Abstract
Although a large number of new drug molecules with varied therapeutic potentials have been discovered in the recent decade, yet most of them are still in developmental process. This can be attributed to the limited aqueous solubility which governs the bioavailability of such drug molecules. Hence, there is a requisite for a technology-based product (formulation) in order to overcome such issues without compromising on the therapeutic response. The purpose of this review is to provide an insight to the formulation of drug nanoparticles for enhancing solubility and dissolution velocity with concomitant enhancement in bioavailability. In the recent decade, nanonization has evolved from a concept to reality owing to its versatile applications, especially in the development of drugs having poor solubility. In this review, a relatively simple and scalable approach for the manufacture of drug nanoparticles and latest characterization techniques utilized to evaluate the drug nanoparticles are discussed. The drug nanoparticulate approach described herein provides a general applicability of the platform technology in designing a formulation for drugs associated with poor aqueous solubility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the advent of new technologies in drug discovery and structure-based drug design, there was an exponential increase in the development of new chemical entities with promising therapeutic potentials. However, due to complex chemistry, nearly 40 % of the drug candidates in the developmental stages and about 60 % of newly synthesized drugs are associated with poor water solubility leading to low and inconsistent bioavailability [1, 2]. The poor solubility of drug may result in sub-optimal dosing resulting in a decreased therapeutic response. Even on parenteral administration of these poorly soluble drugs in the form of microsuspensions, it is often difficult to achieve the desired therapeutic activity because of inadequate solute availability at the injection site. There are instances wherein the solubilizing agents used to improve the solubility of drug have resulted in allergic and toxic reactions. For example, Cremphore EL used as solubilizing agent in Taxol® formulation have shown allergic shock as an adverse effect [3].
The commonly used approach to overcome poor aqueous solubility is preparation of salt form of drug that had a limited success. From a formulation prospective, a crystalline salt is preferred foreseeing the potential physical and chemical stability issues associated with an amorphous drug substance. Identification of a crystalline salt with adequate aqueous solubility requires screening of various counter ions and crystallization conditions which is exhaustive. At times, isolation of a pure crystalline material itself is a difficult task. In some instances, the formed salt is highly hygroscopic posing formulation challenges and stability issues during drug product development [4].
Alternatively, drug analogs or prodrugs with enhanced solubility were explored. But, this approach was not successful since the chemically modified drug molecule is often abandoned in its early phase of development or due to the suboptimal properties of the launched drug product which includes effect of food on the absorption rate kinetics, use of excipients in high amounts, deficient optimal dosing, poor bioavailability and ultimately poor therapeutic outcome. Generally, chemical modification methods are expensive compared to manipulation of drug with formulation strategies because once the chemical structure is altered, the associated pharmacological activity may not be same and, moreover, it is expensive to re-establish the safety and efficacy of the chemically modified drug molecule. Therefore, screening of suitable formulation technology is a preferred approach to develop a viable drug product for poorly soluble drugs [5].
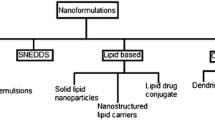
At present, there are limited formulation approaches available to address the problems associated with drug’s poor solubility and bioavailability. Most frequently used approaches include particle size reduction (micronization), inclusion complexation, using lipid carriers (liposomes, self-emulsifying systems) and solid dispersions (in water-soluble carriers) of the drug. Micronization is a process of reducing the average diameter of solid particles. The common technique used in the micronization is the mechanical comminution (e.g., by crushing, grinding and milling). For many years, micronization was successfully used for developing poorly water-soluble drugs. Micronization often results in colloidal drug particles having a particle size >1 μm with less fraction in the sub-micron range. This will result in a moderate enhancement of surface area that may not significantly improve the saturation solubility or dissolution rate so as to impact the bioavailability [6]. In spite of the widespread use of this technique, the milling process does not represent the ideal way for the production of small particles because drug substance properties and surface properties are altered in an uncontrolled manner.
In the inclusion complexation technology, cyclodextrins that are capable of forming inclusion complexes with poorly soluble drugs by entrapping the whole drug molecule or some lipophilic moiety of the molecule into the central cavity are utilized. Incorporation of drug into complexing agents improves the physicochemical properties of the drug molecule. Self-emulsifying systems are isotropic mixtures of oils and surfactants, sometimes containing co-solvents that can spontaneously produce fine oil-in-water emulsions when introduced into an aqueous phase under gentle agitation. These systems can be used for the design of formulations in order to improve the oral absorption of highly lipophilic compounds. However, the success of these systems is mostly dependent on specific properties of drug molecule (ability to ionize, solubility in oils/ lipids, having suitable molecular size, shape and structure to fit into the hydrophobic cavities, etc.) and therefore have limited scope for general application.
Solid dispersions comprise of dispersed drug in an inert carrier or a solid matrix (crystalline or amorphous state). Formation of molecular dispersions (solid solution) provides a means of diminishing the dimensions of drug particles to nearly molecular level. This reduced size of the particle with concomitant increase in surface area results in improved dissolution kinetics and oral absorption. This approach is especially suitable for highly potent compounds with low dose requirement and thus not applicable for drugs with low potency where the dose requirements are relatively high [7]. Liposomes have demonstrated a fair success in formulating poorly soluble drugs; however, because of the poor stability issues and expensive product costs, these approaches were not suitable for all the drug compounds [8]. Hence, a versatile technology is required in order to resolve the product development issues linked with saturation solubility, dissolution velocity and bioavailability enhancement of poorly soluble drugs.
Recent years have marked the gaining interest on nanoparticle formulation technology among the formulation scientists for developing poorly soluble drugs into a viable dosage forms. A significant increase in surface area (40 folds) was observed on reducing the particle size from micro scale to nano scale, i.e. 8 μm to 200 nm [9]. The nanoparticle technology has proven to be promising at all the stages of drug formulation and has opened new avenues for reviving the commercialized products with sub optimal drug delivery. Indeed this technology has been of great value in the development of new chemical entities (NCE’s) especially as a screening tool during the safety and efficacy studies of the early product development phase.
