Abstract
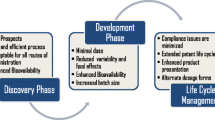
A large proportion of new drug candidates are poorly soluble in water, and therefore have poor bioavailability. A promising approach to overcome solubility problems is the production of nanoparticles (i.e., nanosuspensions). Parenteral nanoparticulate formulations provide an effective way of achieving high drug concentrations with low toxicity and can be administered via the intravenous (IV) route. Major advantages of this technology include ease of scale up and applicability to most drug candidates. Abraxane® was the first FDA approved (2005) IV nanoparticulate product available on the market. This chapter reviews various methods of nanoparticle production and characterization. In addition, formulation considerations and ongoing research specific to parenteral nanoparticles/nanosuspensions are described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Soluble Drug
- Solid Lipid Nanoparticles
- Drug Particle
- Particle Size Reduction
- Photon Correlation Spectroscopy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
13.1 Introduction
The goal of controlled and targeted drug delivery is to provide an appropriate dosage of active pharmaceutical ingredients (APIs) at a desired rate to a specific region in the body. Thirty to forty percent of the new chemical entities discovered or synthesized in pharmaceutical companies have poor solubility and hence, poor bioavailability. The poor solubility of new chemical entities makes their formulation very challenging and is often cited as a main reason for the discontinuation of development of these new compounds [1, 2]. In recent years, nanotechnologies have been used to overcome poor solubility and bioavailability, as well as to achieve site-specific drug delivery [3–5]. Nanotechnology in parenteral drug delivery is a fairly new concept. For many decades, coarse solid suspensions have been produced for the parenteral delivery of poorly water-soluble drugs. For example, a range of coarse suspensions of insulin have been formulated for subcutaneous delivery (such as, HUMULIN, ILETIN, LENTE etc., manufactured by Elli Lily). Other examples are Bicillin® L-A manufactured by Wyeth-Ayerst and Decadron-LA manufactured by Merck, which are administered intramuscularly. Parenteral nanosuspensions are used to reduce irritancy and control the rate of drug delivery [6].
The term nanotechnology was first used by the scientist Norio Taniguchi (1974), at the University of Tokyo, Japan, for any material in the nanometer size range. The prefix nano is derived from the Greek word for dwarf or small. Nanosuspensions consists of drug nanoparticles, stabilizers (such as, surfactants and polymers, etc.) and dispersion medium. The dispersion medium can be aqueous or non-aqueous in nature. The FDA (The US Food and Drug Administration) has not yet established a precise definition/size range for pharmaceutical nanosuspensions. However, pharmaceutical nanosuspensions are generally considered as consisting of particles with mean diameters below 1,000 nm or 1 μm.
A major question in formulation of an API is when to select nano-sized formulations over conventional formulations. This can depend on drug solubility, as well as the desire for controlled and/or localized delivery. In the case of poorly soluble drugs, solubility may be enhanced by salt formation, use of co-solvents, micellization and incorporation within emulsion formulations, as well as size reduction to nanoparticulates [4, 5]. Refer to Fig. 13.1 for a decision tree on different ways of solubility enhancement of poorly soluble drugs.
13.1.1 Saturation Solubility and Dissolution Rate
Nanosuspensions have widespread interest as a drug delivery system due to their relatively high saturation solubilities and dissolution rates. Nanosuspensions differ significantly from all other formulations due to the following two major factors:
-
Surface-to-volume ratio: Surface-to-volume ratio is the amount of surface area per unit volume of an object/drug particle. The surface area-to-volume ratio is measured in units of inverse of the length. For example, in the case of spheres, it is measured as surface area/volume of a sphere (\( 4\pi {r}^{2}/(4/3\pi {r}^{3})\), where, r is radius of the particle) i.e., 3/r. Thus in the case of drug particles, as the size decreases the surface-to-volume ratio increases (Fig. 13.2). The solubility dependence on particle size is described by a modified form of the Kelvin equation:
$$ \frac{S}{S(0)}=\mathrm{exp}\left(\frac{\gamma V}{RTd}\right),$$(13.1)where, S = solubility, S(0) = solubility of bulk material, R = gas constant, V = molar volume, T = temperature, d = diameter of particle and γ = surface free energy.
-
Higher dissolution rate: Surface-to-volume ratio is directly proportional to the dissolution rate, i.e., the higher the surface-to-volume ratio, the higher the dissolution rate of the drug. The kinetics of the drug particle dissolution can be described by the Noyes Whitney equation.
$$ \frac{\text{d}C}{\text{d}t}=\frac{DS}{Vh}({C}_{\text{s}}-C),$$(13.2)where, dC/dt is change in concentration, D is the diffusion coefficient, S is the surface area of the drug particle, h is the thickness of the diffusion layer, C s is the saturation solubility of the drug particle, C is the concentration of the drug in solution with V as total volume of the solution [7].
