Abstract
Telocytes (TCs) are interstitial cells described in multiple structures, including the gastrointestinal tract, respiratory tract, urinary tract, uterus, and heart. Several studies have indicated the possibility that TCs are involved in the pacemaker potential in these organs. It is supposed that TCs are interacting with the neighboring muscular cells and their network contributes to the initiation and propagation of the electrical potentials. In order to understand the contribution of TCs to various excitability mechanisms, it is necessary to analyze the plasma membrane proteins (e.g., ion channels) functionally expressed in these cells. So far, potassium, calcium, and chloride currents, but not sodium currents, have been described in TCs in primary cell culture from different tissues. Moreover, TCs have been described as sensors for mechanical stimuli (e.g., contraction, extension, etc.). In conclusion, TCs might play an essential role in gastrointestinal peristalsis, in respiration, in pregnant uterus contraction, or in miction, but further highlighting studies are necessary to understand the molecular mechanisms and the cell-cell interactions by which TCs contribute to the tissue excitability and pacemaker potentials initiation/propagation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Telocytes
- Interstitial cells of Cajal
- In vitro electrophysiology
- Patch clamp
- Potassium currents
- Calcium currents
- Chloride currents
- Pacemaker potential
19.1 Introduction
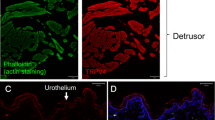
Telocytes (TCs) have been described in a variety of tissues/organs, including the gastrointestinal tract (colon, small intestine, etc.), urinary tract (urethra, prostate, etc.), respiratory tract (lungs, trachea, esophagus, etc.), skeletal muscle, heart, liver, kidney, skin, eye, etc. [1–16]. Extensive immunohistochemical and electron microscopy studies have been conducted on TCs, but their unique features and dynamic changes in cell culture limited the in vitro electrophysiological analysis [17, 18]. In the last years, several patch-clamp studies have been done on TCs in order to identify the ion channels functionally expressed in these cells and to understand their possible contribution to pacemaker potentials. In this chapter will be presented the most recent in vitro electrophysiological studies conducted on TCs from different tissues and the current conclusions based on these studies. At the end of the chapter are discussed some open questions concerning the role played by TCs in the various organs.
19.2 Which Ion Channels Are Functionally Expressed in Telocytes?
Interstitial cells (IC), interstitial cells of Cajal (ICC), interstitial Cajal-like cells (ICLC), and telocytes (TC) were studied in terms of ion channels in a manner which highlights the functions of these cells (Table 19.1). Their distribution in different tissues influenced the evaluation of potential roles played by these cells. It can be assumed that the existence of long extensions, the cell motility, and the ability to develop gap junctions with neighboring cells influence the type of ion channels expressed and their degree of activation and local functions.
19.2.1 Potassium Currents
Voltage-sensitive potassium channels Kv7.5 are involved in the excitation of the interstitial cells of Cajal (ICC) associated with the myenteric plexus but not with those associated with the submuscular plexus of the colon [19]. Immunohistochemical and qRT-PCR characterization revealed the presence of Kv7.5 channels in the colonic ICC. Carbachol, a muscarinic acetylcholine receptor agonist, inhibited the potassium currents, indicating a cholinergic-dependent activation of the voltage-sensitive potassium channels. Moreover, XE991, a specific Kv7 channel blocker, was able to abolish completely the potassium currents [19]. These currents are very similar to the inwardly rectifying maxi-chloride currents that were previously described in the ICC associated with the mouse myenteric plexus from the small intestine [29]. Generally, the M-current is carried through heteromeric Kv7.2 and Kv7.3, Kv7.3 and Kv7.5, or Kv7.4 and Kv7.5, but in the case of colonic ICC, the current seems to be carried exclusively through homomeric Kv7.5 channels [19, 30–32]. By contrast to the myocytes, the ICC in the prostate are characterized by the absence of sensitive outward potassium currents [20]. Hyperpolarization-activated cyclic nucleotide currents (HCN) have been also described in mouse colonic ICC, but only HCN1 and HCN3 channel transcripts were detected [24].
ICC’s presence was previously described in the atrial and ventricular myocardium [33, 34]. In order to understand the role played by TCs in heart contractility, a detailed analysis of the existing potassium currents was done. In atrial and ventricular TCs have been evidenced large conductance Ca2+-activated potassium currents (BKCa) and inwardly rectifying potassium currents (Kir), by applying paxilline and naringenin, or Ba2+, respectively. However, in these cells neither potassium outward currents nor the ATP-sensitive potassium currents have been identified by applying 4-aminopyridine, or pinacidil, respectively [21]. The presence of small-conductance calcium-activated potassium channels (SKCa) was also confirmed in human uterine TCs; their mRNA levels were significantly lower in pregnant myometrium compared to nonpregnant myometrium; and SK activators were suggested to reduce contractility in human myometrium [23].