During later drug product developmental stage, the obtained nanoparticulate formulations can be further processed to several types of dosage forms having utmost drug exposure and patient compliance. Nanoparticle technology provides a means to develop a new drug-delivery platform comprising the marketed drug, thus providing new opportunities to address the unmet medical challenges. Research indicates that nanoparticle solutions in drug delivery will capture significant percentage of the total market based on their capability to minimize the product development time for reaching the market with simultaneous extension in product life cycles and a provision of patent protection. The advantages of nanotechnology-based drug delivery include lower drug toxicity, improved bioavailability and reduced cost of treatment. The potential benefits of nanoparticle technology during the drug product development process are depicted in Fig. 1.
Several researchers have reported the benefits of drug nanoparticles. Roya et al. studied the application of nanosuspension and various methods used to prepare nanosuspension [10]. Elaine et al. reported the improved performance of drug nanoparticles and its potential application for oral and parenteral routes [4]. Junghanns et al. reported the potential of nanoparticle technology and its clinical application [6]. However, this overview is majorly focused on drug nanoparticle technology amenable for development of solid dosage forms for poorly soluble drugs, summarizing their preparation methods and their characterization techniques indicating the key issues to be addressed to ascertain that drug nanoparticles can efficiently work in clinical settings, as they are now an established platform technology with considerable acceptance.
Development history
Nanoparticle technology has a long history of development and application. In the early nineteenth century, heterogeneous catalysts were among the first examples reported [11, 12]. The first example of pharmaceutical drug product was Danazol which was formulated using a bead milling process. The resultant nanosuspension has a median particle size of 169 nm and showed an increased oral bioavailability (82.3 ± 10.1 %) when compared with the conventional drug suspension (5.1 ± 1.9 %). Micro fluidization was used in the production of Atovaquone nanoparticles (100–3000 nm) [13]. Rapamune® (Sirolimus), an immunosuppressant developed by Wyeth’s pharmaceuticals using nanoparticle technology, was the first product approved by FDA. An anti-emetic drug, Emend®, was the second product approved by FDA. The subsequent product developed by Abbott Laboratories was Tricor® which was the successor for Fenofibrate following patent expiry. Triglide® was another product containing Fenofibrate nanoparticles developed by Skyepharma with improved product performance. Par Pharmaceutical companies developed Megace ES® (ES stands for enhanced solubility) using nanoparticle technology. Elan nanosystem developed the Megestrol acetate nanosuspension which has reduced the fed and fast variability. Megestrol acetate in the nanosuspension form demonstrated that physical stability of an aqueous nanosuspension can be retained throughout the product shelf life. A list of approved drug products developed by using nanoparticulate approach is summarized in Table 1 [12, 14].
Fabrication of existing drugs with maximal drug exposure, less toxicity, expanded intellectual property by drug life cycle management and minimized competition during the drug’s life time can be achieved through nanoparticle-based drug delivery systems. In fact, viable formulations for poorly soluble drugs with improved bioavailability can be developed potentially by nanoparticle technology, which has opened the stage gates for reviving currently marketed products, leading to better clinical and commercial benefits. Table 2 highlights the key nanoparticle technology-based approach for enhancing the solubility and oral bioavailability of drugs [15].
Formulation theory
The two important parameters governing the in vivo absorption of drug molecules are aqueous solubility and dissolution rate. These parameters have gained paramount importance because absorption plays a significant role in determining the drug’s therapeutic potential. Thus, considering the behaviour of solids in a solvent system, the Noyes-Whitney equation was developed. This theory highlights the importance of surface area and equilibrium solubility of drug molecule in gastrointestinal fluids all through the process of dissolution and absorption.
According to this theory, increased surface area via decreasing particle size has a significant enhancement on the dissolution rate of a poorly soluble drug [5, 16]. Improved dissolution and drug absorption is correlated with increased surface area (due to reduced particle size). Hence, surface properties imparted on the nanosized particles makes nano formulation beneficial in terms of pharmacokinetic properties. The dissolution rate of drug from a nanoparticulate formulation depends mainly on the principle of nanonization, which includes an increased surface area of drug particles. Hence, drugs with low aqueous solubility can be formulated into a nanoparticulate system so as to enhance the pharmacokinetic properties via increased dissolution rate. In addition, intrinsic solubility has a potential influence on the dissolution rate of a drug.
Furthermore, Nernst-Brunner and Levich incorporated Fick’s law of diffusion and modified Noyes-Whitney equation. This dissolution model indicated a direct proportional relation between rate of drug dissolution and surface area.
Where, ν = dx/dt is the dissolution rate of drug, X is the amount of drug dissolved, t is time, A is the effective surface area of the dissolving solid, D is the diffusion coefficient (diffusivity) of the drug, δ is the thickness/distance of the effective diffusion boundary layer, C s is the saturation solubility of the drug in respective medium and V is the volume of dissolution medium.
Apart from surface area, the drug’s saturation solubility has a major effect on the absorption process. Indeed, this saturation solubility depends on temperature and dissolution pressure, i.e. a function of curvature of the nanoparticle surface. The dissolution pressure enhances significantly with the increased curved surface (due to decreased particle size). Moreover, the diffusional distance decreases leading to an increase in the concentration gradient. Thus, as compared to micronized particles, nanoparticles have enhanced saturation solubility and dissolution velocity owing to this increased surface area and concentration gradient [17]. Approaches that improve dissolution rate kinetics can significantly enhance the bioavailability of poorly water-soluble drug molecules.
Formulation of drug nanoparticles
Various techniques have been described for preparing drug nanoparticles which can be classified into ‘bottom-up’ and ‘top-down’ technologies. Controlled precipitation by adding a suitable anti (non)-solvent is involved in bottom-up technology, whereas milling or homogenization methods are grouped under top-down technologies. However, drug nanoparticles are also prepared by the combination technique that includes a pre-treatment followed by size reduction. In some instances, supercritical fluid technologies and solvent evaporation are also used but at present they are less relevant industrially.
