Abstract
Goto-Kakizaki (GK) rats represent a unique non-obese and lean model with manifestation of type 2 diabetes (T2DM) broadly mimicking the human T2DM development. Therefore, in addition to the use of GK rats to test the efficacy of drugs, it may represent a great tool to study the influence of altered physiological process and/or organ specific pathophysiological changes (i.e., liver, kidney, etc.) on the disposition of drugs. The objectives of the review were: (a) to compile the published pharmacokinetic data of several drugs, such as cephalexin, cyclosporine, exendin-4, gliclazide, grepafloxacin, rosuvastatin, salsalate, salicylic acid, and theophylline, in GK rats relative to normal rats; and (b) critically evaluate the possible role of physiologically altered processes on the pharmacokinetics of reviewed drugs. The drugs chosen for this review provided a spread of various physiological processes and represented reasonable pool of published data set to fulfil the objectives of the review. The use of GK rats for gathering pharmacokinetic data may aid in making decisions on candidate selection and/or anticipating clinical pharmacology-related issues to the aid drug development in the diabetes area. However, given the interplay and complexities of multiple pathways governing drug disposition, caution needs to be exercised in data interpretation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The lineage of Goto-Kakizaki (GK) rats from a selective in-breeding of Wistar rats has resulted in the availability of lean and non-obese model that exhibits spontaneous type 2 diabetes mellitus (T2DM). |
In addition to its use as a pharmacological model for T2DM, GK rats may serve as a great tool to understand if physiological and/or pathophysiological changes would alter the pharmacokinetics of drugs. |
The examination of several drugs in this review has suggested that GK rats can provide useful information relating to absorption, metabolism, and/or excretory process of drugs in T2DM. |
GK rats may be effectively used during drug discovery and development process for making decision in candidate selection and/or assessing risks in clinical pharmacology area. |
1 Introduction
The failure of endocrine pancreas to produce enough insulin to meet the high demand for glucose metabolism is attributable to various physiological reasons, such as the impairment of pancreatic beta-cell secretory process and decreased beta-cell mass over time [1–4]. Moreover, lack of insulin sensitization (i.e., insulin resistance) may also hamper the metabolic process, despite the availability and/or production of blood insulin [1–4]. The combinations of the various physiological and pathophysiological conditions through multi-faceted mechanisms in totality contribute for the occurrence of type 2 diabetes mellitus (T2DM) in humans [1–4]. Goto-Kakizaki (GK) rats, a non-obese phenotype, are well accepted and adequately characterized rodent model to study the different aspects of T2DM, as it relates to both physiological and pathophysiological changes, as a consequence of the disease [5–9]. The lineage of GK rats was as a result of a selective in-breeding of regular Wistar rats utilizing glucose intolerance as the key criteria for the selection of spontaneous type II diabetes mellitus [10, 11]. GK rats have been used as a tool to study the human T2DM, since in this genetic model, fasting hyperglycaemia was evident generally after a few weeks of the birth of the animals [12]. In addition, because of the slow progress of the disease in GK rats, it is more preferred, unlike its obese counterpart exhibiting T2DM, where manifestation of severe hyperlipidaemia and hyperglycaemia is very rapid [12]. This aspect of T2DM development in GK rats appears to mimic the human situation, where the patient suffers from hyperinsulinemia for a considerable duration of time prior to exhibiting hyperglycaemic state.
Because of the commonalities existing in the onset and progression of T2DM between GK rats and humans, GK rats provide an interesting opportunity to study the influence of the disease state on the pharmacokinetics and drug disposition of various drugs. Such pharmacokinetic data gathered in GK rats may render itself useful for either candidate selection in a drug discovery program and/or identifying a priori the developmental challenges from a clinical pharmacology perspective as a result of altered absorption, metabolism, and/or excretion.
2 Scope
The main objective of this review is to examine individual case studies and collate the pharmacokinetic data of several drugs which have been delineated in GK rats relative to control rats with the purpose of ascertaining the intended interaction is absorption, metabolism, and/or elimination process, as a result of the disease condition. The selected drugs in this review, such as cephalexin, cyclosporine, exendin-4, gliclazide, grepafloxacin, rosuvastatin, salsalate, salicylic acid, and theophylline, not only provide diversity in the chemical structures but also represent case studies for the various pharmacokinetic processes which determine drug bioavailability, disposition, and/or elimination from the body. The selection of the chosen drugs in this review was made by PubMed® database search using key words Goto-Kakizaki rats and pharmacokinetics. Table 1 provides a summary of the pathway(s) investigated in each case study for the potential for any altered pharmacokinetics along with the relevant pharmacokinetic data and key conclusive remarks for various drugs [13–21].