19.2.2 Calcium Currents
Voltage-gated L-type calcium channels were evidenced in the urinary bladder based on nifedipine and Bay K 8644 response [26], prostate based on nifedipine response [20], and myometrium [27] based on TCs. These channels have different roles in other cell types. Voltage-gated L-type calcium channels are involved in heart automaticity [35–38]. TCs were identified in the heart [39], and it is possible that these cells possess such properties. Changes in urinary bladder function are made by streptozotocin-induced diabetes [40] and hypercholesterolemia [41] via voltage-gated L-type calcium channels. This may correlate with the involvement of these channels in cellular electrical automatism, in a manner relatively independent of tissue. TCs have the ability to achieve gap junctions with surrounding cells, and linking these issues may explain the existence of this automatism on the tissue. Androgens induce intracellular calcium increase via voltage-gated L-type calcium channels in prostate cancer cells [42]. This could explain the involvement of these channels in cell growth and multiplication. By extension, it is important to verify if these channels are involved in the cellular growth and multiplication in physiological conditions.
Voltage-gated L-type calcium channels are involved in augmentation of spontaneous uterine contractility in pregnant rat modulated by protease-activated receptor 2 [43]. This modulation of rhythmic contractions can be extrapolated that is important at TC level and not just at tissue and organ levels, due to long cell extensions that are influenced by mechanical forces and due to gap junctions of TCs. Voltage-gated L-type calcium channels are modulated by alpha5beta1 integrin-fibronectin interactions, with a role in myogenic tone and vascular wall remodeling [44]. Modulation of L-type Ca2+ channels by hypoxia [45] can create a logical link in the pathophysiological mechanism, explaining the importance of these channels at TC in the muscle tissue under the influence promoting automatism, but also on the tissue by integrating interactions between TCs and muscle cells, and achieving feedback loops that include various other factors such as the vascular factors and humoral factors consecutively.
Voltage-gated T-type calcium channels (Cav3.1 and Cav3.2 subunits) were evidenced in the urinary bladder [26], prostate [20], and myometrium [27] on cultured TC and tissue strips. These channels play various roles in the smooth muscle wall of the blood vessels. Cav3.1 has a role on the blood vessel relaxation in an NO-dependent manner [46] and can induce myogenic constriction in the mesenteric vessels [47] and hypoxia-dependent pulmonary vasoconstriction [48]. These dual behaviors and the dependence on hypoxia may be extrapolated to myometrium, emphasizing the role of TC in uterus development and growth under hypoxic conditions, or even in birth control. Cav3.2 has a role in the relaxation of coronary vascular smooth muscles [49] and augmented contractility during oxidative stress [50]. Cav3.2 functions of myometrium TCs may be involved in fetal growth vascular adaptation.
Intracellular Ca2+ concentration is an important excitability regulator in ICC, and besides the L-type and T-type calcium channels, the sodium-calcium exchanger (NCX3) contributes to the calcium homeostasis in the rat bladder [51].
19.2.3 Chloride Currents
Human myometrial TCs have been described to present calcium-dependent hyperpolarization-activated chloride inward currents [9]. Ca2+-activated Cl− channels on ICC were highlighted indirectly by chloride concentration modulation [52] and subsequently by response to CdCl2 and CsCl [9] and response to niflumic acid [20].
19.2.4 Sodium Currents
Electrophysiological studies on the human myometrium failed to prove the presence of Na+ currents in TCs [9, 22].
19.3 Are Telocytes Involved in the Pacemaker Activity?
Different types of cells, including ICC/TCs, can induce these changes through intracellular mediators, dynamic changes of ionic concentrations, or other local stimulating factors and can contribute to the existence of spontaneous electrical activity in various areas associated with initiation/propagation of pacemaker activities (Table 19.2).
19.3.1 Role of Telocytes in the Pacemaker Activity of Internal Cavitary Organs
ICC-like cells isolated from the urethra [58, 59], bladder [62], prostate [63], corpus cavernosum [64], small intestine [56], embryonic intestine [55], Fallopian tube [60], and myometrium [61] present rhythmic firing activities acting also as neuromodulators [65]. These cells which act as pacemakers can modulate the activities of muscular, nervous, or secretory systems. In ICC from the guinea pig prostate, the spontaneous transient depolarizations are initiated with the opening of a small number of Ca2+-activated Cl− channels followed by a small membrane depolarization which triggers the calcium influx through T-type calcium channels, and furthermore the summation of calcium transients would manifest in the pacemaker potential that opens L-type calcium channels in ICC and their neighboring smooth muscle cells [20].
Patch-clamp experiments using cultured ICC from Balb/C mice urinary bladder revealed that these cells act as pacemaker, presenting individual spikes and bursting potentials similar to those observed in intact bladder tissues [53]. These spontaneous electrical potentials were inhibited by nifedipine (L-type voltage-gated calcium channel blocker) suggesting the involvement of these types of calcium channels [53]. Another study conducted on the rat bladder shows that spontaneous calcium activity is not influenced by L-type Ca2+ channels but rather by the T-type calcium channels [66]. The carbachol-induced calcium oscillations were blocked by atropine (a muscarinic receptor antagonist) [53, 54]. These findings suggested the possible role of voltage-gated calcium channels and muscarinic receptors in generating the pacemaker behavior in bladder ICC.
