Abstract
To investigate a possible relation between hypercholesterolemia and detrusor smooth muscle function, we studied the contractile response to potassium challenge, carbachol (CCh), and the components of CCh-induced contractile mechanism in high-cholesterol diet-fed rats. Adult male Sprague–Dawley rats were fed with standard (control group, N = 17) or 4 % cholesterol diet (hypercholesterolemia group (HC), N = 16) for 4 weeks. Spontaneous contractions of detrusor muscle strips and their responses to potassium chloride (KCl) or cumulative dose–contraction curves to CCh were recorded. The effects of muscarinic receptor antagonists (methoctramin and/or 4-diphenylacetoxy-N-methylpiperidine), L-type Ca+2 channel blocker (nifedipine), and/or rho-kinase inhibitor Y-27632 were investigated. Blood cholesterol level was increased in the HC group with no sign of atherosclerosis. The KCl-induced detrusor smooth muscle contractions were higher in HC, whereas spontaneous and CCh-induced responses were similar in both groups. Preincubation with receptor antagonist for M3 but not for M2 attenuated contraction significantly, shifting the dose–response curve to the right. This response was similar in both groups. Among two effector mechanisms of M3-mediated detrusor smooth muscle contraction, rho-kinase pathway was not affected by hypercholesterolemia, whereas blockade of L-type Ca+2 channels potently reduced contractions. The results of this study point out a relation between hypercholesterolemia and contractile mechanism of detrusor smooth muscle likely to change urinary bladder function, via altering L-type Ca+2 channels. Taken together with escalating incidence of hypercholesterolemia and lower urinary tract symptoms, it is a field which deserves to be investigated further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypercholesterolemia, characterized by elevated plasma levels of low-density lipoproteins (LDL) and cholesterol, plays an important role in several pathological conditions such as atherosclerosis and related cardiovascular disorders (CV) (Mombouli and Vanhoutte 1999). Whereas the importance of hypercholesterolemia in CV diseases has been well documented, to what extent hypercholesterolemia is involved in non-CV pathologies independent of its vascular actions is yet unknown. The young elderly and elderly populations frequently experience lower urinary tract symptoms (LUTS) related to storage, voiding, and post-micturition functions (Mevcha et al. 2010; Smith 2010; Fowke et al. 2011). In these age groups, the incidence of hypercholesterolemia is also high (Hall et al. 2011; Devroey et al. 2011). However, the association between hyperlipidemic conditions and the risk of LUTS is still controversial (Litman et al. 2007; Parsons 2010; Fowke et al. 2011). Previously, decreased plasma high-density lipoprotein (HDL) levels have been linked to urinary storage symptoms (Martin et al. 2011). Moreover, hyperlipidemia has been shown to associate with increased urinary frequency (Huang et al. 2010) and bladder overactivity in rats (Rahman et al. 2007) and contributes to bladder dysfunction in rabbits (Yoshida et al. 2010); LUTS associated with hypercholesterolemia was reported in different species (Azadzoi et al. 1999; Hall et al. 2011; Nomiya et al. 2012).
Detrusor smooth muscle has phasic intrinsic activity exhibited with spontaneous contractions (Kanai et al. 2007). They also respond to potassium challenge, a nonspecific depolarizing agent. Both spontaneous (Hashitani and Brading 2003) and potassium-induced contractions involve calcium influx via L-type calcium (Ca2+) channels (Wegener et al. 2004).