3 Case Studies
3.1 Cephalexin
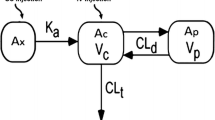
Cephalexin is a beta-lactam antibiotic and being an oligopeptidic drug the intestinal absorption of cephalexin has been suggested to be governed by intestinal peptide carrier-mediated transport system (H+/Oligopeptide transporter) [22, 23]. The delineation of pharmacokinetic data via the influence of PEPT1 transporter has been established in rats with appropriate study design that included quinapril for the inhibition of oligopeptide transporter [24]. Watanabe et al. designed an in vivo study to understand the influence of diabetes disease state on the absorption and pharmacokinetics of cephalexin. In addition, in situ and ex vivo work was carried out to establish the mechanistic aspects to possibly explain the altered pharmacokinetics of cephalexin [13]. The in situ absorption study showed that maximum disappearance of cephalexin occurred in GK rats relative to normal rats in the duodenum loop, whereas the disappearance from both jejunum and ileum loops were similar between GK and normal rats [13]. Regardless of the three intestinal loops, the expression of PEPT1 protein levels was significantly higher (p < 0.05) in GK rats relative to normal rats. Both these findings correlated well with the in vivo pharmacokinetic data of cephalexin in the GK rats relative to normal rats. Because of higher PEPT1 protein expression, absorption rate constant (K a) for cephalexin was about 1.5-fold greater in GK rats relative to normal rats. Furthermore, the T max was also significantly (p < 0.05) shorter in GK rats relative to normal rats, suggesting the important role of PEPT1 transporters in duodenum resulting in a rapid absorption of cephalexin.
3.2 Cyclosporine
Cyclosporine is a widely used immunosuppressive drug, whose absorption is governed by P-glycoprotein (Pgp) efflux mechanism [25]. A previous study performed in streptozotocin-treated diabetic rats suggested an increased intestinal absorption and elevated lymphatic concentrations of cyclosporine [26]. Therefore, Ogata et al. designed a study to understand if such a phenomenon that was observed previously with cyclosporine occurred in GK rats [14]. The inclusion of both oral and intravenous treatment groups provided clarity for the observation of oral-related phenomenon, such as absorption and oral bioavailability, without confounding factors. The use of propylene glycol solution of Na 512 CrO4 in a separate group of GK rats and normal rats enabled the tracking of gastrointestinal motility and the rate of gastric emptying between the two groups of rats [14]. The intravenous data observed for cyclosporine showed comparable plasma concentration vs. time profiles between GK rats and normal rats, suggesting that disposition, including elimination phases, was similar [14]. However, the oral absorption of cyclosporine was significantly (p < 0.05) affected, such that oral concentration data of cyclosporine was very low resulting in an almost 5.7-fold lower oral bioavailability in GK rats relative to normal rats. The subdued absorption of cyclosporine in GK rats was apparent from the first time point itself and continued to manifest during the study duration [14]. In a similar fashion, the lymphatic transport of cyclosporine was affected after oral dosing but not after intravenous dosing of the drug in GK rats relative to normal rats [14]. The lower oral absorption of cyclosporine was complemented by the radio tracer Na 512 CrO4 data obtained from the various intestinal segments of GK rats. While the tracer appeared to undergo rapid gastric emptying followed by a quick transit in normal rats, the transit as well as gastric emptying was impaired in the GK rats [14].
3.3 Exendin-4
Exendin-4 is a GLP analogue which has a longer half-life than the native GLP and shown to exhibit glycaemic control. Recently, Gao and Jusko developed a pharmacokinetic-pharmacodynamic model to describe the disposition of exendin-4 along with the effects on both insulin and glucose homeostasis in GK rats [15]. The data input into this model came from several intravenous doses and a subcutaneous dose of exendin-4. From the interest of this review, this report answered a very important question regarding the renal elimination of exendin-4 [15]. Because exendin-4 is predominantly excreted by the kidneys via glomerular filtration pathway [27], it was important to address whether or not GK rats had an impaired renal excretion of exendin-4. The model data from this study suggested that GK rats had similar renal function as compared with normal rats, and therefore, the renal clearance of exendin-4 was expected to be comparable between GK rats and normal rats [15, 16].
