Abstract
Reactive oxygen species (ROS) have long been considered as one of the major regulatory factors for the intracellular and intercellular signaling cascades. The sensitive redox balance that is controlled through an improved antioxidant system along with the enzymatic and non-enzymatic ROS production pathways sustains physiological functions in the healthy cells. During the course of cancer, a progressive deterioration of the redox balance can be followed via the overproduction of ROS, and results in the formation of malignant phenotype through induction of cancer hallmarks, including death evasion, uncontrolled proliferation, deregulating the cellular energetics, evading the immune response, provoking inflammation, inducing genome instability and mutations, developing drug resistance, angiogenesis, invasiveness, and metastasis. Apart from the carcinogenic roles of ROS, they have been employed as a target, mediator, and weapon in cancer treatment modalities because of the characteristic features considered as a double-edged sword. This chapter has consequently purposed to indicate the sophisticated roles, contributions, activities, and importance of ROS in the progression of cancer and cancer treatment strategies, and drawn the attention of scientists more to enhance the research on the complicated and versatile relationship between ROS and cancer.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Although a mass effort of scientists and the considerable research budgets have been drained to find the convenient cure, drugs, and treatment strategies for cancer diseases, cancer is still ranked as the second leading cause of death and considered as a major public health problem worldwide [1]. The most recent global cancer statics showed that there was an estimated 18.1 million new cancer cases and 9.6 million cancer deaths in 2018, and this bitter truth reminds us once again the importance of the scientific research on the mechanisms of carcinogenesis, cancer treatment strategies, and drugs [2]. It is well known that carcinogenesis is a prolonged, complicated, and multi-stage process that can be induced by the harmful environmental factors along with the genetic predispositions [3,4,5]. Because of the stress occurring in microenvironment, carcinogenesis begins with malignant transformation of some cells in the organism, and the malign transformation of these cells is followed by hyperproliferation, insensitivity to the growth suppressing factors (evasion), resistance to the programmed cell death (apoptosis), invasiveness, production of angiogenic factors to induce the formation of new capillary vessels from the existing ones (angiogenesis), and finally gaining metastatic ability, which is defined as the ability to reach different parts of the organism through veins [6, 7]. Additionally, the irregularities in the cellular energetics and the escape from the immune system are also considered as the substantial parts of carcinogenesis [6, 8]. Although the process of carcinogenesis is common for almost all cancer diseases, it has been demonstrated that there are more than 200 types of cancer, and a tumor tissue exhibits a morphologically and functionally heterogeneous structure that consists of various cancer cells with different physiological characters, mutations, and epigenetic profiles [9,10,11,12]. Thus, understanding the underlying mechanisms of cancer hallmarks has a great importance to find the convenient cure, drugs, and treatment strategies for cancer diseases. It is well known that the cellular levels of oxygen molecules, reactive oxygen species (ROS), and antioxidants have a balance in the healthy cells located in a homeostatic microenvironment [13,14,15]. However, this balance observed in the homeostatic microenvironment can be disrupted in the progress of some diseases such as cancer, diabetes, neurodegenerative diseases, premature aging, and obesity [16,17,18,19]. The disruption of the balance between ROS and antioxidant molecules is considered as a leading factor for many intracellular and intercellular problems such as the disruption of mitochondrial metabolism and cellular energetics, the occurrence of the unstable and hypoxic microenvironment, and the alteration of molecular pathways [20,21,22]. Moreover, it is well known that reactive oxygen species and oxidative stress play key roles in the progress of carcinogenesis and effect the all cancer hallmarks [23]. Therefore, understanding the complicated and sophisticated roles of oxidative stress and reactive oxygen species has an exclusive place in cancer biology and anticancer therapy [24,25,26].
6.2 Cellular Sources and Regulation of ROS
Although all living aerobic organisms need molecular oxygen vitally for their cellular respiration as a central molecule, the oxygen-containing free radicals were determined as toxic compounds for aerobic organisms by Gerschman and coworkers [27, 28]. It is well known today that the increased levels of reactive oxygen species (ROS) take disruptive effects on the function, homeostasis, and structure of cells by inducing oxidative stress and lead to the development of various pathologies such as inflammatory, cardiovascular, and neurodegenerative diseases, age-related disorders, and cancer [22, 29]. Cancer cells are characterized by the overproduction of ROS both in the various cellular compartments and in the cancer cell microenvironment, and this overproduction can alter the genetic stability of cells along with many cellular processes [30,31,32]. Although there is a certain balance between ROS and antioxidant factors in the healthy cells, the balance can be disrupted by endogenous and exogenous ROS generators leading to the excessive ROS production or the antioxidant defenses limitation [33, 34]. The endogenous ROS generators can be listed as mitochondria, peroxisomes, endoplasmic reticulum, transition metal ions, lipoxygenases, cytochrome P450, and NADPH oxidase, though the exogenous ROS generators are ionizing radiation, ultraviolet rays, chemotherapeutics, environmental toxins, and inflammatory cytokines [29, 35]. Reactive oxygen species can be observed as radicals that have at least one unpaired electron, and chemically reactive non-radical species without unpaired electron [36]. The non-radical species such as singlet oxygen (1O2), ozone (O3), hydrogen peroxide (H2O2), hypochlorous acid (HOCl) can be converted to radical ones, though the short-lived and highly electrophilic radicals such as hydroxyl (OH•), superoxide (O2•−), and peroxyl (RO2 •) molecules show substantial cytotoxic activity by oxidizing proteins, lipids, nucleic acids, and other cellular molecules [37,38,39]. The generation of ROS in biological systems can be eventuated by enzymatic and non-enzymatic reactions, and the enzymatic generation of ROS can be achieved by the contribution of the cytochrome P450 enzymes, arachidonic acid, cyclooxygenase (COX), lipoxygenase (LOX), xanthine oxidase (XO), uncoupled endothelial nitric oxide synthase (eNOS), and NADPH oxidases (NOXs) [39,40,41]. Superoxide anion radicals that are considered as the primary reactive oxygen species are formed by transferring one electron to the molecular oxygen (O2), and so the further interaction to generate other reactive oxygen species can be occurred, such as the formation of hydrogen peroxide (H2O2), which can be generated spontaneously or by the effect of the superoxide dismutase enzyme (SOD). Moreover, hydrogen peroxide can be converted to the highly toxic hydroxyl radicals (OH•) through the iron-catalyzed Fenton reaction, and leads to the cellular damage and genomic instability due to the formation of oxidized proteins, lipids, and nucleic acids [37, 42]. Apart from the enzymatic ROS generation, ROS can be non-enzymatically generated by the mitochondrial respiratory chain [43]. During the aerobic respiration, the oxygen molecules are reduced to water in the electron transport chain by cytochrome-c oxidase, though approximately 1–2% of the oxygen molecules are reduced to superoxide (O2•−) because of the electron leakage from the electron transport steps of ATP production [29]. Then, the formed superoxide radicals can be converted by the effect of SOD enzymes to the hydrogen peroxide molecules, which can be further converted to the hydroxyl radicals (OH•) through the Fe2+ or Cu2+ ions-catalyzed Fenton reactions (Fig. 6.1) [31, 36, 44]. Although mitochondria is widely considered as the major source of ROS, mitochondria-generated ROS production may have been overestimated due to the generation of functional damages during the mitochondrial isolation procedures, and performing the new techniques showed that there are much lesser amounts of mitochondria-generated ROS than the previously estimated amounts [36, 45].
Oxidant and antioxidant pathways for ROS homeostasis. O2−• (superoxide radical), OH• (hydroxyl radical), ONOO− (peroxynitrite), H2O2 (hydrogen peroxide), H2O (water), COX (cyclooxygenase), eNOS (endothelial nitric oxide synthase), NO (nitric oxide), SOD (superoxide dismutase), PRX (peroxiredoxins), TRX (thioredoxin reductase), and GPx (glutathione peroxidases)
The membrane-bound NADPH oxidases (NOXs) are also considered as another major source of superoxide radicals [46, 47]. NOXs can be found on the membranes of plasma, nucleus, mitochondria, and endoplasmic reticulum, and so NOXs-catalyzed reduction of oxygen molecules into superoxide radicals can be observed where these membranes are located, and NOX-derived superoxide radical that could not diffuse across membranes can be further converted by SODs into hydrogen peroxides, which have an ability to diffuse across membranes as redox signaling molecules (Fig. 6.1) [31, 37, 48]. Peroxisome organelles are recognized as an another prominent source of ROS by generating superoxide radical, hydrogen peroxide, hydroxyl radical, nitric oxide (NO•), and peroxynitrite (ONOO−) through the reduced catalase (CAT) activity, which has been reported in many cancers such as hepatocellular carcinoma, prostate, lung, colon, and kidney cancers [29]. Another organelle, which is ROS source, is endoplasmic reticulum that has many cellular functions including calcium storage, lipid metabolism and the synthesis, folding, posttranslational modifications, and transport of proteins [49]. Along with the NOX-derived ROS production over the membrane of the endoplasmic reticulum, the accumulation of unfolded and misfolded proteins in the lumen of endoplasmic reticulum due to the alterations in the protein folding pathways may lead to endoplasmic reticulum stress that triggers the ROS production, and the increased levels of ROS in endoplasmic reticulum induce endoplasmic reticulum stress [50, 51]. Although the endogenous and exogenous ROS generators increase the ROS levels in cells, the antioxidant defense factors maintain the ROS homeostasis [25]. The antioxidant defense components include antioxidant enzymes (e.g., catalase (CAT), glutathione peroxidases (GPXs), glutathione reductase (Gr), peroxiredoxins (PRXs), superoxide dismutase (SOD), and thioredoxin reductase (TRX)), antioxidant molecules (e.g., alpha-lipoic acid, bilirubin, coenzyme Q, ferritin, glutathione, l-carnitine, metallothionein, melatonin, and uric acid), dietary natural products (e.g., ascorbic acid, β-carotene, polyphenol metabolites, selenium, and tocopherol), and synthetic products (e.g., butylated hydroxytoluene, N-acetyl cysteine (NAC), and tiron) [36].
6.3 ROS in Cancer Cell Proliferation and Survival
It has been well established that ROS play a key role in mitogenic signaling cascades by prolonging activation of growth factors and boosting levels of cellular signaling factors [52,53,54]. The proliferation of many cancers such as lung, liver, and breast cancers can be enhanced by the increased ROS level though the proliferation of these cancers can be alleviated by the administration of antioxidants [55]. The metabolism of cancer cells is commonly very active because of the oncogenic signals such as Bcr-Abl, c-Myc, and Ras oncogenes-related signals, and these oncogenic signals can also increase endogenous ROS generation without the induction of apoptosis [26, 56, 57]. Oncogenic Ras mutations, for instance, induce ROS generation through NOX isoform (NOX4) that improves cell proliferation, and K-Ras oncoprotein upregulates the pro-proliferative signal epidermal growth factor receptor (EGFR) by elevating mitochondrial ROS production [31, 58]. Thus, it is widely considered that the oncogene-induced ROS generation positively regulates cancer cell proliferation by promoting mitogenic signaling cascades such as protein kinase D (PKD), mitogen activated-protein kinase/extracellular-regulated kinase 1/2 (MAPK/ERK 1/2), and phosphoinositide-3-kinase/protein kinase B (PI3K/Akt) signaling pathways (Fig. 6.2) [52]. For example, increased ROS level inhibits MAPK by oxidation of cysteine residues in the active site and the degradation of MAPK phosphatase 3 (MPK3) prominently reduces ERK 1/2 activity [59]. Similar to the inhibition of MAPK phosphatases, the protein tyrosine phosphatase 1B (PTP1B), phosphatase and tensin homolog (PTEN) protein, and ubiquitin ligase are negatively regulated by the increased level of ROS via oxidation of cysteine residues in the active sites of these proteins [53, 60, 61].