Detrusor smooth muscle contraction is principally mediated by parasympathetic cholinergic stimulation via muscarinic M2 and M3 receptors in various animal species (Andersson 2004; Hegde 2006). Although the M2 subtype outnumbers the M3 subtype, detrusor contraction is predominantly M3 receptor mediated. Main pathways for M3 receptor-mediated contraction in detrusor are Ca2+ influx via sarcolemmal L-type Ca2+ channels and activation of intracellular rho-kinase pathway (Abrams and Andersson 2007). Atropine-resistant, tetrodotoxin-sensitive purinergic contraction also contributes to urinary bladder contraction in small proportions in humans and rats (Son et al. 2007). In some pathological conditions, both alterations in the expression levels of receptors and differences in the contribution of physiological contractile pathways have been observed (Andersson and Wein 2004; Giglio et al. 2007; Smith 2010). To the best of our knowledge, until recently, the effect of hypercholesterolemia on detrusor contractility has been investigated in a limited number of studies. Therefore, we sought to characterize the contractile responses of the urinary bladder in hypercholesterolemic rats. To this end, we obtained contractile response in detrusor strips by using potassium chloride (KCl) and contractile agonist, carbachol (CCh). We further investigated the alterations in the contraction mechanisms by employing muscarinic receptor antagonists methoctramine (selective M2 receptor blocker) or 4-diphenylacetoxy-N-methylpiperidine (4-DAMP; selective M1/M3/M4/M5 receptor blocker) and NG-nitro-l-arginine methyl ester (l-NAME; nonselective nitric oxide synthase blocker), nifedipine (Ca2+ channel blocker), and Y-27632 (rho-kinase inhibitor).
Materials and methods
Animals
All animal experiments were conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals, and the experimental protocol was approved by the Hacettepe University Institutional Ethics Committee for the Care and Use of Experimental Animals. Four- to 7-week-old male Sprague–Dawley rats were allocated into control (N = 17) and hypercholesterolemia (N = 16) groups. Whereas control group (NC) was on standard rat chow, hypercholesterolemia group (HC) was fed with high-cholesterol diet (4 % cholesterol and 0.2 % deoxycholate) for 4 weeks. The animals were housed under standard conditions at 21 ± 2 °C and 30–70 % relative humidity with 12 h dark/12 h light illumination (lights were on between 07:00 and 19:00 hours) with free access to food and water. At the end of 4 weeks, rats were placed in metabolic cages for 24 h to determine food and water consumption, urine output, and body weight.
At the day of killing, abdomen was opened through a midline incision and urinary bladder was excised under ether anesthesia. Blood samples were collected by cardiac puncture for characterization of the serum lipid profile. Since initial signs of atherosclerosis are observed in aorta (Stary et al. 1994), the arch of aorta was dissected, excised, and fixed in 10 % formalin for histopathological evaluation. In the ice-cold oxygenated Krebs–Henseleit solution (118.4 mM NaCl, 4.7 mM KCl, 1.2 mM KH2PO4, 1.2 mM MgSO4, 25.0 mM NaHCO3, 2.5 mM CaCl2, and 12.2 mM glucose; pH 7.35–7.40), urinary bladder was cleared of all surrounding adipose and connective tissues, opened up with a longitudinal incision, and four longitudinal strips (10 × 2 mm) from the bladder body of each rat were prepared. Bladder strips were mounted in 15 ml organ baths containing Krebs–Henseleit solution gassed with a mixture of 95 % O2 and 5 % CO2 and kept at 37 °C. Each strip was connected to a tension transducer (MAY FDT 05, Commat, Ankara, Turkey) under a resting tension of 0.5 g. Before any experimental procedure, detrusor strips were allowed to equilibrate for at least 60 min by refreshing Krebs–Henseleit solution every 15 min until the spontaneous contractions became stable. Mechanical activity was collected real time by data acquisition/analysis system (BIOPAC MP30, Biopac Systems Inc., CA). One strip in each series was allocated as time control, and contraction experiments were carried out in the rest of the three strips as described below. At the end of the contraction protocols, strips were weighed.
Contraction protocols
Following equilibration, the strips were challenged with 80 mM KCl. As the tension returned to baseline, the detrusor strips were allowed to rest and equilibrate for 60 min.
Contractile responses of the detrusor strips to CCh were investigated in a separate series of experiments. CCh response was further studied in the presence of methoctramine (selective M2 receptor blocker), 4-DAMP (selective M1/M3/M4/M5 receptor blocker), nifedipine (Ca2+ channel blocker), and/or Y-27632 (rho-kinase inhibitor).