3.4 Gliclazide
Gliclazide, a sulphonylurea drug, is used in glucose control, and there was a report which suggested that glucose lowering effect was further potentiated when oral antidiabetic drugs, such as gliclazide, were coadministered with angiotensin converting enzyme (ACE) inhibitor [28]. Iso-Mustajarvi et al. performed an interesting study to investigate the pharmacokinetics of gliclazide in GK rats when given alone and in combination with an ACE inhibitor drug, fosinopril, both after oral and intravenous dosing [17]. After the intravenous administration, the elimination of gliclazide appeared to be slower in GK rats relative to normal rats leading to higher exposure values. The oral absorption of gliclazide in GK rats tended to be more protracted but showed increased absorption relative to normal rats, and the elimination phase was slower resulting in a higher bioavailability in GK rats relative to normal rats [17]. The presence of fosinopril did not alter the pharmacokinetics of gliclazide after intravenous administration when the two drugs were administered together. Similarly, although there appeared to be secondary absorption peaks of gliclazide after oral dosing of the two drugs, the overall pharmacokinetics of gliclazide were comparable with and without fosinopril [17]. It was concluded that there was no pharmacokinetic basis to explain the potentiation of the glycaemic control of gliclazide when administered with fosinopril [17].
3.5 Grepafloxacin
Grepafloxacin is a broad spectrum antibiotic, whose absorption is mechanistically governed by the Pgp efflux mechanisms in the small intestine [29] and excess secretion of grepafloxacin back into the intestinal lumen reduced the oral bioavailability of the drug [30]. Watanabe et al. explored the pharmacokinetics of grepafloxacin following intravenous and intra-intestinal dosing in GK rats relative to normal rats to understand the possible role of disease state in altering the pharmacokinetics of grepafloxacin [18]. The intravenous pharmacokinetics of grepafloxacin was similar between GK rats and normal rats, suggesting that metabolism and elimination aspects of the disposition of grepafloxacin were not changed due to T2DM. However, after oral dosing, there appeared to be significant differences in the plasma concentration time profiles, particularly at 1.5, 2, and 4 h post-dosing, where higher plasma concentrations of grepafloxacin were observed in GK rats as compared with normal rats [18]. The simultaneous mechanistic in vitro work deduced that jejunal clearance of grepafloxacin was decreased in GK rats relative to control, and therefore, as a consequence of decreased secretory transport of grepafloxacin, there was a higher plasma concentration of grepafloxacin achieved after intra-intestinal dosing. However, there was a paradoxical observation when the Pgp mRNA protein expression was assessed in the jejunal region of the GK rats, which was found to be higher than those observed for normal rats [18]. While the inconsistency of the secretory transport activity vs. protein expression needs to be further investigated, the data from this study suggested that in GK rats, there was increased bioavailability of grepafloxacin due to reduced secretory transport after intra-intestinal dosing [18]. It is important to note that in rats with streptozotocin-induced diabetes (STZ model), Pgp expression was reduced [31].
3.6 Rosuvastatin
Rosuvastatin a lipid lowering agent is a substrate to breast cancer resistance protein (BCRP) which controls both oral bioavailability and biliary excretory process [32, 33]. Because, in diabetic, conditions may impact the expression of hepatic BCRP, He et al. performed an interesting study in diabetic rat models involving both type 1 diabetes mellitus (i.e., STZ rats) and T2DM (GK rats) [19]. In this study, the mean exposure of rosuvastatin in GK rats appeared to decrease numerically by approximately 18 % as compared with normal rats and this was supported by an approximately 1.2-fold increase in the clearance of rosuvastatin in GK relative to normal rats [19]. However, the numerical change in the corresponding parameter values for rosuvastatin was statistically not significant [19]. In contrast, STZ rats showed a different and distinct pharmacokinetic profile, where the mean exposure of rosuvastatin was increased by approximately 3.2-fold with a concomitant 3-fold reduced clearance of rosuvastatin relative to normal rats [19]. The differential in vivo pharmacokinetics of rosuvastatin in the two diabetes rat models was explained by the examination of various efflux proteins expressions and function in this study [19]. In STZ rats, it was found that MRP2 expression decreased, but BCRP expression increased considerably. In GK rats, however, MRP2 expression increased, but the BCRP expression largely remained unchanged. While there was an inconsistency between the BCRP expression and functional activity as observed with increased plasma concentrations in STZ rats, there was much needed clarity that negligible changes in the pharmacokinetics of rosuvastatin in GK rats as compared with normal rats were as a result of minimal changes in the expression levels of efflux transporters via MRP2 but not with BCRP [19]. The protein expression level of MRP2 slightly increased in GK rats which may have contributed for the observed minor reduction in the exposure of rosuvastatin in GK rats relative to normal rats [19]. However, if one examined the mRNA expression in GK rats, it was found that BCRP mRNA expression was markedly increased and that of the MRP2 was reduced [19]. In addition, the lack of inclusion of an oral dosing of rosuvastatin in this study in either of the two diabetic rat models may have limited the usefulness of this study from judging the expression and functional activity of BCRP at the intestine level which primarily governs the absorption and bioavailability of rosuvastatin [19].