Moreover, the elevated level of ROS activates the cell proliferation-related transcription factors such as nuclear factor-κB (NF-κB) and activator protein-1 (AP1) that upregulate the cancer cell proliferation (Fig. 6.2) [53]. Interestingly, mitochondria-generated ROS can induce both cell proliferation and cell quiescence by playing a dual role in cell cycle. The increased level of mitochondria-generated ROS that mostly formed by superoxide (O2•−) induces cell proliferation as well as superoxide dismutase (SOD) antioxidant defense system (Fig. 6.1), which converts the superoxide to the hydrogen peroxide (H2O2), and the increased hydrogen peroxide drives proliferating cells into quiescence [52, 62, 63]. Moreover, it is well known that ROS can induce DNA damage such as double-strand breaks and the DNA damage results in cell cycle arrest thanks to the cell cycle checkpoints (Fig. 6.2) [64]. For example, it has been reported that the increased ROS can result in a p53 independent G2/M arrest in colorectal cancer cells by activation of checkpoint kinase 1 (Chk1) [65]. Additionally, the phosphatase inhibition activity of ROS also induces cell cycle arrest by effecting on the cell division cycle 25 (Cdc25) protein phosphatase family consisted of Cdc25A, Cdc25B, and Cdc25C proteins that have substantial roles in the progression of the various cell cycle stages such as synthesis (S) and mitosis (M) phases [66]. For example, it has been reported that the ROS-decreased Cdc25C level leads to G2/M cell cycle arrest and the elevated ROS dramatically decrease Cdc25A level and its phosphatase activity [64, 67,68,69]. On the other hand, ROS accumulation can also predictably take an important role in cancer cell survival as well as cell proliferation and cell cycle arrest because of the common signaling factors such as PTEN, PI3K, PKD, Akt, ERK 1/2, and NF-κB (Fig. 6.2) [26, 31, 52]. For example, increased generation of hydrogen peroxide leads to the oxidation of cysteine thiol groups of PTEN, PTP1B, and PP2 (protein phosphatase 2) and inactivation of these phosphatases promote cell survival by negatively regulation of PI3K/Akt signaling [31, 70, 71]. It has been reported that this kind of phosphatases’ inactivation can be observed in many types of cancer such as breast, prostate, ovarian and endometrial cancers, glioblastomas, and melanomas [72, 73]. Ras activation along with growth factor signaling can be also induced by hydrogen peroxide, and this activation leads to blocking the PTEN signaling cascades and induction of PI3K/Akt/mTOR and MAPK/ERK 1/2 cell survival pathways [31, 58]. Moreover, these cell survival pathways can be regulated by ROS-induced inactivation of their downstream pro-apoptotic targets such as Bad, Bax, Bim, Foxo [52, 74,75,76]. Apart from the Ras oncogene, the cell survival can be also regulated by the other oncogenes such as c-Myc oncogene that induce hMre11 signals and improve the cell survival in many cancers such as cervical carcinoma, colon cancer, leukemia, lymphoma, and testicular cancer (Fig. 6.2) [77, 78].
6.4 ROS and Endogenous Signaling Molecules
It is widely known that there is a tight relationship between the ROS generation and the endogenous signaling molecules such as the growth factors and cytokines, which regulate the molecular mechanisms of many cellular phenomena such as proliferation, growth, invasion, healing, differentiation, metastasis, etc., by involving the intracellular and intercellular signaling pathways [53, 79]. Although the ROS production can be induced by the intracellular growth factors and cytokines such as epidermal growth factor (EGF), endothelial cell growth factor (ECGF), transforming growth factor beta 1 (TGF-β1), and hepatocyte growth factor (HGF), the elevated ROS in turn can stimulate the multiple growth factors and cytokines that play crucial roles in carcinogenesis by binding to the cell membrane receptors such as receptor serine/threonine kinases, G protein-coupled receptors, receptor tyrosine kinases, and cytokine receptors [32, 73, 79,80,81]. This phenomenon between the endogenous signaling molecules and ROS display the existence of a positive feedback loop [32]. For example, it has been reported that ROS production in several culture systems may be elevated by TGF-β1, which plays substantial roles in growth regulation and tumor cell progression as a multipotent cytokine [80,81,82]. Similarly, the tight relationship has been shown between ROS production and HGF, which is known as a prognostic marker for hepatocellular carcinoma, ROS can mediate the HGF receptor and c-met signaling [83,84,85]. Moreover, the superoxide level in a cell can be elevated by the stimulation of angiotensin, epidermal growth factor (EGF), lysophosphatidic acid, platelet-derived growth factor (PDGF), and tumor necrosis factor-α (TNF-α) though the oncogenic mutation of RhoGTPase K-ras has been reported to be related with the elevation of superoxide level and the incidences of several cancers [30, 53, 86,87,88,89,90,91]. As well as the oncogenic mutation of RhoGTPase K-ras, the major ones of growth factors and cytokines including HGF, PDGF, vascular endothelial growth factor (VEGF), and TNF-α increase the production of ROS through NADPH oxidases or mitochondrial electron transport chain system depending on the cellular environment [32, 92, 93]. Although the structures of NADPH oxidases are similar to each other, their regulatory subunits and activation mechanisms are different from each other. For example, p22phox is a necessity for the activation of NOX4 though the other NADPH oxidases do not need it [94, 95]. Moreover, NOX4 can be activated by the influences of various growth factors and receptors such as TGF, bone morphogeneticprotein-2 (BMP-2), insulin like growth factor-I (IGF-I) and toll like receptor 4 (TLR4), and the activated NOX4 plays role in the ROS generation [96,97,98]. As the effects of NOX-generated ROS production, the relationship between endogenous signaling molecules and ROS generation generally affects the fate of cancer hallmark such as cancer cell proliferation and cell survival, angiogenesis, invasion, metastasis, and increased genomic instability by the altering and blocking of related signaling cascades [52, 99].
6.5 ROS and Emerging Hallmarks of Cancer
As widely known, Hanahan and Weinberg published an influential paper in the year 2000 that describes the hallmark of cancer, including six major traits, and they updated the described cancer hallmarks in 2011 by adding two emerging and two enabling traits of cancer [6, 7]. The emerging hallmarks of cancer have been described as deregulating the cellular energetics and evading the immune response [6]. It is not surprising that there is a strict relationship between the emerging hallmarks of cancer and the intracellular accumulation of ROS, and the elevated metabolic activity, oncogenic signals, and genetic changes in cancer cells induce an increased ROS production along with the adaptation to the antioxidant system and the compensation for the oxidative damages [31, 100]. Thus, alterations occur in the redox homeostasis and cellular signaling pathways, and cancer cell metabolism is reprogrammed [101]. Cancer cells acquire adaptations to survive under hypoxic conditions and utilize alternative metabolic pathways because of their higher metabolism than the normal cells [23, 101]. This alteration in the energy metabolism of cancer cells was firstly discovered in 1924 by Otto Warburg, who reported that cancer cells convert glucose to lactate using glycolytic pathway instead of pyruvate regardless of the presence of oxygen [102]. This phenomenon has been known as Warburg effect, which contributes an aggressive cancer phonotype because a prolonged survive under hypoxic condition leads to a series of alterations in genetic stability, metabolic pathways, organelles, etc., though the hypoxic condition leads to cell death in normal cells [52, 103]. It can be clearly seen that there is a reciprocal crosstalk between the redox balance and metabolic pathways such as glycolysis, the pentose phosphate pathway, one-carbon metabolism, fatty acid oxidation, and glutaminolysis [31, 104]. For example, redox homeostasis can be regulated by glycolysis through shuttling of the pentose phosphate pathway-generated intermediate nicotinamide adenine dinucleotide phosphate (NADPH) and glutaminolysis-generated intermediate glutathione (GSH) [52]. Although it is expected that the glucose-deprivation causes cell death by the accumulation of hydrogen peroxide, the Warburg effect provides the cancer cells to acquire adaptation of the glucose-deprivation by exaggeratedly using glycolysis pathway to prevent hydrogen peroxide-induced cell death [105, 106]. Targeting glycolysis and lactate dehydrogenase enzyme is therefore considered a successful strategy to prevent the cancer cell progression by inducing oxidative stress and decreasing the production of the intracellular ATP [31, 107,108,109]. For example, let-7a that is an early-discovered microRNA was used as a therapeutic enhancer because let-7a elevates the ROS generation and downregulates some enzymes involved in glycolysis such as glucose 6-phosphate dehydrogenase (G6PD) and inosine monophosphate dehydrogenase (IMPDH) [110]. Pyruvate kinase muscle isoenzyme 2 (PKM2), the isoenzyme of the rate-limiting glycolysis enzyme named pyruvate kinase, plays a crucial role in reprogramming cancer metabolism, but the ectopic expression of microRNA-1 and microRNA-133b inhibits PKM2 through silencing polypyrimidine tract-binding protein 1 (PTBP1), which can convert the active PKM2 to the inactive PKM1 [111, 112]. On the other hand, it is well documented that cancer cells produce an elevated level of ribose 5-phosphate by employing pentose phosphate pathway that is considered a key feature for many cancers, and regulate the ROS homeostasis through NOXs and replenishing the decreased GSH and TRX [31, 113]. As previously mentioned, mitochondria is considered as one of the major sources of ROS because they are inevitably generated in oxidative phosphorylation as the byproducts [114]. The elevated ROS accumulation because of hypoxia causes oxidative stress and consequently results in damages of organelles and the other cellular components such as lipids, proteins, metabolites, etc. [115, 116]. Moreover, the structure, morphology, and dynamics of mitochondria are considered linking with the accumulated amounts of ROS, i.e., there is a mutual interaction between mitochondria and ROS [117]. The overproduction of ROS induces mitochondrial damages and these damages result in the elevated ROS production, so this phenomenon is called as ROS-induced ROS release [115, 118, 119]. For example, mitochondria induce elevated production of ROS under hypoxic condition and the hypoxia-induced ROS production can cause the mitochondrial fragmentation though the mitochondrial fusion is considered as a cellular adaptation process for the alterations in the surrounding environment, and which can prevent the elevated production of ROS [120, 121]. One of the most prominent transcription factors for the cellular adaptation to the hypoxic conditions is hypoxia inducible factor-1 (HIF-1) that is a heterodimer consisted of two subunits HIF-1α and HIF-1β, and it is well known that ROS play a key role in the accumulation of HIF-1 [52, 122, 123]. The increased levels of antioxidants reduce the accumulation of HIF-1 though the increased levels of hydrogen peroxide and superoxide elevate the accumulation of HIF-1 [63, 124, 125]. Apart from the endogenous ROS, the exogenous ROS can alter mitochondrial dynamics by inhibiting mitofusin-1 (Mfn1) and mitofusin-2 (Mfn2) and inducing the depolarization of mitochondrial membrane potential, which trigger the mitochondrial fission along with the overproduction of ROS [115, 126]. Moreover, the oxidative stress-induced mitochondrial fission and fusion influence on the mitochondrial metabolism and function because of the dramatic changes in mitochondrial DNA (mtDNA), ribosomes, proteins, metabolites, etc., that lead to many diseases including cancers, cardiometabolic diseases, neuropathies, and neurodegenerative diseases [127,128,129].