Although, electrophysiological recordings on TCs from human myometrium failed to prove the presence of Na+ currents [9, 22], studies on transgenic mice have proved that longitudinal contractions of the uterus depend on a KIT signaling pathway of ICC-like cells [67]. On the other hand, the spontaneous electrical activity recorded on the ICC urinary bladder, small intestine, or urethra is based on intracellular calcium changes [53–59].
Calcium imaging on urethra ICC suggests that PKA, RyR, IP3R, and NCX are involved in ICC pacemaker activity [58, 59, 65]. The pacemaker activity in small intestine ICC is modulated through 5-HT3 and 5-HT4 receptors, chloride channels, Ca2+-ATPase from the endoplasmic reticulum, phospholipase A, phospholipase C, phospholipase D, and TRPC3 [56, 57]. Calcium imaging studies on embryonic mouse intestinal ICC showed the role of L-type voltage-gated calcium channels in rhythmic electric activities [55]. These results revealed that the pacemaker mechanism is more complex and needs to be studied in an integrated manner. Calcium imaging studies on embryonic mouse intestinal ICC showed the role of L-type voltage-gated calcium channels in rhythmic electric activities [55]. In human myometrium and Fallopian tubes, Cajal-like cells/TC present spontaneous electric activity without a rhythmical pattern [60, 61].
ICC have been proposed to be the pacemaker cells in the gastrointestinal tract. In the small intestine, ICC associated with the myenteric plexus are generating slow waves that contribute to the rhythmic muscle contractions in the proximal intestine [68]. In the colon, ICC associated with the submuscular plexus contribute to slow waves in canine, rat, mouse, and human [69–73], while ICC associated with the myenteric plexus do not contribute to slow waves in rat and mouse but generate rhythmic transient depolarizations of low and variable frequency as a result of L-type calcium channels activation [72, 73]. In the colon, ICC associated with myenteric plexus and intramuscular plexus are cooperating for the generation of pacemaker activity, and their excitability is regulated by the cholinergic inhibition of Kv7.5 channels [19]. Hyperpolarization-activated cyclic nucleotide currents from mouse colonic ICC are tonically activated by basal cAMP production and participate in the regulation of the pacemaker activity [24].
19.3.2 Role of Telocytes in the Pacemaker Activity of the Heart
Cav3.1 plays a role in sinoatrial node automaticity [74] and atrioventricular node automaticity [75]. Extrapolation of Cav3.1 involvement in TC automatism or in tissues containing TC automatism requires further investigations. Cardiac TCs have been suggested to be implicated in cardiac rhythm and atrial fibrillation [76, 77].
Sodium-calcium exchanger is involved in the pacemaker activity of the sinoatrial node [78] and in the overactive bladder in transgenic mice overexpressing NCX1.3 [79]. It is assumed that the activity of NCX on TC is modulated by ionic concentrations, by gap junctions, and telepods length that can develop the pacemaker functionality of a tissue rather than of individual and independent cells.
Ca2+-activated Cl− channels are found in many cell types and have different roles, among them being cardiac rhythmic depolarization, modulation of smooth muscle contraction, and taste receptor modulation. Their role is unknown in TCs, but the ability of these cells to have long extensions, gap junctions, and an increased dynamic of telepods apparently without stimulus creates opportunities for studying TC behavior under the influence of Ca2+-activated Cl− channels. TC feature to have a rhythmic electrical activity could be attributed to these channels. In vivo gap junctions between TC and adjacent cells could explain TC calcium dynamics changes in the presence of neighboring muscle cells and also the lack of in vivo electric automatism in the absence of gap junctions. Further studies are needed to assess the role of Ca2+-activated Cl− channels in TCs and their possible modulatory effect on chemoreceptors.
19.4 What’s Next?
19.4.1 TCs Are Sensitive to Stimuli That Modulate Membrane Fluidity
It was evidenced that TC uterine motility can be modulated by mechanical stimuli via optical tweezer [28]. Blocking the voltage-gated T-type calcium channels, which have a degree of mechanosensitivity, decreases this optical modulation by means of mechanical forces. Channels that have a degree of mechanosensitivity are sensitive to external mechanical stimulation but also to changes in membrane fluidity. Imatinib, a tyrosine kinase inhibitor that can be used in treating patients with chronic myeloid leukemia, may alter membrane fluidity through alteration of lipid metabolism [80]. Imatinib can decrease spontaneous contractile activity in guinea pig models and in human nonpregnant myometrium [81, 82]. Moreover, any change in the concentration of steroid hormones can cause changes in membrane fluidity and influence the functionality of mechanosensitive-like ion channels.
Future studies should focus on cell-cell communication and to explore the influence exerted on TC function by the surrounding myocytes through various factors that might affect membrane fluidity. Our hypothesis is that TCs could be involved in the stimulation of muscle development where mechanical stress is elevated (e.g., uterine musculature). Besides the uterus, TCs may represent a mechanical sensor that contributes to the pacemaker activity in the heart, gastrointestinal tract, or urinary tract.