13.1.2 Clinical Performance
Increase in surface-to-volume ratio and dissolution rate of nanoparticles/nanosuspensions improves their pharmacokinetic properties in terms of: increased rate and extent of release and absorption [8, 9]; rapid onset of action; reduced side effects and improved clinical performance [10, 11]. Nanoparticles are generally well tolerated via IV delivery. The inner diameter of the smallest blood vessels is in the range of 5–7 μm. Large quantities of inert polystyrene-divinylbenzene particles even up to 25-μm particles have been shown to be tolerated, if administered slowly over 1 h [12]. Whereas, hemodynamic effects, such as hypotension were observed when 3-μm size inert polystyrene beads were administered intravenously [13]. The concentration and rate of infusion play are important with respect to the hemodynamic effects. For example, reducing the concentration to 5% and the infusion rate from 1 to 0.5 ml/min reduced hemodynamic effects in anesthetized dogs. The hemodynamic effect appears to be mediated by histamine release, but further elaboration is required.
Another major advantage of nanoparticles as parenteral formulations is delivery of large quantities of drug with lower toxicity than would otherwise be possible by drug solutions, micellar solutions, co-solvent systems, etc. Nanosuspensions generally require low amounts of stabilizers (i.e., surfactants and/or polymers). Other approaches to increase drug solubility (such as, the use of high levels of surfactants, co-solvents, cyclodextrin complexes, etc.) may cause hypersensitivity reactions in certain individuals [14, 15] when administered parenterally. The commercial product SPORANOX® IV (Janssen Pharmaceutica Products, L.P.) contains 400 mg of excipient (2-hydroxy propyl-β-cyclodextrin) per 10 mg of itraconazole (Janssen, SPORANOX package).
13.2 Theory
Manufacturing of nanosuspensions involves the generation of a large number of small particles with enormous surface area. This significantly increases the Gibb’s free energy of the system and, due to the high interfacial tension, these systems are thermodynamically unstable. Accordingly, nanoparticles will tend to minimize their total energy by undergoing agglomeration. The increase in free energy is given by the Gibb’s free energy equation:
where, ΔA is the change in surface area, γ is the surface tension, T is the absolute temperature and ΔS is the change in entropy.
The process of agglomeration depends on the activation energy, which is influenced by the addition of stabilizers to the system (such as, surfactants and polymers). These stabilizers reduce the interfacial tension between the particles and the dispersion medium. To achieve maximum stability, stabilizers are added at the early stages of nanosuspension preparation. The first and foremost requirement of these stabilizers is to reduce interfacial tension and act as wetting agents. The second requirement is to provide a barrier between the drug particles to prevent agglomeration. Possible mechanisms for providing a barrier are:
-
Electrostatic repulsion
-
Steric stabilization
13.2.1 Electrostatic Repulsion
The concept of electrostatic repulsion can be explained by the DLVO theory. The DLVO theory is named after Derjaguin and Landau, Verwey and Overbeek. According to the DLVO theory, the interaction of solid particles in liquid medium can be described by: (a) attractive or Lifshitz-van der Walls interaction; (b) repulsive, electrostatic repulsive forces due to overlap of electrical double layers; and (c) structural forces due to solvent molecules around the drug particle that can be attractive or repulsive in nature. When a drug particle is suspended or dispersed in a liquid medium, an electrostatic double layer forms around it. This electrostatic double layer arises as a consequence of the charge at the solid–liquid interface, which arises due to adsorption of ions, dissociation of ionizable groups, isomorphic substitution or accumulation of electrons on the surface, etc. Counter ions present in the liquid medium are attracted towards the charged particle surface and form a double layer of ions which consist of: (a) a tightly bound layer and (b) a diffuse layer of ions. The ions in the tightly bound layer are determined by the charge on the drug particle, whereas ions in the diffuse layer are distributed around the drug particle due to diffusive forces associated with random motion. Accordingly, the diffuse layer includes both ions of the opposite charge and ions of the same charge. At the outside of the diffuse layer the charge on the drug particle is neutralized (Fig. 13.3). The total energy of the interaction (V total) between drug particles is given by:
where, V repulsion is calculated using the approximation approach (called Derjaguin approximation).
where, a is the radius of the particle, n ∞ is the bulk concentration of the ions, 1/κ is the Debye screening length, K B is the Boltzmann constant, T is the absolute temperature and H is the separation distance between the particles.
and where, Ψ is the potential associated with double layer and z is the valency of the ions.
Whereas the attractive forces between the two dispersed particles/sphere of equal radius and separated by distance H (for a >> H) is calculated as:
where, A is the Hamaker constant, and a is the radius of the particles.
These attractive and repulsive forces can be easily explained using a potential energy diagram (Fig. 13.4). The attractive forces dominate at very small and large distances. At intermediate distances, the repulsive forces dominate resulting in net repulsion between particles which prevents agglomeration.
13.2.2 Steric Stabilization
Another approach/mechanism for the stabilization of nanosuspensions is “steric stabilization,” using polymeric additives such as, HPMC, PVP, etc. In this approach, a high concentration of polymers is added to the colloidal system. These polymers are adsorbed onto the drug particle and their long hydrophilic chains (extend into the water) preventing the particles from agglomerating (Fig. 13.5). This approach has advantages over other stabilization methods such as, relative insensitivity to the presence of the electrolyte and equal efficacy in both aqueous and non-aqueous media (the polymer used should have a good affinity for the external medium, as well as for the insoluble drug particle to provide good surface coverage and even distribution on the nanoparticles).