In the first series of experiments, cumulative dose–response curve to increasing concentrations of CCh (10−8–10−4 M) was obtained. Strips were then washed out and cumulative dose–response curve to CCh was re-obtained in the second series of experiments, after pretreatment with methoctramine (10−5 M), 4-DAMP (10−7 M), or methoctramine (10−5 M) + 4-DAMP (10−7 M). To examine solely the M3 receptor-mediated contractile function, cumulative dose–response curves to CCh were repeated in the presence of methoctramine (10−5 M) and l-NAME (10−4 M). Furthermore, in the last series, the same curve was also obtained following incubation with nifedipine (10−6 M), Y-27632 (10−5 M), or nifedipine (10−6 M) + Y-27632 (10−5 M) in the presence of methoctramine (10−5 M) and l-NAME (10−4 M). Each protocol was followed by three complete washouts with Krebs–Henseleit solution in each organ bath, and the strips were allowed to equilibrate at least 60 min between protocols.
Serum lipid profile
Serum lipid profile (total cholesterol, triglyceride, HDL, LDL, and very-low-density lipoprotein (VLDL)) was determined by diagnostic kits using modular system autoanalyzer (Roche/Hitachi, IN) at the Clinical Biochemistry Laboratory of Hacettepe University Hospital.
Histopathological evaluation
Arch of aorta was fixed in 10 % formaldehyde and processed by routine light microscopy tissue processing techniques. Sections were stained with hematoxylin–eosin and evaluated for atherosclerotic changes, as described previously (Cai et al. 2005).
Chemicals
All chemicals were purchased from Sigma-Aldrich (Sigma-Aldrich, St. Louis, MO). With the exception of nifedipine which was dissolved in dimethyl sulfoxide, distilled water was used to suspend and dilute the compounds.
Calculations and statistical analysis
Data were analyzed by BSL Pro Version 3.6.7 software (Biopac Systems Inc., Santa Barbara, CA). Contraction data were normalized to wet tissue weight (g/100 mg wet tissue weight). The number of animals and strips were indicated by N and n, respectively. Data were expressed as mean ± SEM. SPSS 15.0 for Windows (SPSS Inc., Chicago, IL) software was used for statistical analysis. Differences were considered significant at P < 0.05.
The general metabolic profile, body and urinary bladder weights, serum cholesterol levels, and spontaneous and KCl-induced contractions were compared by Student's t test for independent samples. Intra- and intergroup comparisons of cumulative dose–response curves were compared by repeated measures analysis of variance followed by Tukey's post hoc test for multiple comparisons.
Maximal contraction response to CCh (E max) and negative logarithm of molar concentration that causes 50 % of maximum contraction (pD2) values were calculated by using SigmaPlot 9.01 for Windows (Systat Software, Inc., San Jose, CA) software and compared by Student's t test for independent samples.
Results
Animal characteristics and effects of high-cholesterol diet
Body weights, bladder weights, food and water consumptions, and urine outputs were similar in NC and HC rats (Table 1). In the HC group, total serum cholesterol and LDL levels were higher compared with controls (P < 0.05). Triglyceride, HDL, and VLDL levels were similar in both groups. Histological evaluation of aortic arch revealed no sign of atherosclerosis.
Contraction response of bladder strips
The amplitudes and frequencies of basal spontaneous contractions were similar in the HC (n = 16; 2.62 ± 0.22 g/100 mg wet tissue weight; 0.067 ± 0.003 Hz) and the NC groups (n = 17; 2.48 ± 0.21 g/100 mg wet tissue weight; 0.063 ± 0.002 Hz). Maximal contractile response to 80 mM KCl was higher in the HC group (n = 10; 30.8 ± 1.7 g/100 mg wet tissue weight) compared with the NC group (n = 12; 24.7 ± 1.9 g/100 mg wet tissue weight; P < 0.05). The amplitudes and frequencies of basal spontaneous contractions were similar in both groups before and after KCl stimulation.
The cumulative dose–contraction curves to CCh (10−8–10−4 M) were also similar in both groups and abolished completely by atropine (10−5 M) pretreatment (data not shown). E max of dose–response curves and pD2 values obtained from bladder strips in NC and HC groups were similar (Table 2).
