Abstract
The effects of diabetes mellitus on the pharmacokinetics and pharmacodynamics of drugs have been well described in experimental animal models; however, only minimal data exist for humans and the current knowledge regarding the effects of diabetes on these properties remains unclear. Nevertheless, it has been observed that the pharmacokinetics and pharmacodynamics of drugs are changed in subjects with diabetes. It has been reported that diabetes may affect the pharmacokinetics of various drugs by affecting (i) absorption, due to changes in subcutaneous adipose blood flow, muscle blood flow and gastric emptying; (ii) distribution, due to non-enzymatic glycation of albumin; (iii) biotransformation, due to regulation of enzymes/transporters involved in drug biotransformation; and (iv) excretion, due to nephropathy. Previously published data also suggest that diabetes-mediated changes in the pharmacokinetics of a particular drug cannot be translated to others.
Although clinical studies exploring the effect of diabetes on pharmacodynamics are still very limited, there is evidence that disease-mediated effects are not limited only to pharmacokinetics but also alter pharmacodynamics. However, for many drugs it remains unclear whether these influences reflect diabetes-mediated changes in pharmacokinetics rather than pharmacodynamics. In addition, even though diabetes-mediated pharmacokinetics and pharmacodynamics might be anticipated, it is important to study the effect on each drug and not generalize from observed data.
The available data indicate that there is a significant variability in drug response in diabetic subjects. The discrepancies between individual clinical studies as well as between ex vivo and clinical studies are probably due to (i) the restricted and focused population of subjects in clinical studies; (ii) failure to consider type, severity and duration of the disease; (iii) histopathological characteristics generally being missing; and (iv) other factors such as varying medication use, dietary protein intake, age, sex and obesity. The obesity epidemic in the developed world has also inadvertently influenced the directions of pharmacological research.
This review attempts to map new information gained since Gwilt published his paper in Clinical Pharmacokinetics in 1991. Although a large body of research has been conducted and significant progress has been made, we still have to conclude that the available information regarding the effect of diabetes on pharmacokinetics and pharmacodynamics remains unclear and further clinical studies are required before we can understand the clinical significance of the effect. An understanding of diabetes-mediated changes as well as of the source of the variability should lead to the improvement of the medical management and clinical outcomes in patients with this widespread disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Introduction
Diabetes mellitus is one of the most significant public health problems. The number of patients with diabetes is increasing due to population growth and a growing prevalence of physical inactivity leading to obesity.[1] In 1985, approximately 30 million people were reported to have diabetes worldwide.[2] A decade later, this estimate had reached 140 million.[3] In 2003, the global prevalence of diabetes was estimated to be 250 million.[3] Including undiagnosed cases of diabetes, this number is expected to reach 438 million by 2030 (approximately 7.5% of the adult population).[1,3,4] There seems to be no region of the world that will not be affected by the disease. While some of this increase will be observed in Australia, Europe and North America, the majority will be seen in countries undergoing westernization (the African continent, South America, China, India and the Middle East).[1] The majority of diabetic patients are between 45 and 65 years of age in developing countries, while they are ≥65 years of age in developed countries.[3,5] Although type 2 diabetes was previously considered to be a chronic disease of middle and late adulthood, it is increasingly becoming prevalent in adolescents.[6] The number of deaths attributable to diabetes has been estimated at around 3 million per year, which is approximately 5% of global mortality.[7]
Two types of diabetes predominate in the population. Type 1 diabetes is characterized by an inability of the body to produce insulin, whereas type 2 diabetes reflects deficient insulin secretion and/ or insulin resistance (approximately 90% of all cases of diabetes).[8] Some patients are difficult to classify as having type 1 or 2 diabetes, thus other specific types of the disease have been described (e.g. gestational diabetes, malnutrition-related diabetes, etc.). Gestational diabetes represents a separate entity as do other specific types of diabetes associated with genetic defects, diseases of the exocrine pancreas (i.e. pancreatitis, cancer or cystic fibrosis), drug- or chemical-induced, infection-related or immune-mediated diabetes. Risk factors for diabetes are anthropometric factors (e.g. obesity), metabolic factors (e.g. parameters of glucose metabolism), lifestyle factors (e.g. physical activity), metabolic syndrome, age, sex and ethnicity.[9] Most people with type 2 diabetes are obese and the degree of duration of obesity correlates with the risk of the diabetes. Obesity and inactivity are two of the most important lifestyle risk factors for type 2 diabetes.[10] It has been observed that changes in lifestyle and a moderate level of physical activity can prevent type 2 diabetes.[11,12]
One of the major concerns with the diabetes epidemic is the increase in both morbidity and mortality related to complications of the disease. Diabetes is associated with a progression of microvascular (e.g. nephropathy, neuropathy, retinopathy) and macrovascular (e.g. myocardial infarction, stroke) complications.[13] Thus, the use of drugs by patients with diabetes is expectedly higher than in an age-matched population without the disease.[14,15] Total diabetes costs were estimated at $US174 billion in the US[16] and £3.5 billion in the UK in 2007.[17] On the other hand, Aggarwal[18] reported that US sales of insulin products reached $US8.4 billion.
Although the effect of diabetes on chemically induced animal models of the disease has been studied extensively, minimal data are available on the effect of diabetes on pharmacokinetics and pharmacodynamics in humans. An understanding of diabetes-mediated changes as well as the source of the variability should lead to the improvement of medical management and clinical outcomes in patients with this widespread disease. Since the last review covering the effect of the diabetes on the pharmacokinetics and pharmacodynamics of drugs,[19] a number of related original publications have appeared. In this review, general information related to diabetes-mediated changes in clinical pharmacokinetics and pharmacodynamics is discussed. We conducted a systemic review of previously published literature (end date January 2012) by searching the PubMed and relevant bibliographies. Only papers from the English and German literature were included in the review.
2. Effect of Diabetes Mellitus on Pharmacokinetics
Not only is drug use more widespread, but the pharmacokinetics of these drugs may also be altered by the disease itself.[19–21] Diabetes affects protein, lipids and carbohydrate metabolism, and the systems that regulate these biochemical pathways are also in many cases involved in drug biotransformation. Thus, it is not surprising that diabetes affects the pharmacokinetics of drugs. Diabetes may influence the pharmacokinetics of numerous drugs by affecting (i) absorption, due to changes in subcutaneous/muscle blood flow and delayed gastric emptying; (ii) distribution, due to non-enzymatic glycation of albumin; (iii) biotransformation, due to differential regulation of enzymes involved in drug biotransformation and drug transporters; and (iv) excretion, due to nephropathy.[20–22] However, pharmacokinetic studies in diabetic patients are limited compared with pharmacokinetic studies in animals.[23] Moreover, different results were obtained between these studies and, thus, animal data should be extrapolated only very carefully to humans.[23]
2.1 Absorption
Micro- and macrovascular changes are probably the main long-term complication of diabetes. Gastric mucosal blood flow has been reported to be significantly reduced in diabetic patients (2.81 ± 0.15 V) compared with non-diabetic subjects (4.77 ± 0.29 V).[24] Because it has been demonstrated that gastric mucosal blood flow varies in the same direction as gastric acid secretion,[25–27] changed mucosal blood flow might explain gastric pH changes in diabetic patients.[28]
It is long known that longstanding type 1 and 2 diabetes can be associated with a change in the gastric emptying time and intestinal transit time,[29–50] which was first reported by Boas[51] in 1925. The prevalence of delayed gastric emptying in diabetic patients has ranged from 28% to 65%;[52,53] however, the relationship between delayed emptying and symptoms is variable[52,54,55] (it should be pointed out that the number of diabetic patients with emptying delay was underestimated in early studies that employed less sensitive diagnostic methods to quantify gastric emptying[56]). Numerous studies have observed delayed gastric emptying time in poorly controlled diabetic patients[30] and showed a strong correlation with the progression of the disease.[52,57–59] In most cases, the emptying of solid meat components and low-nutrient liquids is delayed to a varying degree in diabetic patients,[39,48,60,61] whereas the emptying of liquids has not been found to be affected by the disease.[39,48,60–62] However, there are discrepancies in the literature; for example, gastric emptying rates in patients with type 2 diabetes have been reported to be decreased,[33,36,45,60,63,64] unchanged[65] or accelerated.[66,67] Some of these discrepancies may be explained by (i) differences in the study design; (ii) uncontrolled hyperglycaemia;[68–70] or (iii) diabetes-related changes in intestinal hormones.[71] Increased knowledge of the pathophysiology of diabetes has contributed to a development of new treatments such as glucagon-like peptide-1 agonists and dipeptidyl peptidase-4 inhibitors. These new classes of antidiabetic drugs can mask the effect of the disease on gastrointestinal tract motility and make it harder to distinguish the effect of the disease and the effect of the drug.[72] It has also been reported that cystic fibrosis reduces level of free incretin hormones,[73] resulting in decreased gastric emptying time.[73,74] Although many studies have reported diabetes-mediated changes in gastric emptying time, it seems that the magnitude of the delay is modest and should not be clinically important.