As previously mentioned, the second emerging hallmark has been described as evading the immune response, and ROS have been identified as immunosuppressive factors in the cancer microenvironment to facilitate the other cancer hallmarks such as growth, invasion, and metastasis [6, 31, 130]. Apart from the pathological conditions such as cancer, ROS play key roles in the regulation of immune responses and serve as central mediators of immune cells [131]. For example, dendritic cells (DC) that have a substantial role in antigen specific immune response as the major antigen-presenting cells (APC) are activated by hydrogen peroxide, which can be produced in a large quantity by phagocytic cells [132]. On the other hand, the pathological conditions such as cancer or chronic inflammatory diseases can alleviate the function of natural killer cells (NK cells) and the effector T cells depending on the macrophages- and granulocytes-generated ROS levels [133,134,135]. Although NK cells increase the ROS production in the early stage of the encounter with cancer cells to mediate cytolysis, it has been reported that monocyte-generated ROS production in cancer patients inhibits the interferon gamma (IFN-γ) production, proliferation, activation, and cytotoxicity of NK cells along with the induction of NK cells’ apoptosis [136, 137]. The differences of NK cells responses to the ROS generation are regulated by the CD56bright and CD56dim that are the NK cells antigen subsets [138]. Monocyte-derived ROS direct CD56dim NK cells to apoptosis though the CD56bright NK cells display a significant resistance to the ROS-induced functional inhibition and apoptosis because of their stronger antioxidant capacity than CD56dim NK cells [139,140,141]. Thus, the resistance of CD56bright NK cells provides the cancer cells to evade immune system because the ROS-sensitive CD56dim NK cells have higher cytotoxic activity than the ROS-resistant CD56bright NK cells [136]. Similarly, the oxidative stress in the cancer microenvironment provides cancer cells to evade immune system by regulating the accumulation of different subsets of T cells because the conventional T cells are more sensitive to the hydrogen peroxide-induced cell death than the regulatory T cells (Tregs) that have an ability to inhibit the functions of other infiltrating immune cells [142,143,144]. Moreover, either the functions of T cells can be suppressed or the apoptosis of T cells can be induced via Jak3/STAT5 signaling pathway, which is regulated through the inducible nitric oxide synthase (iNOS)-generated nitric oxide (NO) production by myeloid-derived suppressor cells (MDSCs) [136, 145,146,147].
6.6 ROS and Enabling Hallmarks of Cancer
In the paper published by Hanahan and Weinberg [6], two enabling hallmarks of cancer have been added to the previously described six hallmarks along with the two emerging hallmarks, and these two enabling hallmarks have been described as the tumor-promoting inflammation, and the genome instability and mutation [6, 7]. Actually, the relationship between inflammation and carcinogenesis has been known far before the paper of Hanahan and Weinberg [6]. In 1863, Rudolf Virchow reported that the “lymphoreticular infiltrate” reflected the origin of cancer at the locations of chronic inflammation by observing white blood cells or leukocytes in neoplastic tissues [23, 148,149,150]. The currently known data obtained from the numerous studies performed after the Virchow’s hypothesis clearly indicate that there is a tight and intricate relationship between the cancer progression and the promotion of inflammation coordinated by the level of inflammatory cytokines (TNF, interleukin-1 (IL-1), and IL-6), chemokines (CXC chemokine receptor 4 (CXCR4) and IL-8), and inflammation-related factors, especially located in the tumor microenvironment [151,152,153]. Moreover, it is well known that ROS predictably take important roles in the regulation of the sophisticated interaction between the course of cancer and the promotion of inflammation by effecting the presences, levels, and types of the inflammatory cytokines, chemokines, and inflammation-modulating factors such as activator protein 1 (AP-1), HIF-1α, specificity protein 1 (Sp1), β-catenin, wingless-type MMTV integration site family (Wnt), HIF-1α, NF-κB, peroxisome proliferator-activated receptors-gamma (PPAR-γ), p53, signal transducer and activator of transcription 1 (STAT1)/STAT3, and nuclear factor erythroid 2-related factor 2 (Nrf2) [154,155,156,157]. A series of signal transduction cascades can be activated by the accumulation of inflammatory cells in the tumor microenvironment, which provokes the further recruiting of inflammatory cells by producing cytokines and chemokines, and a massive ROS production is therefore occurred by the activation of the oxidation-related enzymes such as iNOS, NOX, XO, and myeloperoxidase (MPO), and the upregulation of the expression of COX2 and LOXs [156, 158]. The massively produced ROS leads to significant oxidative damages in genetic materials, macromolecules, and organelles, which support the progression of carcinogenesis and overpowered production of supplemental ROS, and this excessively produced ROS activate again the inflammatory cytokines, chemokines, and inflammation-modulating factors. This phenomenon may be named as “inflammatory response-mediated ROS-induced ROS release” by considering its similarity with “ROS-induced ROS release” because ROS-induced inflammatory responses release excessive ROS that induce again inflammatory responses [154, 155, 159, 160].
The other enabling hallmark of cancer has been described as the genome instability and mutation, the main cause of the genetic diversity in many cancers and the cancer cell heterogeneity within the tumor tissue, and the overproduced ROS are known as the prominent factors leading the oxidative DNA damages, including base damages and modifications, deletions and insertions in DNA sequence, DNA miscoding lesions, DNA single-strand and double-strand breaks, gene amplification, and the activation of oncogenes, which contribute in cancer initiation and progression [26, 31, 161,162,163,164]. It can be possible to say that there is a cycle between the overproduction of ROS and the oxidative DNA damages. As previously mentioned, the elevated ROS level can activate the oncogenes such as Bcr-Abl, c-Myc, and Ras, which can play substantial roles in the regulation of tumor suppressor genes, cancer cell proliferation, mitochondrial dysfunction, angiogenesis, and metastasis, and the oncogene activation is known as the main cause of the overproduction of ROS that leads to the formation of replication stress [165,166,167]. For example, it has been reported that the replication fork velocity can be reduced because the polymerase activity is affected by the occurrences of ROS-oxidized deoxyribonucleotide triphosphates (dNTPs) [168, 169]. The progression of replication fork can be regulated by ROS by dissociation of peroxiredoxin2 oligomers (PRDX2), and the fork accelerator named TIMELESS can be inhibited by a replisome associated ROS sensor formed PRDX2 [170]. Thus, the replication fork speed can be reduced through the dissociation of PRDX2 and TIMELESS, which is regulated by the overproduced ROS [170]. Moreover, the replication forks can be prevented physically due to the occurrences of oxidized bases, and this phenomenon can cause the breakdown of replication forks at fragile sites across the genetic material along with the under-replicated or over-replicated DNA [64, 171]. On the other hand, the highly accumulated ROS may directly effect on DNA through reacting with purines, pyrimidines, and chromatin proteins, and causing the DNA single-strand and double-strand breaks [172, 173]. A point mutation, for example, can be formed because of the production of 8-hydroxy-2′-deoxyadenosine (8-OH-dAdo) or 8-hydroxy-2′-deoxyguanosine (8-OHdG) that are the widely known oxidative DNA damage markers, which can be occurred through the reaction of hydroxyl radicals with adenine or guanine nucleotides, respectively [173,174,175,176]. Additionally, it should be noted that quinine is considered as the most sensitive nucleobase to oxidation than other nucleotides, and so 8-OHdG emerges as the most common oxidized nucleobase [177]. Apart from the 8-OHdG, there are some other oxidative DNA damage markers such as 8-oxo-7,8-dihydroguanine (8-oxoGua), 8-oxo-7,8-dihydroadenine (8-oxoAde), 8-oxo-7,8-dihydro-2-deoxyguanosine (8-oxodG), 5,6-dihydroxy-5,6-dihydrothymine, 2,6-diamino-4-hydroxy-5-formamido-pyrimidine, and 4,6-diamino-5-formamido-pyrimidine [29, 172, 178]. ROS-induced production of oxidized nucleobases generally leads to further mutations and DNA damages along with the accumulation on some specific location such as telomere sites, which are less efficiently repaired than the other genomic sites [179]. 8-oxoGua can be, for example, accumulated on the telomere sites, and behaves as a blockage for telomerase activity through reducing the binding potential of telomeric proteins, disrupting telomere length, and precluding of chromosomal-end capping, and this phenomenon can result in cell death, aging, carcinogenesis, chromosome instability, and genotoxic formations such as nuclear buds (NBUDs), nucleoplasmic bridges (NPBs), and micronuclei (MN) [179,180,181].
6.7 ROS and Angiogenesis
Angiogenesis can be considered as one of the most important cancer hallmarks because cancer cells rapidly proliferate to form and expand the tumor tissue, but the tumor tissue expansion increases the distance between cells and capillary vessels [12]. However, the appropriate distance between the cells and capillary vessels is restricted to 100–200 μm to maintain the balanced composition of oxygen, carbon dioxide, nutrient substances, and metabolic wastes [182, 183]. Additionally, the tumor tissue enlargement provides a hypoxic, hypoglycemic, hypoferric, and acidified microenvironment along with the occurrence of an intolerable mechanical stress on the cancer cells, and so the cancer cells are driven to migrate, invade, and metastasize [12]. The cancer cells induce therefore angiogenesis to form new capillary vessels originated from the existing vessels, run away from the stressed microenvironment by participating in the circulatory system, and sustain the course of carcinogenesis [184]. Angiogenesis is regulated via an angiogenic switch, which can be opened and closed by variation of the balance between angiogenesis promoting (angiogenic) and suppression (anti-angiogenic) factors [185]. The formation of ROS and the occurrence of oxidative stress within the cells and microenvironment predictably regulate the direction of the angiogenic switch along with the activation of angiogenic or anti-angiogenic factors through the regulation of transcriptional factors, releasing of some growth factors, and alteration of the cellular signaling cascades (Fig. 6.3) [186, 187]. For example, the cancer cells in a hypoxic microenvironment can induce the releasing of proangiogenic growth factors such as vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), fibroblast growth factor (FGF), hepatocyte growth factor (HGF), and platelet-derived growth factor (PDGFB) and the increased production of the other angiogenic proteins such as angiopoietin-1, leptin, endoglin, prominin-1, transforming growth factor beta (TGF-beta), integrins, and matrix metalloproteinase (MMP) enzymes [12, 188,189,190]. After the opening of angiogenic switch and the formation of new capillaries surrounding the tumor tissue, the tumor cells and their microenvironments are re-oxygenated. Contrary to the expectations, the tumor-induced angiogenesis and re-oxygenation of tumor cells lead to larger problems instead of solving the problem of cancer cells [187].