Bottom-up technologies
These technologies are also known as precipitation methods and are being used since many years especially in the photographic film development [18, 19]. Since the last decade, these precipitation methods have been successfully applied for the preparation of sub-micron-sized particles for drug delivery applications. Few examples of products prepared by precipitation techniques include Hydrosols developed by Sucker (Sandoz, presently Novartis) and NanoMorph® by Soliqs/Abbott (previously Knoll/ BASF) [20–23].
This process involves the addition of drug to a solvent so as to obtain a solution that is subsequently added to an anti-solvent. This leads to high super saturation followed by rapid nucleation and formation of numerous small nuclei [24]. After solvent elimination, the obtained suspension can be sterile filtered and subsequently lyophilized. The technique behind the formation of very fine particles by the addition of solvent to non-solvent is dependent on the Ostwald-Mier’s supersaturation theory [25]. The mixing processes may vary considerably, and therefore through careful control of this process, particles with a narrow size distribution can be obtained. Amorphous nanocrystals of drug were also produced so as to further improve the solubility and dissolution kinetics of drug [26–29]. Amorphous nanocrystals are often referred to nanocrystals in amorphous state. This technology is used for pharmaceuticals by Soliqs (Ludwigshafen, Germany) and advertised under the trade name NanoMorph®.
Precipitation method was also reported in the food industry for the preparation of amorphous drug nanoparticles, e.g. carotene nanoparticles (Lucarotin® or Lucantin®) [30]. In this process, carotenoid along with surfactant was added to digestible oil. This solution was then mixed with an appropriate solvent along with the addition of a protective colloid so as to obtain an O/W system. The carotenoid gets localized in the oily phase due to the stabilization by the added colloid. Post lyophilisation of this system, X-ray analysis indicated that 90 % of the carotenoids were in amorphous state.
The precipitation technique in comparison to other technologies is relatively simple and requires no expensive equipment. This method does not necessitate high energy process like disintegration; hence, drug degradation can be prevented. However, precipitation methods are associated with many limitations; obtaining a narrow particle size by controlling nucleation and crystal growth is very difficult. Most often, an amorphous (metastable) solid is formed which is then converted to a more stable crystalline form [31, 32]. Furthermore, the precipitation process utilizes non-aqueous solvents because of the limited solubility of many drugs in the aqueous media. Hence, the quantity of non-aqueous solvent used in the end product must be decreased to a minimum so as to meet the acceptable toxicological limits. Thus for the production of nanocrystalline drug particles, top-down technologies are more frequently used instead of bottom-up technologies.
Top-down technologies
In these technologies, the larger particles are size reduced to nanoscale level using the mechanical breakdown process. The two top-down technologies frequently used in the preparation of drug nanoparticles include the following:
-
1.
High pressure homogenization
-
2.
Milling methods
High pressure homogenization technique
High-pressure homogenization is one of the disintegration method used for size reduction. The two homogenization principles/homogenizer types used are as follows:
-
1.
Microfluidizers (Microfluidics, Inc.)
-
2.
Piston-gap homogenizers (e.g. APV Gaulin, Avestin, etc.)
Microfluidization
Microfluidization technique uses high shear forces and impaction to produce the drug nanoparticles. It works on the principle of a jet stream, where the dispersion is passed at a high velocity in a specially designed ‘Y’ and ‘Z’ type homogenization chambers.
In the first type (Y type), the flow of suspension is bifurcated into streams, which are then made to collide head-on resulting in high shear and particle size reduction. In the second type (Z type), size reduction is favoured by the particle collision and shear forces that are brought by the sudden change in the direction of flow of drug suspension. A disadvantage of this technology is its increased process time. This is because the suspension is passed for several times through microfluidizer so as to obtain particles with in sub-micron range. In addition, the obtained microfluidized product may contain a fraction of microparticles especially when hard drugs are used.
Piston-gap technologies
Piston-gap homogenization is the second generation technology that was developed in 1990s. In this process, drug nanoparticles can be produced by performing homogenization in water (DISSO CUBES) [16] or non-aqueous medium or hydro alcoholic medium (NANOPURE). Alternatively, a combination process was also developed that involves the precipitation followed by a homogenization step so as to avoid the particle growth (NANOEDGE) [17, 33].
A high energy input and impact forces are required for effective size reduction. Generally in piston-gap homogenization, higher turbulent energy is produced by way of cavitation. In this process, the suspension is passed through a narrow gap with an extremely high pressure of around 15,000 to 30,000 psi. The width of the gap is very small when compared to the diameter of cylinder in which the suspension is placed (prior to entering the gap). For example in APV LAB 40, the width of gap is 25 mm (can be varied with applied pressure), whereas the cylinder’s diameter is about 3 cm. The resultant size of the particle is a function of the applied pressure and number of homogenization sequences. Increase in temperature during the homogenization process is one of the important parameter which can be controlled by positioning a heat exchanger before the homogenizer valve. A major limitation of high pressure homogenizers is that they are unable to handle dispersions with high solid content (usually >10 % w/w). A schematic mechanism of size reduction by high pressure homogenization technique is represented in Fig. 2.