19.4.2 Hormonal Regulation of TCs: Role in Birth Delivery
We hypothesize the TCs involvement in a feedback loop control of uterus that triggers the contraction initiation in birth delivery. The plasticity of the uterine musculature in pregnancy [83] might be under the influence of TCs that can modulate the activity of the surrounding myocytes. Rhythmic muscular activities are associated to significant vascular changes in the uterus involving endocrine and humoral factors release that could be detected by TCs.
The increase in placental volume and the level of secreted steroid hormones can modulate the cellular membrane fluidity [84, 85] and subsequently the activity of TCs, the function of myocytes, the frequency and force of contractions, and finally the endocrine feedback loop leading to fetal expulsion. These hypotheses should be tested in future studies on the interactions of TCs with surrounding cells in a such manner that can integrate mechanical and hormonal modulation with the therapeutic purpose of preventing the premature birth.
19.4.3 Integrating Information About TCs
There is a lack of comprehensive knowledge on the ion channels functionally expressed in TCs due to the variety of experimental approaches, including species, age differences, and methodology of analysis (in vitro and in vivo studies, staining on living and fixed tissue, presence or absence of neighboring cells, etc.). An important limitation in clinical studies is represented by the reduced number of samples from patients.
The studies conducted so far led to the hypothesis that TCs play a role in intercellular communication. However, the role of TCs in tissue excitability and pacemaker activity is still unclear. Therefore, it is imperative to connect all the information available on TCs and to understand their physiological role and their involvement in a variety of pathological conditions (e.g., psoriasis, myocardial infarction, focal lymphocytic sialadenitis, preeclampsia, ulcerative colitis, etc.) [86–90]. In conclusion, it is a great challenge to explain how TCs with distinct protein expression profiles (e.g., ion channels) from different tissues are correlated with similar functions, morphology, and dynamics of these cells.
References
Ceafalan L, Gherghiceanu M, Popescu LM, Simionescu O. Telocytes in human skin – are they involved in skin regeneration? J Cell Mol Med. 2012;16(7):1405–20.
Gevaert T, De Vos R, Van Der Aa F, Joniau S, van den Oord J, Roskams T, De Ridder D. Identification of telocytes in the upper lamina propria of the human urinary tract. J Cell Mol Med. 2012;16(9):2085–93.
Koh BH, Roy R, Hollywood MA, Thornbury KD, McHale NG, Sergeant GP, Hatton WJ, Ward SM, Sanders KM, Koh SD. Platelet-derived growth factor receptor-α cells in mouse urinary bladder: a new class of interstitial cells. J Cell Mol Med. 2012;16(4):691–700.
Rusu MC, Nicolescu MI, Jianu AM, Lighezan R, Mănoiu VS, Păduraru D. Esophageal telocytes and hybrid morphologies. Cell Biol Int. 2012;36(12):1079–88.
Rusu MC, Jianu AM, Mirancea N, Didilescu AC, Mănoiu VS, Păduraru D. Tracheal telocytes. J Cell Mol Med. 2012;16(2):401–5.
Suciu LC, Popescu BO, Kostin S, Popescu LM. Platelet-derived growth factor receptor-β-positive telocytes in skeletal muscle interstitium. J Cell Mol Med. 2012;16(4):701–7.
Qi G, Lin M, Xu M, Manole CG, Wang X, Zhu T. Telocytes in the human kidney cortex. J Cell Mol Med. 2012;16(12):3116–22.
Corradi LS, Jesus MM, Fochi RA, Vilamaior PS, Justulin Jr LA, Góes RM, Felisbino SL, Taboga SR. Structural and ultrastructural evidence for telocytes in prostate stroma. J Cell Mol Med. 2013;17(3):398–406.
Cretoiu SM, Cretoiu D, Marin A, Radu BM, Popescu LM. Telocytes: ultrastructural, immunohistochemical and electrophysiological characteristics in human myometrium. Reproduction. 2013;145(4):357–70.
Díaz-Flores L, Gutiérrez R, Sáez FJ, Díaz-Flores Jr L, Madrid JF. Telocytes in neuromuscular spindles. J Cell Mol Med. 2013;17(4):457–65.
Luesma MJ, Gherghiceanu M, Popescu LM. Telocytes and stem cells in limbus and uvea of mouse eye. J Cell Mol Med. 2013;17(8):1016–24.
Matyja A, Gil K, Pasternak A, Sztefko K, Gajda M, Tomaszewski KA, Matyja M, Walocha JA, Kulig J, Thor P. Telocytes: new insight into the pathogenesis of gallstone disease. J Cell Mol Med. 2013;17(6):734–42.
Vannucchi MG, Traini C, Manetti M, Ibba-Manneschi L, Faussone-Pellegrini MS. Telocytes express PDGFRα in the human gastrointestinal tract. J Cell Mol Med. 2013;17(9):1099–108.
Xiao J, Wang F, Liu Z, Yang C. Telocytes in liver: electron microscopic and immunofluorescent evidence. J Cell Mol Med. 2013;17(12):1537–42.