Although the hypoxic microenvironment induces an overproduction of ROS by disrupting the mitochondrial metabolism and the electron transport system, an oxygen abundance occurs because of the angiogenesis-motivated re-oxygenation phase, which results in 100 times higher ROS production than hypoxic state [191,192,193]. This phenomenon is named as “cyclic hypoxia” because hypoxia-induced angiogenesis leads to an excessive production of ROS and these ROS induce again angiogenesis through the direct activation of HIF-1α, VEGF, and VEGFR2, and the oxidation of lipids that stimulate NF-κB pathway-mediated angiogenesis [187]. ROS-induced equilibrium corruptions in the angiogenic switch can lead to many structural and functional abnormalities within the newly formed capillaries surrounding tumor tissue, and these abnormalities result in hyperpermeability, hypoglycemia, hypoxia, abnormal blood flow, and increased pressure, which also increase the ROS production [187, 194]. Additionally, ROS such as superoxide anion and hydrogen peroxide molecules have a special importance for the vascular cells because they can regulate the fate of these cells depending on the concentrations [195]. For example, the low concentrations of hydrogen peroxide such as 0.1–10 μM induce the capillary tube-like formation of endothelial cells though its high concentrations (>125 μM) induce lethal damages [187, 195]. Consequently, ROS have a substantial role in the regulation of angiogenesis though the tumor-induced angiogenesis is one of the major causes of the excessive ROS production, and it is widely considered that the main source of ROS caused by tumor-induced angiogenesis is mitochondria and electron transport system because of the hypoxic condition and the cyclic hypoxia-induced oxygen abundance [12, 187].
6.8 ROS in Cancer Cell Invasion and Metastasis
Cancer cell invasion and metastasis are commonly considered as the carcinogenesis processes that can be possible depending on the formation of angiogenesis though the metastasis can be observed in many solid tumors regardless of the early or late stages of the carcinogenesis [6, 187, 196]. Besides the similarities of the underlying reasons of the tumor-induced angiogenesis and metastasis, the close interaction between angiogenesis and metastasis has been known since the first observations of Judah Folkman (1971) and Pietro Gullino (1978) [189, 197,198,199]. As previously mentioned, the uncontrolled expansion of tumor tissue results in an unsuited microenvironment qualified with the hypoxic, hypoglycemic, hypoferric, and acidified features along with the mechanical stress, and so the cells forming tumor tissue would like to escape from this microenvironment by inducing angiogenesis and operating the complex processes of metastasis [12, 187]. Metastasis can be occurred employing a series of cellular phenomena, including the degradation of extracellular matrix (ECM), losing the cellular polarity and detaching from the ECM, cancer cell invasion along with the amoeboid or mesenchymal migration, accessing to the capillary vessels, intravasation, sustaining the anchorage-independent growth and survival by evading anoikis (anchorage-dependent apoptosis), bypassing the immune surveillance, extravasation, adhesion, proliferation, and colonization within the secondary tumor site [200,201,202,203]. Numerous papers have revealed that ROS have substantial regulative roles in the complex processes of metastasis as well as in the angiogenesis, and many clinical and experimental data have suggested that the level of ROS is changed during the metastasis [204]. For example, several studies reported that the overproduced ROS induce the epithelial to mesenchymal transition (EMT), a biological phenomenon that acts on the metastasis-related cellular functions such as the cell–cell and cell–matrix interactions along with the cellular motility and migration, and EMT can be regulated by various cytokines such as TGF-β1 and EGF, transcription factors including Twist, Snai1, Slug and ZEB1/2 (zinc-finger E-box-binding homeobox), and signaling pathways such as the inhibitory kappa B kinase (IKK)/NF-kB, MAPK, Notch, PI3K/Akt, TGF-b/Smad, and Wnt/b-catenin signaling pathways [205,206,207,208]. Although the cell invasion is facilitated by the elevated expression of urokinase plasminogen activator (uPA) and matrix metalloproteinases (MMPs), the cell–cell and cell–matrix adhesions are emaciated by decreasing the epithelial markers and tight junction proteins such as occludin, claudin, and e-cadherin, and increasing the mesenchymal markers such as fibronectin, vimentin, and n-cadherin [205, 208]. The overproduced ROS are commonly considered as the prominent regulator for the processes of EMT and metastasis, and ROS-induced cancer cell metastasis by affecting the molecular pathways, transcription factor, cytokines, and growth factor have been extensively reviewed by many scientists [204, 205, 209,210,211,212]. For example, one of the prominent inducer of EMT named TGF-β1 can be regulated by ROS-dependent pathway; the Rac1-NOXs-ROS-dependent activation of NF-κB pathway mediates the TGF-β1-regulated uPA and MMP9 activities on cell migration and invasion [210, 213]. Additionally, the Rac-dependent ROS production has been suggested to be related to the activities of MMPs (e.g., MMP2, MMP3, and MMP9) and the transduction of mechanical perturbations into a pro-invasive gene expression [209, 214,215,216]. Moreover, the loss of TGF-β1-activated kinase 1 (TAK1) can lead to the integrin-Ras-induced ROS production that activates the EMT signaling cascade [217]. Pelicano and coworkers reported that mitochondria-derived ROS production leads to the AP-1 signaling pathway-mediated upregulation of C-X-C motif chemokine 14 (CXCL14) expression and the boost in cell motility by increasing the amount of cytosolic Ca2+ levels [218]. On the other hand, the evading anoikis (anchorage-dependent apoptosis), which is the most important part of metastasis is succeeded by ROS-dependent mechanisms. Anoikis resistance of cancer cells can be conferred through NOX4-induced ROS-activated the epidermal growth factor receptors (EGFR) and angiopoietin-like 4 (ANGPTL4)-integrin complex-induced ROS-activated PI3K/Akt and ERK pathway [219,220,221].
6.9 ROS and Cancer Cell Death Pathways
Although the overproduced ROS are well known as a key factor in the initiation and development of cancer through the disrupting effects on the genetic materials, cellular macromolecules, organelles, signaling cascades, components, and homeostatic balances along with the significant contribution in the cancer cell survival, the disproportionately increased ROS emerge as a substantial approach for the cancer treatment strategies because of the cell death provoking activity [23, 52]. Apart from the non-inflammatory, caspase-independent, and ROS-sensitive special cell death pathway named “oxeiptosis,” there are well-described ROS-induced cell death pathways such as caspase-dependent apoptosis, caspase-independent ferroptosis, and necroptosis, inflammasome-driven pyroptosis, and autophagic cell death (Fig. 6.4) [222,223,224,225,226,227].
Kelch-like ECH-associated protein 1 (Keap1) is known as a main sensor to monitor oxidative and electrophilic stress, and regulates the expression of cytoprotective molecules by ubiquitination and degradation of Nrf2 under the physiological conditions, though the overproduced ROS-oxidized Keap1 leads to insufficient expression of cytoprotective molecules and highly expressed antioxidant factors, viz., NAD(P)H quinone dehydrogenase 1 (NQO1), homeobox protein 1 (Hox1), and Thioredoxin (Txn) because of the highly accumulated Nrf2 [227, 228]. Besides the accumulation and translocation of Nrf2, the oxidized Keap1 could not interact with the phosphoglycerate mutase 5 (PGAM5) that is known as a common factor for many caspase-independent cell death pathways, and so the released PGAM5 dephosphorylates the apoptosis inducing factor mitochondria associated 1 (AIFM1) at Ser116 [227, 229]. Thus, AIFM1-deficient cells undergo to the oxeiptosis by ROS-induced cell death pathway that includes KEAP1, PGAM5 and AIFM1 [227].
On the other hand, the ROS-induced caspase-dependent cell death pathways are well known and the cellular pathways have been broadly described in many papers [222,223,224,225,226,227]. For example, cytochrome-c is released from mitochondria because of the ROS-induced mitochondrial abnormalities and dysfunctions, and so apoptosome complex can be formed by the incorporation of the released cytochrome-c, Apaf-1 (apoptotic peptidase activating factor 1), and procaspase-9 to activate effector caspases, e.g., caspase-3, which leads to the cleavage of cellular proteins and apoptosis [23, 230]. Additionally, the intracellular accumulation of ROS regulates the expression of the pro-apoptotic (Bad, Bak, Bax, Bid, and Bim) and anti-apoptotic (Bcl-2, Bcl-w, and Bcl-xL) members of the Bcl-2 family via their phosphorylation and ubiquitination, and the Bcl-2 family proteins play key roles in the regulation of the mitochondrial membrane permeabilization and apoptotic signaling [52, 231, 232]. The other well-known ROS-induced cell death is autophagy that can be regulated by several kinase cascades such as the most familiar mammalian target of rapamycin complex1 (mTORC1), which can be regulated by PTEN/PI3K/AKT signaling pathway [233]. The overproduced ROS-induced autophagy results in degradation of the mitochondria that excessively produce ROS, and so this kind of autophagy is called as mitophagy that leads to the reduced ROS levels as a result of the NIX/BNIP3L and PARKIN/PTEN induced putative kinase 1 (PINK1) molecular pathways [52, 234,235,236]. Moreover, the ROS-induced autophagy can be occurred through Nrf2/Keap1 pathway by preventing degradation of Nrf2 as well as the ROS-induced oxeiptosis [237]. The attentions of many scientists seem to be focused on the ROS-dependent cell death pathways because there is certainly a complex relationship between the intracellular ROS and the cell death pathways, and the ROS-mediated anticancer drugs and treatment strategies are commonly considered as the beneficial treatment modalities.