Effect of muscarinic receptor blockers on CCh-induced contractions
Muscarinic receptor blockers (methoctramine and 4-DAMP) shifted the cumulative dose–contraction curves to CCh to the right in both groups (P < 0.05; Fig. 1a, b). E max and pD2 values are presented in Table 2. Although maximal response to CCh was not altered in the presence of methochtramine, it was significantly lower in the presence of 4-DAMP or methochtramine + 4-DAMP both in the NC and HC groups (P < 0.05). Comparison of the HC and NC groups revealed no significant difference in terms of the effects of M2 and/or M3 receptor blockers. CCh dose–response curves obtained in the presence of methoctramine and l-NAME revealed similar E max and pD2 values when compared with control and methoctramine curves both in the NC and HC groups (data not shown).
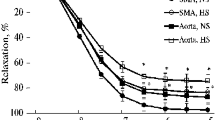
Effect of nifedipine and Y-27632 on CCh-induced contractions
The comparison of the dose–response curves between the NC and HC groups exhibited a difference only for nifedipine-treated strips in the presence of metoctramine and l-NAME (P < 0.05). E max values were significantly lower in the nifedipine-treated strips both in the NC and HC groups. The E max values for nifedipine-impaired contractions in the HC group were lower than the NC group (P < 0.05; Table 3). Pretreatment of bladder strips with nifedipine resulted in 34 % inhibition in the NC group and 76 % inhibition in the HC group. The effect of Y-27632 alone or in combination with nifedipine was similar in both groups. The cumulative dose–contraction curves of CCh shifted to the right in both groups following preincubation with Y-27632 or nifedipine + Y-27632 in the presence of methoctramine and l-NAME (P < 0.05; Fig. 2a, b). E max and pD2 values are presented in Table 3.
Dose–response curves for the effects of CCh in the presence of Met (10−5 M) + l-NAME (10−4 M), Met (10−5 M) + l-NAME (10−4 M) + Nif (10−6 M), Met (10−5 M) + l-NAME (10−4 M) + Y-27632 (10−5 M), or Met (10−5 M) + l-NAME (10−4 M) + Nif (10−6 M) + Y-27632 (10−5 M) in control (a) and hypercholesterolemia (b) groups. Data are presented as mean ± SEM. Met methoctramine, Nif nifedipine
Discussion
This study shows that a sustained increase in plasma cholesterol (1) leads to augmented contractile responses in the isolated rat urinary bladder strips to 80 mM KCl whereas spontaneous and CCh-induced contractions are unaltered, (2) has no effect on the M3 muscarinic receptor-mediated contractions, and (3) associates with prominent depressing effect of L-type Ca+2channel blockage on CCh-induced contractions of detrusor strips. The protocol applied in this study created hypercholesterolemia and high LDL levels. The duration, 4 weeks long, of high-cholesterol diet is sufficient both to achieve a stable high plasma cholesterol (Getz and Reardon 2006) and also to observe changes in tissues (Fotis et al. 2012). Hypercholesterolemia is related to the regulation of functions of the ion channels (Levitan et al. 2010). Nifedipine-sensitive L-type Ca+2 channels which are involved in spontaneous, KCl-induced (Wegener et al. 2004) and M3-mediated (Christ and Andersson 2007) contractions are good examples for this modulation (Cox and Tulenko 1995).
Spontaneous contractions often develop upon action potential discharges which result in Ca2+ influx through L-type Ca2+channels (Hashitani and Brading 2003). Spontaneous activity is lower in amplitude and disorganized and does not lead to micturition contractions in healthy adult animals. But it was shown to become significantly higher in amplitude and organized leading to micturition in various pathological conditions such as spinal cord-transected animals (Fry et al. 2012) and overactive bladder due to cystitis (Pan et al. 2012). A stronger spontaneous bladder activity was reported in an earlier study in which a relation between the hypercholesterolemia and the detrusor function was investigated (Son et al. 2007). It was slightly but not significantly higher in HC animals in our study similar to the results of Azadzoi et al. (1999).