Zhao B, Chen S, Liu J, Yuan Z, Qi X, Qin J, Zheng X, Shen X, Yu Y, Qnin TJ, Chan JY, Cai D. Cardiac telocytes were decreased during myocardial infarction and their therapeutic effects for ischaemic heart in rat. J Cell Mol Med. 2013;17(1):123–33.
Li L, Lin M, Li L, Wang R, Zhang C, Qi G, Xu M, Rong R, Zhu T. Renal telocytes contribute to the repair of ischemically injured renal tubules. J Cell Mol Med. 2014;18(6):1144–56.
Niculite CM, Regalia TM, Gherghiceanu M, Huica R, Surcel M, Ursaciuc C, Leabu M, Popescu LM. Dynamics of telopodes (telocyte prolongations) in cell culture depends on extracellular matrix protein. Mol Cell Biochem. 2015;398(1–2):157–64.
Roatesi I, Radu BM, Cretoiu D, Cretoiu SM. Uterine telocytes: a review of current knowledge. Biol Reprod. 2015;93(1):10.
Wright GW, Parsons SP, Loera-Valencia R, Wang XY, Barajas-López C, Huizinga JD. Cholinergic signalling-regulated KV7.5 currents are expressed in colonic ICC-IM but not ICC-MP. Pflugers Arch. 2014;466(9):1805–18.
Lang RJ, Tonta MA, Takano H, Hashitani H. Voltage-operated Ca2+ currents and Ca2+ -activated Cl- currents in single interstitial cells of the guinea pig prostate. BJU Int. 2014;114(3):436–46.
Sheng J, Shim W, Lu J, Lim SY, Ong BH, Lim TS, Liew R, Chua YL, Wong P. Electrophysiology of human cardiac atrial and ventricular telocytes. J Cell Mol Med. 2014;18(2):355–62.
Duquette RA, Shmygol A, Vaillant C, Mobasheri A, Pope M, Burdyga T, Wray S. Vimentin-positive, c-kit-negative interstitial cells in human and rat uterus: a role in pacemaking? Biol Reprod. 2005;72(2):276–83.
Rosenbaum ST, Svalø J, Nielsen K, Larsen T, Jørgensen JC, Bouchelouche P. Immunolocalization and expression of small-conductance calcium-activated potassium channels in human myometrium. J Cell Mol Med. 2012;16(12):3001–8.
Shahi PK, Choi S, Zuo DC, Kim MY, Park CG, Kim YD, Lee J, Park KJ, So I, Jun JY. The possible roles of hyperpolarization-activated cyclic nucleotide channels in regulating pacemaker activity in colonic interstitial cells of Cajal. J Gastroenterol. 2013;49(6):1001–10.
Si X, Huang L, Gong Y, Lu J, Lin L. Role of calcium in activation of hyperpolarization-activated cyclic nucleotide-gated channels caused by cholecystokinin octapeptide in interstitial cells of cajal. Digestion. 2012;85(4):266–75.
McCloskey KD. Calcium currents in interstitial cells from the guinea-pig bladder. BJU Int. 2006;97(6):1338–43.
Cretoiu SM, Radu BM, Banciu A, Banciu DD, Cretoiu D, Ceafalan LC, Popescu LM. Isolated human uterine telocytes: immunocytochemistry and electrophysiology of T-type calcium channels. Histochem Cell Biol. 2015;143(1):83–94.
Campeanu RA, Radu BM, Cretoiu SM, Banciu DD, Banciu A, Cretoiu D, Popescu LM. Near-infrared low-level laser stimulation of telocytes from human myometrium. Lasers Med Sci. 2014;29(6):1867–74.
Parsons SP, Kunze WA, Huizinga JD. Maxi-channels recorded in situ from ICC and pericytes associated with the mouse myenteric plexus. Am J Physiol Cell Physiol. 2012;302:C1055–69.
Lerche C, Scherer CR, Seebohm G, Derst C, Wei AD, Busch AE, Steinmeyer K. Molecular cloning and functional expression of KCNQ5, a potassium channel subunit that may contribute to neuronal M-current diversity. J Biol Chem. 2000;275:22395–400.
Schroeder BC, Hechenberger M, Weinreich F, Kubisch C, Jentsch TJ. KCNQ5, a novel potassium channel broadly expressed in brain, mediates M-type currents. J Biol Chem. 2000;275:24089–95.
Bal M, Zhang J, Zaika O, Hernandez CC, Shapiro MS. Homomeric and heteromeric assembly of KCNQ(Kv7) K+ channels assayed by total internal reflection fluorescence/fluorescence resonance energy transfer and patch clamp analysis. J Biol Chem. 2008;283:30668–76.
Hinescu ME, Popescu LM. Interstitial Cajal-like cells (ICLC) in human atrial myocardium. J Cell Mol Med. 2005;9(4):972–5.
Hinescu ME, Gherghiceanu M, Mandache E, Ciontea SM, Popescu LM. Interstitial Cajal-like cells (ICLC) in atrial myocardium: ultrastructural and immunohistochemical characterization. J Cell Mol Med. 2006;10(1):243–57.