3.7 Salsalate and salicylic acid
Salsalate which is a dimer of salicylic acid has been in therapy for decades for its analgesic and anti-inflammatory properties [34]. The beneficial effects of salsalate exerted in patients with diabetes with respect to glucose, lipid, and free fatty acid modulation due to anti-inflammatory mechanisms of salsalate have been documented [35, 36]. Cao et al. designed a study to explore the pharmacokinetics of salsalate and salicylic acid in GK rats relative to normal rats [20], because it was postulated that non-linear clearance, altered renal function, and the protein status may possibly influence the disposition of salsalate in diabetic conditions. In one portion of the study, which was part of longitudinal investigation (5–19 weeks), where both pharmacokinetics and pharmacodynamic aspects of salsalate and salicylic acid were determined, the administration of salsalate and salicylic acid was via diet feeding to GK rats [20]. From the pharmacokinetic model approach to fit the steady-state pharmacokinetic data in GK rats, it was deduced that it was a slow absorption process with a sustained hydrolysis of salsalate to salicylic acid. The absence of salsalate in the circulation of GK rats suggested that salsalate would have been effectively converted to salicylic acid. Because it was a longitudinal study, it was found that apparent clearance increased over time for both GK rats and normal rats; however, GK rats showed higher increase in the apparent clearance as compared with normal rats during any paired comparison in the longitudinal study [20]. However, at the end of the 19 week study, it appeared that the apparent clearance of salicylic acid in GK rats was slightly higher than the normal rats.
3.8 Theophylline
Theophylline used extensively in respiratory disorders undergoes hepatic metabolism via CYP1A2 and shown to exhibit non-linearity in its disposition [37]. Takahashi et al. designed a study to understand the role of diabetes on the pharmacokinetic disposition of theophylline using both STZ rats and GK rats relative to normal rats [21]. After intravenous dosing of theophylline, the plasma concentration vs time profile observed in STZ rats was overlapping with that of normal rats; however, GK rats showed that a distinct profile posts the initial distribution phase, suggesting that theophylline hepatic metabolism may have been decreased in GK rats. This resulted in an almost twofold lower clearance in GK rats relative to normal rats [21]. After oral dosing, it was observed that both STZ rats and normal rats exhibited similar pharmacokinetics. Although GK rats showed somewhat slower absorption rate and protracted absorption, the exposure appeared to be comparable with that observed for normal rats [21]. However, the bioavailability of theophylline in GK rats was lower approximately lower by 28 % as compared with normal rats, suggesting that the complete absorption may have been hindered in GK rats [21].
4 Discussion
This is the first report that has examined and collated the pharmacokinetics of several drugs in GK rats, a lean and non-obese model of T2DM. Due to the altered physiological process and/or disease modified pathophysiological changes in T2DM, the pharmacokinetics of drugs may be altered and this may have implications in the therapy from a dosage adjustment point of view to ensure efficacy and safety of the drug in question is not compromised. In conjunction with a previously published review in chemically induced diabetic rats [38], the present compiled data provide an understanding of the complex interplay of pharmacokinetic processes in diabetes, either naturally occurring or chemically induced.
One of the distinct advantages of chemically induced model of diabetes is relatively faster onset of diabetes; however, with the caveat that they are more representative of type 1 diabetes model [38]. Because the models provide a rapid onset of diabetes, the physiological and physical stresses on the animals should be factored in the interpretation of the pharmacokinetic data of the coadministered drugs. As the experiments are typically done within 5 to 7 days after the chemical induction of diabetes, the pharmacokinetic data may not be truly reflecting the altered disposition of the drugs due to full blown diabetes, especially on renal excretory pathway [38]. Interestingly, chemically induced models of diabetes have been shown to influence absorption, distribution, metabolism, and excretion of the coadministered drugs, suggesting that the impairment of various physiological processes need to be factored in patients with T2DM. Because of the rapid development of diabetes in chemically induced models, it may be speculated that certain physiological functioning especially those of cytochrome P450 enzymes and/or transporters may be more exaggerated in chemically induced models of diabetes as compared with GK rats.