Milling methods
Traditional micronization techniques are based on friction to reduce particle size. Such methods include milling, pulverizing and grinding. A typical industrial mill is composed of a cylindrical metallic drum that usually contains steel spheres. As the drum rotates, the spheres inside collide with the particles of the drug, thus crushing them into smaller particles. In the case of grinding, the micronized drug particles are formed when the grinding units of the device shear against each other creating attrition between the particles. In 1990, the first generation mill based on disintegration technique was developed by Liversidge which lead to the production of sub-micron particles [34]. Conventional milling methods generally produce larger particles (>1 μm). These milling techniques were later refined to produce solid drug particles of sub-micron range. In the twentieth century, bead mills are employed for the production of fine suspensions. Bead mill works in accordance with the principle of agitation, where grinding media is accelerated in the grinding chamber by an agitator shaft. The energy given to the media is translated to the solid particles by virtue of collision and de-acceleration. Once the desired particle size is achieved, the product and the beads are separated by a separation system (slotted pipe) at the discharge outlet of the mill. In this process, the suspension comprising of drug crystals, surfactant and stabilizers along with milling media are charged into the recirculation chamber (grinding chamber). The particle size reduction mainly occurs due to the high shear forces of impact that are produced due to the agitation of milling media. This method is a low energy milling technique when compared to high energy homogenization technique. Drugs that are insoluble in both aqueous and non-aqueous media can be size reduced by this bead milling technique. The beads are made up of yttrium or cerium stabilized zirconium dioxide, stainless steel, glass or sometimes coated with a highly cross linked polystyrene resin. However, a common problem linked with this technique is metallic contamination of the product (caused by the wearing of milling media during the process). To overcome this issue, the milling beads are often coated [7]. An additional problem with milling process is the product adherence to the inner surface of the milling chamber and surface of the beads. In order to achieve the desired particle size, the milling time may vary from minutes to several hours to days, since it is dependent on various factors like properties and concentration of drug, concentration of surfactant, viscosity of the suspension, energy input, temperature, milling media, etc. [6].
In wet bead milling process, the drug suspension is passed through a grinding chamber containing the milling media (beads) of sizes varying between 0.2 and 3 mm. To achieve the desired particle size, drug concentration in the suspension can be varied from 5 to 40 % w/v. To prevent aggregation/agglomeration of the dispersed particles, stabilizers and surfactants are used in the formulation. Lack of suitable stabilizer leads to particle aggregation owing to the high surface energy of the nanosized particles. The stabilizers act as an energy barrier across the dispersed particles to prevent aggregation or agglomeration. Usually, the optimum concentration of surfactants is <1 % w/v and that for polymeric stabilizers can vary from 0.5 to 10 % w/v. The selection of stabilizers and surfactants largely depends on the physical stabilization (steric versus electrostatic) and route of administration. Generally, steric stabilization is a recommended choice because of its less susceptibility to physiological electrolytes. Electrolytes in the GI tract reduce the surface charge of the drug particles leading to physical instability, especially of ionic surfactants. In some instances, combination of steric and electrostatic stabilization, i.e. a steric stabilizer along with an ionic surfactant, is preferred for stabilization of the drug product. There are various charged surfactants (generally regarded as safe (GRAS)) available in case of drug nanoparticles for oral administration. In order to enhance stability and further processing, various excipients like mannitol, lactose and sugars can be incorporated in the dispersion [17]. A laboratory agitator bead mill (Netzsch®) used in the production of drug nanoparticles is shown in Fig. 3.
After the addition of grinding/milling media (beads) into the milling chamber, the suspension comprising of surfactant and stabilizer is charged into the mill. The milling chamber has a rotor fitted with disks that can be accelerated at a desired speed. The milling media is agitated by the rotation of the rotor disk radially in the chamber. When the product flows axially through the chamber, the beads impact with drug particles and generates high shear forces that act as energy source to split the particles to finer size. The milling process can be operated in a batch mode or in a continuous mode (re-circulation) and by circulating a coolant through the outer jacket can help in controlling the temperature. Using a separation system, the milled product (nanosized) is subsequently separated from the grinding media (beads). A schematic representation of the agitator bead mill is depicted in Fig. 4.
Scaling up the process using bead mills is relatively simple and convenient. This can be achieved by increasing the batch size above the void volume in circulation mode and continuous pumping of the suspension through the mill in a circular motion. The factors such as shaft motor speed, pump speed and bead volume are of paramount important as they not only influence the final particle size but also the process time required to produce the desired product. Nekkanti et al. has reported a pilot-scale study optimizing the process parameters that enable commercial manufacturing of the fenofibrate product using bead mill. In addition, validation was performed at optimal conditions to assess the repeatability and reproducibility of bead milling process for the manufacture of drug nanoparticles with desired quality attributes [35].
Bead mills ranging from laboratory to commercial scale are available in the market. In fact, the ability of the developed technology to produce in large scale is a major prerequisite for the commercialization of product. To sum up, among the drug nanoparticle technologies available, bead milling offers a convenient process for production of nanoparticle dispersion at high concentrations for solid dosage form processing that offers ease of scale-up to enable commercial manufacturing. The pros and cons of nanoparticle technologies are summarized in Table 3 [5].
Conversion of nanosuspension into solid intermediate
The obtained nanosuspension can be converted into a solid intermediate by removing the solvent from the suspension using various drying operations like fluid bed coating, spray drying, lyophilization and spray granulation. Of all these, lyophilization (freeze drying) is considered as a more complex and cost-intensive process predominantly applicable to highly sensitive drug products. The challenge in this process is to retain the dispersibility of the nanoparticles up on reconstitution with water or gastric fluids. If aggregation or agglomeration of drug particles occurs, then the potential benefits obtained from the drug nanoparticles due to increased surface area may be completely lost or compromised. Hence, addition of re-dispersants to the nanosuspensions prior to or during the drying process can be helpful in preventing aggregation. Commonly used re-dispersants are sugars such as sucrose, lactose, mannitol, etc. [36]. The objectives of drug nanoparticle system are to release the drug nanoparticles along the gastrointestinal tract (GIT) as a fine non-aggregated suspension following oral administration with concomitant increase in the physical stability of the drug product on long storage [37]. For drugs that can withstand high temperatures, the most suitable method is spray drying. A schematic representation of the spray dryer is shown in Fig. 5. Depending on the formula composition and spraying conditions, the obtained dry powders can easily be filled into capsules or blended with extra granular excipients and compressed into tablets [38]. In the case of drugs which are susceptible to gastric fluids, technique like coating the tablet or capsule with enteric polymers can help in protecting the drug from gastric environment.