Platzer J, Engel J, Schrott-Fischer A, Stephan K, Bova S, Chen H, Zheng H, Striessnig J. Congenital deafness and sinoatrial node dysfunction in mice lacking class D L-type Ca2+ channels. Cell. 2000;102:89–97.
Zhang Z, Xu Y, Song H, Rodriguez J, Tuteja D, Namkung Y, Shin HS, Chiamvimonvat N. Functional roles of Ca(v)1.3 (alpha(1D)) calcium channel in sinoatrial nodes: insight gained using gene-targeted null mutant mice. Circ Res. 2002;90:981–7.
Mangoni ME, Couette B, Bourinet E, Platzer J, Reimer D, Striessnig J, Nargeot J. Functional role of L-type Cav1.3 Ca2+ channels in cardiac pacemaker activity. Proc Natl Acad Sci U S A. 2003;100:5543–8.
Mesirca P, Torrente AG, Mangoni ME. Functional role of voltage gated Ca(2+) channels in heart automaticity. Front Physiol. 2015;6:19.
Popescu LM, Manole CG, Gherghiceanu M, Ardelean A, Nicolescu MI, Hinescu ME, Kostin S. Telocytes in human epicardium. J Cell Mol Med. 2010;14(8):2085–93.
Leiria LO, Mónica FZ, Carvalho FD, Claudino MA, Franco-Penteado CF, Schenka A, Grant AD, De Nucci G, Antunes E. Functional, morphological and molecular characterization of bladder dysfunction in streptozotocin-induced diabetic mice: evidence of a role for L-type voltage-operated Ca2+ channels. Br J Pharmacol. 2011;163(6):1276–88.
Balkanci ZD, Pehlivanoğlu B, Bayrak S, Karabulut I, Karaismailoğlu S, Erdem A. The effect of hypercholesterolemia on carbachol-induced contractions of the detrusor smooth muscle in rats: increased role of L-type Ca2+ channels. Naunyn Schmiedeberg’s Arch Pharmacol. 2012;385(11):1141–8.
Sun YH, Gao X, Tang YJ, Xu CL, Wang LH. Androgens induce increases in intracellular calcium via a G protein-coupled receptor in LNCaP prostate cancer cells. J Androl. 2006;27(5):671–8.
Kim YH, Chung S, Lee YH, Kim EC, Ahn DS. Increase of L-type Ca2+ current by protease-activated receptor 2 activation contributes to augmentation of spontaneous uterine contractility in pregnant rats. Biochem Biophys Res Commun. 2012;418(1):167–72.
Gui P, Chao JT, Wu X, Yang Y, Davis GE, Davis MJ. Coordinated regulation of vascular Ca2+ and K+ channels by integrin signaling. Adv Exp Med Biol. 2010;674:69–79.
Peers C, Scragg JL, Boyle JP, Fearon IM, Taylor SC, Green KN, Webster NJ, Ramsden M, Pearson HA. A central role for ROS in the functional remodelling of L-type Ca2+ channels by hypoxia. Philos Trans R Soc Lond B Biol Sci. 2005;360(1464):2247–54.
Svenningsen P, Andersen K, Thuesen AD, Shin HS, Vanhoutte PM, Skott O, Jensen BL, Hill C, Hansen PB. T-type Ca channels facilitate NO-formation, vasodilatation and NO-mediated modulation of blood pressure. Pflügers Arch. 2014;466:2205–14.
Ball CJ, Wilson DP, Turner SP, Saint DA, Beltrame JF. Heterogeneity of L- and T-channels in the vasculature: rationale for the efficacy of combined L- and T-blockade. Hypertension. 2009;53:654–60.
Thuesen A, Andersen H, Cardel M, Toft A, Walter S, Marcussen Jensen B, Bie P, Hansen P. Differential effect of T-type voltage-gated calcium channel disruption on renal plasma flow and glomerular filtration rate in vivo. Am J Physiol Ren Physiol. 2014;307:F445–52.
Chen CC, Fan YP, Shin HS, Su CK. Basal sympathetic activity generated in neonatal mouse brainstem-spinal cord preparation requires T-type calcium channel subunit 1H. Exp Physiol. 2011;96:486–94.
Hofmann F, Lacinova L, Klugbauer N. Voltage-dependent calcium channels: from structure to function. Rev Physiol Biochem Pharmacol. 1999;139:33–87.
Zhong X, Deng J, He P, You N, Wang Q, Song B, Li L. Reverse mode of the sodium/calcium exchanger subtype 3 in interstitial cells of Cajal from rat bladder. Urology. 2013;82(1):254.e7–12.
Zhu Y, Mucci A, Huizinga JD. Inwardly rectifying chloride channel activity in intestinal pacemaker cells. Am J Physiol Gastrointest Liver Physiol. 2005;288(4):G809–21.
Kim SO, Jeong HS, Jang S, Wu MJ, Park JK, Jiao HY, Jun JY, Park JS. Spontaneous electrical activity of cultured interstitial cells of cajal from mouse urinary bladder. Korean J Physiol Pharmacol. 2013;17(6):531–6.