Transit time in diabetic patients has been reported to be significantly lower than in non-diabetic patients (gastric transit time: 24 [4–108] vs 87 [1–478] min;[75] small bowel transit time: 302.0 ± 62.7 vs 261.2 ± 55.5 min;[75] transit time: 20.4 ± 15.6 vs 34.9 ± 29.6 hours,[76] 24.3 ± 11.9 vs 43.2 ± 22 hours,[77] 9.9 ± 6.1 vs 14.4 ± 8.3 hours[78] and 35.4 ± 4.7 vs 53.8 ± 5.5 hours[79]). Delayed transit time is probably due to vagal denervation[80] and seems to be more frequent in patients with autonomic neuropathy.[45,81,82] Recent studies have demonstrated that the blood glucose concentration itself has a major impact on gastrointestinal tract motility; marked hyperglycaemia appears to affect every region of gastrointestinal tract.[68,76,83] The mechanisms by which hyperglycaemia affects gastric emptying include suppression of antral contraction,[68] increased pyloric contractions,[68] proximal stomach relaxation[68] and induction of gastric electrical dysrhythmias.[84]
Della-Coletta and Eller[85] reported slower absorption (26%) of tolazamide in diabetic patients than in healthy volunteers. In addition, Adithan et al.[86] reported a decrease (26%) in the absorption of orally administered ampicillin in patients with type 2 diabetes. By contrast, O’Connell et al.[87] reported that basic pharmacokinetic parameters of metoclopramide after single- and multiple-dose administration were not affected by diabetes. In addition, Wahlin-Boll et al.[88] reported complete absorption of the oral sulfonylurea glipizide (administered as a solution as well as tablet form) in patients with type 2 diabetes as compared with previously reported studies with healthy volunteers.[89] Prokinetic drugs in general result in dose-related improvement in gastric emptying time; however, variations in the blood glucose concentration may account for variability in results from studies that are related to the effect of these drugs on gastric emptying in diabetic patients.[90–94]
It has been suggested that differences in the absorption rate and bioavailability between patients with diabetes and healthy subjects depend on several factors (table I). Previously published studies have reported that the rate of absorption of subcutaneously administered insulin strongly correlates with subcutaneous blood flow.[99–102] It is well known that abdominal subcutaneous fat tissue blood flow is increased in subjects with type 1 diabetes, probably due to reduced subcutaneous fat tissue (5.0 ± 2.3 vs 11.3 ± 9.1 mL/100 g/min[95]).[103] Nosadini et al.[95] reported faster absorption of insulin in subjects with type 1 diabetes; however, no difference was found in bioavailability of the drug. On the other hand, in insulin resistant and/or obese patients subcutaneous adipose tissue blood flow is reduced compared with healthy normal-weight subjects (by approximately 50%[104]).[105–109]
Diabetic patients exhibit compromised muscle blood flow (59.4 ± 12.9 vs 46.7 ± 14.1 mL/100 g/min[97]) at rest[97,110] and also after exercise.[111] This may be a result of blunted endothelium-dependent vasodilation,[111–113] an increased plasma level of endothelin-1,[114] a reduction in capillary density[115,116] or decreased mitochondrial volume[117] and function.[118] These changes may lead to a reduced rate of absorption for drugs with an intramuscular route of administration. This finding was supported by studies when insulin,[96] aminoglycosides[119] and benzylpenicillin[98,120] were administered to diabetic patients.
2.2 Distribution
The volume of distribution of a drug correlates with the degree of obesity, and because obesity is one of the most important factors in the development of insulin resistance and diabetes, the volume of distribution of lipophilic drugs is affected by the disease[121,122] (for more information, see the review by Hanley et al.[123]). On the other hand, obesity does not affect serum albumin and drug binding to albumin; however, data regarding α1-glycoprotein are contradictory.[123] A modest increase in concentration of free diazepam (1.9 vs 1.5 L/kg)[124] nitrazepam (19.7 vs 17.9 L/kg)[125] and oxazepam (5.1 vs 4.0 L/kg)[126] reported in obese individuals might be explained by elevation in serum free fatty acids found in obese individuals. Reduced tissue blood flow as well as alterations in cardiac structure and function has also been reported in obese patients.[107,127]
Diabetic patients have higher level of circulating glucose in the blood, leading to non-enzymatic glycation of several proteins including albumin. Glycated albumin exhibits atherogenic effects in various cells.[128] Non-enzymatic glycation of albumin produces conformational changes in the structure of albumin (affinity of the phenytoin binding site on albumin based on a modification of the lysine group[129]), which can increase the free fraction of acidic drugs in patients with type 1 and 2 diabetes (for more detail, see table II).[21,137–144] Worner et al.[138] reported a 50% decrease in binding of dansylsarcosine to albumin in diabetic patients, whereas the concentration of circulating albumin was the same in diabetic patients.[139,145,146] Glycation of blood and plasma proteins leads to reduction in protein binding capacity.[21,22,147] A linear relationship has been reported between the degree of albumin glycation and the unbound fraction of drug in the serum of diabetic patients.[137,139,140] Thus, for highly albumin bound acidic compounds the reduction in the plasma serum protein binding capacity has been shown in diabetic patients.[19,137] However, studies employing a smaller number of diabetic patients might easily fail to show this linear relationship. There are also inconsistencies in the reported studies; for example, the volume of distribution of antipirine has been increased,[132] unchanged[133–135] or decreased[136] in diabetic compared with non-diabetic patients. In addition, the volume of distribution of paracetamol (acetaminophen)[130] as well as theophylline[86,130] was increased in diabetic patients. These inconsistencies may reflect the degree of control of the diabetes, the duration of the disease and/or the presence of complications of the disease. It has been reported that diabetes can affect drug binding in several ways: (i) changing the amount and concentration of circulating free fatty acids, the level of which is increased in diabetic patients[137,148,149] (e.g. the binding of valproic acid was significantly decreased in diabetic patients;[150] a strong correlation has been previously observed between the free fraction of valproic acid and serum free fatty acid concentration[145]); (ii) increasing blood concentration of substrates possibly inhibits drug binding; and (iii) conformation changes of plasma proteins (as shown in table III).
2.3 Biotransformation
The effect of obesity on drug biotransformation is very variable. Obesity has been linked to decreased hepatic blood flow, non-alcohol fatty acid disease and the accumulation of fat in the liver tissue.[153,154] The effect of obesity on cytochrome P450 (CYP) appears to be enzyme specific: the enzyme activity of CYP2E1 has been increased in obese individuals.[155] Oral clearance of triazolam (CYP3A subfamily marker) has been decreased in obese compared with non-obese individuals (340 ± 44 vs 531 ± 38 mL/min).[156] On the other hand, obesity did not significantly affect clearance of midazolam (CYP3A subfamily marker) [471 ± 38 vs 530 ± 54 mL/min].[156] The effect of the disease on the activity of other CYP enzymes remains controversial or insufficiently studied.[155,156]
The clearance of drugs undergoing glucuronidation and sulfatation appears to be increased in obese individuals.[156] Abernethy et al.[126] reported increased biotransformation of oxazepam (3.1 times greater) and lorazepam (1.6 times greater) in obese individuals.
In diabetic patients, abnormal hepatic function occurs frequently, especially non-alcohol steatohepatitis, macrovesicular steatosis, liver fibrosis/cirrhosis and focal fatty liver.[157,158] Hence, it is not surprising that diabetes affects drug biotransformation. There have been numerous studies on the effect of chemically induced diabetes on drug biotransformation in both mice and rats.[159–161] Animal models of diabetes fall into two main groups: type 1 (chemically induced diabetes using, for example, alloxan and streptozotocin) and type 2 (spontaneous autosomal recessive mutations, e.g. C57BL/6J ob/ob, C57BL/KsJ db/db, yellow obese mice, Zucker diabetic rats), consistent with the aetiologies of the two main types of the disease in humans. However, data from animal studies (especially from small laboratory animals[23]) should be evaluated with care when trying to predict changes in humans.[162]
Hepatic-mediated biotransformation in diabetic humans is characterized only for a few compounds.[163] In addition, a correlation between diabetes and the activity of enzymes involved in the biotransformation is poorly known. In general, it is apparent that uncontrolled diabetes causes an overall increase in CYP enzymes although phase II enzymes are significantly decreased. Total hepatic CYP content in biopsies of diabetic patients is significantly increased in type 1 and decreased in type 2 diabetic patients.[164] The majority of studies have examined the effect of diabetes on the modulation of CYP2E1; however, varied data exist regarding whether diabetes affects expression and activity of this CYP enzyme.[165–170] Song et al.[169] reported that CYP2E1 protein levels were elevated in the lymphocytes of children and adolescents with type 1 diabetes, and a strong correlation has been observed between the enzyme level and glycosylated haemoglobin. On the other hand, enzyme activity was not changed in a group of seven type 1 and 15 type 2 patients with diabetes using chlorozoxazone as a marker of CYP2E1.[165] In addition, the protein level of CYP2E1 has not been affected by diabetes.[169] Several studies that focused on the effect of diabetes on the clearance of theophylline or caffeine (a marker of CYP1A2 enzyme activity) have suggested that there is no difference in the enzyme activity of non-diabetic and type 1 and 2 diabetic patients.[130,171–174] Sotaniemi et al.[164] found that among type 2 diabetic patients, women biotransformed antipyrin normally whereas men over 40 years of age showed reduced biotransformation. In addition, no change was found in the biotransformation of tolbutamide (a marker of CYP2C9 enzyme activity)[175] and hepatic aryl hydrocarbon hydroxylase (mediated by CYP1A1).[164] Dyer et al.[176] did not observe any change in quinidine (a non-validated marker of CYP3A subfamily activity) between non-diabetic and diabetic patients. However, other studies have described significant downregulation of liver CYP3A4 enzyme activity[177] as well as in the biotransformation of lidocaine (non-validated marker of CYP3A subfamily marker)[178,179] [for more details, see table IV].
Minimal data exist on the effect of diabetes on the phase II biotransformation in human.[23] Evidence suggests that oxidative stress is increased in diabetes because of extensive production of reactive oxygen species and an impaired antioxidant defence mechanism.[183] Thus, the majority of studies have studied the effect of diabetes on the activity of enzymes that are part of the antioxidant defence system such as the glutathione-S-transferase (GST) superfamily. Controversy exists regarding the effect of diabetes on phase II biotransformation enzymes.[23] Some studies did not show a difference in erythrocyte GST between patients with type 1 and 2 diabetes and healthy controls.[184,185] On the other hand, McRobie et al.[180] has reported significant downregulation in placental GST activity in type 1 diabetic patients. Dostalek et al.[177] described significant downregulation in gene expression, protein levels and enzyme activity of liver uridine diphosphate glucuronosyltransferase (UGT) 2B7 in liver samples from diabetic donors (for more details, see table V). No changes have been observed for selected enzymes from the UGT 1A subfamily.[177] The effect of diabetes on drug clearance is summarized in table VI.