An alternative way to convert nanosuspension into solid intermediate is the suspension layering on to an inert solid carrier such as sugar beads, lactose, cellulose derivatives, etc. [39]. The suspensions can be layered on to the carrier (water soluble or insoluble) at a predetermined spray rate using a top spray fluid bed process. A schematic representation of the fluid bed granulator is shown in Fig. 6. The granules are suspended in air stream as they move up while the suspension is sprayed from top of the system onto the fluidized bed, resulting in uniformly sized particles/granules.
Characterization of drug nanoparticles
Characterization of drug nanoparticles is mainly performed to understand the behaviour of the drug product during manufacturing processes and to have better control of the product quality. Various techniques have been reported for the characterization of drug nanoparticles. But no single method can be considered as the “best” for analysis, since various parameters like data requirement, nature of sampling, time and cost of analysis are to be considered while selecting a specific method. The following methods are used for characterization of drug nanoparticles [40].
Particle size distribution
Measurement of particle size and understanding its effects on the product and processes are of paramount importance for the success of a manufacturing industry. The particle size characterization is primarily performed to obtain information about the changes in average particle size and its distribution during the manufacturing process and on long storage (e.g. aggregation or agglomeration). Size distribution of drug nanoparticles can be measured using the following techniques.
Photon correlation spectroscopy
Photon correlation spectroscopy is one of the most widely used light scattering techniques for measuring particle size and its distribution. This is based on the principle of dynamic light scattering, where fluctuations in the intensity of scattered light are measured. When a laser beam is passed through the sample suspension, then it (light) gets diffracted due to the random motion (Brownian movement) of sub-micron-sized particles. This leads to rapid fluctuations in the scattered intensity of the beam. These variations in light intensities are correlated to the diffusion coefficient of the particles that can be converted to particle size.
The extent of increase in the particle size is a measure for the extent of instability of the suspension. Therefore, photon correlation spectroscopy (PCS) is considered as a reliable technique to detect the instabilities during storage [41]. This technique can be used to determine the average size of particles ranging from 3 to 3000 nm. In addition, a polydispersity index (PI) can be obtained so as to measure the width of the distribution. If PI = 0, then it indicates a monodisperse particle population. In case of narrow distribution, the PI values are around 0.10–0.20 and if PI ≥ 0.5, it indicates a very broad distributions. Checking the values of mean particle size (z average) and PI, the changes in nanoparticles size with time can be measured.
Laser diffraction
Laser diffractometry (LD) was developed around 1980 and is used as a routine method in many research laboratories. When a laser beam is passed thought a sample containing colloidal particles (sub-micron range), then diffraction of light occurs and LD measures the angular variation in intensities of the light scattered. This data relating to the intensity of angular scattering is analysed to calculate the particle size, using the Mie theory of light scattering. Relative to the laser beam, large angled scattering is observed with small particles where as small angled scattering is observed with larger particles. This theory takes into account the optical properties such as refractive index and imaginary component of the test samples as well as the dispersant’s refractive index value. Unfortunately for most of the pharmaceutical solids, the refractive indices are unknown. However, because of its simplicity, laser diffractometry is frequently used as the second characterization method for drug nanoparticles.
Dynamic light scattering
Dynamic light scattering (DLS) is a technique that can be used to determine the size distribution profile of small particles in a suspension. It is a powerful light-scattering technique for studying the properties of suspensions and solutions of colloids, macromolecules and polymers that are absolute, non-invasive and non-destructive. The time decay of the near-order of the particles caused by the Brownian motion is used to evaluate the size of nanoparticles applying the Stokes-Einstein relation.
Morphology
Microscopy-based techniques are considered as most direct measurements of particle size and morphology. A wide range of materials having a broad particle size distribution ranging from nanometre to millimetre can be studied using this technique. Instruments used in this technique include optical light microscopes, electron microscopes (scanning (SEM) and transmission (TEM)) and atomic force microscopes (AFM). Particle size range, magnification and resolution are the key factors to be considered while selecting an instrument for evaluation. However, the cost of analysis is increased exponentially as the size of the particles decreases due to requirements of higher magnification, improved resolution, greater reliability and reproducibility. The analysis cost also depends upon the instrument being studied, as it dictates the techniques of sample preparation and image analysis. Optical microscopes tend to be more affordable, comparatively simple to operate and maintain as compared to electron microscopes, but have a drawback of limited magnification and resolution. The surface morphology of un-milled drug and spray-coated nanoparticles for a poorly soluble drug, camptothecin analog, examined using scanning electron microscope (Hitachi S-520SEM, Tokyo, Japan) is shown in Fig. 7 [42].
SEM micrographs of un-milled camptothecin analog (left); spray-coated nanoparticles (right). Reproduced with permission from Inventi Journals (P) Ltd., from reference [42]
Zeta potential
The interactions occurring between nanoparticles are measured by the surface charge density (zeta potential). In fact, charge on the particle plays a vital role in defining the stability of nanosuspensions. The higher the number of equally charged particles, the greater is the electrostatic repulsion between them and the longer is the physical stability. Typically, charge on the particle can be quantified as zeta potential that can be measured via the electrophoretic mobility of the particles in an electrical field. In order to formulate a stabilized nanosuspension, a zeta potential of −20 mV for sterically stabilized systems and −30 mV for electrostatically stabilized systems is desirable [43].
Solid state properties
Differential scanning calorimetry
Measuring the melting temperature, glass transition temperature and their associated enthalpies can be helpful in determining the nature of crystallinity within the drug nanoparticles. This can be accomplished by using differential scanning calorimetry (DSC). The extent of which multiple phases exist in the interior and their corresponding interactions with the drug can be determined using this method along with X-ray powder diffraction (XRPD).
X-ray powder diffraction
Crystalline or polycrystalline materials can be investigated using XRPD. When a beam of X-rays is passed through a sample, then some part of it gets diffracted by the atoms of the material. This leads to constructive interference of X-rays with each other. Using Bragg’s law, this interference can be studied so as to determine the crystallinity of the materials [43].