Wu Y, Shi C, Deng J, Zhang X, Song B, Li L. Expression and function of muscarinic subtype receptors in bladder interstitial cells of cajal in rats. Urol J. 2014;11(3):1642–7.
Ito-Dufros Y, Funakoshi Y, Uehara A, Oishi K. In vitro development of gut-like tissue demonstrating rhythmic contractions from embryonic mouse intestinal cells. Neurogastroenterol Motil. 2007;19(4):288–300.
Kim BJ, Kim HW, Lee GS, Choi S, Jun JY, So I, Kim SJ. Poncirus trifoliate fruit modulates pacemaker activity in interstitial cells of Cajal from the murine small intestine. J Ethnopharmacol. 2013;149(3):668–75.
Kim BJ, Kwon YK, Kim E, So I. Effects of histamine on cultured interstitial cells of cajal in murine small intestine. Korean J Physiol Pharmacol. 2013;17(2):149–56.
Drumm BT, Sergeant GP, Hollywood MA, Thornbury KD, McHale NG, Harvey BJ. The role of cAMP dependent protein kinase in modulating spontaneous intracellular Ca2+ waves in interstitial cells of Cajal from the rabbit urethra. Cell Calcium. 2014;56(3):181–7.
Drumm BT, Large RJ, Hollywood MA, Thornbury KD, Baker SA, Harvey BJ, McHale NG, Sergeant GP. The role of Ca(2+) influx in spontaneous Ca(2+) wave propagation in interstitial cells of Cajal from the rabbit urethra. J Physiol. 2015;593(15):3333–50.
Popescu LM, Ciontea SM, Cretoiu D, Hinescu ME, Radu E, Ionescu N, Ceausu M, Gherghiceanu M, Braga RI, Vasilescu F, Zagrean L, Ardeleanu C. Novel type of interstitial cell (Cajal-like) in human fallopian tube. J Cell Mol Med. 2005;9(2):479–523.
Ciontea SM, Radu E, Regalia T, Ceafalan L, Cretoiu D, Gherghiceanu M, Braga RI, Malincenco M, Zagrean L, Hinescu ME, Popescu LM. C-kit immunopositive interstitial cells (Cajal-type) in human myometrium. J Cell Mol Med. 2005;9(2):407–20.
McCloskey KD. Interstitial cells in the urinary bladder—localisation and function. Neurourol Urodyn. 2010;29:82–7.
Nguyen DT, Dey A, Lang RJ, Ventura S, Exintaris B. Contractility and pacemaker cells in the prostate gland. J Urol. 2011;185:347–51.
Hashitani H, Suzuki H. Identification of interstitial cells of Cajal in corporal tissues of the guinea-pig penis. Br J Pharmacol. 2004;141:199–204.
Drumm BT, Koh SD, Andersson KE, Ward SM. Calcium signalling in Cajal-like interstitial cells of the lower urinary tract. Nat Rev Urol. 2014;11(10):555–64.
Deng J, He P, Zhong X, Wang Q, Li L, Song B. Identification of T‐type calcium channels in the interstitial cells of Cajal in rat bladder. Urology. 2012;80(6):1389.e1–e7.
Allix S, Reyes-Gomez E, Aubin-Houzelstein G, Noël D, Tiret L, Panthier JJ, Bernex F. Uterine contractions depend on KIT-positive interstitial cells in the mouse: genetic and pharmacological evidence. Biol Reprod. 2008;79(3):510–7.
Thomsen L, Robinson TL, Lee JC, Farraway LA, Hughes MJ, Andrews DW, Huizinga JD. Interstitial cells of Cajal generate a rhythmic pacemaker current. Nat Med. 1998;4:848–51.
Smith TK, Reed JB, Sanders KM. Interactions of two electrical pacemakers in muscularis of canine proximal colon. Am J Physiol. 1987;252:C290–9.
Liu LW, Huizinga JD. Electrical coupling of circular muscle to longitudinal muscle and interstitial cells of Cajal in canine colon. J Physiol. 1993;470:445–61.
Rae MG, Fleming N, McGregor DB, Sanders KM, Keef KD. Control of motility patterns in the human colonic circular muscle layer by pacemaker activity. J Physiol. 1998;510(Pt1):309–20.
Pluja L, Alberti E, Fernandez E, Mikkelsen HB, Thuneberg L, Jiminez M. Evidence supporting presence of two pacemakers in rat colon. Am J Physiol Gastrointest Liver Physiol. 2001;281:G255–66.
Yoneda S, Fukui H, Takaki M. Pacemaker activity from submucosal interstitial cells of Cajal drives high-frequency and low-amplitude circular muscle contractions in the mouse proximal colon. Neurogastroenterol Motil. 2004;16:621–7.
Mangoni ME, Traboulsie A, Leoni AL, Couette B, Marger L, Le Quang K, Kupfer E, Cohen-Solal A, Vilar J, Shin HS, Escande D, Charpentier F, Nargeot J, Lory P. Bradycardia and slowing of the atrioventricular conduction in mice lacking CaV3.1/alpha1G T-type calcium channels. Circ Res. 2006;98(11):1422–30.