Clinical studies investigating the effect of diabetes on gene expression and protein levels of drug transporters are limited. It has been demonstrated that gene and protein expression of ABCA1 and ABCG1 in leukocytes from patients with type 2 diabetes was reduced and strongly correlated with the level of glycaemia.[188–190]
2.4 Excretion
The effect of obesity on kidney function is not clear.[125,191] However, glomerular filtration and tubular secretion has been shown to be increased in obese individuals, whereas tubular reabsorption has been decreased by the disease.[125] Clearance does not linearly increase with body weight in obese individuals.[123]
Diabetes-related nephropathy is the leading cause of end-stage renal disease in industrialized countries.[192,193] Nephropathy develops in approximately 40% of diabetic patients.[194,195] It has been observed that function of the renin-angiotensin system is stimulated in diabetic patients with nephropathy and angiotensin II affects the synthesis of glomerular proteins.[196] Inhibitors of angiotensin-converting enzyme are used in type 2 diabetic patients with nephropathy to slow the progression of the disease.[197–199] Diabetes causes micro- and macrovascular changes and leads to hyperfiltration and, hence, an increased glomerular filtration rate.[200,201] It has also been observed that lowering medication doses correlates with a lowering of the glomerular filtration rate.[201] Although poor glycaemic control is an important risk factor, the glucose level does not fully explain why only a subset of patients with diabetes progress to end-stage renal disease.[202]
Numerous studies have been conducted to examine the effect of diabetes on the disposition of antibacterials in children. For example, the half-life and glomerular filtration rate of carbenicillin were determined in diabetic children[203] and the glomerular filtration rate was significantly increased. However, serum concentrations were not been affected for kanamycin, bekanamicin and amikacin.[204] Although diabetic patients are more prone to developing renal failure, studies show weak correlations between renal function and the clearance of drugs.
3. Effect of Diabetes Mellitus on Pharmacodynamics
Information regarding the effect of diabetes on the pharmacodynamics of drugs is very limited; however, evidence that the effect of diabetes is not limited to the pharmacokinetics of drugs exists. Almost all previously published studies have reported the effect of diabetes on the pharmacodynamics of cardiovascular and immunosuppressive drugs. However, the question is whether these influences reflect diabetes-mediated changes in pharmacokinetics rather than pharmacodynamics?
Cardiovascular diseases are the cause of death in approximately 80% of patients with diabetes and account for 75% of all hospitalizations in diabetes patients. Hence, not surprisingly, cardiovascular drug therapy is frequently started in subjects with diabetes. It has been suggested that diabetes may alter the pharmacokinetics of several cardiovascular drugs.[19] Recently published studies show a marginal effect; discrepancies occur in lipid-lowering[205–207] and antihypertensive drugs.[151,178,179] However, very few clinically significant diabetes-mediated changes in the pharmacokinetics of cardiovascular drugs have been reported. It has been demonstrated that diabetic patients exhibited significant reduction in isoprenalin-induced heart rate as compared with non-diabetic patients.[142,208] Similar data have been observed for both atropine and propranolol (pharmacokinetic data have not been reported).[209] Reduced biological activity of catecholamines due to changes protein binding has been suggested as one possible mechanism. However, no changes were found in the protein binding of catecholamines.[141] Tissue adaptation on changes in the insulin level is also suggested as pathophysiological,[210,211] and the hypothesis of changed G-protein function has been proposed.[212] In addition, Terada et al.[213] reported an increase in the chronothropic response to administration of exogenous epinephrine in diabetic patients as compared with non-diabetic patients. Packer et al.[214] reported a greater reduction in left ventricular filling pressure and mean right atrial pressure in diabetic patients as compared with non-diabetic patients. These changes can be attributed to a renin/aldosterone synthesis and angiotensin-mediated vasoregulation that are known to exist in diabetic patients. On the other hand, no difference in mean prothrombin time has been reported between diabetic and non-diabetic patients when warfarin was administered.[215]
Because diabetes is associated with renal microvascular damage, the glomerular filtration rate finally declines below 15 mL/min, leading to end-stage renal disease, which is irreversible and fatal if untreated, but a patient’s life can be sustained through haemodialysis followed by kidney transplantation. Approximately 40% of all kidney transplant recipients in the US have diabetes at the time of transplantation surgery.[216] In addition, post-transplant diabetes occurs in 4–20% of renal transplant recipients.[217,218] However, post-transplant diabetes is not only typical for renal transplant recipients, it also develops in 2.5–25% of liver transplant recipients, 4–40% of heart transplant recipients and 30–35% of lung transplant recipients.[219] To prevent organ rejection, a transplant recipient remains dependent on lifelong therapy with a cocktail of immunosuppressive agents (a calcineurin/mammalian target of rapamycin [mTOR] inhibitor, antiproliferative drug and corticosteroid).
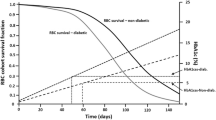
The literature is consistent about the effect of the disease on the pharmacokinetics of immunosuppressive drugs, reporting no change in the unbound fraction of pharmacologically active ciclosporin,[220,221] or the area under the plasma concentration-time curve of tacrolimus[222,223] and mycophenolic acid.[224–226] However, diabetes has been shown to reduce expression of B-cell surface markers and markers of T-cell activity,[227,228] and increase the risk of infection-related mortality in diabetic subjects.[229,230] Previously published studies also demonstrated diabetes-mediated reductions in (i) protein leakage;[231–233] (ii) microvascular responses to inflammatory mediators;[234,235] (iii) degranulation of mast cells;[236] (iv) leukocyte-endothelial cell interactions;[237–242] (v) lymph node retention capacity;[243] and (vi) release of tumour necrosis factor-α and interleukin-1β by leukocytes upon exposure to lipopolysaccharide.[244]
Although no effect of diabetes on the mycophenolic acid plasma concentration has previously been reported,[227,245,246] the disease highly significantly reduced gene expression, protein level and enzyme activity of both inosine 5′-monophosphate (IMP) dehydrogenase (IMPDH) type 1 and type 2.[227,246,247] The enzyme catalyses nicotinamide adenine dinucleotide-dependent oxidation of IMP to xanthosine 5′-monophosphate. This is the rate-limiting step in the de novo pathway for guanine nucleotide biosynthesis in B and T lymphocytes.[248] Although a clear relationship between increased infection-related morbidity and downregulation of IMPDH has not been reported, the present investigation provides novel observations that may partially explain the increased susceptibility to infections in diabetic patients.[249,250] Because of lower immune system activity, diabetic patients may require an increased dose of antibacterials or immunosuppressive drugs to achieve an adequate level of immunosuppressive activity. However, further clinical studies in a larger number of patients with diabetes are needed to verify whether optimization of antibacterial/immunosuppressive drug dosing is required for these patients.
Last, but not least, we would like to discuss antidiabetic drugs, which are used to keep diabetes under control. It is hard to study the effect of diabetes on the pharmacokinetics and pharmacodynamics of antidiabetic drugs because they are used mainly for the treatment of the disease. The major organs involved in elimination of these drugs are the liver and kidney (e.g. rosiglitazone and pioglitazone are eliminated mainly by CYP enzymes, whereas metformin is eliminated mainly via glomerular filtration and tubular secretion and to some extent via liver CYP enzymes). CYP2C and 3A subfamilies are the main enzymes involved in the biotransformation of antidiabetic drugs. Although diabetes affects the activity of CYP3A (discussed in section 2.3), no changes in the pharmacokinetics of antidiabetic drugs have previously been reported.[131,182,251–253]
4. Discussion and Conclusion
There are always ethical limitations in performing clinical studies. In order to overcome these limitations, chemically induced animal models of diabetes have been established. The effects of diabetes on the pharmacokinetics and pharmacodynamics of drugs have been well described in experimental models of diabetes; however, in humans only minimal data exists and the effects of the disease on such properties are not yet clear. Nevertheless, it has been shown that the pharmacokinetics and pharmacodynamics of drugs are changed in diabetes. Available data also indicate that there is a significant variability in drug response in diabetic patients. For example, gastric emptying rates in patients with type 2 diabetes have been reported to be decreased, unchanged or accelerated (as discussed in section 2.1). The reasons for the discrepancies between individual clinical studies as well as between experimental and clinical studies are probably due to (i) the restricted and focused population of subjects in clinical studies; (ii) failure to consider type, severity and duration of the disease; (iii) histopathological characteristics generally being missing; and (iv) other factors, including varying medication use, dietary protein intake, obesity, age and sex. An understanding of diabetes-mediated changes in pharmacodynamics as well as the source of the variability in patient responses to treatment should lead to better medical management of diabetic patients and improvement of clinical outcomes in this population.
In 1991, Gwilt et al.[19] concluded their excellent comprehensive review on the effect of diabetes on pharmacokinetics and pharmacodynamics by saying that further clinical studies are warranted to explain the variability in observed data and to understand the mechanisms behind diabetes-mediated changes. Although clinical research has begun to make significant progress in characterizing the pathophysiology and genetic basis of diabetes, available information regarding the effect of the disease on pharmacokinetics and pharmacodynamics, efficacy and safety of drugs is limited and inconsistent. In addition, diabetes-related changes in the pharmacodynamics of drugs have been studied less than changes in pharmacokinetics. Previously published data also suggest that these diabetes-mediated changes in the pharmacokinetics of a particular drug cannot be translated to others. Unfortunately, our conclusions are similar to those published by Gwilt and colleagues[19] 20 years ago. The effect of diabetes on pharmacokinetics and pharmacodynamics remains unclear and further clinical studies are required to understand the clinical significance of the effects.