13.3 Different Types of Nanoparticles
Pharmaceutical nanoparticles can be classified into four main categories:
-
(a)
Crystalline drug nanosuspensions stabilized using polymers and/or surfactants.
-
(b)
Polymeric nanoparticles such as, poly(lactic co-glycolic) acid (PLGA) containing entrapped API.
-
(c)
Solid lipid nanoparticles – Solid lipid nanoparticles are submicron particles made up of an oily core, surrounded by a solid or semi-solid shell. In lipid nanoparticles, the drug is encapsulated within the lipid matrix. Lipid nanoparticles are usually produced via high-pressure homogenization techniques.
-
(d)
Liposomes – Liposomes are small spherical shaped vesicles, made up of lipid bilayers. The drug can either be dissolved or dispersed in the inner aqueous compartment or the lipid bilayer depending on the hydrophobicity of the drug molecule.
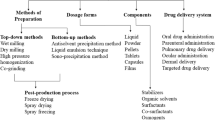
13.4 Methods of Preparation
13.4.1 Top Down Processes
The top down approach consists of reducing the particle size from larger to smaller particles using different techniques such as, high pressure homogenization, media milling, etc. In these processes, heat is generated during particle size reduction; therefore, auxiliary cooling systems are required to prevent degradation of thermo-labile compounds or to prevent any polymorphic changes. Different top-down methods are explained below.
13.4.1.1 Media Milling
Media milling processes are commonly used for the production of ultrafine particles. Media milling processes involve attrition of the particles in a mill using milling media such as, glass, zirconium oxide, etc. This process involves feeding the milling chamber with milling media, stabilizer and drug particles and rotating the milling shaft at a desired speed (Fig. 13.6). The high forces generated during the process cause the particles to break along weak points and finally smaller particles are produced. Milling media can be selected from a variety of dense and hard materials such as, silicon carbide, ceramics, zirconium silicate, glass, alumina, titanium and polymers (e.g., cross-linked polystyrene). The media milling process is a patented technology of Elan® drug technologies (known as Nanocrystals®). This technology was first used to prepare and market an inflammatory drug nanosuspension formulation, Rapamune®. Some of the major advantages of this process are reproducibility, cost-effectiveness and control over drug particle size. The major disadvantage of this technique is contamination of the final product with milling media or machine parts as a result of erosion during milling [16].
13.4.1.2 High Pressure Homogenization
High-pressure homogenization has emerged as a powerful and reliable technique for the preparation of nanosuspensions. It was first developed and patented by Muller and Becker [17] and is now owned by Sykepharma LLC, known as Dissocubes®. This technique has been used for the production of nanoemulsions for parenteral nutrition. Scaling up is easier as compared to other techniques.
The high-pressure homogenization process can be divided into two broad categories:
-
Hot homogenization
-
Cold homogenization
Generally, nanosuspensions are prepared via cold homogenization, where temperature regulation is required to prevent any degradation of the drug. Hot homogenization is generally used for the preparation of microemulsions. The main disadvantages of these methods are strict temperature control and pre-micronization of macro-suspensions to prevent any blockage during homogenization.
Further, high-pressure homogenization can be classified into three different technologies:
13.4.1.2.1 Microfluidics® Technology
In this technology, nanoparticles are generated by high shear stress using a jet steam homogenizer. The microfluidizer was originally designed by the Arthur D. Little Co., but was later taken over by the Microfluidics Corp. The principle of particle size reduction is based on the collision of two fluid streams under high-pressure, which leads to the generation of high shear and cavitation forces (Fig. 13.7) [18]. In this process, macro suspensions are passed through specialized chambers under high pressure. These chambers consist of narrow openings, which divide the macro suspensions into several parts. At high pressure and velocity, different streams of liquid collide against each other inside the interaction chamber, which causes the drug particles to fracture and break. The major disadvantage of this method is production time. The advantage of this method is narrower distribution of the particles as compared with other homogenization methods.
13.4.1.2.2 Piston-Gap Homogenization in Water (Dissocubes® Technology)
This technique involves the passage of macro suspensions through a small slit/aperture under high pressure (100–2,000 bar). Depending on the viscosity and concentration of the particle suspension, the width of the slit is in the range of 5–20 μm. The fluid accelerates to a high velocity and the pressure reduces tremendously at the small slit/aperture. When the suspension emerges from the aperture there is a drop in velocity and an increase in pressure as per Bernoulli’s law, which creates high-energy shock waves. These high-energy shock waves are mainly responsible for the particle size reduction or fracture of the drug particles (Fig. 13.8) [19, 20].
13.4.1.2.3 Nanopure® Technology
Nanopure® Technology was developed and owned by PharmaSol GmbH/Berlin. In this process, homogenization is conducted using low vapor pressure dispersion media at very low temperature (e.g., 0°C). Drug nanocrystals are produced using pure water as a dispersion medium. The turbulent flow and shear forces generated during homogenization are responsible for breaking the drug particles into the nano-size range. Non-aqueous homogenization is beneficial if the nanosuspensions are to be finally converted into solid dosage forms using spray drying, fluidized bed drying, etc. Another advantage of this method is that thermo-labile drugs can be used, since the process is performed at low temperature.