Saturation solubility
Determination of saturation solubility of nanoparticles is very important not only in assessing the advantages (as compared to microparticles) but also in predicting the in vivo performances such as plasma levels and bioavailability following dosage administration. Shake flask method is used to investigate the saturation solubility of drug nanoparticles in different buffer media at varied pH conditions. Indeed, particle size and crystallinity of the drug molecule have a marked role in governing the saturation solubility [44].
In vitro dissolution
An important step in the characterization of drug nanoparticle formulations is in vitro dissolution studies. Drug nanoparticles have been used as a drug delivery tool to improve the solubility and/or dissolution rate kinetics of poorly water-soluble drugs. Hence, it is important to know the dissolution profile of the prepared formulation in a physiologically discriminating dissolution media. This will help in understanding the rate and extent of drug release and absorption characteristics from the administered dosage form in vivo. In general, selection of release media for nanoparticle formulation is generally based on drug solubility and stability, assay sensitivity and the analytical method used. Although maintenance of sink conditions using surfactants and/or buffers is preferable, non-sink conditions have also been reported. Agitation of the dissolution media that is frequently employed to prevent aggregation of nanoparticles during an in vitro release study will in turn depend on the apparatus used. Similarly, sampling and media replacement (total or partial) techniques are also used depending on the type of method selected. As such, drug release from nano-sized dosage forms can be measured using one of the following three categories: (a) conventional dissolution method (UPS types 1 and II), (b) continuous flow apparatus (USP IV) and (c) dialysis membrane methods. More recently, apparatus that combine the principles of conventional and continuous flow or dialysis membrane has also been reported. Lastly, a few novel methods that use voltammetry, turbidimetry, and so forth are discussed.
Conventional dissolution methods
In general, the conventional dissolution method (UPS types 1 and II) provides a direct approach to monitor drug release. With this method, most sample set-ups, agitation modes and sampling techniques are straightforward and simple. Commonly reported set-ups include USP I (basket) and USP II (paddle) [45–47]. Several researchers have reported the use of syringe filters to separate the nanoparticles from the samples of release media; alternately, high energy separation techniques like centrifugation, ultracentrifugation and ultrafiltration can also be used for separation [48–50]. After sampling, an equal amount of fresh release media or buffer is replenished to maintain sink conditions during the study.
Continuous flow apparatus
In this method, drug release from the nanoparticulate dosage form is monitored using the USP IV dissolution apparatus. Drug release occurs as a result of buffer or media constantly circulating through a column containing the immobilized dosage form and the concentration of drug is measured by drawing the samples at predetermined intervals [46, 51].
Dialysis membrane method
Among the dissolution methods, the dialysis method is the most versatile and widely accepted. In this method, physical separation of the dosage forms is achieved by usage of a dialysis membrane which allows for ease of sampling at periodic intervals. Several modifications of the dialysis membrane method have been reported in literature with alterations in set-up, container size and molecular weight cut-off [52, 53]. A few alternate approaches have also been utilized to monitor drug release. A majority of these appear to be targeted towards electroactive drugs. Electrochemical methods offer the possibility of rapid in situ measurements while avoiding the interference caused by the presence of undissolved dosage form in the release media [54]. Differential pulse polarography was used to assess continuous drug release from Piroxicam, Chloramphenicol and Diazepam [55, 56]. Non-electrochemical methods like calorimetry, turbidimetry and laser diffraction have also been evaluated as in vitro release methods. Solution calorimetry was employed by Kayaert et al. during in vitro release measurement of Naproxen and Cinnarizine [57]; Helle et al. designed a novel online system for evaluating the drug release from Indomethacin and Beclomethasone dipropionate nanoparticles. In this method, nanoparticles are packed into small column which is connected to multiport modulation valve attached to an HPLC system allowing for rapid analysis [58]. Microdialysis, another set-up utilized to measure drug release from nanoparticles, is based on passive diffusion of drug through a concentration gradient across a semipermeable membrane [59].
In vivo pharmacokinetic studies
The in vivo pharmacokinetic studies including drug release kinetics from the administered dosage form, absorption, distribution and elimination are evaluated by dosing the nanoparticulate formulation in suitable animal model or human subjects. The in vivo pharmacokinetic studies provide a mathematical platform to estimate the time course of drug and its effects in vivo. Nekkanti et al. reported the effect of particle size of camptothecin analog following oral administration in male Wistar rats. The results indicated a 7.32-fold increase in area under the curve (AUC0-t) and 7.27-fold increase in maximum concentration (C max) for the nanoparticle suspension over the micronized suspension (Fig. 8). The increase in rate and extent of absorption for the nanoparticle dispersion could be attributed to the increase in the rate and extent of drug dissolution in the GI tract [42].
Plasma concentration–time profiles following oral administration of micronized suspension and drug nanosuspension to male Wister rats. Reproduced with permission from Inventi Journals (P) Ltd., from reference [42]
Conclusion
Drug nanoparticle technology can be applied to poorly soluble compounds to overcome their solubility and bioavailability problems. The decrease in particle size to nanometre range contributes to the increased surface area, saturation solubility, dissolution velocity and further improved bioavailability. In the recent years, many investigations on drug nanoparticles demonstrated excellent in vivo performances of poorly soluble drugs. Upon oral administration, drug nanoparticles offer great benefits of enhanced drug bioavailability. Additionally, drug nanoparticles allow rapid absorption of drug due to the enhanced dissolution resulting in rapid onset of action. At present, drug nanoparticles are gaining attention as a promising approach owing to increasing number of poorly soluble drugs in drug discovery process, pharmaco-economic value, production feasibility and safer composition.
Future trends
In the future, development of active targeting of drug nanoparticles by altering the functional surface will be the next essential part of investigation so as to enable site-specific delivery. The surface modification of nanoparticles may significantly impact the drug adsorption pattern and regulates the cellular uptake. Conceptually nanoparticle technology-based products are expected to revolutionize the field of modern medicine. It is believed that nanoparticles will provide potential solutions to encounter the problems emerging from pharmaceutical industry’s drug discovery pipeline. Further advancements in nanoparticle technology will spur the complete evolvement of drug nanoparticles as potential drug delivery system.