References
Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004 May; 27(5): 1047–53
International Diabetes Federation Task Force on Diabetes Health Economy. Diabetes heath economics: facts, figures, and forecasts. Brussels: International Diabetes Federation, 1997
King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 1998 Sep; 21(9): 1414–31
Rossing P, de Zeeuw D. Need for better diabetes treatment for improved renal outcome. Kidney Int Suppl 2011 Mar; (120): S28–32
King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults: WHO Ad Hoc Diabetes Reporting Group. Diabetes Care 1993 Jan; 16(1): 157–77
Arslanian S. Type 2 diabetes in children: clinical aspects and risk factors. Horm Res 2002; 57 Suppl. 1: 19–28
World Health Organization. Diabetes fact sheet no. 312, August 2011 [online]. Available from URL: http://www.who.int/mediacentre/factsheets [Accessed 2012 May 5]
Morwessel NJ. The genetic basis of diabetes mellitus. AACN Clin Issues 1998 Nov; 9(4): 539–54
Herder C, Karakas M, Koenig W. Biomarkers for the prediction of type 2 diabetes and cardiovascular disease. Clin Pharmacol Ther 2011 Jul; 90(1): 52–66
Wing RR, Goldstein MG, Acton KJ, et al. Behavioral science research in diabetes: lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care 2001 Jan; 24(1): 117–23
Bassuk SS, Manson JE. Epidemiological evidence for the role of physical activity in reducing risk of type 2 diabetes and cardiovascular disease. J Appl Physiol 2005 Sep; 99(3): 1193–204
LaMonte MJ, Blair SN, Church TS. Physical activity and diabetes prevention. J Appl Physiol 2005 Sep; 99(3): 1205–13
Engelgau MM, Geiss LS, Saaddine JB, et al. The evolving diabetes burden in the United States. Ann Intern Med 2004 Jun 1; 140(11): 945–50
Rendell M, Lassek WD, Ross DA, et al. A pharmaceutical profile of diabetic patients. J Chronic Dis 1983; 36(2): 193–202
Isacson D, Stalhammar J. Prescription drug use among diabetics: a population study. J Chronic Dis 1987; 40(7): 651–60
American Diabetes Association. Economic costs of diabetes in the U.S. in 2007 [published erratum appears in Diabetes Care 2008; 31 (6): 1271]. Diabetes Care 2008; 31(3): 596–615
Watkins P. Diabetes and its management. Oxford: Blackwell Publishing, 2003
Aggarwal S. What’s fueling the biotech engine-2010 to 2011. Nat Biotechnol 2011; 29(12): 1083–9
Gwilt PR, Nahhas RR, Tracewell WG. The effects of diabetes mellitus on pharmacokinetics and pharmacodynamics in humans. Clin Pharmacokinet 1991 Jun; 20(6): 477–90
Cashion AK, Holmes SL, Hathaway DK, et al. Gastroparesis following kidney/pancreas transplant. Clin Transplant 2004 Jun; 18(3): 306–11
Zini R, Riant P, Barre J, et al. Disease-induced variations in plasma protein levels: implications for drug dosage regimens (part I). Clin Pharmacokinet 1990 Aug; 19(2): 147–59
Okabe N, Hashizume N. Drug binding properties of glycosylated human serum albumin as measured by fluorescence and circular dichroism. Biol Pharm Bull 1994 Jan; 17(1): 16–21
Wang T, Shankar K, Ronis MJ, et al. Mechanisms and outcomes of drug- and toxicant-induced liver toxicity in diabetes. Crit Rev Toxicol 2007 Jun; 37(5): 413–59
Zhu L. Gastric mucosal blood flow and blood viscosity in patients with diabetes [in Chinese]. Zhonghua Yi Xue Za Zhi 1993 Aug; 73(8): 476–8, 511
Jacobson ED, Chang AC. Comparison of gastrin and histamine on gastric mucosal blood flow. Proc Soc Exp Biol Med 1969 Feb; 130(2): 484–6
Jacobson ED, Linford RH, Grossman MI. Gastric secretion in relation to mucosal blood flow studied by a clearance technic. J Clin Invest 1966 Jan; 45(1): 1–13
Moody FG. Oxygen consumption during thiocyanate inhibition of gastric acid secretion in dogs. Am J Physiol 1968 Jul; 215(1): 127–31
Hasler WL, Coleski R, Chey WD, et al. Differences in intragastric pH in diabetic vs. idiopathic gastroparesis: relation to degree of gastric retention. Am J Physiol Gastrointest Liver Physiol 2008 Jun; 294(6): G1 384–91
Stacher G. Diabetes mellitus and the stomach. Diabetologia 2001 Sep; 44(9): 1080–93
Samsom M, Bharucha A, Gerich JE, et al. Diabetes mellitus and gastric emptying: questions and issues in clinical practice. Diabetes Metab Res Rev 2009 Sep; 25(6): 502–14
Domstad PA, Kim EE, Coupal JJ, et al. Biologic gastric emptying time in diabetic patients, using Tc-99m-labeled resin-oatmeal with and without metoclopramide. J Nucl Med 1980 Nov; 21(11): 1098–100
Horowitz M, McNeil JD, Maddern GJ, et al. Abnormalities of gastric and esophageal emptying in polymyositis and dermatomyositis. Gastroenterology 1986 Feb; 90(2): 434–9
Keshavarzian A, Iber FL, Vaeth J. Gastric emptying in patients with insulin-requiring diabetes mellitus. Am J Gastroenterol 1987 Jan; 82(1): 29–35
Gilbey SG, Watkins PJ. Measurement by epigastric impedance of gastric emptying in diabetic autonomic neuropathy. Diabet Med 1987 Mar–Apr; 4(2): 122–6
Caballero-Plasencia AM, Muros-Navarro MC, Martin-Ruiz JL, et al. Gastroparesis of digestible and indigestible solids in patients with insulin-dependent diabetes mellitus or functional dyspepsia. Dig Dis Sci 1994 Jul; 39(7): 1409–15
Ziegler D, Schadewaldt P, Pour Mirza A, et al. [13C]octanoic acid breath test for non-invasive assessment of gastric emptying in diabetic patients: validation and relationship to gastric symptoms and cardiovascular autonomic function. Diabetologia 1996 Jul; 39(7): 823–30
Lipp RW, Schnedl WJ, Hammer HF, et al. Evidence of accelerated gastric emptying in longstanding diabetic patients after ingestion of a semisolid meal. J Nucl Med 1997 May; 38(5): 814–8
Dutta U, Padhy AK, Ahuja V, et al. Double blind controlled trial of effect of cisapride on gastric emptying in diabetics. Trop Gastroenterol 1999 Jul–Sep; 20(3): 116–9
Loo FD, Palmer DW, Soergel KH, et al. Gastric emptying in patients with diabetes mellitus. Gastroenterology 1984 Mar; 86(3): 485–94
Merio R, Festa A, Bergmann H, et al. Slow gastric emptying in type I diabetes: relation to autonomic and peripheral neuropathy, blood glucose, and glycemic control. Diabetes Care 1997 Mar; 20(3): 419–23
De Block CE, De Leeuw IH, Pelckmans PA, et al. Delayed gastric emptying and gastric autoimmunity in type 1 diabetes. Diabetes Care 2002 May; 25(5): 912–7
Meier M, Linke R, Tatsch K, et al. An advanced approach for the assessment of gastric motor function in long-term type 1 diabetes mellitus with and without autonomic neuropathy. Clin Auton Res 2002 Jun; 12(3): 197–202
Iber F, Parveen S, Vandrunen M, et al. Relation of symptoms to impaired stomach, small bowel, and colon motility in long-standing diabetes. Dig Dis Sci 1993; 38(1): 45–50
Horowitz M, Harding PE, Maddox AF, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1989 Mar; 32(3): 151–9
Wegener M, Borsch G, Schaffstein J, et al. Gastrointestinal transit disorders in patients with insulin-treated diabetes mellitus. Dig Dis 1990; 8(1): 23–36
Cotroneo P, Grattagliano A, Rapaccini GL, et al. Gastric emptying rate and hormonal response in type II diabetics. Diabetes Res 1991 Jun; 17(2): 99–104
Annese V, Bassotti G, Caruso N, et al. Gastrointestinal motor dysfunction, symptoms, and neuropathy in noninsulin-dependent (type 2) diabetes mellitus. J Clin Gastroenterol 1999 Sep; 29(2): 171–7
Chang CS, Kao CH, Wang YS, et al. Discrepant pattern of solid and liquid gastric emptying in Chinese patients with type II diabetes mellitus. Nucl Med Commun 1996 Jan; 17(1): 60–5
Qi HB, Luo JY, Zhu YL, et al. Gastric myoelectrical activity and gastric emptying in diabetic patients with dyspeptic symptoms. World J Gastroenterol 2002 Feb; 8(1): 180–2
Camilleri M. Clinical practice: diabetic gastroparesis. N Engl J Med 2007 Feb 22; 356(8): 820–9
Boas I. Diseases of stomach. Leipzig: Georg Thieme, 1925
Horowitz M, Fraser R. Disordered gastric motor function in diabetes mellitus. Diabetologia 1994 Jun; 37(6): 543–51
Horowitz M, Wishart JM, Jones KL, et al. Gastric emptying in diabetes: an overview. Diabet Med 1996 Sep; 13 (9 Suppl. 5): S16–22
Jones KL, Russo A, Stevens JE, et al. Predictors of delayed gastric emptying in diabetes. Diabetes Care 2001 Jul; 24(7): 1264–9
Kong MF, Horowitz M. Gastric emptying in diabetes mellitus: relationship to blood-glucose control. Clin Geriatr Med 1999 May; 15(2): 321–38
Chang J, Rayner C, Jones K, et al. Diabetic gastroparesis: backwards and forwards. J Gastroenterol Hepatol 2011; 26 Suppl. 1: 46–57
Horowitz M, O’Donovan D, Jones KL, et al. Gastric emptying in diabetes: clinical significance and treatment. Diabet Med 2002 Mar; 19(3): 177–94
