseases. J Appl Physiol 72:998–1003
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Matthay MA (2002) Clinical measurement of pulmonary edema. Chest 122:1877–1879
Fernandez-Mondejar E, Castano-Perez J, Rivera-Fernandez R, Colmenero-Ruiz M, Manzano F, Perez-Villares J, de la Chica R (2003) Quantification of lung water by transpulmonary thermodilution in normal and edematous lung. J Crit Care 18:253–258
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0499-5
Rights and permissions
About this article
Cite this article
Monnet, X., Anguel, N., Osman, D. et al. Assessing pulmonary permeability by transpulmonary thermodilution allows differentiation of hydrostatic pulmonary edema from ALI/ARDS. Intensive Care Med 33, 448–453 (2007). https://doi.org/10.1007/s00134-006-0498-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0498-6