Marger L, Mesirca P, Alig J, Torrente A, Dubel S, Engeland B, Kanani S, Fontanaud P, Striessnig J, Shin HS, Isbrandt D, Ehmke H, Nargeot J, Mangoni ME. Functional roles of Ca(v)1.3, Ca(v)3.1 and HCN channels in automaticity of mouse atrioventricular cells: insights into the atrioventricular pacemaker mechanism. Channels (Austin). 2011;5:251–61.
Popescu LM, Gherghiceanu M, Manole CG, Faussone-Pellegrini MS. Cardiac renewing: interstitial Cajal-like cells nurse cardiomyocyte progenitors in epicardial stem cell niches. J Cell Mol Med. 2009;13(5):866–86.
Kostin S, Popescu LM. A distinct type of cell in myocardium: interstitial Cajal-like cells (ICLCs). J Cell Mol Med. 2009;13(2):295–308.
Torrente AG, Zhang R, Zaini A, Giani JF, Kang J, Lamp ST, Philipson KD, Goldhaber JI. Burst pacemaker activity of the sinoatrial node in sodium-calcium exchanger knockout mice. Proc Natl Acad Sci U S A. 2015;112(31):9769–74.
Yamamura H, Cole WC, Kita S, Hotta S, Murata H, Suzuki Y, Ohya S, Iwamoto T, Imaizumi Y. Overactive bladder mediated by accelerated Ca2+ influx mode of Na+/Ca2+ exchanger in smooth muscle. Am J Physiol Cell Physiol. 2013;305(3):C299–308.
Iurlo A, Orsi E, Cattaneo D, Resi V, Bucelli C, Orofino N, Sciumè M, Elena C, Grancini V, Consonni D, Orlandi EM, Cortelezzi A. Effects of first- and second-generation tyrosine kinase inhibitor therapy on glucose and lipid metabolism in chronic myeloid leukemia patients: a real clinical problem? Oncotarget. 2015;6(32):33944–51.
Lam M, Dey A, Lang RJ, Exintaris B. Effects of imatinib mesylate on the spontaneous activity generated by the guinea-pig prostate. BJU Int. 2013;112(4):E398–405.
Cretoiu SM, Simionescu AA, Caravia L, Curici A, Cretoiu D, Popescu LM. Complex effects of imatinib on spontaneous and oxytocin-induced contractions in human non-pregnant myometrium. Acta Physiol Hung. 2011;98(3):329–38.
Wu X, Morgan KG, Jones CJ, Tribe RM, Taggart MJ. Myometrial mechanoadaptation during pregnancy: implications for smooth muscle plasticity and remodelling. J Cell Mol Med. 2008;12(4):1360–73.
Jansson T, Powell TL, Illsley NP. Gestational development of water and non-electrolyte permeability of human syncytiotrophoblast plasma membranes. Placenta. 1999;20(2–3):155–60.
Whiting KP, Restall CJ, Brain PF. Steroid hormone-induced effects on membrane fluidity and their potential roles in non-genomic mechanisms. Life Sci. 2000;67(7):743–57.
Manole CG, Gherghiceanu M, Simionescu O. Telocyte dynamics in psoriasis. J Cell Mol Med. 2015;19(7):1504–19.
Manole CG, Cismaşiu V, Gherghiceanu M, Popescu LM. Experimental acute myocardial infarction: telocytes involvement in neo-angiogenesis. J Cell Mol Med. 2011;15(11):2284–96.
Alunno A, Ibba-Manneschi L, Bistoni O, Rosa I, Caterbi S, Gerli R, Manetti M. Telocytes in minor salivary glands of primary Sjögren’s syndrome: association with the extent of inflammation and ectopic lymphoid neogenesis. J Cell Mol Med. 2015;19(7):1689–96.
Bosco C, Díaz E, Gutiérrez R, González J, Parra-Cordero M, Rodrigo R, Barja P. A putative role for telocytes in placental barrier impairment during preeclampsia. Med Hypotheses. 2015;84(1):72–7.
Manetti M, Rosa I, Messerini L, Ibba-Manneschi L. Telocytes are reduced during fibrotic remodelling of the colonic wall in ulcerative colitis. J Cell Mol Med. 2015;19(1):62–73.
Acknowledgments
We are grateful for the financial support received through the program Partnerships in priority areas – PN II, UEFISCDI, Project No. 82/2012. B M Radu has a PhD fellowship from the Italian Ministry of Research (MIUR). DD Banciu is financed by the Sectoral Operational Programme Human Resources Development (SOPHRD), the European Social Fund, and the Romanian Government under the contract number POSDRU/159/1.5/S/141531.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Banciu, D.D., Banciu, A., Radu, B.M. (2016). Electrophysiological Features of Telocytes. In: Wang, X., Cretoiu, D. (eds) Telocytes. Advances in Experimental Medicine and Biology, vol 913. Springer, Singapore. https://doi.org/10.1007/978-981-10-1061-3_19
Download citation
DOI: https://doi.org/10.1007/978-981-10-1061-3_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-1060-6
Online ISBN: 978-981-10-1061-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)