Naesens M, Verbeke K, Vanrenterghem Y, et al. Effects of gastric emptying on oral mycophenolic acid pharmacokinetics in stable renal allograft recipients. Br J Clin Pharmacol 2007 May; 63(5): 541–7
Bian RW, Lou QL, Gu LB, et al. Delayed gastric emptying is related to cardiovascular autonomic neuropathy in Chinese patients with type 2 diabetes. Acta Gastroenterol Belg 2011 Mar; 74(1): 28–33
Lyrenas EB, Olsson EH, Arvidsson UC, et al. Prevalence and determinants of solid and liquid gastric emptying in unstable type I diabetes: relationship to postprandial blood glucose concentrations. Diabetes Care 1997 Mar; 20(3): 413–8
Wright RA, Clemente R, Wathen R. Diabetic gastroparesis: an abnormality of gastric emptying of solids. Am J Med Sci 1985 Jun; 289(6): 240–2
Troncon LE, Rosa-e-Silva L, Oliveira RB, et al. Abnormal intragastric distribution of a liquid nutrient meal in patients with diabetes mellitus. Dig Dis Sci 1998 Jul; 43(7): 1421–9
Horowitz M, Maddox AF, Wishart JM, et al. Relationships between oesophageal transit and solid and liquid gastric emptying in diabetes mellitus. Eur J Nucl Med 1991; 18(4): 229–34
Nowak TV, Johnson CP, Kalbfleisch JH, et al. Highly variable gastric emptying in patients with insulin dependent diabetes mellitus. Gut 1995 Jul; 37(1): 23–9
Kong MF, King P, Macdonald IA, et al. Euglycaemic hyperinsulinaemia does not affect gastric emptying in type I and type II diabetes mellitus. Diabetologia 1999 Mar; 42(3): 365–72
Frank JW, Saslow SB, Camilleri M, et al. Mechanism of accelerated gastric emptying of liquids and hyperglycemia in patients with type II diabetes mellitus. Gastroenterology 1995 Sep; 109(3): 755–65
Schwartz JG, Green GM, Guan D, et al. Rapid gastric emptying of a solid pancake meal in type II diabetic patients. Diabetes Care 1996 May; 19(5): 468–71
Rayner CK, Samsom M, Jones KL, et al. Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care 2001 Feb; 24(2): 371–81
MacGregor IL, Gueller R, Watts HD, et al. The effect of acute hyperglycemia on gastric emptying in man. Gastroenterology 1976 Feb; 70(2): 190–6
Russo A, Stevens JE, Chen R, et al. Insulin-induced hypoglycemia accelerates gastric emptying of solids and liquids in long-standing type 1 diabetes. J Clin Endocrinol Metab 2005 Aug; 90(8): 4489–95
Asmar M. New physiological effects of the incretin hormones GLP-1 and GIP. Dan Med Bull 2011 Feb; 58(2): B4248
Drucker DJ, Nauck MA. The incretin system: glucagon-like pep tide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 2006 Nov 11; 368(9548): 1696–705
Hillman M, Eriksson L, Mared L, et al. Reduced levels of active GLP-1 in patients with cystic fibrosis with and without diabetes mellitus. J Cyst Fibros 2012 Mar; 11(2): 144–9
Kuo P, Stevens JE, Russo A, et al. Gastric emptying, incretin hormone secretion, and postprandial glycemia in cystic fibrosis: effects of pancreatic enzyme supplementation. J Clin Endocrinol Metab 2011 May; 96(5): E851–5
Triantafyllou K, Kalantzis C, Papadopoulos AA, et al. Video-capsule endoscopy gastric and small bowel transit time and completeness of the examination in patients with diabetes mellitus. Dig Liver Dis 2007 Jun; 39(6): 575–80
Jung HK, Kim DY, Moon IH, et al. Colonic transit time in diabetic patients: comparison with healthy subjects and the effect of autonomic neuropathy. Yonsei Med J 2003 Apr 30; 44(2): 265–72
Wu MJ, Chang CS, Cheng CH, et al. Colonic transit time in long-term dialysis patients. Am J Kidney Dis 2004 Aug; 44(2): 322–7
Iida M, Ikeda M, Kishimoto M, et al. Evaluation of gut motility in type II diabetes by the radiopaque marker method. J Gastroenterol Hepatol 2000 Apr; 15(4): 381–5
Werth B, Meyer-Wyss B, Spinas GA, et al. Non-invasive assessment of gastrointestinal motility disorders in diabetic patients with and without cardiovascular signs of autonomic neuropathy. Gut 1992 Sep; 33(9): 1199–203
Scarpello JH, Greaves M, Sladen GE. Small intestinal transit in diabetics. Br Med J 1976 Nov 20; 2(6046): 1225–6
Dooley CP, el Newihi HM, Zeidler A, et al. Abnormalities of the migrating motor complex in diabetics with autonomic neuropathy and diarrhea. Scand J Gastroenterol 1988 Mar; 23(2): 217–23
Oliveira RB, Troncon LE, Meneghelli UG, et al. Gastric accommodation to distension and early gastric emptying in diabetics with neuropathy. Braz J Med Biol Res 1984; 17(1): 49–53
Fraser RJ, Horowitz M, Maddox AF, et al. Hyperglycaemia slows gastric emptying in type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1990 Nov; 33(11): 675–80
Jebbink RJ, Samsom M, Bruijs PP, et al. Hyperglycemia induces abnormalities of gastric myoelectrical activity in patients with type I diabetes mellitus. Gastroenterology 1994 Nov; 107(5): 1390–7
Della-Coletta A, Eller M. The bioavailability of tolazamid in diabetic patients and healthy subjects [abstract no. PP 1301]. Pharmacol Res 1988; 5: S174
Adithan C, Danda D, Shashindran CH, et al. Differential effect of type I and type II diabetes mellitus on antipyrine elimination. Methods Find Exp Clin Pharmacol 1989 Dec; 11(12): 755–8
O’Connell ME, Awni WM, Goodman M, et al. Bioavailability and disposition of metoclopramide after single- and multiple-dose administration in diabetic patients with gastroparesis. J Clin Pharmacol 1987 Aug; 27(8): 610–4
Wahlin-Boll E, Almer LO, Melander A. Bioavailability, pharmacokinetics and effects of glipizide in type 2 diabetics. Clin Pharmacokinet 1982 Jul–Aug; 7(4): 363–72
Fuccella LM, Tamassia V, Valzelli G. Metabolism and kinetics of the hypoglycemic agent glipizide in man: comparison with glibenclamide. J Clin Pharmacol New Drugs 1973 Feb–Mar; 13(2): 68–75
Stacher G, Lenglinger J, Bergmann H, et al. Gastric emptying: a contributory factor in gastro-oesophageal reflux activity? Gut 2000 Nov; 47(5): 661–6
Maganti K, Onyemere K, Jones MP. Oral erythromycin and symptomatic relief of gastroparesis: a systematic review. Am J Gastroenterol 2003 Feb; 98(2): 259–63
Havelund T, Oster-Jorgensen E, Eshoj O, et al. Effects of cisapride on gastroparesis in patients with insulin-dependent diabetes mellitus: a double-blind controlled trial. Acta Med Scand 1987; 222(4): 339–43
de Caestecker JS, Ewing DJ, Tothill P, et al. Evaluation of oral cisapride and metoclopramide in diabetic autonomic neuropathy: an eight-week double-blind crossover study. Aliment Pharmacol Ther 1989 Feb; 3(1): 69–81
Camilleri M, Malagelada JR, Abell TL, et al. Effect of six weeks of treatment with cisapride in gastroparesis and intestinal pseudoobstruction. Gastroenterology 1989 Mar; 96(3): 704–12
Nosadini R, De Kreutzenberg S, Duner E, et al. Porcine and human insulin absorption from subcutaneous tissues in normal and insulin-dependent diabetic subjects: a deconvolution-based approach. J Clin Endocrinol Metab 1988; 67(3): 551–9
Moore EW, Mitchell ML, Chalmers TC. Variability in absorption of insulin-I 131 in normal and diabetic subjects after subcutaneous and intramuscular injection. J Clin Invest 1959 Jul; 38(7): 1222–7
Leinonen H, Matikainen E, Juntunen J. Permeability and morphology of skeletal muscle capillaries in type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1982 Mar; 22(3): 158–62
Weinstein L, Meade RH. Absorption and excretion of penicillin injected into the muscles of patients with diabetes mellitus. Nature 1961 Dec 9; 192: 987–8
Hildebrandt P, Sestoft L, Nielsen SL. The absorption of subcutaneously injected short-acting soluble insulin: influence of injection technique and concentration. Diabetes Care 1983 Sep–Oct; 6(5): 459–62
Sestoft L, Volund A, Gammeltoft S, et al. The biological properties of human insulin: subcutaneous absorption, receptor binding and the clinical effect in diabetics assessed by a new statistical method. Acta Med Scand 1982; 212(1–2): 21–8
Kolendorf K, Bojsen J, Nielsen SL. Adipose tissue blood flow and insulin disappearance from subcutaneous tissue. Clin Pharmacol Ther 1979 May; 25 (5 Pt 1): 598–604
Lauritzen T, Binder C, Faber OK. Importance of insulin absorption, subcutaneous blood flow, and residual beta-cell function in insulin therapy. Acta Paediatr Scand Suppl 1980; 283: 81–5
Haggendal E, Steen B, Svanborg A. Blood flow in subcutaneous fat tissue in patients with diabetes mellitus. Acta Med Scand 1970 Jan–Feb; 187(1–2): 49–53
Dimitriadis G, Lambadiari V, Mitrou P, et al. Impaired postprandial blood flow in adipose tissue may be an early marker of insulin resistance in type 2 diabetes. Diabetes Care 2007 Dec; 30(12): 3128–30
Coppack SW, Evans RD, Fisher RM, et al. Adipose tissue metabolism in obesity: lipase action in vivo before and after a mixed meal. Metabolism 1992 Mar; 41(3): 264–72