6.10 ROS and Anticancer Treatment Strategies
Although unexpected and long-term changes in the intracellular ROS level are considered as the main factors for the occurrence of extremely complex cellular processes that induce carcinogenesis, numerous studies have shown that cancer cells are more susceptible to the changes in intracellular ROS accumulations and more dependent on the antioxidant systems than their healthy counterparts [39]. The exogenous ROS generation is therefore considered as a promising option for the anticancer treatment strategies because the vulnerability of cancer cells towards oxidative stress provides a therapeutic selectivity in anticancer therapies [238]. ROS-dependent treatment strategies are generally based on three different approaches such as directing cancer cells to the cell death pathways by promoting an excessive ROS generation, activating ROS-dependent cancer cell death by blocking the antioxidant systems, and inhibiting carcinogenesis by reducing ROS generation via activating antioxidant systems and employing antioxidant molecules. There are many chemotherapeutic agents that increase ROS generation to selectively induce cancer cell death because of the ROS-induced irreparable damages [54]. Examples of these chemotherapeutics include, but not limited to the arsenic trioxide, anthracyclines (e.g., daunorubicin, doxorubicin, epirubicin, and idarubicin), bleomycin, β-lapachone, cisplatin, elesclomol, and sulindac [54, 238,239,240]. These drugs can induce ROS generation by using different cellular mechanisms. For example, doxorubicin that is a topoisomerase inhibitor, DNA intercalation agent, and also one of the most known chemotherapeutics employed in the treatment of many cancers, including bile duct, breast, endometrium, esophagus, gastric, pancreatic and liver cancers, osteosarcoma, Kaposi’s sarcoma and soft tissue sarcomas, Hodgins and non-Hodgins lymphomas, induces intracellular ROS generation by reacting with flavoprotein reductases, intracellular chelation of iron, which respectively result in apoptosis and ferroptosis [52, 241, 242]. Apart from the application of chemotherapy-induced ROS generation, there are different cancer treatment strategies that induce intracellular ROS generation, such as photodynamic cancer therapy (PDT) and sonodynamic cancer therapy (SDT) [243, 244]. PDT is a non-invasive and clinically approved treatment method that induces excessive ROS generation in the presence of molecular oxygen thanks to the synergic interactions of a non-thermal light source and a nontoxic photosensitizer molecule to induce apoptosis by damaging the cellular components of target cells [244, 245]. Similar to the PDT, the ultrasound-mediated cancer therapy (SDT) induces apoptosis in the target cells through the production of ultrasonic cavitation, sonochemical bubble collapse, and finally free radicals and ROS generation [243, 246]. The second ROS-dependent cancer treatment approach emerges as the suppressing cellular antioxidant systems (e.g., glutathione and thioredoxin) resulting in the overproduced ROS-dependent activation of cell death pathways, and examples of these chemotherapeutics include 2-methoxyestradiol, buthionine sulfoximine, phenylethyl isothiocyanate, imexon, mangafodipir, and tetrathiomolybdate [39]. For example, buthionine sulfoximine, phenylethyl isothiocyanate, and imexon lead to the increased accumulation of intracellular ROS by reducing the intracellular GSH level [247,248,249]. Moreover, it has been thought that the redox adaptation mechanisms can be evaded by combining the first and second ROS-depended anticancer treatment approaches, viz., the promoting an excessive ROS generation and the suppressing cellular antioxidant systems [39]. The last one of the ROS-dependent treatment approaches is known as the targeting ROS production by using antioxidant molecules that can be employed as a cancer preventive therapy by using daily dietary compounds such as green tea-derived epigallocatechin-3-gallate (EGCG), carotenes vitamin C and vitamin D [250, 251]. However, it should be noted that there are also some reports indicating that some antioxidants such as carotene, vitamin A, and vitamin E can be effective on the elevated risk of cancer [252,253,254]. The substantial contributions of ROS into the drug resistance development processes and further progression of carcinogenesis should be also noted, because the overproduced ROS are well known as the prominent factors for the oncogenic signaling, genetic instability, and DNA damages along with the metabolic adaptations, enhanced proliferation, and survival [255]. Consequently, it should be thoroughly considered the advantages, disadvantages, and the exact activity mechanisms of the ROS-dependent anticancer therapies because it is clear that targeting redox homeostasis of cells may lead to the unexpected and unwanted consequences as well as the expected and wanted outcomes.
6.11 Concluding Remarks and Future Prospects
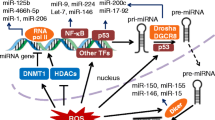
As can be clearly seen in the previous parts of the chapter, ROS play substantial roles in the regulation of physiological homeostasis such as the controlling of cellular signaling cascades via low-level productions and the provoking of cell death pathways via overproductions. Although numerous studies have shown that more than 150 human disorders are related to the disruption of redox homeostasis, the bulk of ROS-mediated intracellular signaling pathways and the consequences remain unknown. It is well known that cancer cells induce the overproduction of ROS and the elevated ROS production contributes in the progression of carcinogenesis through provoking the DNA damage and genetic instability, cancer cell proliferation and survival, metabolic adaptations, and drug resistance. Interestingly, ROS-induced cell deaths in a cancer tissue can result in a more aggressive and chemotherapy resistant cancer tissue in some cases because the elevated ROS can kill the sensitive cancer cells though the aggressive ones can cope with the same amount of ROS. Conversely, the combination therapy that is employed by using redox-active molecules and conventional treatment strategies is considered as a rational option to overcome chemotherapy resistance. Many anticancer drugs, for example, kill the cancer cells by activation of ROS-dependent cell death pathways though the cancer cells develop resistance towards them by activating the antioxidant systems. The antioxidant system inhibitors can be therefore employed to evade the cancer cell resistance. It should be also noted that the anticancer drugs that kill the cancer cells by ROS-dependent cell death pathways are preferred more to perform a selective treatment because the cancer cells are regarded as more sensitive that health counterparts due to the lack of redox homeostasis. On the other hand, the antioxidant dietary substances are generally considered as beneficial to preclude carcinogenesis and many scientists have recommended people to include these substances in their daily diets to keep them away the cancer risks. However, some papers have displayed the link between the increased cancer risks and some dietary antioxidants such as carotene, vitamin A, and vitamin E. Thus, the activity mechanisms of the dietary antioxidants need to be extensively investigated to understand well their benefits and harms, and give recommendations to the people who would like to keep themselves healthy. Although the consequences of the enhanced ROS production in the cells seem to be not predictable because of the dependence on many different factors, the ROS-mediated treatment strategies such as photodynamic therapy and sonodynamic therapy seem to be promising because of their non-invasive features. The relationship between microRNAs and ROS was not extensively discussed to keep concise in this chapter, but this relationship seems to be substantial for the regulation of many intracellular signals and epigenetic changes. Moreover, the extensive investigations of ROS-mediated effects of drugs on epigenetic mechanisms seem to be quite beneficial because ROS are known as the effective factors on epigenetic regulations and aberrations that play crucial roles in cancer heterogeneity and carcinogenesis. Consequently, ROS are considered as a double-edged sword and the effects of the edges should be therefore extensively investigated by developing interdisciplinary projects and collaborations to understand well and employ efficiently this sword as a weapon, target, or mediator in the cancer treatment modalities.
References
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Plon SE, Lupo PJ (2019) Genetic predisposition to childhood cancer in the genomic era. Annu Rev Genomics Hum Genet 20:241–263
Walsh T et al (2017) Genetic predisposition to breast cancer due to mutations other than BRCA1 and BRCA2 founder alleles among Ashkenazi Jewish women. JAMA Oncol 3(12):1647–1653
Chaffer CL, Weinberg RA (2015) How does multistep tumorigenesis really proceed? Cancer Discov 5(1):22–24
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100(1):57–70
Voron T et al (2014) Control of the immune response by pro-angiogenic factors. Front Oncol 4:70
Meacham CE, Morrison SJ (2013) Tumour heterogeneity and cancer cell plasticity. Nature 501(7467):328–337
Hansen KD et al (2011) Increased methylation variation in epigenetic domains across cancer types. Nat Genet 43(8):768
Dagogo-Jack I, Shaw AT (2018) Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol 15(2):81
Varol M (2020) Natural remedies and functional foods as angiogenesis modulators. In: Functional foods in cancer prevention and therapy. Elsevier, pp 1–31
Tsuda K (2012) Associations of oxidative stress and inflammation and their role in the regulation of membrane fluidity of red blood cells in hypertensive and normotensive men: an electron spin resonance investigation. Adv Biosci Biotechnol 3(7A):1020–1027
Cook JA et al (2004) Oxidative stress, redox, and the tumor microenvironment. In: Seminars in radiation oncology. Elsevier
Costa A, Scholer-Dahirel A, Mechta-Grigoriou F (2014) The role of reactive oxygen species and metabolism on cancer cells and their microenvironment. In: Seminars in cancer biology. Elsevier
Sena LA, Chandel NS (2012) Physiological roles of mitochondrial reactive oxygen species. Mol Cell 48(2):158–167
Yang S et al (2000) Mitochondrial adaptations to obesity-related oxidant stress. Arch Biochem Biophys 378(2):259–268
Matsuda M, Shimomura I (2013) Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes Res Clin Pract 7(5):e330–e341
Kruk J (2014) Overweight, obesity, oxidative stress and the risk of breast cancer. Asian Pac J Cancer Prev 15(22):9579–9586
Waypa GB, Smith KA, Schumacker PT (2016) O2 sensing, mitochondria and ROS signaling: the fog is lifting. Mol Asp Med 47:76–89