Potassium, a nonspecific depolarizing agent, opens L-type Ca+2 channels leading to contraction (Wibberley et al. 2003; Wegener et al. 2004). Hyperlipidemia leads to increased smooth muscle reactivity and sensitivity to KCl in uterine artery in women (Fleischhacker et al. 2000) and strengthens KCl-induced contractions in coronary arteries of pigs (Thompson et al. 2004). We also found significantly higher KCl-induced contractions in detrusor strips in the HC group. However, previous reports suggest no change in KCl-induced contractions of urinary bladder in correlation with plasma cholesterol (Shenfeld et al. 2005; Son et al. 2007; Yoshida et al. 2010). Moreover, these studies are not comparable with the present one since these abovementioned studies were conducted under ischemic conditions caused by atherosclerosis. On the other hand, our treatment resulted in hypercholesterolemia but no atherosclerotic changes in the vessels. A previous study pointed out unaltered blood flow in empty bladder whereas only short-lived ischemia during bladder contraction in the HC animals (Azadzoi et al. 1999). Since one of the limitations of our study includes not being able to measure the blood flow, the ischemic changes could not be ruled out while explaining our results.
Taking the above findings together, we come to a conclusion that hyperlipidemia may modulate contractile function of detrusor muscles. To expand our research and find out the main components of contraction that may be affected by hyperlipidemia, we investigated the cholinergic component, main contractile pathway of the detrusor muscle contraction. We obtained cumulative dose–response curves to CCh which revealed no difference between the NC and HC groups. M2 and M3 muscarinic receptors are prominent in the rat detrusor muscle, and M2 receptor density is about twofold higher than M3 (Hegde 2006). However, in physiological conditions, the main contraction pathway is operated through M3 receptors, and M2 receptors serve mainly a supportive role (Abrams et al. 2006; Abrams and Andersson 2007; Pak et al. 2010). Our data suggest that 4-week long hypercholesterolemic diet-induced hyperlipidemia does not change relative contributions of muscarinic receptor subtypes, although we are aware of the previous studies reporting changes in the expression levels of the muscarinic receptor subtypes (Abrams and Andersson 2007) mediating urinary bladder contractions in various pathological conditions such as diabetic bladder (Leiria et al. 2011), neurogenic bladder (Pontari et al. 2004), or cystitis (Giglio et al. 2007). On the other hand, Stevens et al. showed increased sensitivity to CCh whereas no change in receptor subtypes contribution to contraction in the neurogenic or idiopathic overactive bladder (Stevens et al. 2007), and Nobe et al. reported attenuated detrusor contractions in spontaneously hypertensive hyperlipidemic rats without involvement of muscarinic receptor alterations (Nobe et al. 2009). To the best of our knowledge, this study is the first one investigating receptor subtype distribution in diet-induced hypercholesterolemic rats and should be supported by further studies especially employing receptor subtype knockout animal models.
Since the contribution of M2 and M3 receptors was similar in the NC and HC groups in our study, we further investigated the intracellular pathways of physiological M3-mediated detrusor contraction which is operated by increased cytoplasmic calcium concentration, through sarcolemmal L-type Ca2+ channels and rho-kinase activation (Wibberley et al. 2003; Abrams and Andersson 2007; Wuest et al. 2007) (Christ and Hodges 2006; Hegde 2006). In this study, the intracellular pathways were studied in the presence of both M2 receptor blocker and nitric oxide synthase inhibitor to be able to solely investigate the M3-mediated contractile response. The role of rho-kinase pathway in CCh-induced contractile responses in bladder smooth muscle in hyperlipidemic rats was investigated for the first time in the current study. Preincubation of detrusor strips with the rho-kinase inhibitor Y-27632 did not significantly affect the CCh-induced contractions either in the HC or NC groups, and this was comparable between groups. But, the only study to our knowledge relating rho-kinase pathway with hyperlipidemia is conducted in spontaneously hypertensive hyperlipidemic rats (Nobe et al. 2009) which points out a role for the inactivation of the rho-kinase pathway.