Unlike chemically induced diabetic rats, GK rats provide a different model, where the progression of diabetes is not just spontaneous and as well as it provides a basis to study the disposition effects of coadministered drugs in non-obese/lean phenotype of the diabetes, which is prevalent in many T2DM patients. In the drug development, it is important to collect and collate data from various experimental designs to make an informed decision on the candidate considered for the clinical development. Hence, both GK rats and chemically induced diabetes models serve as important tools for evaluation of drug candidates to anticipate and/or prepare for potential drug–drug interaction issues in the clinic.
4.1 Absorption
The retardation of gastrointestinal motility and gastric emptying time in GK rats may have consequences in the drug absorption of drugs as exemplified by the case studies of cyclosporine, gliclazide, salsalate, salicylic acid, and theophylline [14, 17, 20, 21]. In all the cases, a reduced or prolonged oral absorption and decreased oral exposure/bioavailability were reported. It is important to critically evaluate, each example, to understand the possible underlying mechanism(s) for the altered pharmacokinetics. First, with cyclosporine, a longer gastric retention of the drug would render cyclosporine amenable for metabolism via intestinal CYP3A4 and as well as render it for efflux mechanism via Pgp [25]. Second, with gliclazide, there was a protracted oral absorption of the drug; although the prolonged nature of absorption, it did not appear to affect the oral bioavailability of gliclazide, it may lead to secondary peaks and inconsistent surges in the plasma concentrations of gliclazide which may lead to unsuspected hypoglycaemic episodes [17]. Third, with the example of salsalate, a dimer of salicylic acid, it appeared that reduced gastric transit significantly limited the oral absorption of salicylic acid [20]. However, a complete conversion of salsalate to salicylic acid was presumed due to the lack of the presence of circulatory salsalate in the plasma of GK rats. It may be additionally speculated that salicylic acid may have a specific window for absorption in the gastrointestinal tract, and/or efflux mechanisms may have also hindered the absorption. Finally, with theophylline, there was slower and lower absorption of the drug in GK rats due to impaired gastrointestinal motility. As a corollary, a recently published article has reviewed the issues of gastric motility associated with diabetes in human patients [39]. Because of the retardation of gastric motility and gastric emptying time due to diabetes, certain acute therapies for managing pain and/or nausea should be done with caution in T2DM patients. In addition, accompanying medications for hypoglycaemic control, such as GLP-1 analogues, may further retard the gastric emptying in diabetic patients [40] and this may result in a complex interplay of various factors to understand the oral absorption of other drugs in T2DM patients.
4.2 Efflux and Transporters
With regard to the effect of Pgp expression and functional activity in GK rats, the case study of grepafloxacin was somewhat difficult to interpret [18]. On one hand, the increased Pgp expression found in the jejunum should have resulted in lower intra-intestinal absorption of grepafloxacin; however, the study data suggested that there was an increased absorption of grepafloxacin at specific time points (between 1.5 to 4 h), indicating the involvement of decreased secretory transport of grepafloxacin [18]. The in vivo findings was confirmed by the mechanistic in vitro work performed using jejunum loop, where it was found that there was a reduced amount of grepafloxacin left in the jejunum loop of GK rats relative to normal rats at the end of the experiment [18]. It is unknown if other efflux mechanism or a specific transporter is involved that may be possibly explain the observed phenomenon with grepafloxacin.
The increased absorption rate and higher bioavailability of cephalexin in GK rats were attributed to the specific PEPT1 transporter which is involved in the transport of oligopeptidic drugs like cephalexin [13]. The observed finding of cephalexin in GK rats should be considered for extrapolation to other drugs, such as the class of beta-lactam antibiotics [41], ACE inhibitors [41], and sulpiride [42], which may all be subjected to PEPT1-based transporter phenomenon for oral absorption.
In the case of rosuvastatin [19], the expression of MRP2 increased, but that of the BCRP remained unaltered in GK rats. In relation to the transporter data, the exposure of rosuvastatin decreased by approximately 18 % suggesting a possible role of MRP2 in the biliary efflux of rosuvastatin. Because the oral route of rosuvastatin administration was not performed in this study, the fate of oral absorption of rosuvastatin (i.e., governed by BCRP) in GK rats was unknown.