Blaak EE, van Baak MA, Kemerink GJ, et al. Beta-adrenergic stimulation and abdominal subcutaneous fat blood flow in lean, obese, and reduced-obese subjects. Metabolism 1995 Feb; 44(2): 183–7
Summers LK, Samra JS, Humphreys SM, et al. Subcutaneous abdominal adipose tissue blood flow: variation within and between subjects and relationship to obesity. Clin Sci (Lond) 1996 Dec; 91(6): 679–83
Jansson PA, Larsson A, Lonnroth PN. Relationship between blood pressure, metabolic variables and blood flow in obese subjects with or without non-insulin-dependent diabetes mellitus. Eur J Clin Invest 1998 Oct; 28(10): 813–8
Karpe F, Fielding BA, Ilic V, et al. Impaired postprandial adipose tissue blood flow response is related to aspects of insulin sensitivity. Diabetes 2002 Aug; 51(8): 2467–73
Regensteiner JG, Popylisen S, Bauer TA, et al. Oral L-arginine and vitamins E and C improve endothelial function in women with type 2 diabetes. Vasc Med 2003; 8(3): 169–75
Kingwell BA, Formosa M, Muhlmann M, et al. Type 2 diabetic individuals have impaired leg blood flow responses to exercise: role of endothelium-dependent vasodilation. Diabetes Care 2003 Mar; 26(3): 899–904
McVeigh GE, Brennan GM, Johnston GD, et al. Impaired endothelium-dependent and independent vasodilation in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1992 Aug; 35(8): 771–6
Williams SB, Cusco JA, Roddy MA, et al. Impaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 1996 Mar 1; 27(3): 567–74
Schneider JG, Tilly N, Hierl T, et al. Elevated plasma endothelin-1 levels in diabetes mellitus. Am J Hypertens 2002 Nov; 15(11): 967–72
Marin P, Andersson B, Krotkiewski M, et al. Muscle fiber composition and capillary density in women and men with NIDDM. Diabetes Care 1994 May; 17(5): 382–6
Mathieu-Costello O, Kong A, Ciaraldi TP, et al. Regulation of skeletal muscle morphology in type 2 diabetic subjects by troglitazone and metformin: relationship to glucose disposal. Metabolism 2003 May; 52(5): 540–6
Ritov VB, Menshikova EV, He J, et al. Deficiency of subsarcolemmal mitochondria in obesity and type 2 diabetes. Diabetes 2005 Jan; 54(1): 8–14
Kelley DE, He J, Menshikova EV, et al. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002 Oct; 51(10): 2944–50
Yee GC, Evans WE. Reappraisal of guidelines for pharmacokinetic monitoring of aminoglycosides. Pharmacotherapy 1981 Jul–Aug; 1(1): 55–75
Lerner PI, Weinstein L. Abnormalities of absorption of benzylpenicillin G and sulfisoxazole in patients with diabetes mellitus. Am J Med Sci 1964 Jul; 248:37–51
Bonadonna RC, Groop L, Kraemer N, et al. Obesity and insulin resistance in humans: a dose-response study. Metabolism 1990 May; 39(5): 452–9
Rexrode KM, Manson JE, Hennekens CH. Obesity and cardiovascular disease. Curr Opin Cardiol 1996 Sep; 11(5): 490–5
Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet 2010; 49(2): 71–87
Benedek IH, Fiske 3rd WD, Griffen WO, et al. Serum alpha 1-acid glycoprotein and the binding of drugs in obesity. Br J Clin Pharmacol 1983 Dec; 16(6): 751–4
Abernethy DR, Greenblatt DJ. Drug disposition in obese humans: an update. Clin Pharmacokinet 1986 May–Jun; 11(3): 199–213
Abernethy DR, Greenblatt DJ, Divoll M, et al. Enhanced glucuronide conjugation of drugs in obesity: studies of lorazepam, oxazepam, and acetaminophen. J Lab Clin Med 1983 Jun; 101(6): 873–80
Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity. Physiol Rev 2008 Apr; 88(2): 389–419
Cohen MP, Ziyadeh FN, Chen S. Amadori-modified glycated serum proteins and accelerated atherosclerosis in diabetes: pathogenic and therapeutic implications. J Lab Clin Med 2006 May; 147(5): 211–9
Day JF, Thorpe SR, Baynes JW. Nonenzymatically glucosylated albumin: in vitro preparation and isolation from normal human serum. J Biol Chem 1979 Feb 10; 254(3): 595–7
Adithan C, Danda D, Swaminathan RP, et al. Effect of diabetes mellitus on salivary paracetamol elimination. Clin Exp Pharmacol Physiol 1988 Jun; 15(6): 465–71
Daintith H, Stevenson IH, O’Malley K. Influence of diabetes mellitus on drug metabolism in man. Int J Clin Pharmacol Biopharm 1976 Jan; 13(1): 55–8
Salmela PI, Sotaniemi EA, Pelkonen RO. The evaluation of the drug-metabolizing capacity in patients with diabetes mellitus. Diabetes 1980 Oct; 29(10): 788–94
Murali KV, Adithan C, Shashindran CH, et al. Antipyrine metabolism in patients with diabetes mellitus. Clin Exp Pharmacol Physiol 1983 Jan–Feb; 10(1): 7–13
Pirttiaho HI, Salmela PI, Sotaniemi EA, et al. Drug metabolism in diabetic subjects with fatty livers. Br J Clin Pharmacol 1984 Dec; 18(6): 895–9
Narang AP, Dutta DV, Khare AK. Impairment of drug clearance in patients with diabetes mellitus & liver cirrhosis. Indian J Med Res 1987 Mar; 85: 321–5
Zysset T, Wietholtz H. Differential effect of type I and type II diabetes on antipyrine disposition in man. Eur J Clin Pharmacol 1988; 34(4): 369–75
Ruiz-Cabello F, Erill S. Abnormal serum protein binding of acidic drugs in diabetes mellitus. Clin Pharmacol Ther 1984 Nov; 36(5): 691–5
Worner W, Preissner A, Rietbrock N. Drug-protein binding kinetics in patients with type I diabetes. Eur J Clin Pharmacol 1992; 43(1): 97–100
Kearns GL, Kemp SF, Turley CP, et al. Protein binding of phenytoin and lidocaine in pediatric patients with type I diabetes mellitus. Dev Pharmacol Ther 1988; 11(1): 14–23
Kemp SF, Kearns GL, Turley CP. Alteration of phenytoin binding by glycosylation of albumin in IDDM. Diabetes 1987 Apr; 36(4): 505–9
Trovik TS, Jaeger R, Jorde R, et al. Plasma protein binding of catecholamines, prazosin and propranolol in diabetes mellitus. Eur J Clin Pharmacol 1992; 43(3): 265–8
Trovik TS, Jaeger R, Jorde R, et al. Reduced sensitivity to beta-adrenoceptor stimulation and blockade in insulin dependent diabetic patients with hypoglycaemia unawareness. Br J Clin Pharmacol 1994 Nov; 38(5): 427–32
Reidenberg MM, Drayer DE. Alteration of drug-protein binding in renal disease. Clin Pharmacokinet 1984 Jan; 9 Suppl. 1: 18–26
Keller F, Maiga M, Neumayer HH, et al. Pharmacokinetic effects of altered plasma protein binding of drugs in renal disease. Eur J Drug Metab Pharmacokinet 1984 Jul–Sep; 9(3): 275–82
Gatti G, Crema F, Attardo-Parrinello G, et al. Serum protein binding of phenytoin and valproic acid in insulin-dependent diabetes mellitus. Ther Drug Monit 1987 Dec; 9(4): 389–91
McNamara PJ, Blouin RA, Brazzell RK. The protein binding of phenytoin, propranolol, diazepam, and AL01576 (an aldose reductase inhibitor) in human and rat diabetic serum. Pharm Res 1988 May; 5(5): 261–5
Zini R, Riant P, Barre J, et al. Disease-induced variations in plasma protein levels. Implications for drug dosage regimens (part II). Clin Pharmacokinet 1990 Sep; 19(3): 218–29
Chase HP, Glasgow AM. Juvenile diabetes mellitus and serum lipids and lipoprotein levels. Am J Dis Child 1976 Oct; 130(10): 1113–7
Fraze E, Donner CC, Swislocki AL, et al. Ambient plasma free fatty acid concentrations in noninsulin-dependent diabetes mellitus: evidence for insulin resistance. J Clin Endocrinol Metab 1985 Nov; 61(5): 807–11
Grainger-Rousseau T, McElnay J, Collier P. The influence of disease on plasma protein binding of drugs. Int J Pharmacol 1989; 54: 1–13
O’Byrne S, Barry MG, Collins WC, et al. Plasma protein binding of lidocaine and warfarin in insulin-dependent and non-insulin-dependent diabetes mellitus. Clin Pharmacokinet 1993 Feb; 24(2): 183–6
Stafford WL. Abnormality in the binding of an organic anion by diabetic serum. Lancet 1962 Feb 3; 1(7223): 243–5
Saadeh S. Nonalcoholic Fatty liver disease and obesity. Nutr Clin Pract 2007 Feb; 22(1): 1–10
Ijaz S, Yang W, Winslet MC, et al. Impairment of hepatic microcirculation in fatty liver. Microcirculation 2003 Dec; 10(6): 447–56
Kotlyar M, Carson SW. Effects of obesity on the cytochrome P450 enzyme system. Int J Clin Pharmacol Ther 1999 Jan; 37(1): 8–19
Abernethy DR, Greenblatt DJ. Pharmacokinetics of drugs in obesity. Clin Pharmacokinet 1982 Mar–Apr; 7(2): 108–24
Petrides AS, Vogt C, Schulze-Berge D, et al. Pathogenesis of glucose intolerance and diabetes mellitus in cirrhosis. Hepatology 1994 Mar; 19(3): 616–27
Katbamma B, Petrelli M, McCullough A. The liver in diabetes mellitus and hyperlipidemia. In: Gitlin N, editor. The liver and the systemic disease. New York: Churchill Livingstone, 1997: 73–113
Wang T, Fontenot RD, Soni MG, et al. Enhanced hepatotoxicity and toxic outcome of thioacetamide in streptozotocin-induced diabetic rats. Toxicol Appl Pharmacol 2000 Jul 15; 166(2): 92–100