13.4.2 Bottom Up Processes
13.4.2.1 Solvent–Anti-solvent Technique or Precipitation Method
List and Sucker have utilized this method for the formulation of poorly soluble drugs, which was patented as Hydrosol technology in 1988 [21, 22] (owned by Sandoz, now Novartis). Hydrosols are colloidal particles in a size range of a few nanometers to 10,000 nm. In this technique, the poorly soluble drug is dissolved in the organic solvent (water-miscible) such as, ethanol. After dissolving the drug, the anti-solvent or non-solvent is poured or mixed slowly with the previously made drug–solvent solution. This leads to precipitation of drug particles from the solvent–anti-solvent mixture. These nanoparticles tend to grow bigger in size, driven by the “Oswald Ripening” phenomenon. To prevent or preserve the size of these particles different approaches have been utilized. For example, freeze-drying or spray drying is conducted immediately after precipitation to preserve the particle size [23]. In another approach, polymeric growth inhibitors are used in the system to preserve the size of the precipitated particles.
Another variation of this process, was developed by Sarkari et al. [24], and is called “evaporative precipitation.” In this process, a heated solution of drug–water immiscible phase is atomized into a stabilizer containing aqueous solution, causing precipitation of the nanoparticles. In another approach, change in temperature and pH has been used to prepare a drug as a nanoparticle dry powder [25].
13.4.2.2 Supercritical Fluid Process
In this technology, both drug and polymer/stabilizer are dissolved in the organic solvent and then atomized through a nozzle into supercritical CO2, where CO2 acts as an anti-solvent (Fig. 13.9). As the dispersed organic phase containing drug and polymer comes into contact with CO2, both phases diffuse into each other. CO2 is only miscible with the solvent, thus the solvent is extracted and expelled from the outlet causing the insoluble solid to precipitate and fall out as nanoparticles [26].
13.4.2.3 Emulsion-Solvent Evaporation
An emulsion-solvent evaporation technique can be used to prepare polymeric self-assembled nanoparticles. These polymeric self-assembled nanoparticles offer many advantages such as, their hydrophobic core serves as a reservoir for poorly soluble drug and the hydrophilic shell reduces their interaction with plasma proteins. These self-assembled nanoparticles are in the size range of 150–500 nm. In this technique, drug and polymeric amphiphiles are suspended in an appropriate buffer solution and then an organic solvent (such as, chloroform) is added to form an emulsion. This emulsion is sonicated to reduce the particle size. Chloroform is evaporated using a rotary evaporator and then the product is passed through a syringe filter to achieve a nanoparticle suspension [27] (Fig. 13.10). Later it can be mixed with appropriate sugars to undergo freeze-drying.
Schematic representation of generation of polymeric nanoparticles (reprinted with permission, from, Lee [27])
13.4.2.4 Spray Drying
Spray drying processing is utilized for a number of applications in the pharmaceutical industry such as, drying of solutions and emulsions, coating, nanoparticle manufacture, etc. In spray drying, drug-containing macro-suspensions are forced through an atomizer or nozzle, producing tiny droplets or mists, which are then dried in the drying chamber to obtain fine particles (Fig. 13.11). The spray-dried powder can easily be re-suspended in water and used when needed. This process has several advantages over other methods such as: it is a continuous process, it is less time consuming than other processes, it is easy to scale-up and it is cost effective. However, the one-droplet-to-one-particle mechanism during spray drying sets the lower size limit; therefore, it is difficult to generate particle sizes below 200 nm.
13.4.2.5 Electro Spraying
Electro spraying is a technique in which a micro-capillary electrospray atomizer and high voltage is used to generate small droplets of macro-suspensions/emulsions [28]. The application of high voltage causes the potential of the solution to increase due to the accumulation of electrostatic charges. The increase in potential increases the electrostatic forces and thus decreases the effect of surface tension on the droplets at the interface. When the surface tension and the applied electrostatic charge are equal, a Taylor cone is formed at the micro-capillary interface (Fig. 13.12). Further application of electrostatic charges disturbs the cone and breaks the suspension into smaller droplets at the tip of the cone. To achieve a required droplet size, the ratio of flow rate and conductivity should be controlled. These small charged droplets then travel in the gas phase under the electric field towards a counter electrode, where the solvent evaporates and this leads to further size shrinkage. The main advantages of this method are its versatility, inexpensiveness and simplicity to operate.
13.4.3 Other Techniques
13.4.3.1 Nanoedge Technology
BAXTER owns Nanoedge technology and this process relies on the combination of a micro-precipitation technique with a subsequent annealing step either by applying high shear or thermal energy. Nanosuspensions are formed using the solvent–anti-solvent technology (as explained above) and depending on the precipitation conditions, either amorphous or crystalline drug particles are formed. A subsequent annealing process will preserve the size of the drug particles without changing the mean diameter. Particle sizes in the range of 400–2,000 nm can be easily obtained using this technology [4, 5].
13.4.3.2 Microfluidization Reaction Technology
Microfluidization reaction technology (MRT) is a continuous and scalable microreactor system, which is an amalgamation of the “bottom up” and “bottom down” approaches. In MRT pressurized solutions of drug and anti-solvent are pumped through a Microfluidizer® reaction chamber. In the reaction chamber, streams of the liquids collide with each other at supersonic speeds up to 300 m/s (Fig. 13.13). The particle size reduction achieved in the interaction chamber is mainly due to cavitation and high shear forces produced during particle collision.