L-type Ca2+ channels are essential for normal bladder function (Wegener et al. 2004). Different species exhibit differences in sensitivity to the blockade of the L-type Ca2+ channels in response to CCh stimulation of urinary bladder (Wuest et al. 2007). This effect is very prominent in rats (Schneider et al. 2004). In line with these, L-type Ca2+ channel blockade potently attenuated maximum response in both groups in the present study. These channels contributed to CCh-induced contractions to a greater extent in hypercholesterolemic rats. Previously, it was reported that high-fat diet associates with increased ratio of L-type Ca2+ channels in the vascular smooth muscles of hypertensive rats (Wilde et al. 2000). Similarly augmented L-type Ca2+ current in myocytes from rabbit portal vein under dietary hypercholesterolemia was shown (Cox and Tulenko 1995). Moreover, Leira et al. showed higher expression of L-type Ca2+ mRNA in the bladders of diabetic mice (Leiria et al. 2011). Although some of the reported data are contradictory (Jennings et al. 1999) to the abovementioned studies and to the results of the current study, the contractile response of smooth muscle involving L-type Ca+2 channels is certainly altered in various pathological conditions. This study is the first experiment studying the effect of diet-induced hypercholesterolemia on L-type Ca2+ channels in detrusor smooth muscles.
In conclusion, significant differences observed both in KCI-induced contractions and attenuation of CCh-induced contractions by nifedipine in this study suggest an increased role of L-type Ca2+ channels in bladder contraction in diet-induced hypercholesterolemic rats. As the incidence of hypercholesterolemia and related comorbidities are increasing, the studies subjecting functional outcomes of hypercholesterolemia for the urinary bladder functions should be studied further.
References
Abrams P, Andersson KE (2007) Muscarinic receptor antagonists for overactive bladder. BJU Int 100:987–1006
Abrams P, Andersson KE, Buccafusco JJ, Chapple C, de Groat WC, Fryer AD, Kay G, Laties A, Nathanson NM, Pasricha PJ, Wein AJ (2006) Muscarinic receptors: their distribution and function in body systems, and the implications for treating overactive bladder. Br J Pharmacol 148:565–578
Andersson KE (2004) Detrusor contraction—focus on muscarinic receptors. Scand J Urol Nephrol Suppl 215:54–57
Andersson KE, Wein AJ (2004) Pharmacology of the lower urinary tract: basis for current and future treatments of urinary incontinence. Pharmacol Rev 56:581–631
Azadzoi KM, Tarcan T, Kozlowski R, Krane RJ, Siroky MB (1999) Overactivity and structural changes in the chronically ischemic bladder. J Urol 162:1768–1778
Cai GJ, Miao CY, Xie HH, Lu LH, Su DF (2005) Arterial baroreflex dysfunction promotes atherosclerosis in rats. Atherosclerosis 183:41–47
Christ GJ, Andersson KE (2007) Rho-kinase and effects of rho-kinase inhibition on the lower urinary tract. Neurourol Urodyn 26:948–954
Christ GJ, Hodges S (2006) Molecular mechanisms of detrusor and corporal myocyte contraction: identifying targets for pharmacotherapy of bladder and erectile dysfunction. Br J Pharmacol 147(Suppl 2):S41–S55
Cox RH, Tulenko TN (1995) Altered contractile and ion channel function in rabbit portal vein with dietary atherosclerosis. Am J Physiol 268:H2522–H2530
Devroey D, Senesael E, Moerenhout T, Van De Vijver E, Vandevoorde J (2011) Follow-up of a cardiovascular prevention campaign. Cent Eur J Public Health 19(4):190–196
Fleischhacker E, Esenabhalu VE, Holzmann S, Skrabal F, Koidl B, Kostner GM, Graier WF (2000) In human hypercholesterolemia increased reactivity of vascular smooth muscle cells is due to altered subcellular Ca(2+) distribution. Atherosclerosis 149:33–42