Watkins 3rd JB, Sherman SE. Long-term diabetes alters the hepatobiliary clearance of acetaminophen, bilirubin and digoxin. J Pharmacol Exp Ther 1992 Mar; 260(3): 1337–43
Shankar K, Vaidya VS, Apte UM, et al. Type 1 diabetic mice are protected from acetaminophen hepatotoxicity. Toxicol Sci 2003 Jun; 73(2): 220–34
Lee JH, Yang SH, Oh JM, et al. Pharmacokinetics of drugs in rats with diabetes mellitus induced by alloxan or streptozotocin: comparison with those in patients with type I diabetes mellitus. J Pharm Pharmacol 2010; 62(1): 1–23
Cheng PY, Morgan ET. Hepatic cytochrome P450 regulation in disease states. Curr Drug Metab 2001 Jun; 2(2): 165–83
Sotaniemi EA, Pelkonen O, Arranto AJ, et al. Diabetes and elimination of antipyrine in man: an analysis of 298 patients classified by type of diabetes, age, sex, duration of disease and liver involvement. Pharmacol Toxicol 2002 Mar; 90(3): 155–60
Lucas D, Farez C, Bardou LG, et al. Cytochrome P450 2E1 activity in diabetic and obese patients as assessed by chlorzoxazone hydroxylation. Fundam Clin Pharmacol 1998; 12(5): 553–8
Wang Z, Hall SD, Maya JF, et al. Diabetes mellitus increases the in vivo activity of cytochrome P450 2E1 in humans. Br J Clin Pharmacol 2003 Jan; 55(1): 77–85
Hannon-Fletcher MP, O’Kane MJ, Moles KW, et al. Lymphocyte cytochrome P450-CYP2E1 expression in human IDDM subjects. Food Chem Toxicol 2001 Feb; 39(2): 125–32
Haufroid V, Ligocka D, Buysschaert M, et al. Cytochrome P4502E1 (CYP2E1) expression in peripheral blood lymphocytes: evaluation in hepatitis C and diabetes. Eur J Clin Pharmacol 2003 May; 59(1): 29–33
Song BJ, Veech RL, Saenger P. Cytochrome P450IIE1 is elevated in lymphocytes from poorly controlled insulin-dependent diabetics. J Clin Endocrinol Metab 1990 Oct; 71(4): 1036–40
Pucci L, Chirulli V, Marini S, et al. Expression and activity of CYP2E1 in circulating lymphocytes are not altered in diabetic individuals. Pharmacol Res 2005 Jun; 51(6): 561–5
Adithan C, Sriram G, Swaminathan RP, et al. Effect of type II diabetes mellitus on theophylline elimination. Int J Clin Pharmacol Ther Toxicol 1989 May; 27(5): 258–60
Zysset T, Wietholtz H. Pharmacokinetics of caffeine in patients with decompensated type I and type II diabetes mellitus. Eur J Clin Pharmacol 1991; 41(5): 449–52
Matzke GR, Frye RF, Early JJ, et al. Evaluation of the influence of diabetes mellitus on antipyrine metabolism and CYP1A2 and CYP2D6 activity. Pharmacotherapy 2000 Feb; 20(2): 182–90
Korrapati MR, Vestal RE, Loi CM. Theophylline metabolism in healthy nonsmokers and in patients with insulin-dependent diabetes mellitus. Clin Pharmacol Ther 1995 Apr; 57(4): 413–8
Ueda H, Sakurai T, Ota M, et al. Disappearance rate of tolbutamide in normal subjects and in diabetes mellitus, liver cirrhosis, and renal disease. Diabetes 1963 Sep–Oct; 12: 414–9
Dyer JR, Davis TM, Giele C, et al. The pharmacokinetics and pharmacodynamics of quinine in the diabetic and non-diabetic elderly. Br J Clin Pharmacol 1994 Sep; 38(3): 205–12
Dostalek M, Court MH, Yan B, et al. Significantly reduced cytochrome P450 3A4 expression and activity in liver from humans with diabetes mellitus. Br J Pharmacol 2011 Jul; 163(5): 937–47
Marques MP, Coelho EB, Dos Santos NA, et al. Dynamic and kinetic disposition of nisoldipine enantiomers in hypertensive patients presenting with type-2 diabetes mellitus. Eur J Clin Pharmacol 2002 Dec; 58(9): 607–14
Moises EC, Duarte Lde B, Cavalli Rde C, et al. Pharmacokinetics of lidocaine and its metabolite in peridural anesthesia administered to pregnant women with gestational diabetes mellitus. Eur J Clin Pharmacol 2008 Dec; 64(12): 1189–96
McRobie DJ, Glover DD, Tracy TS. Effects of gestational and overt diabetes on human placental cytochromes P450 and glutathione S-transferase. Drug Metab Dispos 1998 Apr; 26(4): 367–71
McRobie DJ, Korzekwa KR, Glover DD, et al. The effects of diabetes on placental aromatase activity. J Steroid Biochem Mol Biol 1997 Sep–Oct; 63(1–3): 147–53
Juan D, Molitch ME, Johnson MK, et al. Unaltered drug metabolizing enzyme systems in type II diabetes mellitus before and during glyburide therapy. J Clin Pharmacol 1990 Oct; 30(10): 943–7
West IC. Radicals and oxidative stress in diabetes. Diabet Med 2000 Mar; 17(3): 171–80
Atalay M, Laaksonen DE, Niskanen L, et al. Altered antioxidant enzyme defences in insulin-dependent diabetic men with increased resting and exercise-induced oxidative stress. Acta Physiol Scand 1997 Oct; 161(2): 195–201
Dincer Y, Alademir Z, Ilkova H, et al. Susceptibility of glutatione and glutathione-related antioxidant activity to hydrogen peroxide in patients with type 2 diabetes: effect of glycemic control. Clin Biochem 2002 Jun; 35(4): 297–301
Graber R, Farine JC, Fumagalli I, et al. Apoptosis and oxidative status in peripheral blood mononuclear cells of diabetic patients. Apoptosis 1999 Aug; 4(4): 263–70
Sailaja YR, Baskar R, Saralakumari D. The antioxidant status during maturation of reticulocytes to erythrocytes in type 2 diabetics. Free Radic Biol Med 2003 Jul 15; 35(2): 133–9
Albrecht C, Simon-Vermot I, Elliott JI, et al. Leukocyte ABCA1 gene expression is associated with fasting glucose concentration in normoglycemic men. Metabolism 2004 Jan; 53(1): 17–21
Zhou H, Tan KC, Shiu SW, et al. Determinants of leukocyte adenosine triphosphate-binding cassette transporter G1 gene expression in type 2 diabetes mellitus. Metabolism 2008 Aug; 57(8): 1135–40
Mauldin JP, Nagelin MH, Wojcik AJ, et al. Reduced expression of ATP-binding cassette transporter G1 increases cholesterol accumulation in macrophages of patients with type 2 diabetes mellitus. Circulation 2008 May 27; 117(21): 2785–92
Blouin RA, Warren GW. Pharmacokinetic considerations in obesity. J Pharm Sci 1999 Jan; 88(1): 1–7
Suzuki Y, Arakawa M. The treatment of the uraemic diabetic. Are we doing enough? A view from Japan. Fumitake Gejyo and Collaborate Study Group. Nephrol Dial Transplant 1995; 10 Suppl. 7: 47–55
Raine AE. The rising tide of diabetic nephropathy: the warning before the flood? Nephrol Dial Transplant 1995; 10(4): 460–1
Andersen AR, Christiansen JS, Andersen JK, et al. Diabetic nephropathy in type 1 (insulin-dependent) diabetes: an epidemiological study. Diabetologia 1983 Dec; 25(6): 496–501
Sasso FC, De Nicola L, Carbonara O, et al. Cardiovascular risk factors and disease management in type 2 diabetic patients with diabetic nephropathy. Diabetes Care 2006 Mar; 29(3): 498–503
Hasslacher C, Kempe HP, Bostedt-Kiesel A. ACE inhibitors and diabetic nephropathy: clinical and experimental findings. Clin Investig 1993; 71 (5 Suppl.): S20–4
Ebihara I, Nakamura T, Shimada N, et al. Increased plasma metalloproteinase-9 concentrations precede development of microalbuminuria in non-insulin-dependent diabetes mellitus. Am J Kidney Dis 1998 Oct; 32(4): 544–50
Ravid M, Lang R, Rachmani R, et al. Long-term renoprotective effect of angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus: a 7-year follow-up study. Arch Intern Med 1996 Feb 12; 156(3): 286–9
Ahmad J, Siddiqui MA, Ahmad H. Effective postponement of diabetic nephropathy with enalapril in normotensive type 2 diabetic patients with microalbuminuria. Diabetes Care 1997 Oct; 20(10): 1576–81
Gill GV, Hardy KJ, Patrick AW, et al. Random blood glucose estimation in type 2 diabetes: does it reflect overall glycaemic control? Diabet Med 1994 Aug–Sep; 11(7): 705–8
Meeme A, Kasozi H. Effect of glycaemic control on glomerular filtration rate in diabetes mellitus patients. Afr Health Sci 2009 Aug 1; 9 Suppl. 1: S23–6
Maurer AC. The therapy of diabetes. Am Sci 1979 Jul–Aug; 67(4): 422–31
Madacsy L, Bokor M, Matusovits L. Penicillin clearance in diabetic children. Acta Paediatr Acad Sci Hung 1975; 16(2): 139–42
Garcia G, de Vidal EL, Trujillo H. Serum levels and urinary concentrations of kanamicin, bekanamicin and amikacin (BB-K8) in diabetic children and a control group. J Int Med Res 1977; 5(5): 322–9
Graham DJ, Staffa JA, Shatin D, et al. Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs. JAMA 2004 Dec 1; 292(21): 2585–90
Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004 Aug 21–27; 364(9435): 685–96
Skottheim IB, Gedde-Dahl A, Hejazifar S, et al. Statin induced myotoxicity: the lactone forms are more potent than the acid forms in human skeletal muscle cells in vitro. Eur J Pharm Sci 2008 Apr 23; 33(4–5): 317–25
Berlin I, Grimaldi A, Bosquet F, et al. Decreased beta-adrenergic sensitivity in insulin-dependent diabetic subjects. J Clin Endocrinol Metab 1986 Jul; 63(1): 262–5