Michiels C, Tellier C, Feron O (2016) Cycling hypoxia: a key feature of the tumor microenvironment. Biochim Biophys Acta 1866(1):76–86
Zhang J et al (2016) ROS and ROS-mediated cellular signaling. Oxidative Med Cell Longev 2016:4350965
Aggarwal V et al (2019) Role of reactive oxygen species in cancer progression: molecular mechanisms and recent advancements. Biomol Ther 9(11):735
Yang Y et al (2013) Reactive oxygen species in cancer biology and anticancer therapy. Curr Med Chem 20(30):3677–3692
Panieri E, Santoro M (2016) ROS homeostasis and metabolism: a dangerous liason in cancer cells. Cell Death Dis 7(6):e2253–e2253
de Sá Junior PL et al (2017) The roles of ROS in cancer heterogeneity and therapy. Oxidative Med Cell Longev 2017:2467940
Gerschman R (1954) Oxygen poisoning and x-irradiation: a mechanism in common. In: Glutathione. Elsevier, pp 288–291
Gerschman R et al (1954) Influence of x-irradiation on oxygen poisoning in mice. Proc Soc Exp Biol Med 86(1):27–29
Snezhkina AV et al (2019) ROS generation and antioxidant defense systems in normal and malignant cells. Oxidative Med Cell Longev 2019:6175804
Storz P (2005) Reactive oxygen species in tumor progression. Front Biosci 10(1–3):1881–1896
Kumari S, Badana AK, Malla R (2018) Reactive oxygen species: a key constituent in cancer survival. Biomark Insights 13:1177271918755391
Galadari S et al (2017) Reactive oxygen species and cancer paradox: to promote or to suppress? Free Radic Biol Med 104:144–164
Dickinson BC, Chang CJ (2011) Chemistry and biology of reactive oxygen species in signaling or stress responses. Nat Chem Biol 7(8):504
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82(1):47–95
Krumova K, Cosa G (2016) Overview of reactive oxygen species. In: Singlet oxygen: applications in biosciences and nanosciences. Royal Society of Chemistry
Hecht F et al (2016) The role of oxidative stress on breast cancer development and therapy. Tumor Biol 37(4):4281–4291
Chio IIC, Tuveson DA (2017) ROS in cancer: the burning question. Trends Mol Med 23(5):411–429
Jones DP (2008) Radical-free biology of oxidative stress. Am J Phys Cell Phys 295(4):C849–C868
Zhang W, Huang P (2017) ROS. In: Cancer therapeutic targets. Springer, New York, pp 935–944
Sosa V et al (2013) Oxidative stress and cancer: an overview. Ageing Res Rev 12(1):376–390
Gorrini C, Harris IS, Mak TW (2013) Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discov 12(12):931–947
Dizdaroglu M, Jaruga P (2012) Mechanisms of free radical-induced damage to DNA. Free Radic Res 46(4):382–419
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417(1):1–13
Handy DE, Loscalzo J (2012) Redox regulation of mitochondrial function. Antioxid Redox Signal 16(11):1323–1367
Nohl H et al (2003) Are mitochondria a spontaneous and permanent source of reactive oxygen species? Redox Rep 8(3):135–141
Blanchetot C, Boonstra J (2008) The ROS-NOX connection in cancer and angiogenesis. Crit Rev Eukaryot Gene Expr 18(1):35–45
Bedard K, Krause K-H (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87(1):245–313
Fisher AB (2009) Redox signaling across cell membranes. Antioxid Redox Signal 11(6):1349–1356
Schwarz DS, Blower MD (2016) The endoplasmic reticulum: structure, function and response to cellular signaling. Cell Mol Life Sci 73(1):79–94
Papaioannou A, Chevet E (2017) Driving cancer tumorigenesis and metastasis through UPR signaling. In: Coordinating organismal physiology through the unfolded protein response. Springer, pp 159–192
Clarke HJ et al (2014) Endoplasmic reticulum stress in malignancy. Cancer Cell 25(5):563–573
Moloney JN, Cotter TG (2018) ROS signalling in the biology of cancer. In: Seminars in cell and developmental biology. Elsevier
Raza MH et al (2017) ROS-modulated therapeutic approaches in cancer treatment. J Cancer Res Clin Oncol 143(9):1789–1809
Pelicano H, Carney D, Huang P (2004) ROS stress in cancer cells and therapeutic implications. Drug Resist Updat 7(2):97–110
Glasauer A, Chandel NS (2014) Targeting antioxidants for cancer therapy. Biochem Pharmacol 92(1):90–101
Torti D, Trusolino L (2011) Oncogene addiction as a foundational rationale for targeted anti-cancer therapy: promises and perils. EMBO Mol Med 3(11):623–636
Luo J, Solimini NL, Elledge SJ (2009) Principles of cancer therapy: oncogene and non-oncogene addiction. Cell 136(5):823–837
Ma L et al (2018) Breast cancer-associated mitochondrial DNA haplogroup promotes neoplastic growth via ROS-mediated AKT activation. Int J Cancer 142(9):1786–1796
Chan DW et al (2008) Loss of MKP3 mediated by oxidative stress enhances tumorigenicity and chemoresistance of ovarian cancer cells. Carcinogenesis 29(9):1742–1750
Chiarugi P (2005) Review PTPs versus PTKs: the redox side of the coin. Free Radic Res 39(4):353–364
Ravid T et al (2004) C-Cbl-mediated ubiquitinylation is required for epidermal growth factor receptor exit from the early endosomes. J Biol Chem 279(35):37153–37162
Sarsour EH et al (2008) Manganese superoxide dismutase activity regulates transitions between quiescent and proliferative growth. Aging Cell 7(3):405–417
Wang M et al (2005) Manganese superoxide dismutase suppresses hypoxic induction of hypoxia-inducible factor-1 α and vascular endothelial growth factor. Oncogene 24(55):8154–8166
Srinivas US et al (2019) ROS and the DNA damage response in cancer. Redox Biol 25:101084
Macip S et al (2006) Oxidative stress induces a prolonged but reversible arrest in p53-null cancer cells, involving a Chk1-dependent G 2 checkpoint. Oncogene 25(45):6037–6047
Boutros R, Lobjois V, Ducommun B (2007) CDC25 phosphatases in cancer cells: key players? Good targets? Nat Rev Cancer 7(7):495–507
Xiao D et al (2005) Diallyl trisulfide-induced G 2–M phase cell cycle arrest in human prostate cancer cells is caused by reactive oxygen species-dependent destruction and hyperphosphorylation of Cdc25C. Oncogene 24(41):6256–6268
Brisson M et al (2007) Independent mechanistic inhibition of cdc25 phosphatases by a natural product caulibugulone. Mol Pharmacol 71(1):184–192
Okoh V et al (2015) Redox signalling to nuclear regulatory proteins by reactive oxygen species contributes to oestrogen-induced growth of breast cancer cells. Br J Cancer 112(10):1687–1702
Lee S-R et al (2002) Reversible inactivation of the tumor suppressor PTEN by H2O2. J Biol Chem 277(23):20336–20342
Salmeen A et al (2003) Redox regulation of protein tyrosine phosphatase 1B involves a sulphenyl-amide intermediate. Nature 423(6941):769–773
Wu H, Goel V, Haluska FG (2003) PTEN signaling pathways in melanoma. Oncogene 22(20):3113–3122
Liu L-Z et al (2006) Reactive oxygen species regulate epidermal growth factor-induced vascular endothelial growth factor and hypoxia-inducible factor-1α expression through activation of AKT and P70S6K1 in human ovarian cancer cells. Free Radic Biol Med 41(10):1521–1533
Brunet A et al (1999) Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor. Cell 96(6):857–868
Kawamura N et al (2007) Akt1 in osteoblasts and osteoclasts controls bone remodeling. PLoS One 2(10):e1058
Zhao Y et al (2017) ROS signaling under metabolic stress: cross-talk between AMPK and AKT pathway. Mol Cancer 16(1):79
Shi X et al (2012) Reactive oxygen species in cancer stem cells. Antioxid Redox Signal 16(11):1215–1228
Vafa O et al (2002) c-Myc can induce DNA damage, increase reactive oxygen species, and mitigate p53 function: a mechanism for oncogene-induced genetic instability. Mol Cell 9(5):1031–1044
Kasiappan R, Safe SH (2016) ROS-inducing agents for cancer chemotherapy. Reactive Oxygen Species 1(1):22–37-22–37
Wu W-S (2006) The signaling mechanism of ROS in tumor progression. Cancer Metastasis Rev 25(4):695–705
Rhyu DY et al (2005) Role of reactive oxygen species in TGF-β1-induced mitogen-activated protein kinase activation and epithelial-mesenchymal transition in renal tubular epithelial cells. J Am Soc Nephrol 16(3):667–675
Akhurst RJ, Derynck R (2001) TGF-β signaling in cancer—a double-edged sword. Trends Cell Biol 11:S44–S51
Ren Y et al (2005) Hepatocyte growth factor promotes cancer cell migration and angiogenic factors expression: a prognostic marker of human esophageal squamous cell carcinomas. Clin Cancer Res 11(17):6190–6197
Daveau M et al (2003) Hepatocyte growth factor, transforming growth factor α, and their receptors as combined markers of prognosis in hepatocellular carcinoma. Mol Carcinog 36(3):130–141
Ferraro D et al (2006) Pro-metastatic signaling by c-Met through RAC-1 and reactive oxygen species (ROS). Oncogene 25(26):3689–3698
Bae YS et al (2000) Platelet-derived growth factor-induced H2O2 production requires the activation of phosphatidylinositol 3-kinase. J Biol Chem 275(14):10527–10531
Chen X-L et al (2004) Superoxide, H2O2, and iron are required for TNF-α-induced MCP-1 gene expression in endothelial cells: role of Rac1 and NADPH oxidase. Am J Phys Heart Circ Phys 286(3):H1001–H1007
Cheng J-C, Klausen C, Leung PC (2010) Hydrogen peroxide mediates EGF-induced down-regulation of E-cadherin expression via p38 MAPK and snail in human ovarian cancer cells. Mol Endocrinol 24(8):1569–1580
Shin I et al (1999) Lysophosphatidic acid increases intracellular H2O2 by phospholipase D and RhoA in rat-2 fibroblasts. Mol Cells 9(3):292–299
Griendling KK et al (1994) Angiotensin II stimulates NADH and NADPH oxidase activity in cultured vascular smooth muscle cells. Circ Res 74(6):1141–1148
Rahman M (2016) Systems biology in cancer immunotherapy, vol 2. Bentham Science Publishers
Wang C-A et al (2014) Vascular endothelial growth factor C promotes breast cancer progression via a novel antioxidant mechanism that involves regulation of superoxide dismutase 3. Breast Cancer Res 16(5):462
Lee KH, Kim SW, Kim J-R (2009) Reactive oxygen species regulate urokinase plasminogen activator expression and cell invasion via mitogen-activated protein kinase pathways after treatment with hepatocyte growth factor in stomach cancer cells. J Exp Clin Cancer Res 28(1):73
Cheng G et al (2001) Homologs of gp91phox: cloning and tissue expression of Nox3, Nox4, and Nox5. Gene 269(1–2):131–140
Wedgwood S et al (2013) Increased p22phox/Nox4 expression is involved in remodeling through hydrogen peroxide signaling in experimental persistent pulmonary hypertension of the newborn. Antioxid Redox Signal 18(14):1765–1776
Edderkaoui M et al (2011) NADPH oxidase activation in pancreatic cancer cells is mediated through Akt-dependent up-regulation of p22phox. J Biol Chem 286(10):7779–7787
Lee JK et al (2007) NADPH oxidase promotes pancreatic cancer cell survival via inhibiting JAK2 dephosphorylation by tyrosine phosphatases. Gastroenterology 133(5):1637–1648
Maloney E et al (2009) Activation of NF-κB by palmitate in endothelial cells: a key role for NADPH oxidase-derived superoxide in response to TLR4 activation. Arterioscler Thromb Vasc Biol 29(9):1370–1375
Block K, Gorin Y (2012) Aiding and abetting roles of NOX oxidases in cellular transformation. Nat Rev Cancer 12(9):627–637