References
Lipinski C. Avoiding investment in doomed drugs, is poor solubility an industry wide problem. Curr Drug Dis. 2001;4:17–9.
Lipinski CA. Poor aqueous solubility—an industry wide problem in ADME screening. Am Pharm Rev. 2002;5:82–5.
Müller RH, Peters K. Nanosuspensions for the formulation of poorly soluble drugs: I. Preparation by a size-reduction technique. Int J Pharm. 1998;160(2):229–37.
Merisko-Liversidge EM, Liversidge GG. Drug nanoparticles: formulating poorly water-soluble compounds. Toxicol Pathol. 2008;36(1):43–8.
Gao L, Zhang D, Chen M. Drug nanocrystals for the formulation of poorly soluble drugs and its application as a potential drug delivery system. J Nanoparticle Res. 2008;10(5):845–62.
Junghanns J-UA, Müller RH. Nanocrystal technology, drug delivery and clinical applications. Int J Nanomedicine. 2008;3(3):295.
Merisko-Liversidge E, Liversidge GG, Cooper ER. Nanosizing: a formulation approach for poorly-water-soluble compounds. Eur J Pharm Sci. 2003;18(2):113–20.
Mohammed A, Weston N, Coombes A, Fitzgerald M, Perrie Y. Liposome formulation of poorly water soluble drugs: optimisation of drug loading and ESEM analysis of stability. Int J Pharm. 2004;285(1):23–34.
Liversidge GG, Cundy KC. Particle size reduction for improvement of oral bioavailability of hydrophobic drugs: I. Absolute oral bioavailability of nanocrystalline danazol in beagle dogs. Int J Pharm. 1995;125(1):91–7.
Yadollahi R, Vasilev K, Simovic S. Nanosuspension technologies for delivery of poorly soluble drugs. J Nanomater. 2014.
Rogers T, Johnston K, Williams III R. A comprehensive review: solution-based particle formation of pharmaceutical powders by supercritical or compressed fluid CO2 and cryogenic spray-freezing technologies. Drug Dev Ind Pharm. 2001;27(10):1003–16.
Shegokar R, Müller RH. Nanocrystals: industrially feasible multifunctional formulation technology for poorly soluble actives. Int J Pharm. 2010;399(1):129–39.
Robertson A. The development of ideas on heterogeneous catalysis. Platinum Metals Rev. 1983;27:31–9.
Dubey R. Impact of nanosuspension technology on drug discovery and development. Drug Deliv Technol. 2006;6(5):67–71.
Saffie-Siebert R, Ogden J, Parry-Billings M. Nanotechnology approaches to solving the problems of poorly water-soluble drugs. Drug Discov World. 2005;6(3):71.
Müller R, Dingler A, Schneppe T, Gohla S. Large scale production of solid lipid nanoparticles (SLN™) and nanosuspensions (DissoCubes™). Handbook of Pharmaceutical Controlled Release Technology. New York: Marcel Dekker; 2000. p. 359–76.
Keck CM, Müller RH. Drug nanocrystals of poorly soluble drugs produced by high pressure homogenisation. Eur J Pharm Biopharm. 2006;62(1):3–16.
Otsuka M, Kaneniwa N. Effect of seed crystals on solid‐state transformation of polymorphs of chloramphenicol palmitate during grinding1. J Pharm Sci. 1986;75(5):506–11.
Illingsworth BD. Preparation of silver halide grains. Google Patents; 1972.
Keritsis GD. Precipitation of metal salts. Google Patents; 1985.
Sjöström B, Bergenståhl B, Kronberg B. A method for the preparation of submicron particles of sparingly water‐soluble drugs by precipitation in oil‐in‐water emulsions. II: influence of the emulsifier, the solvent, and the drug substance. J Pharm Sci. 1993;82(6):584–9.
Gassmann P, List M, Schweitzer A, Sucker H. Hydrosols: alternatives for the parenteral application of poorly water soluble drugs. Eur J Pharm Biopharm. 1994;40(2):64–72.
Sucker H, Gassmann P. Improvements in pharmaceutical compositions. GB Patent A. 1994;2269536:1994.
Kipp JE, Wong JCT, Doty MJ, Rebbeck CL. Microprecipitation method for preparing submicron suspensions. Google Patents; 2003.
Mahajan AJ, Kirwan D. Rapid precipitation of biochemicals. J Phys D Appl Phys. 1993;26(8B):B176.
Müller RH, Böhm BH. Dispersion techniques for laboratory and industrial scale processing: Wissenschaftliche Verlagsgesellschaft; 2001.
Lonare AA, Patel SR. Antisolvent crystallization of poorly water soluble drugs. Int J Chem Eng Appl. 2013;4:337–41.
Thorat AA, Dalvi SV. Liquid antisolvent precipitation and stabilization of nanoparticles of poorly water soluble drugs in aqueous suspensions: recent developments and future perspective. Chem Eng J. 2012;181:1–34.
Matteucci ME, Hotze MA, Johnston KP, Williams RO. Drug nanoparticles by antisolvent precipitation: mixing energy versus surfactant stabilization. Langmuir. 2006;22(21):8951–9.
Shackleford DM, Faassen WF, Houwing N, Lass H, Edwards GA, Porter CJ, et al. Contribution of lymphatically transported testosterone undecanoate to the systemic exposure of testosterone after oral administration of two andriol formulations in conscious lymph duct-cannulated dogs. J Pharmacol Exp Ther. 2003;306(3):925–33.
Violanto MR. Method for making uniformly sized particles from water-insoluble organic compounds. Google Patents; 1989.
Bruno JA, Doty BD, Gustow E, Illig KJ, Rajagopalan N, Sarpotdar P. Method of grinding pharmaceutical substances. Google Patents; 1996.
Nekkanti V, Venkateswarlu V, Akhter Ansari K, Pillai R. Development and pharmacological evaluation of a PEG based nanoparticulate camptothecin analog for oral administration. Curr Drug Deliv. 2011;8(6):661–6.