Lloyd-Mostyn RH, Watkins PJ. Defective innervation of heart in diabetic autonomic neuropathy. Br Med J 1975 Jul 5; 3(5974): 15–7
Berlin I, Grimaldi A, Landault C, et al. Lack of hypoglycemic symptoms and decreased beta-adrenergic sensitivity in insulin-dependent diabetic patients. J Clin Endocrinol Metab 1988 Feb; 66(2): 273–8
Berlin I, Grimaldi A, Payan C, et al. Hypoglycemic symptoms and decreased beta-adrenergic sensitivity in insulin-dependent diabetic patients. Diabetes Care 1987 Nov–Dec; 10(6): 742–7
Lynch C, Exton J. Alterations in G-protein-mediated cell signaling in diabetes mellitus. In: Milligan G, Wakelam M, editors. G-proteins: signal transduction and disease. London: Academic Press Limited, 1992: 87–108
Terada M, Yasuda H, Kashawagi A, et al. Sympathetic nerve dysfunction and increased heart rate response to epinephrine in diabetic patients. Amsterdam: Elsevier Science Publishers, 1987
Packer M, Lee WH, Medina N, et al. Influence of diabetes mellitus on changes in left ventricular performance and renal function produced by converting enzyme inhibition in patients with severe chronic heart failure. Am J Med 1987 Jun; 82(6): 1119–26
Self TH, Hood J, Miller ST. Diabetes mellitus and the hypoprothrombinemic response to warfarin [letter]. JAMA 1978 May 26; 239(21): 2239
Lansang MC, Ma L, Schold JD, et al. The relationship between diabetes and infectious hospitalizations in renal transplant recipients. Diabetes Care 2006 Jul; 29(7): 1659–60
First MR. Posttransplant diabetes mellitus [letter]. Transplantation 2003 May 27; 75(10): 1769
Kasiske BL, Snyder JJ, Gilbertson D, et al. Diabetes mellitus after kidney transplantation in the United States. Am J Transplant 2003 Feb; 3(2): 178–85
Ye X, Kuo HT, Sampaio MS, et al. Risk factors for development of new-onset diabetes mellitus after transplant in adult lung transplant recipients. Clin Transplant 2011; 25(6): 885–91
Mendonza AE, Gohh RY, Akhlaghi F. Blood and plasma pharmacokinetics of ciclosporin in diabetic kidney transplant recipients. Clin Pharmacokinet 2008; 47(11): 733–42
Akhlaghi F, Dostalek M, Falck P, et al. The concentration of cyclosporine metabolites is significantly lower in kidney transplant recipients with diabetes mellitus. Ther Drug Monit 2012; 34(1): 38–45
Mendonza AE, Zahir H, Gohh RY, et al. Tacrolimus in diabetic kidney transplant recipients: pharmacokinetics and application of a limited sampling strategy. Ther Drug Monit 2007 Aug; 29(4): 391–8
van Duijnhoven E, Christiaans M, Undre N, et al. The effect of breakfast on the oral bioavailability of tacrolimus in diabetic and nondiabetic patients before transplantation. Transplant Proc 1998 Jun; 30(4): 1268–70
Akhlaghi F, Patel CG, Zuniga XP, et al. Pharmacokinetics of mycophenolic acid and metabolites in diabetic kidney transplant recipients. Ther Drug Monit 2006 Feb; 28(1): 95–101
van Hest RM, Mathot RA, Vulto AG, et al. Mycophenolic acid in diabetic renal transplant recipients: pharmacokinetics and application of a limited sampling strategy. Ther Drug Monit 2004 Dec; 26(6): 620–5
Pescovitz MD, Guasch A, Gaston R, et al. Equivalent pharmacokinetics of mycophenolate mofetil in African-American and Caucasian male and female stable renal allograft recipients. Am J Transplant 2003 Dec; 3(12): 1581–6
Akhlaghi F, Dostalek M, Mendonza AE, et al. Reduced levels of biomarkers of immunosuppressive activity in diabetic kidney transplant recipients [poster no. P204]. International Association of Therapeutic Drug Monitoring and Clinical Toxicology; 2011 Oct 2–6; Stuttgart, Germany
Akhlaghi F, Chitnis SD, Ionita I, et al. Impact of diabetes mellitus on metabolism of immunosuppressive agents: cyclosporin, tacrolimus and prednisone [poster no. P201]. International Association of Therapeutic Drug Monitoring and Clinical Toxicology; 2011 Oct 2–6; Stuttgart, Germany
Bertoni AG, Saydah S, Brancati FL. Diabetes and the risk of infection-related mortality in the U.S. Diabetes Care 2001 Jun; 24(6): 1044–9
Alba-Loureiro TC, Munhoz CD, Martins JO, et al. Neutrophil function and metabolism in individuals with diabetes mellitus. Braz J Med Biol Res 2007 Aug; 40(8): 1037–44
Jolin T, Tarin MJ, Garcia MD. Induction of goitre by PTU or KCIO4 in male and female rats: effect of gonadectomy. Acta Endocrinol (Copenh) 1973 Sep; 74(1): 88–104
Garcia-Leme J, Bohm GM, Migliorini RH, et al. Possible participation of insulin in the control of vascular permeability. Eur J Pharmacol 1974 Dec; 29(2): 298–306
Llorach MA, Bohm GM, Leme JG. Decreased vascular reactions to permeability factors in experimental diabetes. Br J Exp Pathol 1976 Dec; 57(6): 747–54
Fortes ZB, Garcia Leme J, Scivoletto R. Vascular reactivity in diabetes mellitus: role of the endothelial cell. Br J Pharmacol 1983 Jul; 79(3): 771–81
Fortes ZB, Garcia Leme J, Scivoletto R. Vascular reactivity in diabetes mellitus: possible role of insulin on the endothelial cell. Br J Pharmacol 1984 Nov; 83(3): 635–43
Cavalher-Machado SC, de Lima WT, Damazo AS, et al. Down-regulation of mast cell activation and airway reactivity in diabetic rats: role of insulin. Eur Respir J 2004 Oct; 24(4): 552–8
Sannomiya P, Pereira MA, Garcia-Leme J. Inhibition of leukocyte chemotaxis by serum factor in diabetes mellitus: selective depression of cell responses mediated by complement-derived chemoattractants. Agents Actions 1990 Jun; 30(3–4): 369–76
Sannomiya P, Oliveira MA, Fortes ZB. Aminoguanidine and the prevention of leukocyte dysfunction in diabetes mellitus: a direct vital microscopic study. Br J Pharmacol 1997 Nov; 122(5): 894–8
Fortes ZB, Farsky SP, Oliveira MA, et al. Direct vital microscopic study of defective leukocyte-endothelial interaction in diabetes mellitus. Diabetes 1991 Oct; 40(10): 1267–73
Cruz JW, Oliveira MA, Hohman TC, et al. Influence of tolrestat on the defective leukocyte-endothelial interaction in experimental diabetes. Eur J Pharmacol 2000 Mar 10; 391(1–2): 163–74
Zanardo RC, Cruz JW, Martinez LL, et al. Probucol restores the defective leukocyte-endothelial interaction in experimental diabetes. Eur J Pharmacol 2003 Oct 8; 478(2–3): 211–9
Anjos-Valotta EA, Martins JO, Oliveira MA, et al. Inhibition of tumor necrosis factor-alpha-induced intercellular adhesion molecule-1 expression in diabetic rats: role of insulin. Inflamm Res 2006 Jan; 55(1): 16–22
Moriguchi P, Sannomiya P, Lara PF, et al. Lymphatic system changes in diabetes mellitus: role of insulin and hyperglycemia. Diabetes Metab Res Rev 2005; 21(2): 150–7
Boichot E, Sannomiya P, Escofier N, et al. Endotoxin-induced acute lung injury in rats: role of insulin. Pulm Pharmacol Ther 1999; 12(5): 285–90
Shaw LM, Figurski M, Milone MC, et al. Therapeutic drug monitoring of mycophenolic acid. Clin J Am Soc Nephrol 2007 Sep; 2(5): 1062–72
Patel CG, Richman K, Yang D, et al. Effect of diabetes mellitus on mycophenolate sodium pharmacokinetics and inosine monophosphate dehydrogenase activity in stable kidney transplant recipients. Ther Drug Monit 2007 Dec; 29(6): 735–42
Jain J, Almquist SJ, Ford PJ, et al. Regulation of inosine monophosphate dehydrogenase type I and type II isoforms in human lymphocytes. Biochem Pharmacol 2004 Feb 15; 67(4): 767–76
Fulton B, Markham A. Mycophenolate mofetil: a review of its pharmaco-dynamic and pharmacokinetic properties and clinical efficacy in renal transplantation. Drugs 1996 Feb; 51(2): 278–98
Abbott KC, Hypolite I, Poropatich RK, et al. Hospitalizations for fungal infections after renal transplantation in the United States. Transpl Infect Dis 2001 Dec; 3(4): 203–11
Dharnidharka VR, Agodoa LY, Abbott KC. Risk factors for hospitalization for bacterial or viral infection in renal transplant recipients: an analysis of USRDS data. Am J Transplant 2007 Mar; 7(3): 653–61
Redman DR, Prescott LF. Failure of induction of liver microsomal enzymes by tolbutamide in maturity-onset diabetics. Diabetes 1973 Mar; 22(3): 210–1
Sambol NC, Chiang J, O’Conner M, et al. Pharmacokinetics and pharmaco-dynamics of metformin in healthy subjects and patients with noninsulin-dependent diabetes mellitus. J Clin Pharmacol 1996 Nov; 36(11): 1012–21
Plosker GL, Figgitt DP. Repaglinide: a pharmacoeconomic review of its use in type 2 diabetes mellitus. Pharmacoeconomics 2004; 22(6): 389–411
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dostalek, M., Akhlaghi, F. & Puzanovova, M. Effect of Diabetes Mellitus on Pharmacokinetic and Pharmacodynamic Properties of Drugs. Clin Pharmacokinet 51, 481–499 (2012). https://doi.org/10.1007/BF03261926
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03261926