4.3 Metabolism and Elimination
After intravenous dosing of theophylline, the hepatic metabolism of the drug occurring via CYP1A2 appeared to be decreased in GK rats resulting in a slower elimination of the drug [21]. However, in this study, there was no specific metabolite(s) measured to corroborate the parent pharmacokinetics. To underscore this point, Moises et al. demonstrated that the metabolism of lidocaine and its metabolite mono-ethylglycinexylidide, both substrates to CYP1A2/CYP3A4 isozymes, was hindered in diabetic women relative to non-diabetic healthy women [43]. In contrast, patients with type 1 diabetes mellitus showed increased metabolism of antipyrine due to increased CYP1A2 activity [44]. Therefore, caution needs to be exercised in the translatability of the data from specific rodent diabetic models to the appropriate human diabetes conditions. In the case of exendin-4, through an interesting pharmacokinetic modelling exercise, it was suggested that elimination via renal mechanism was not affected in GK rats [15]. However, this area needs further probing, because various secretory and uptake transporters may get affected in co-morbid conditions, including T2DM [45]. Because of the existence of both cationic and anionic transporters in proximal renal tubules ensure safe and effective transport of endogenous and exogenous substrates, diligence is required to establish dependency, if any, on the drug disposition [46–48].
5 Conclusions
The compilation of pharmacokinetic data for several drugs has suggested that GK rats may serve as an interesting model to examine the role of altered physiological process, including changes in enzymatic and/or transporters levels in T2DM, on the drug disposition. The case studies reviewed in this report unequivocally support the verification and reappraisal of dosing strategy for some important drugs which may be either due to altered absorption and/or due to clearance mechanism in T2DM. However, caution needs to be exercised in the interpretation of the data, because of the influence of multiplicity of competing pathways which may govern the overall drug disposition.
References
Blair M. Diabetes mellitus review. Urol Nurs. 2016;36:27–36.
George AM, Jacob AG, Fogelfeld L. Lean diabetes mellitus: an emerging entity in the era of obesity. World J Diabetes. 2015;6:613–20.
Zaccardi F, Webb DR, Yates T, Davies MJ. Pathophysiology of type 1 and type 2 diabetes mellitus: a 90-year perspective. Postgrad Med J. 2016;92:63–9.
Cornell S. Continual evolution of type 2 diabetes: an update on pathophysiology and emerging treatment options. Ther Clin Risk Manag. 2015;11:621–32.
Buchwald H, Menchaca HJ, Michalek VN, Bertin NT. Ileal effect on blood glucose, HbA1c, and GLP-1 in Goto-Kakizaki rats. Obes Surg. 2014;24:1954–60.
Portha B, Giroix MH, Tourrel CC, Le-Stunff H, Movassat J. The GK rat: a prototype for the study of non-overweight type 2 diabetes. Methods Mol Biol. 2012;933:125–59.
Xue B, Sukumaran S, Nie J, Jusko WJ, Dubois DC, Almon RR. Adipose tissue deficiency and chronic inflammation in diabetic Goto-Kakizaki rats. PLoS One. 2011;6:e17386.
Almon RR, DuBois DC, Lai W. XueB, Nie J, JuskoWJ. Gene expression analysis of hepatic roles in cause and development of diabetes in Goto-Kakizaki rats. J Endocrinol. 2009;200:331–46.
Santos MS, Santos DL, Palmeira CM, Seiça R, Moreno AJ, Oliveira CR. Brain and liver mitochondria isolated from diabetic Goto-Kakizaki rats show different susceptibility to induced oxidative stress. Diabetes Metab Res Rev. 2001;17:223–30.
Goto Y, Kakizaki M. The spontaneous diabetic rat: a model of non-insulin dependent diabetes mellitus. Proc Jpn Acad. 1981;57:381–4.
Goto Y, Suzuki K, Sasaki M, Toyota T. Development of diabetes in the non-obese NIDDM rat (GK rat). AdvExp Med Biol. 1988;246:29–31.
McIntosh CHS, Pederson RA. Noninsulin-dependent animal models of diabetes mellitus. In: McNeill JH, editor. Experimental models of diabetes. Boca Raton: CRC; 1999. p. 337–98.
Watanabe K, Terada K, Sato J. Intestinal absorption of cephalexin in diabetes mellitus model rats. Eur J Pharm Sci. 2003;19:91–8.
Ogata M, Uchimura T, Iizuka Y, Murata R, Suzuki S, Toyota T, Hikichi N. Effect of non-insulin dependent diabetes on cyclosporin a disposition in Goto-Kakizaki (GK) Rats. Biol Pharm Bull. 1997;20:1026–9.