Liversidge GG, Cundy KC, Bishop JF, Czekai DA. Dispersion, bioavailability. Google Patents; 1992.
Nekkanti V, Marwah A, Pillai R. Media milling process optimization for manufacture of drug nanoparticles using design of experiments (DOE). Drug Devel Ind Pharm. 2013;41(1):124–30.
Chu B, Liu T. Characterization of nanoparticles by scattering techniques. J Nanoparticle Res. 2000;2(1):29–41.
Jain RA, Ruddy SB, Cumming KI, Clancy MJA, Codd JE. Rapidly disintegrating solid oral dosage form. Google Patents; 2001.
Nekkanti V, Pillai R, Venkateshwarlu V, Harisudhan T. Development and characterization of solid oral dosage form incorporating candesartan nanoparticles. Pharm Dev Technol. 2009;14(3):290–8.
Vijaykumar N, Venkateswarlu V, Raviraj P. Development of oral tablet dosage form incorporating drug nanoparticles. Res J Pharm Biol Chem Sci. 2010;1:952–63.
Nekkanti V, Pillai R, Vabalaboina V. Drug nanoparticles-an overview: INTECH Open Access Publisher; 2012.
Kerker M. The scattering of light and other electromagnetic radiation: physical chemistry: a series of monographs. New York: Academic Press; 2013.
Nekkanti V, Venkateswarlu V, Harisudhan T, Pillai R. Development and characterization of solid dosage form incorporating camptothecin analog nanoparticles. Inventi Impact: Pharm Tech. 2010; 1(2).
Hunter RJ. Zeta potential in colloid science: principles and applications. New York: Academic Press; 2013.
Böhm BH, Müller RH. Lab-scale production unit design for nanosuspensions of sparingly soluble cytotoxic drugs. Pharm Sci Technol Today. 1999;2(8):336–9.
Cetin M, Atila A, Kadioglu Y. Formulation and in vitro characterization of Eudragit® L100 and Eudragit® L100-PLGA nanoparticles containing diclofenac sodium. Aaps Pharmscitech. 2010;11(3):1250–6.
Heng D, Cutler DJ, Chan H-K, Yun J, Raper JA. What is a suitable dissolution method for drug nanoparticles? Pharm Res. 2008;25(7):1696–701.
Sanna V, Roggio AM, Siliani S, Piccinini M, Marceddu S, Mariani A, et al. Development of novel cationic chitosan-and anionic alginate-coated poly (D, L-lactide-co-glycolide) nanoparticles for controlled release and light protection of resveratrol. Int J Nanomedicine. 2012;7:5501.
Danhier F, Lecouturier N, Vroman B, Jérôme C, Marchand-Brynaert J, Feron O, et al. Paclitaxel-loaded PEGylated PLGA-based nanoparticles: in vitro and in vivo evaluation. J Control Release. 2009;133(1):11–7.
Wallace SJ, Li J, Nation RL, Boyd BJ. Drug release from nanomedicines: selection of appropriate encapsulation and release methodology. Drug Deliv Transl Res. 2012;2(4):284–92.
Juenemann D, Jantratid E, Wagner C, Reppas C, Vertzoni M, Dressman JB. Biorelevant in vitro dissolution testing of products containing micronized or nanosized fenofibrate with a view to predicting plasma profiles. Eur J Pharm Biopharm. 2011;77(2):257–64.
Sievens-Figueroa L, Pandya N, Bhakay A, Keyvan G, Michniak-Kohn B, Bilgili E, et al. Using USP I and USP IV for discriminating dissolution rates of nano-and microparticle-loaded pharmaceutical strip-films. Aaps Pharmscitech. 2012;13(4):1473–82.
Chidambaram N, Burgess D. A novel in vitro release method for submicron-sized dispersed systems. AAPS PharmSci. 1999;1(3):32–40.
Calvo P, Vila‐Jato JL, Alonso MJ. Comparative in vitro evaluation of several colloidal systems, nanoparticles, nanocapsules, and nanoemulsions, as ocular drug carriers. J Pharm Sci. 1996;85(5):530–6.
Tan JP, Goh CH, Tam KC. Comparative drug release studies of two cationic drugs from pH-responsive nanogels. Eur J Pharm Sci. 2007;32(4):340–8.
Rosenblatt KM, Douroumis D, Bunjes H. Drug release from differently structured monoolein/poloxamer nanodispersions studied with differential pulse polarography and ultrafiltration at low pressure. J Pharm Sci. 2007;96(6):1564–75.
Charalampopoulos N, Avgoustakis K, Kontoyannis CG. Differential pulse polarography: a suitable technique for monitoring drug release from polymeric nanoparticle dispersions. Anal Chim Acta. 2003;491(1):57–62.
Kayaert P, Li B, Jimidar I, Rombaut P, Ahssini F, Van den Mooter G. Solution calorimetry as an alternative approach for dissolution testing of nanosuspensions. Eur J Pharm Biopharm. 2010;76(3):507–13.
Helle A, Hirsjärvi S, Peltonen L, Hirvonen J, Wiedmer SK, Hyötyläinen T. Novel, dynamic on-line analytical separation system for dissolution of drugs from poly (lactic acid) nanoparticles. J Pharm Biomed Anal. 2010;51(1):125–30.
Borkar N, Xia D, Holm R, Gan Y, Müllertz A, Yang M, et al. Investigating the correlation between in vivo absorption and in vitro release of fenofibrate from lipid matrix particles in biorelevant medium. Eur J Pharm Sci. 2014;51:204–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) confirm that this article content has no conflict of interest.
Rights and permissions
About this article
Cite this article
Kalepu, S., Nekkanti, V. Improved delivery of poorly soluble compounds using nanoparticle technology: a review. Drug Deliv. and Transl. Res. 6, 319–332 (2016). https://doi.org/10.1007/s13346-016-0283-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-016-0283-1