Kim J, Kim J, Bae J-S (2016) ROS homeostasis and metabolism: a critical liaison for cancer therapy. Exp Mol Med 48(11):e269–e269
D’Souza LC et al (2020) Oxidative stress and cancer development: are noncoding RNAs the missing links? Antioxid Redox Signal. https://doi.org/10.1089/ars.2019.7987
Liberti MV, Locasale JW (2016) The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci 41(3):211–218
Dang CV (2012) Links between metabolism and cancer. Genes Dev 26(9):877–890
Du W et al (2013) TAp73 enhances the pentose phosphate pathway and supports cell proliferation. Nat Cell Biol 15(8):991–1000
Aykin-Burns N et al (2009) Increased levels of superoxide and H2O2 mediate the differential susceptibility of cancer cells versus normal cells to glucose deprivation. Biochem J 418(1):29–37
Owada S et al (2013) Critical role of H2O2 generated by NOX4 during cellular response under glucose deprivation. PLoS One 8(3):e56628
Minamoto T, Ougolkov AV, Mai M (2002) Detection of oncogenes in the diagnosis of cancers with active oncogenic signaling. Expert Rev Mol Diagn 2(6):565–575
Xie H et al (2014) Targeting lactate dehydrogenase-a inhibits tumorigenesis and tumor progression in mouse models of lung cancer and impacts tumor-initiating cells. Cell Metab 19(5):795–809
Ganapathy-Kanniappan S, Geschwind J-FH (2013) Tumor glycolysis as a target for cancer therapy: progress and prospects. Mol Cancer 12(1):152
Serguienko A et al (2015) Metabolic reprogramming of metastatic breast cancer and melanoma by let-7a microRNA. Oncotarget 6(4):2451
Lockney NA et al (2015) Pyruvate kinase muscle isoenzyme 2 (PKM2) expression is associated with overall survival in pancreatic ductal adenocarcinoma. J Gastrointest Cancer 46(4):390–398
Taniguchi K et al (2016) PTBP1-associated microRNA-1 and-133b suppress the Warburg effect in colorectal tumors. Oncotarget 7(14):18940
Riganti C et al (2012) The pentose phosphate pathway: an antioxidant defense and a crossroad in tumor cell fate. Free Radic Biol Med 53(3):421–436
Mittler R (2017) ROS are good. Trends Plant Sci 22(1):11–19
Kim B, Song YS (2016) Mitochondrial dynamics altered by oxidative stress in cancer. Free Radic Res 50(10):1065–1070
Indo HP et al (2015) A mitochondrial superoxide theory for oxidative stress diseases and aging. J Clin Biochem Nutr 56(1):1–7
Cid-Castro C, Hernandez-Espinosa DR, Morán J (2018) ROS as regulators of mitochondrial dynamics in neurons. Cell Mol Neurobiol 38(5):995–1007
Zorov DB, Juhaszova M, Sollott SJ (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev 94(3):909–950
Zorov DB et al (2000) Reactive oxygen species (Ros-induced) Ros release: a new phenomenon accompanying induction of the mitochondrial permeability transition in cardiac myocytes. J Exp Med 192(7):1001–1014
Han Y et al (2019) Mitochondrial fission causes cisplatin resistance under hypoxic conditions via ROS in ovarian cancer cells. Oncogene 38(45):7089–7105
Sabouny R, Shutt TE (2020) Reciprocal regulation of mitochondrial fission and fusion. Trends Biochem Sci 45(7):564–577
Movafagh S, Crook S, Vo K (2015) Regulation of hypoxia-inducible factor-1a by reactive oxygen species: new developments in an old debate. J Cell Biochem 116(5):696–703
Lamberti MJ et al (2017) Transcriptional activation of HIF-1 by a ROS-ERK axis underlies the resistance to photodynamic therapy. PLoS One 12(5):e0177801
Hagen T (2012) Oxygen versus reactive oxygen in the regulation of HIF-1: the balance tips. Biochem Res Int 2012:436981
Kaewpila S et al (2008) Manganese superoxide dismutase modulates hypoxia-inducible factor-1α induction via superoxide. Cancer Res 68(8):2781–2788
Muñoz JP et al (2013) Mfn2 modulates the UPR and mitochondrial function via repression of PERK. EMBO J 32(17):2348–2361
Westermann B (2010) Mitochondrial fusion and fission in cell life and death. Nat Rev Mol Cell Biol 11(12):872–884
Archer SL (2013) Mitochondrial dynamics—mitochondrial fission and fusion in human diseases. N Engl J Med 369(23):2236–2251
Vásquez-Trincado C et al (2016) Mitochondrial dynamics, mitophagy and cardiovascular disease. J Physiol 594(3):509–525
Ghosh S et al (2015) Reactive oxygen species in the tumor niche triggers altered activation of macrophages and immunosuppression: role of fluoxetine. Cell Signal 27(7):1398–1412
Nathan C, Cunningham-Bussel A (2013) Beyond oxidative stress: an immunologist’s guide to reactive oxygen species. Nat Rev Immunol 13(5):349–361
Rutault K et al (1999) Reactive oxygen species activate human peripheral blood dendritic cells. Free Radic Biol Med 26(1–2):232–238
Schmielau J, Finn OJ (2001) Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of t-cell function in advanced cancer patients. Cancer Res 61(12):4756–4760
Malmberg K-J et al (2001) Inhibition of activated/memory (CD45RO+) T cells by oxidative stress associated with block of NF-κB activation. J Immunol 167(5):2595–2601
Li W et al (2008) NK cell apoptosis in coronary artery disease: relation to oxidative stress. Atherosclerosis 199(1):65–72
Yang Y et al (2013) Reactive oxygen species in the immune system. Int Rev Immunol 32(3):249–270
Herberman RB (2002) Cancer immunotherapy with natural killer cells. In: Seminars in oncology. Elsevier
Frey M et al (1998) Differential expression and function of L-selectin on CD56bright and CD56dim natural killer cell subsets. J Immunol 161(1):400–408
Romero AI et al (2006) NKp46 and NKG2D receptor expression in NK cells with CD56dim and CD56bright phenotype: regulation by histamine and reactive oxygen species. Br J Haematol 132(1):91–98
Harlin H et al (2007) The CD16− CD56bright NK cell subset is resistant to reactive oxygen species produced by activated granulocytes and has higher antioxidative capacity than the CD16+ CD56dim subset. J Immunol 179(7):4513–4519
Thorén FB et al (2007) The CD16−/CD56bright subset of NK cells is resistant to oxidant-induced cell death. J Immunol 179(2):781–785
Gupta S et al (2007) Differential sensitivity of naive and subsets of memory CD4+ and CD8+ T cells to hydrogen peroxide-induced apoptosis. Genes Immun 8(7):560–569
Mougiakakos D, Johansson CC, Kiessling R (2009) Naturally occurring regulatory T cells show reduced sensitivity toward oxidative stress–induced cell death. Blood 113(15):3542–3545
Nishikawa H, Sakaguchi S (2014) Regulatory T cells in cancer immunotherapy. Curr Opin Immunol 27:1–7
Jia W, Jackson-Cook C, Graf MR (2010) Tumor-infiltrating, myeloid-derived suppressor cells inhibit T cell activity by nitric oxide production in an intracranial rat glioma+ vaccination model. J Neuroimmunol 223(1–2):20–30
Harari O, Liao JK (2004) Inhibition of MHC II gene transcription by nitric oxide and antioxidants. Curr Pharm Des 10(8):893–898
Ohl K, Tenbrock K (2018) Reactive oxygen species as regulators of MDSC-mediated immune suppression. Front Immunol 9:2499
Korniluk A et al (2017) From inflammation to cancer. Ir J Med Sci 186(1):57–62
Trinchieri G (2011) Innate inflammation and cancer: is it time for cancer prevention? F1000 Med Rep 3:11
Singh N et al (2019) Inflammation and cancer. Ann Afr Med 18(3):121
Greten FR, Grivennikov SI (2019) Inflammation and cancer: triggers, mechanisms, and consequences. Immunity 51(1):27–41
Gonda TA, Tu S, Wang TC (2009) Chronic inflammation, the tumor microenvironment and carcinogenesis. Cell Cycle 8(13):2005–2013
Landskron G et al (2014) Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014:149185
Forrester SJ et al (2018) Reactive oxygen species in metabolic and inflammatory signaling. Circ Res 122(6):877–902
Kashyap D et al (2019) Role of reactive oxygen species in cancer progression. Curr Pharmacol Rep 5(2):79–86
Wu Y et al (2014) Molecular mechanisms underlying chronic inflammation-associated cancers. Cancer Lett 345(2):164–173
Reuter S et al (2010) Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med 49(11):1603–1616
Giannoni E, Parri M, Chiarugi P (2012) EMT and oxidative stress: a bidirectional interplay affecting tumor malignancy. Antioxid Redox Signal 16(11):1248–1263
Azad N, Rojanasakul Y, Vallyathan V (2008) Inflammation and lung cancer: roles of reactive oxygen/nitrogen species. J Toxicol Environ Health B Crit Rev 11(1):1–15
Gomes M et al (2016) Inflammation and lung cancer oxidative stress, ROS, and DNA damage. In: Reactive oxygen species in biology and human health. CRC Press
Cadet J, Davies KJ (2017) Oxidative DNA damage & repair: an introduction. Free Radic Biol Med 107:2–12
Karanjawala ZE et al (2002) Oxygen metabolism causes chromosome breaks and is associated with the neuronal apoptosis observed in DNA double-strand break repair mutants. Curr Biol 12(5):397–402
Cooke MS et al (2003) Oxidative DNA damage: mechanisms, mutation, and disease. FASEB J 17(10):1195–1214
Levine AS et al (2017) The oxidative DNA damage response: a review of research undertaken with Tsinghua and Xiangya students at the University of Pittsburgh. Sci China Life Sci 60(10):1077–1080
Traverso N et al (2013) Role of glutathione in cancer progression and chemoresistance. Oxidative Med Cell Longev 2013:972913
Maya-Mendoza A et al (2015) Myc and Ras oncogenes engage different energy metabolism programs and evoke distinct patterns of oxidative and DNA replication stress. Mol Oncol 9(3):601–616
Park M et al (2014) Novel signaling axis for ROS generation during K-Ras-induced cellular transformation. Cell Death Discov 21(8):1185–1197
Meng Y et al (2018) DUOXA1-mediated ROS production promotes cisplatin resistance by activating ATR-Chk1 pathway in ovarian cancer. Cancer Lett 428:104–116
Graindorge D et al (2015) Singlet oxygen-mediated oxidation during UVA radiation alters the dynamic of genomic DNA replication. PLoS One 10(10):e0140645
Somyajit K et al (2017) Redox-sensitive alteration of replisome architecture safeguards genome integrity. Science 358(6364):797–802
Sedletska Y, Radicella JP, Sage E (2013) Replication fork collapse is a major cause of the high mutation frequency at three-base lesion clusters. Nucleic Acids Res 41(20):9339–9348
Fruehauf JP, Meyskens FL (2007) Reactive oxygen species: a breath of life or death? Clin Cancer Res 13(3):789–794
Halliwell B (2007) Oxidative stress and cancer: have we moved forward? Biochem J 401(1):1–11
Qing X et al (2019) Prognostic significance of 8-hydroxy-2′-deoxyguanosine in solid tumors: a meta-analysis. BMC Cancer 19(1):997
Jaruga P, Rodriguez H, Dizdaroglu M (2001) Measurement of 8-hydroxy-2′-deoxyadenosine in DNA by liquid chromatography/mass spectrometry. Free Radic Biol Med 31(3):336–344
Valavanidis A, Vlachogianni T, Fiotakis C (2009) 8-hydroxy-2′-deoxyguanosine (8-OHdG): a critical biomarker of oxidative stress and carcinogenesis. J Environ Sci Health C 27(2):120–139
Hajas G et al (2013) 8-Oxoguanine DNA glycosylase-1 links DNA repair to cellular signaling via the activation of the small GTPase Rac1. Free Radic Biol Med 61:384–394