13.5 Characterization of Nanosuspensions
Nanoparticles are characterized by both chemical and physical methods. Chemical methods are specific for APIs such as, analysis of API, as well as their degradation products (including HPLC, UV, Mass Spectrometry, etc.).
13.5.1 Physical Methods
13.5.1.1 Particle Size and Shape
Different approaches have been used to measure the particle size of nanoparticles. Photon correlation spectroscopy (PCS) and laser diffraction (LD) are the most powerful and popular techniques to measure nanoparticle size. Dynamic light scattering (also called as PCS) measures the intensity of scattered light caused by particle movement in the solution/suspending agent. Laser diffraction (LD) utilizes a correlation between the intensity of scattered light and its diffraction angle from the particles.
Particle size techniques can be divided into three major categories for easy explanation:
-
1.
Ensemble methods, such as, laser diffraction assess bulk property.
-
2.
Counting methods, individual particles are counted, for example electron microscopy.
-
3.
Separation methods, classify particles in different size ranges depending on their behavior such as, centrifugation and chromatography.
13.5.1.2 Zeta Potential
Zeta potential, also known as “electrokinetic potential,” is a measure of the electric potential at the interface of the electrical double layer. Zeta potential provides a way of expressing the stability of colloidal dispersions such as, nanosuspensions. There are several instruments available for measuring zeta potential, based on the electrophoretic mobility of particles suspended in a medium.
13.5.1.3 Re-suspendability
Many pharmaceutical formulations are aqueous suspensions or nanosuspensions of poorly water-soluble drug together with appropriate excipients. Their sedimentation characteristics during storage are of significant importance, since these can give rise to non-uniform distributions of drug and hence failure and/or side effects due to overdosing. There are many techniques/methods available to study sedimentation (e.g., optical analysis, ionizing radiation absorption, electrical sensing, etc.).
13.5.1.4 Dissolution
The dissolution rate of a drug is dependent upon its crystalline/amorphous form and particle size distribution. There are different apparatus/methods available to test the dissolution profile of different formulations. For nanosuspension dissolution, there is no current compendial method. Their rapid release and small particle size restrict the use of various compendial methods. The most commonly used method for dissolution testing of nanosuspensions is USP II apparatus (paddle type). However, non-compendial methods such as, the dialysis sac method have been investigated for dissolution testing of nanosuspensions. Recently a dialysis sac adapter for the USP IV apparatus has been developed for liposome release testing and is under investigation for use with nanosuspensions [29]. Another method used for dissolution testing of nanosuspensions involves measurement of the %-transmitted light using a UV-spectrophotometer [30]. This method is based on the principle that the nanosuspensions being colloidal in nature block/refract light. Accordingly, by measuring the % of transmitted light, a dissolution profile can be obtained.
13.5.1.5 Polymorphs/Crystallinity
Drugs may exist in numerous solid forms (or nanoparticle generation process can yield different polymorphs), which may feature different physical and chemical properties. It is important to understand the solid form a nanosuspension, as this affects both the solubility and the stability of the product. These solid forms include polymorphs (true), solvates (pseudo-polymorphs), desolvates and the amorphous state. This phenomenon is known as “polymorphism.” There are different techniques used to characterize polymorphs such as, crystallography, spectroscopy, microscopy and thermal techniques. Microscopic (light or electron) characterization is based either on the thermal technique or on the morphological properties of the drug. Alternative techniques are also available to characterize drugs that are not perfectly crystalline or pure, including X-ray diffraction and solid-state spectroscopy.
13.5.1.6 Excipients
Excipients play a major role in nanosuspension stability. The tendency of smaller particles in nanosuspensions to dissolve and re-grow on bigger particles, termed Ostwald ripening, is one mode of nanosuspension instability. The speed of Ostwald ripening is controlled by molecular diffusion and surface reaction [31] and happens as a result of the Kelvin effect [32]. Accordingly, faster ripening can be expected for smaller particle size suspensions such as, nanosuspensions. Addition of excipients can delay or totally prevent this phenomenon. Thus selection of excipients is an important concern for the stability of nanosuspensions. In one study, an AFM technique has been used to explain the type of adsorption of different stabilizers on nanosuspension formulations and this method is suggested as a rapid screening method for nanosuspension stabilizer selection [33].
Different stabilizers are used for nanosuspension stabilization either alone or in combination. The most popular are non-ionic surfactants such as, poloxamers, Tween 80, sodium lauryl sulfate, etc. Polymers are also used for stabilization such as, cellulosics (such as, HPMC, HPC, etc.) and polyvinyl alcohol. Additionally, natural excipients (such as, lecithins, cholic acid derivative, etc.) are frequently used. Table 13.1 provides an overview of different excipients used in nanosuspension stabilization. Few examples are included, since the list is too extensive (for example, Elan’s NanoCrystal® technology has over 700 patents on file).