Gao W, Jusko WJ. Pharmacokinetic and pharmacodynamic modeling of exendin-4 in type 2 diabetic Goto-Kakizaki rats. JPET. 2011;336:881–90.
Center for drug evaluation research. BYETTA® (exenatide injection) pharmacology review, US FDA, NDA 21-773, 2005. pp. 1–393.
Mustajarvi II, Ihalmo P, Uutela P, Madetoja M, Kortejarvi H, Ketola RA, Yliperttula M. Hypoglycemic interaction of two drugsin control rats and in a rat model of diabetes. Univ Helsinki. 2013:52–54.
Watanabea M, Kobayashia M, Oguraa J, Takahashib N, Yamaguchia H, Isekia K. Alteration of pharmacokinetics of grepafloxacin in type 2 diabetic rats. J Pharm Pharm Sci. 2014;17:25–33.
He L, Yang Y, Guo C, Yao D, Liu HH, Sheng JJ, Zhou WP, Ren J, DongLiu X, Pan GY. Opposite regulation of hepatic breast cancer resistance protein in type 1 and 2 diabetesmellitus. Eur J Pharmacol. 2014;724:185–92.
Cao Y, DuBois DC, Almon RR, Jusko WJ. Pharmacokinetics of salsalate and salicylic acid in normal and diabetic rats. Biopharm Drug Dispos. 2012;33:285–91.
Takahashi A, Saito K, Takizawa Y, Murata R. Effect of Diabetes on theophylline disposition in the rat. Jpn J Hosp Pharm. 1999;25:603–7.
Terada T, Sawada K, Saito H, Hashimoto Y, Inui K. Functional characteristics of basolateral peptide transporter in the human intestinal cell line Caco-2. Am J Physiol. 1999;276:1435–41.
Ogihara H, Saito H, Shin BC, Terada T, Takenoshita S, Nagamachi Y, Inui K, Takata K. Immuno-localization of1 H/peptide co-transporter in rat digestive tract. Biochem Biophys Res Commun. 1996;220:848–52.
Padoin C, Tod M, Perret G, Petitjean O. Analysis of the pharmacokinetic interaction between cephalexin and quinapril by a nonlinear mixed-effect model. Antimicrob Agents Chemother. 1998;42:1463–9.
Hsiu SL, Hou YC, Wang YH, Tsao CW, Su SF, Chao PD. Quercetin significantly decreased cyclosporin oral bioavailability in pigs and rats. Life Sci. 2002;72:227–35.
Ogata M, Iizuka Y, Murata R, Hikichi N. Effect of streptozotocin-induced diabetes on cyclosporin A disposition in rats. Biol Pharm Bull. 1996;19:1586–90.
Copley K, McCowen K, Hiles R, Nielsen LL, Young A, Parkes DG. Investigation of exenatide elimination and its in vivo and in vitro degradation. Curr Drug Metab. 2006;7:367–74.
Herings RM, de Boer A, Stricker BH, Leufkens HG, Porsius A. Hypoglycaemia associated with use of inhibitors of angiotensin converting enzyme. Lancet. 1995;345:1195–8.
Yamaguchi H, Yano I, Hashimoto Y, Inui K. Secretory mechanisms of grepafloxacin andlevofloxacin in the human intestinal cell line Caco-2. J Pharmacol Exp Ther. 2000;295:360–6.
Yamaguchi H, Yano I, Saito H, Inui K. Pharmacokinetic role of P-glycoprotein in oral bioavailability and intestinal secretion of grepafloxacin in vivo. J Pharmacol Exp Ther. 2002;300:1063–9.
Nawa A, Fujita-Hamabe W, Tokuyama S. Inducible nitric oxide synthase-mediated decrease of intestinal P-glycoprotein expression under streptozotocin-induced diabetic conditions. Life Sci. 2010;86:402–9.
Hobbs M, Parker C, Birch H, Kenworthy K. Understanding the interplay of drug transporters involved in the disposition of rosuvastatin in the isolated perfused rat liver using a physiologically-based pharmacokinetic model. Xenobiotica. 2012;42:327–38.
Huang L, Wan Y, Grimm S. ATP-dependent transport of rosuvastatin in membrane vesicles expressing breast cancer resistance protein. Drug Metab Dispos. 2006;34:738–42.