Fotis L, Agrogiannis G, Vlachos IS, Pantopoulou A, Margoni A, Kostaki M, Verikokos C, Tzivras D, Mikhailidis DP, Perrea D (2012) Intercellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1 at the early stages of atherosclerosis in a rat model. In Vivo 26:243–250
Fowke JH, Munro H, Signorello LB, Blot WJ, Penson DF (2011) Association between socioeconomic status (SES) and lower urinary tract symptom (LUTS) severity among black and white men. J Gen Intern Med 26:1305–1310
Fry CH, Young JS, Jabr RI, McCarthy C, Ikeda Y, Kanai AJ (2012) Modulation of spontaneous activity in the overactive bladder—the role of P2Y agonists. Am J Physiol Renal Physiol 302:F1447–F1454
Getz GS, Reardon CA (2006) Diet and murine atherosclerosis. Arterioscler Thromb Vasc Biol 26:242–249
Giglio D, Aronsson P, Eriksson L, Tobin G (2007) In vitro characterization of parasympathetic and sympathetic responses in cyclophosphamide-induced cystitis in the rat. Basic Clin Pharmacol Toxicol 100:96–108
Hall SA, Chiu GR, Link CL, Steers WD, Kupelian V, McKinlay JB (2011) Are statin medications associated with lower urinary tract symptoms in men and women? Results from the Boston Area Community Health (BACH) Survey. Ann Epidemiol 21:149–155
Hashitani H, Brading AF (2003) Ionic basis for the regulation of spontaneous excitation in detrusor smooth muscle cells of the guinea-pig urinary bladder. Br J Pharmacol 140:159–169
Hegde SS (2006) Muscarinic receptors in the bladder: from basic research to therapeutics. Br J Pharmacol 147(Suppl 2):S80–S87
Huang YC, Shindel AW, Ning H, Lin G, Harraz AM, Wang G, Garcia M, Lue TF, Lin CS (2010) Adipose derived stem cells ameliorate hyperlipidemia associated detrusor overactivity in a rat model. J Urol 183:1232–1240
Jennings LJ, Xu QW, Firth TA, Nelson MT, Mawe GM (1999) Cholesterol inhibits spontaneous action potentials and calcium currents in guinea pig gallbladder smooth muscle. Am J Physiol 277:G1017–G1026
Kanai A, Roppolo J, Ikeda Y, Zabbarova I, Tai C, Birder L, Griffiths D, de Groat W, Fry C (2007) Origin of spontaneous activity in neonatal and adult rat bladders and its enhancement by stretch and muscarinic agonists. Am J Physiol Ren Physiol 292(3):F1065–F1072
Leiria LO, Monica FZ, Carvalho FD, Claudino MA, Franco-Penteado CF, Schenka A, Grant AD, De Nucci G, Antunes E (2011) Functional, morphological and molecular characterization of bladder dysfunction in streptozotocin-induced diabetic mice: evidence of a role for L-type voltage-operated Ca2+ channels. Br J Pharmacol 163:1276–1288
Levitan I, Fang Y, Rosenhouse-Dantsker A, Romanenko V (2010) Cholesterol and ion channels. Subcell Biochem 51:509–549
Litman HJ, Steers WD, Wei JT, Kupelian V, Link CL, McKinlay JB (2007) Relationship of lifestyle and clinical factors to lower urinary tract symptoms: results from Boston Area Community Health survey. Urology 70:916–921
Martin SA, Haren MT, Marshall VR, Lange K, Wittert GA (2011) Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol 29:179–184
Mevcha A, Gulur DM, Gillatt D (2010) Diagnosing urological disorders in ageing men. Practitioner 254:25–26, 28-29, 22-23
Mombouli JV, Vanhoutte PM (1999) Endothelial dysfunction: from physiology to therapy. J Mol Cell Cardiol 31:61–74
Nobe K, Yamazaki T, Tsumita N, Hashimoto T, Honda K (2009) Glucose-dependent enhancement of diabetic bladder contraction is associated with a rho kinase-regulated protein kinase C pathway. J Pharmacol Exp Ther 328:940–950
Nomiya M, Yamaguchi O, Andersson KE, Sagawa K, Aikawa K, Shishido K, Yanagida T, Kushida N, Yazaki J, Takahashi N (2012) The effect of atherosclerosis-induced chronic bladder ischemia on bladder function in the rat. Neurourol Urodyn 31:195–200
Pak KJ, Ostrom RS, Matsui M, Ehlert FJ (2010) Impaired M3 and enhanced M2 muscarinic receptor contractile function in a streptozotocin model of mouse diabetic urinary bladder. Pharmacology Naunyn Schmiedeberg's Arch Pharmacol 381(5):441–454