13.6 Nanosuspensions for Drug Delivery
Nanoparticulates can be used for compounds that are water insoluble and have high log P values to deliver large amount of drug with minimal or no toxicity. Their small size and increased surface-to-volume ratio leads to an increase in dissolution rate and bioavailability. The particulate nature of nanosuspensions can be useful for drug targeting (such as, targeting to the monocyte phagocytic system). Marketed products and those that are currently in clinical trials, which include nanoparticulates, are listed in Table 13.2. Nanosuspension performance can be further improved by controlled surface modification of the drug nanoparticles. To create targeted nanoparticles with desired surface properties, specific surfactants or polymeric stabilizers are used. The degree of modification can be measured in terms of surface charge (i.e., zeta potential) or hydrophobic interaction chromatography (HIC) analysis.
13.7 Nanosuspensions for Parenteral Delivery
The approval of Abraxane® in 2005, as an IV nanoparticle dosage form (130 nm amorphous particles entrapped in an albumin matrix) for the treatment of breast cancer has resulted an increase in activity in the area of nanoparticles for parenteral delivery. IV drug infusion/injection provides the most rapid delivery of drug to the body. For other parenteral routes such as, intramusular (IM), absorption of drug must take place and this can take minutes to months. Hence, this route can be utilized for controlled and delayed drug delivery. Release of drug from nanosuspensions following IM delivery includes two major steps: (a) dissolution of the nanosuspensions and (b) diffusion of dissolved drug. Dissolution is generally a rate-limiting step for absorption of poorly soluble drugs and nanosuspensions provide better solubility and faster dissolution.
Factors to be considered in injectable nanoparticle formulation:
-
1.
Excipients: Different types of stabilizers are used to stabilize nanosuspensions for parentral use. There are only a limited number of excipients that have been approved for parenteral use, these include poloxamers and phospholipids. In the case of surfactants, only non-ionic and anionic surfactants are preferred since cationic surfactants can cause hemolysis and cell toxicity. In addition, drug nanoparticles can be coated with special coating materials to avoid capture by the reticuloendothelial system. For example, phospholipid–PEG coatings on the drug particle can be used to increase the half-life of the nanoparticles [34].
-
2.
Particle size: Particle size distribution and morphology are the major parameters for characterizing nanoparticle formulations and their safety upon administration. Different methods are used to determine the particle size of nanoparticles (as described above) such as, dynamic light scattering, photon correlation spectroscopy, etc.
-
3.
Syringeability: Syringeability is an important factor to consider for nanosuspension used for IV delivery. Syringeability is measured as the pressure associated with injection using a needle of predetermined gauge and length. A method to measure syringeability using a specific apparatus has been proposed [35]. For non-aqueous suspensions, syringeability is given by a following equation:
$$ \text{Syringeability}=\frac{\pi {d}^{4}}{128\text{}\text{\hspace{0.05em}}m{l}_{\text{n}}},$$(13.8)where, d = diameter of the needle, l n = length of the needle, μ = viscosity of suspension/solution.
-
4.
Sterility and pyrogenicity: One of the most important requirements for IV and other parenteral nanosuspensions is sterility. It has been shown that the process of crystallization can entrap bacterial spores and these entrapped spores may be resistant to chemical sterilization [36, 37], as well as moist and dry heat [38, 39] sterilization. Sterilization of the final product at 121°C for an extended period of time and then cooling can promote physical and chemical instability such as, Ostwald ripening, drug degradation, etc. If the particle size of the IV nanosuspensions is small enough, then sterile filtration may be performed. For example, sterile filtration is used for NanoCrystal® iodipamide of mean particle size 98 nm with all particles <220 nm [40].
Aseptic manufacturing of IV nanosuspensions is another way to achieve sterile formulation. The risk factors associated with sterility assurance include personnel, facility, aseptic process, quality assurance, etc. and have been described by the FDA.
Another requirement of IV injectable nanosuspensions is that they are free from endotoxins and pyrogens. A bacterial endotoxin test is required to check the endotoxin levels in the final formulation. An alternative to the endotoxin test is the USP pyrogen test.
13.8 Concluding Remarks
Drug nanoparticulates represent a technology to overcome solubility and bioavailability problems of poorly soluble drugs. Nanoparticles offer various advantages such as, an increase in drug-to-volume ratio and saturation solubility that lead to an increase absorption and bioavailability. Other major advantages offered by nanoparticulates are high drug loading and minimal or no side effects. Over the last several years, there has been rapidly growing interest in nanotechnology for parenteral delivery. Selection of excipients plays an important role in the stability, as well as the targetability of nanoparticles. Most of the marketed products are solid dosage form. Drying (such as, freeze or spray drying) of the nanosuspensions can be used to prevent both physical and chemical instabilities (such as, Ostwald ripening and drug degradation) associated with them.