Anderson K, Wherle L, Park M, Nelson K, Nguyen L. Salsalate, an old, inexpensive drug with potential new indications: a review of the evidence from 3 recent studies. Am Health Drug Benefits. 2014;7:231–5.
Faghihimani E, Aminorroaya A, Rezvanian H, Adibi P, Ismail-Beigi F, Amini M. Salsalate improves glycemic control in patients with newly diagnosed type 2 diabetes. Acta Diabetol. 2013;5:537–43.
Goldfine AB, Silver R, Aldhahi W, Cai D, Tatro E, Lee J, Shoelson SE. Use of salsalate to target inflammation in the treatment of insulin resistance and type 2. Clin Transl Sci. 2008;1:36–43.
Dahlqvist R, Billing B, Miners JO, Birkett DJ. Nonlinear metabolic disposition of theophylline. Ther Drug Monit. 1984;6:290–7.
Srinivas NR. Strategies for preclinical pharmacokinetic investigation in streptozotocin-induced diabetes mellitus (DMIS) and alloxan-induced diabetes mellitus (DMIA) rat models: case studies and perspectives. Eur J Drug Metab Pharmacokinet. 2015;40:1–12.
Marathe CS, Rayner CK, Jones KL, Horowitz M. Novel insights into the effects of diabetes on gastric motility. Expert Rev Gastroenterol Hepatol. 2016;10:581–93.
Thazhath SS, Marathe CS, Wu T, Chang J, Khoo J, Kuo P, Checklin HL, Bound MJ, Rigda RS, Crouch B, Jones KL, Horowitz M, Rayner CK. The glucagon-like peptide 1 receptor agonist exenatide inhibits small intestinal motility, flow, transit, and absorption of glucose in healthy subjects and patients with type 2 diabetes: a randomized controlled trial. Diabetes. 2016;65:269–75.
Boll M, Markovich D, Weber WM, Korte H, Daniel H, Murer H. Expression cloning of a cDNA from rabbit small intestine related to proton-coupled transport of peptides, beta-lactam antibiotics and ACE-inhibitors. Pflugers Arch. 1994;429:146–9.
Watanabe K, Sawano T, Endo T, Sakata M, Sato J. Studies on intestinal absorption of sulpiride: transepithelial transport of sulpiride across the human intestinal cell line Caco-2. Biol Pharm Bull. 2002;25:1345–50.
Moisés EC, Duarte LB, Cavalli RC, Marques MP, Lanchote V, Duarte G, da Cunha SP. Pharmacokinetics of lidocaine and its metabolite in peridural anesthesia administered to pregnant women with gestational diabetes mellitus. Eur J Clin Pharmacol. 2008;64:1189–96.
Matzke GR, Frye RF, Early JJ, Straka RJ, Carson SW. Evaluation of the influence of diabetes mellitus on antipyrine metabolism and CYP1A2 and CYP2D6 activity. Pharmacotherapy. 2000;20:182–90.
Moss DM, Neary M, Owen A. The role of drug transporters in the kidney: lessons from tenofovir. Front Pharmacol. 2014;5:248.
Tzvetkov MV, dos Santos Pereira JN, Meineke I, Saadatmand AR, Stingl JC, Brockmöller J. Morphine is a substrate of the organic cation transporter OCT1 and polymorphisms in OCT1 gene affect morphine pharmacokinetics after codeine administration. Biochem. Pharmacol. 2013;86:666–78.
Moss DM, Kwan WS, Liptrott NJ, Smith DL, Siccardi M, Khoo SH, Back DJ, Owen A. Raltegravir is a substrate for SLC22A6: a putative mechanism for the interaction between raltegravir and tenofovir. Antimicrob Agents Chemother. 2011;55:879–87.
DeGorter MK, Xia CQ, Yang JJ, Kim RB. Drug transporters in drug efficacy and toxicity. Annu Rev Pharmacol Toxicol. 2012;52:249–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors are employees of Cadila Health Care Ltd. and wish to declare that they have no conflict of interest or competing interests in the contents of the review manuscript (ZRC Publication No. 488).
Funding
The present work was not funded by any external sources.
Rights and permissions
About this article
Cite this article
Patel, H., Giri, P. & Srinivas, N.R. Review of Pharmacokinetic Data of Different Drug Classes in Goto-Kakizaki Rats, a Non-obese Model for Type 2 Diabetes Mellitus: Case Studies and Perspectives. Eur J Drug Metab Pharmacokinet 42, 173–182 (2017). https://doi.org/10.1007/s13318-016-0373-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-016-0373-y