Pan F, Liu D, Han XM, Li WC, Pang ZL, Li B, Zhang XP, Xiao YJ, Zeng FQ (2012) Urodynamic investigation of cyclophosphamide-induced overactive bladder in conscious rats. Chin Med J (Engl) 125:321–325
Parsons JK (2010) Benign prostatic hyperplasia and male lower urinary tract symptoms: epidemiology and risk factors. Curr Bladder Dysfunct Rep 5:212–218
Pontari MA, Braverman AS, Ruggieri MR Sr (2004) The M2 muscarinic receptor mediates in vitro bladder contractions from patients with neurogenic bladder dysfunction. Am J Physiol Regul Integr Comp Physiol 286:R874–R880
Rahman NU, Phonsombat S, Bochinski D, Carrion RE, Nunes L, Lue TF (2007) An animal model to study lower urinary tract symptoms and erectile dysfunction: the hyperlipidaemic rat. BJU Int 100:658–663
Schneider T, Hein P, Michel MC (2004) Signal transduction underlying carbachol-induced contraction of rat urinary bladder. I. Phospholipases and Ca2+ sources. J Pharmacol Exp Ther 308:47–53
Shenfeld OZ, Meir KS, Yutkin V, Gofrit ON, Landau EH, Pode D (2005) Do atherosclerosis and chronic bladder ischemia really play a role in detrusor dysfunction of old age? Urology 65:181–184
Smith PP (2010) Aging and the underactive detrusor: a failure of activity or activation? Neurourol Urodyn 29:408–412
Son H, Lee SL, Park WH, Park K, Park S, Kang MS, Kim DY, Kim SW, Paick JS (2007) New unstable bladder model in hypercholesterolemia rats. Urology 69:186–190
Stary HC, Chandler AB, Glagov S, Guyton JR, Insull W Jr, Rosenfeld ME, Schaffer SA, Schwartz CJ, Wagner WD, Wissler RW (1994) A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 89:2462–2478
Stevens LA, Chapple CR, Chess-Williams R (2007) Human idiopathic and neurogenic overactive bladders and the role of M2 muscarinic receptors in contraction. Eur Urol 52:531–538
Thompson MA, Henderson KK, Woodman CR, Turk JR, Rush JW, Price E, Laughlin MH (2004) Exercise preserves endothelium-dependent relaxation in coronary arteries of hypercholesterolemic male pigs. J Appl Physiol 96:1114–1126
Wegener JW, Schulla V, Lee TS, Koller A, Feil S, Feil R, Kleppisch T, Klugbauer N, Moosmang S, Welling A, Hofmann F (2004) An essential role of Cav1.2 L-type calcium channel for urinary bladder function. FASEB J 18:1159–1161
Wibberley A, Chen Z, Hu E, Hieble JP, Westfall TD (2003) Expression and functional role of rho-kinase in rat urinary bladder smooth muscle. Br J Pharmacol 138:757–766
Wilde DW, Massey KD, Walker GK, Vollmer A, Grekin RJ (2000) High-fat diet elevates blood pressure and cerebrovascular muscle Ca(2+) current. Hypertension 35:832–837
Wuest M, Hiller N, Braeter M, Hakenberg OW, Wirth MP, Ravens U (2007) Contribution of Ca2+ influx to carbachol-induced detrusor contraction is different in human urinary bladder compared to pig and mouse. Eur J Pharmacol 565:180–189
Yoshida M, Masunaga K, Nagata T, Satoji Y, Shiomi M (2010) The effects of chronic hyperlipidemia on bladder function in myocardial infarction-prone Watanabe heritable hyperlipidemic (WHHLMI) rabbits. Neurourol Urodyn 29:1350–1354
Acknowledgments
This study was supported by the Hacettepe University Research Foundation (HUBAB; 01-G-019 and 07-D09-101-03) and The Scientific and Technological Research Council of Turkey (TUBITAK: 106-S-244). The authors would like to thank Gülsen Öner, Ph.D., Professor of Physiology for her critical and initiative contribution in this study and Rıfkı Finci, MD, Professor of Pathology for histopathological evaluation of aortic arch.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balkanci, Z.D., Pehlivanoğlu, B., Bayrak, S. et al. The effect of hypercholesterolemia on carbachol-induced contractions of the detrusor smooth muscle in rats: increased role of L-type Ca2+ channels. Naunyn-Schmiedeberg's Arch Pharmacol 385, 1141–1148 (2012). https://doi.org/10.1007/s00210-012-0784-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-012-0784-5