References
Kipp JE (2004) The role of solid nanoparticle technology in the parenteral delivery of poorly water-soluble drugs. Int J Pharm 284(1–2):109–22
Lipinski C (2002) Poor aqueous solubility-an industry wide problem in drug discovery. Am Pharm Rev 5:82–85
Muller RH (1998) Emulsions and nanosuspensions for the formulation of poorly soluble drugs. Medpharm Scientific, Stuttgart
Muller RH, Jacobs C, Kayser O (2001) Nanosuspensions as particulate drug formulations in therapy. Rationale for development and what we can expect for the future. Adv Drug Deliv Rev 47(1):3–19
Rabinow BE (2004) Nanosuspensions in drug delivery. Nat Rev Drug Discov 3(9):785–96
Wong J et al (2008) Suspensions for intravenous (IV) injection: a review of development, preclinical and clinical aspects. Adv Drug Deliv Rev 60(8):939–54
Martin A (2001) Physical pharmacy. Lippincott Williams & Wilkins, Philadelphia, PA
Yin SX et al (2005) Bioavailability enhancement of a COX-2 inhibitor, BMS-347070, from a nanocrystalline dispersion prepared by spray-drying. J Pharm Sci 94(7):1598–607
Jinno J et al (2006) Effect of particle size reduction on dissolution and oral absorption of a poorly water-soluble drug, cilostazol, in beagle dogs. J Control Release 111(1–2):56–64
Liversidge GG, Conzentino P (1995) Drug particle-size reduction for decresing gastric irritancy and enhancing absorption of naproxen in rats. Int J Pharm 122(2):309–313
Kayser O et al (2003) Formulation of amphotericin B as nanosuspension for oral administration. Int J Pharm 254(1):73–5
Schroeder HG et al (1978) Physiological effects of subvisible microspheres administered intravenously to beagle dogs. J Pharm Sci 67(4):508–13
Slack JD et al (1981) Acute hemodynamic effects and blood pool kinetics of polystyrene microspheres following intravenous administration. J Pharm Sci 70(6):660–4
Volcheck GW, Van Dellen RG (1998) Anaphylaxis to intravenous cyclosporine and tolerance to oral cyclosporine: case report and review. Ann Allergy Asthma Immunol 80(2):159–63
Singla AK, Garg A, Aggarwal D (2002) Paclitaxel and its formulations. Int J Pharm 235(1–2):179–92
Verma S, DJ Burgess (2009) Solid nanosuspensions: the emerging technology and pharmaceutical applications as nanomedicine, Chapter 10. In: Pharmaceutical suspensions: from formulation development to manufacturing. DOI 10.1007/978-1-4419-1087-5_10
Muller RH, Becker R (1996) Pharmaceutical nanosuspensions for medicament administration as systems with increased saturation solubility and speed of dissolution. US Patent 5858410
Gruverman IJ (2003) Breakthrough ultraturbulent reaction technology opens frontier for developing life-saving nanometer-scale suspensions and dispersions. Drug Deliv Technol 3(1):52
Phipps LW (1971) Mechanism of oil droplet fragmentation in high pressure homogenizers. Nature 233(5322):617–9
Schultz S, Wagner GK (2004) High-pressure homogenization as a process for emulsion formation. Chem Eng Technol 27(4):361–368
List M, Sucker H (1995) Hydrosols of pharmacologically active agents and their pharmaceutical compositions comprising them. US patent 5389382
List M, Sucker HB (1988) Pharmaceutical colloidal hydrosols for injection. GB patent 5145684
Gassmann P, List M (1994) Hydrosols-alternative for the parenteral application of poorly water soluble drugs. Eur J Pharm Biopharm 40(2):64–72
Sarkari M et al (2002) Enhanced drug dissolution using evaporative precipitation into aqueous solution. Int J Pharm 243(1–2):17–31
Pozarnsky GA, Matijevic NK (1997) Preparation of monodisperse colloids of biologically active compounds.1. Naproxen. Colloids Surf, A Physicochem Eng Asp 125(1):47–52
Jung J, Perrut M (2001) Particle design using supercritical fluids: literature and patent survey. J Supercrit Fluids 20(3):179–219
Lee M (2005) Size control of self-assembled nanoparticles by an emulsion/solvent evaporation method. Colloid Polym Sci 284:506–512
Lee M (2006) Size control of self-assembled nanoparticles by an emulsion/solvent evaporation method. Colloid Polym Sci 284:506–512
Peltonen L et al (2010) Electrospraying, spray drying and related techniques for production and formulation of drug nanoparticles. Expert Opin Drug Deliv 7(6):705–19
Rabinow B (2004) Nanoedge drug delivery solves the problems of insoluble injectable drugs. Supplement to Scrip World Phamaceutical News, October, 13–16
Bhardwaj U, Burgess DJ (2010) A novel USP apparatus 4 based release testing method for dispersed systems. Int J Pharm 388(1–2):287–94
Nie K (2009) Monitoring ambroxol hydrochloride sustained-release tablets release by fiber-optic drug dissolution in situ test system. Dissolution Technologies
Mullin J (2004) Crystallization, 4th edn. Elsevier, Oxford, pp 320–322
Welin-Berger K, Bergenstahl B (2000) Inhibition of Ostwald ripening in local anesthetic emulsions by using hydrophobic excipients in the disperse phase. Int J Pharm 200(2):249–60
Verma S, Huey BD, Burgess DJ (2009) Scanning probe microscopy method for nanosuspension stabilizer selection. Langmuir 25(21):12481–7