Tudek B et al (2010) Involvement of oxidatively damaged DNA and repair in cancer development and aging. Am J Transl Res 2(3):254
Opresko PL et al (2005) Oxidative damage in telomeric DNA disrupts recognition by TRF1 and TRF2. Nucleic Acids Res 33(4):1230–1239
Coluzzi E et al (2014) Oxidative stress induces persistent telomeric DNA damage responsible for nuclear morphology change in mammalian cells. PLoS One 9(10):e110963
Gisselsson D et al (2001) Telomere dysfunction triggers extensive DNA fragmentation and evolution of complex chromosome abnormalities in human malignant tumors. Proc Natl Acad Sci 98(22):12683–12688
Grimes DR et al (2014) A method for estimating the oxygen consumption rate in multicellular tumour spheroids. J R Soc Interface 11(92):20131124
Pittman RN (2013) Oxygen transport in the microcirculation and its regulation. Microcirculation 20(2):117–137
Felmeden D, Blann A, Lip G (2003) Angiogenesis: basic pathophysiology and implications for disease. Eur Heart J 24(7):586–603
Bergers G, Benjamin LE (2003) Tumorigenesis and the angiogenic switch. Nat Rev Cancer 3(6):401–410
Kim Y-M et al (2017) ROS-induced ROS release orchestrated by Nox4, Nox2, and mitochondria in VEGF signaling and angiogenesis. Am J Phys Cell Phys 312(6):C749–C764
Varol M (2017) Angiogenesis as an important target in cancer therapies. Researches on Science and Art in 21st Century Turkey. Gece Publishing, Turkey, pp 1971–1981
Salajegheh A (2016) Angiogenesis in health, disease and malignancy. Springer
Carmeliet P (2005) Angiogenesis in life, disease and medicine. Nature 438(7070):932–936
Weis SM, Cheresh DA (2011) Tumor angiogenesis: molecular pathways and therapeutic targets. Nat Med 17(11):1359
Granger DN, Kvietys PR (2015) Reperfusion injury and reactive oxygen species: the evolution of a concept. Redox Biol 6:524–551
Hsieh C-H et al (2010) Cycling hypoxia increases U87 glioma cell radioresistance via ROS induced higher and long-term HIF-1 signal transduction activity. Oncol Rep 24(6):1629–1636
Toffoli S et al (2009) Intermittent hypoxia is an angiogenic inducer for endothelial cells: role of HIF-1. Angiogenesis 12(1):47–67
Wang Z et al (2015) Broad targeting of angiogenesis for cancer prevention and therapy. In: Seminars in cancer biology. Elsevier
Kim Y-W, Byzova TV (2014) Oxidative stress in angiogenesis and vascular disease. Blood 123(5):625–631
Talmadge JE, Fidler IJ (2010) AACR centennial series: the biology of cancer metastasis: historical perspective. Cancer Res 70(14):5649–5669
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285(21):1182–1186
Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407(6801):249–257
Gullino PM (1978) Angiogenesis and oncogenesis. Oxford University Press
Talkenberger K et al (2017) Amoeboid-mesenchymal migration plasticity promotes invasion only in complex heterogeneous microenvironments. Sci Rep 7(1):1–12
Kim Y-N et al (2012) Anoikis resistance: an essential prerequisite for tumor metastasis. Int J Cell Biol 2012:306879
Clark AG, Vignjevic DM (2015) Modes of cancer cell invasion and the role of the microenvironment. Curr Opin Cell Biol 36:13–22
Smith HA, Kang Y (2013) The metastasis-promoting roles of tumor-associated immune cells. J Mol Med 91(4):411–429
Nishikawa M (2008) Reactive oxygen species in tumor metastasis. Cancer Lett 266(1):53–59
Denisenko TV, Gorbunova AS, Zhivotovsky B (2019) Mitochondrial involvement in migration, invasion and metastasis. Front Cell Develop Biol 7:355
Chaffer CL, Weinberg RA (2011) A perspective on cancer cell metastasis. Science 331(6024):1559–1564
Lamouille S, Xu J, Derynck R (2014) Molecular mechanisms of epithelial–mesenchymal transition. Nat Rev Mol Cell Biol 15(3):178
Lu W, Kang Y (2019) Epithelial-mesenchymal plasticity in cancer progression and metastasis. Dev Cell 49(3):361–374
Pani G, Galeotti T, Chiarugi P (2010) Metastasis: cancer cell’s escape from oxidative stress. Cancer Metastasis Rev 29(2):351–378
Liao Z, Chua D, Tan NS (2019) Reactive oxygen species: a volatile driver of field cancerization and metastasis. Mol Cancer 18(1):65
Thews O, Riemann A (2019) Tumor pH and metastasis: a malignant process beyond hypoxia. Cancer Metastasis Rev 38(1–2):113–129
Lu J (2019) The Warburg metabolism fuels tumor metastasis. Cancer Metastasis Rev 38(1–2):157–164
Saitoh M (2018) Regulation of EMT by TGF-β signaling in cancer cells, in regulation of signal transduction in human cell research. Springer, pp 71–84
Radisky DC et al (2005) Rac1b and reactive oxygen species mediate MMP-3-induced EMT and genomic instability. Nature 436(7047):123–127
Binker MG et al (2009) EGF promotes invasion by PANC-1 cells through Rac1/ROS-dependent secretion and activation of MMP-2. Biochem Biophys Res Commun 379(2):445–450
Kheradmand F et al (1998) Role of Rac1 and oxygen radicals in collagenase-1 expression induced by cell shape change. Science 280(5365):898–902
Lam C et al (2013) Loss of TAK1 increases cell traction force in a ROS-dependent manner to drive epithelial–mesenchymal transition of cancer cells. Cell Death Dis 4(10):e848–e848
Pelicano H et al (2009) Mitochondrial dysfunction and reactive oxygen species imbalance promote breast cancer cell motility through a CXCL14-mediated mechanism. Cancer Res 69(6):2375–2383
Zhu P et al (2011) Angiopoietin-like 4 protein elevates the prosurvival intracellular O2−: H2O2 ratio and confers anoikis resistance to tumors. Cancer Cell 19(3):401–415
Du S et al (2018) NADPH oxidase 4 regulates anoikis resistance of gastric cancer cells through the generation of reactive oxygen species and the induction of EGFR. Cell Death Dis 9(10):1–18
Kim H et al (2017) Regulation of anoikis resistance by NADPH oxidase 4 and epidermal growth factor receptor. Br J Cancer 116(3):370–381
Amri F et al (2017) Neuroglobin protects astroglial cells from hydrogen peroxide-induced oxidative stress and apoptotic cell death. J Neurochem 140(1):151–169
Kim J-Y, Park J-H (2003) ROS-dependent caspase-9 activation in hypoxic cell death. FEBS Lett 549(1–3):94–98
Radogna F et al (2016) Cell type-dependent ROS and mitophagy response leads to apoptosis or necroptosis in neuroblastoma. Oncogene 35(29):3839–3853
Ravindran J et al (2011) Modulation of ROS/MAPK signaling pathways by okadaic acid leads to cell death via, mitochondrial mediated caspase-dependent mechanism. Apoptosis 16(2):145–161
Shen C et al (2017) Aldehyde dehydrogenase 2 deficiency negates chronic low-to-moderate alcohol consumption-induced cardioprotection possibly via ROS-dependent apoptosis and RIP1/RIP3/MLKL-mediated necroptosis. Biochim Biophys Acta 1863(8):1912–1918
Holze C et al (2018) Oxeiptosis, a ROS-induced caspase-independent apoptosis-like cell-death pathway. Nat Immunol 19(2):130–140
Bryan HK et al (2013) The Nrf2 cell defence pathway: Keap1-dependent and-independent mechanisms of regulation. Biochem Pharmacol 85(6):705–717
Wang Z et al (2012) The mitochondrial phosphatase PGAM5 functions at the convergence point of multiple necrotic death pathways. Cell 148(1–2):228–243
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta 1863(12):2977–2992
Li D et al (2004) Reactive oxygen species (ROS) control the expression of Bcl-2 family proteins by regulating their phosphorylation and ubiquitination. Cancer Sci 95(8):644–650
Hildeman DA et al (2003) Control of Bcl-2 expression by reactive oxygen species. Proc Natl Acad Sci 100(25):15035–15040
Li Z et al (2011) Mitochondrial ROS generation for regulation of autophagic pathways in cancer. Biochem Biophys Res Commun 414(1):5–8
Zhang J, Ney PA (2009) Role of BNIP3 and NIX in cell death, autophagy, and mitophagy. Cell Death Differ 16(7):939–946
Novak I (2012) Mitophagy: a complex mechanism of mitochondrial removal. Antioxid Redox Signal 17(5):794–802
Youle RJ, Narendra DP (2011) Mechanisms of mitophagy. Nat Rev Mol Cell Biol 12(1):9–14
Taguchi K et al (2012) Keap1 degradation by autophagy for the maintenance of redox homeostasis. Proc Natl Acad Sci 109(34):13561–13566
Pelicano H et al (2003) Inhibition of mitochondrial respiration a novel strategy to enhance drug-induced apoptosis in human leukemia cells by a reactive oxygen species-mediated mechanism. J Biol Chem 278(39):37832–37839
Lo Y-L, Wang W (2013) Formononetin potentiates epirubicin-induced apoptosis via ROS production in HeLa cells in vitro. Chem Biol Interact 205(3):188–197
Marchetti M et al (2009) Sulindac enhances the killing of cancer cells exposed to oxidative stress. PLoS One 4(6):e5804
Koleini N et al (2019) Oxidized phospholipids in doxorubicin-induced cardiotoxicity. Chem Biol Interact 303:35–39
Tsang W et al (2003) Reactive oxygen species mediate doxorubicin induced p53-independent apoptosis. Life Sci 73(16):2047–2058
Varol M (2016) Ultrasound-mediated cancer therapy as a noninvasive and repeatable treatment strategy. J App Pharm 8:e109
Varol M (2015) An alternative treatment modality of diseases using photodynamic therapy with a wide range biological targeting possibility. Res J Biol 3:21–25
Varol M (2020) Photodynamic therapy assay. Methods Mol Biol 2109:241–250
You DG et al (2016) ROS-generating TiO 2 nanoparticles for non-invasive sonodynamic therapy of cancer. Sci Rep 6:23200
Maeda H et al (2004) Effective treatment of advanced solid tumors by the combination of arsenic trioxide and L-buthionine-sulfoximine. Cell Death Differ 11(7):737–746
Trachootham D et al (2006) Selective killing of oncogenically transformed cells through a ROS-mediated mechanism by β-phenylethyl isothiocyanate. Cancer Cell 10(3):241–252
Dragovich T et al (2007) Phase I trial of imexon in patients with advanced malignancy. J Clin Oncol 25(13):1779–1784
Lambert JD, Elias RJ (2010) The antioxidant and pro-oxidant activities of green tea polyphenols: a role in cancer prevention. Arch Biochem Biophys 501(1):65–72
Rani K (2017) Role of antioxidants in prevention of diseases. J Appl Biotechnol Bioeng 4(1):00091
Middha P et al (2017) β-carotene supplementation and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: the role of tar and nicotine. Nicotine Tob Res 21(8):1045–1050
Omenn GS et al (1996) Effects of a combination of beta carotene and vitamin a on lung cancer and cardiovascular disease. N Engl J Med 334(18):1150–1155
Klein EA et al (2011) Vitamin E and the risk of prostate cancer: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 306(14):1549–1556
Okon IS, Zou M-H (2015) Mitochondrial ROS and cancer drug resistance: implications for therapy. Pharmacol Res 100:170–174
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Varol, M. (2020). ROS and Oxidative Stress in Cancer: Recent Advances. In: Tuli, H.S. (eds) Drug Targets in Cellular Processes of Cancer: From Nonclinical to Preclinical Models. Springer, Singapore. https://doi.org/10.1007/978-981-15-7586-0_6
Download citation
DOI: https://doi.org/10.1007/978-981-15-7586-0_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-7585-3
Online ISBN: 978-981-15-7586-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)