Muller RH, Peters K (1998) Nanosuspensions for the formulation of poorly soluble drugs. I. Preparation by a size-reduction technique. Int J Pharm 2:229–237
Jacobs C, Muller RH (2002) Production and characterization of a budesonide nanosuspension for pulmonary administration. Pharm Res 19:189–194
Zhang D et al (2007) Preparation of azithromycin nanosuspensions by high pressure homogenization and its physicochemical characteristics studies. Drug Dev Ind Pharm 33:569–575
Muller RH, Jacobs C (2002) Buparvaquone mucoadhesive nanosuspension: preparation, optimisation and long-term stability. Int J Pharm 237(1–2):151–61
Krause KP, Muller RH (2001) Production and characterisation of highly concentrated nanosuspensions by high pressure homogenisation. Int J Pharm 214(1–2):21–4
Kumar MP, Rao YM, Apte S (2008) Formulation of nanosuspensions of albendazole for oral administration. Curr Nanosci 4:53–58
Wu Y et al (2004) The role of biopharmaceutics in the development of a clinical nanoparticle formulation of MK-0869: a Beagle dog model predicts improved bioavailability and diminished food effect on absorption in human. Int J Pharm 285(1–2):135–46
Deng Z, Xu S, Li S (2008) Understanding a relaxation behavior in a nanoparticle suspension for drug delivery applications. Int J Pharm 351(1–2):236–43
Peters K, Muller RH, Craig DQ (1999) An investigation into the distribution of lecithins in nanosuspension systems using low frequency dielectric spectroscopy. Int J Pharm 184(1):53–61
Mouton JW, van Peer A, de Beule K, Van Vliet A, Donnelly JP, Soons PA (2006) Pharmacokinetics of itraconazole and hydroxyitraconazole in healthy subjects after single and multiple doses of a novel formulation. Antimicrob Agents Chemother 50:4096–4102
Na GC, Stevens HJ, Yuan BO, Rajagopalan N (1999) Physical stability of ethyl diatrizoate nanocrystalline suspension in steam sterilization. Pharm Res 16:569–574
Jacobs C, Muller RH (2002) Production and characterization of a budesonide nanosuspension for pulmonary administration. Pharm Res 19(2):189–94
Hecq J, Deleers M, Fanara D, Vranckx H, Boulanger P, Le Lamer S, Amighi K (2006a) Preparation and in vitro/in vivo evaluation of nano-sized crystals for dissolution rate enhancement of ucb-35440-3, a highly dosed poorlywater-soluble weak base. Eur J Pharm Biopharm 64:360–368
Hecq J, Nollevaux G, Deleers M, Fanara D, Vranckx H, Peulen O, Dandrifosse G, Amighi K (2006b) Nifedipine nanocrystals: pharmacokinetic evaluation in the rat and permeability studies in Caco-2/HT29-5M21 (co)-cultures. J Drug Deliv Sci Technol 16:437–442
Lee J, Cheng Y (2006) Critical freezing rate in freeze drying nanocrystal dispersions. J Control Release 111:185–192
Wiedmann TS, DeCastro L, Wood RW (1997) Nebulization of NanoCrystalsTM: production of a respirable solid-in-liquid-in-air colloidal dispersion. Pharm Res 14:112–116
Liversidge GG, Cundy KC (1995) Particle size reduction for improvement of oral bioavailability of hydrophobic drugs. I. Absolute oral bioavailability of nanocrystalline danazol in beagle dogs. Int J Pharm 125:91–97
Owens DE 3rd, Peppas NA (2006) Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int J Pharm 307(1):93–102
Chien YW, Przybyszewski P, Shami EG (1981) Syringeability of nonaqueous parenteral formulations–development and evaluation of a testing apparatus. J Parenter Sci Technol 35(6):281–4
Dulmage HT, Correa JA, Martinez AJ (1970) Coprecipitation with lactose as a means of recovering the sporte-crystal complex of Bacillus thuringiensis. J Invertebr Pathol 15(1):15–20
Abbott CF, Cockton J, Jones W (1956) Resistance of crystalline substances to gas sterilisation. J Pharm Pharmacol 8(10):709–20
Doyle JE, Ernst RR (1967) Resistance of Bacillus subtilis var. niger spores occluded in water-insoluble crystals to three sterilization agents. Appl Microbiol 15(4):726–30
Mullican CL, Hoffman RK (1968) Dry heat or gaseous chemical resistance of Bacillus subtilis var. niger spores included within water-soluble crystals. Appl Microbiol 16(8):1110–3
Zheng J, Bosch H (1997) Sterile filtration of nanocrystal drug formulations. Drug Dev Ind Pharm 23:1087–1093
Chapter 85, Bacterial Endotoxins Test, The United State Pharmacopoeia, The National Formulary, USP30/NF25, Vol 1, The United State Pharmacopoeial Convection, Rockville, 2007, pp 109–113
Chapter 151, Pyrogen Test, The United State Pharmacopoeia, The National Formulary, USP30/NF25, Vol 1, 2007, pp 135–136
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Controlled Release Society
About this chapter
Cite this chapter
Kumar, S., Burgess, D.J. (2012). Nanosuspensions. In: Wright, J., Burgess, D. (eds) Long Acting Injections and Implants. Advances in Delivery Science and Technology. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-0554-2_13
Download citation
DOI: https://doi.org/10.1007/978-1-4614-0554-2_13
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-0553-5
Online ISBN: 978-1-4614-0554-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)