Abstract
Knowledge about meniscal root tears and their consequences is rapidly evolving among sports medicine surgeons. Probably unrecognized for decades, the natural evolution of medial meniscal posterior root tears can resemble an imaging pattern of an avascular necrosis of the knee and therefore mistakenly were named “spontaneous osteonecrosis of the knee.” Lateral meniscal root tears commonly occur acutely with a concurrent anterior cruciate ligament tears. Conversely, medial root tears are generally more chronic and can be caused by preexisting knee degenerative changes. Meniscal root repair is recommended in patients without significant osteoarthritis to restore native knee biomechanics and to avoid the long-term deleterious effects of its absence. Several repair techniques have been reported with satisfactory outcomes and low rate of complications. This chapter will provide a comprehensive review on meniscal root tears, diagnosis, indications, and treatment options currently available.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Introduction
Meniscal root tears constitute one of the most relevant pathologies of the knee because of its biomechanical immediate consequences and the long-term effects derived from its loss of functionality. These tears can be either an avulsion of the insertion of the meniscus attachment or radial tears which are within 1 cm of the meniscus insertion [2]. The uncompromised menisci absorb 40–70% of the contact force that is generated between the femur and the tibia, which allows for the menisci to convert the axial loads into circumferential hoop stresses [5]. When meniscal root tears occur, they result in the failure of the meniscus to distribute and absorb these forces, and this leads to degenerative changes in the knee [2]. These changes include accelerated cartilage degeneration, which are comparable to changes seen following a total meniscectomy [2]. Additionally, both partial and total meniscal root tears have been observed to cause extrusion of the meniscus. Extrusion of more than 3 mm has been reported to be associated with osteophyte formation and increased articular cartilage degeneration [43]. Up to a fifth of medial meniscus tears can occur in the posterior root attachments [25]. Anterior cruciate ligament (ACL) tears are oftentimes associated with posterior lateral meniscus root tears with one study reporting these root tears in 8 % of cases involving ACL tears [13]. Posterior medial meniscal root tears are oftentimes degenerative, but they can also occur with multiple ligament knee injuries in acute settings [13, 16, 42]. Patients with medial meniscal tear were more likely to have concomitant chondral defects, while on the other hand, 81 % of lateral meniscal root tears occurred concomitantly with ACL tears [42]. In addition to tears that occur with ACL injuries, malposition of the ACL tibial tunnel and reaming for tibial shaft fractures during ACL reconstruction can damage the anterior root attachments of the menisci [14, 34, 36, 53]. It has been widely reported that failing to preserve the meniscal tissue accelerates degeneration of the knee cartilage surfaces [22]. The goal of meniscal root surgery is to restore the joint to its previous function without causing adverse side effects like cartilage degradation and an inability to convert force loads that are often seen when the injury is ignored or a meniscectomy is performed [43]. The most common surgical approaches to treat meniscal root tears are meniscectomy, partial meniscectomy, transosseous root repair, and suture anchor repair techniques [43]. This chapter will provide a comprehensive review on meniscal root tears, diagnosis, indications, and treatment options currently available.
5.2 Anatomy
The medial tibial eminence (MTE) apex is the most reproducible osseous landmark for the medial meniscal posterior root attachment. The distance between the MTE and the center of the root attachment is located approximately 10 mm posterior and 1 mm lateral. The most proximal posterior cruciate ligament (PCL) tibial attachment and the medial tibial plateau articular cartilage inflection point are two other consistent landmarks to identify the root attachment and are located 8 mm and 4 mm lateral from the posterior root attachment, respectively. Therefore, during arthroscopic root repair surgery, the primary objective would be to locate the apex of the medial tibial eminence and follow it posteriorly and laterally along the bony surface to find the anatomic root attachment site. The lateral meniscus posterior root attachment can also be identified using the apex of the lateral tibial eminence (LTE) which is the most consistent landmark. The center of the lateral meniscal posterior root is consistently found to be 4 mm medial and 1.5 mm posterior to the LTE. According to Johannsen et al. [26], the posterior root of the lateral meniscus attachment is located 4 mm medial to the lateral tibial plateau articular cartilage edge and 13 mm to the most proximal edge of the posterior cruciate ligament (PCL) tibial attachment. The footprint of the central main attachment fibers of the posterior roots of the menisci is 39 mm2 for the lateral meniscus and 30 mm2 for the medial meniscus [26].
Axial view of the tibial plateau showing the menisci and their attachments along with the ACL and PCL footprints. LARA lateral anterior root attachment, LPRA lateral posterior root attachment, MARA medial anterior root attachment, MPRA medial posterior root attachment, LME lateral medial eminence, SWF shiny white fibers, AIL anterior intermeniscal ligament, ACL anterior cruciate ligament, PCL posterior cruciate ligament
5.3 Meniscal Root Biomechanics
The anteromedial (AM) root attachment is the strongest root attachment in the meniscus with an ultimate failure strength of 655 N, and the posterolateral (PL) root is the weakest with an ultimate failure strength of 509 N [15]. The increased mobility of the anterior roots compared to the posterior roots may account for the anterior root’s higher failure strength [3].
Lateral complete root tears prevent the circumferential fibers from withstanding the hoop stresses which cause the contact area to decrease and the mean and peak contact pressures to increase, which emulates a complete meniscectomy [35]. The overall failure to reproduce the native attachments in a functional anatomic location will result in the continuation of the previously mentioned issues with contact area and contact pressure [32]. Repair of posterolateral meniscal root avulsions resulted in reduced contact areas that were significantly less than the contact areas of intact roots when combined across all angles [47] even though the repair of posteromedial meniscal root avulsions can restore the contact area to intact levels at all angles [2]. A recent biomechanical study concluded that lateral meniscus posterior root avulsion produces significant alterations in the contact areas and pressures from full extension to 90° of flexion. Meniscectomy causes greater disorders than the avulsion left in situ. Transosseous repair with a single suture restores these alterations to conditions close to intact at 0° and 30° but not at 60° and 90° [49].
5.4 Natural History of Root Tears
There has been a recent push to understand the effects of meniscal root tears including both contact pressure distributions, similarities to meniscectomized states, and overall long-term outcomes. Harner et al. [23] reported that in tears of the posterior medial meniscus, peak contact pressures were on average 25 % higher than in the intact state. Additionally, when the peak contact pressures were compared to those following a medial meniscectomy, there was no significant difference between the two [23]. Another recent study by Chung et al. [9, 10] reported on the long-term results of patients who had a posterior meniscal root tear in their medial meniscus, and either underwent a refixation or a partial meniscectomy. The results of this study showed that those who underwent a refixation of the posterior root in the medial meniscus slowed the progression of arthritic changes compared to those who had a meniscectomy, although the refixation did not prevent the arthritic changes completely [9, 10]. Along with the overall difference in arthritic changes, 35 % of the patients who had undergone a meniscectomy underwent conversion to total knee arthroplasty (TKA) in contrast, whereas none of the patients who had undergone a repair underwent conversion to TKA [9, 10].
Choi et al. [7] reported that meniscal root tears were positively correlated with the grade of osteoarthritis (p=0.017), BMI (p=0.025), mechanical axis deviation (p=0.043), and varus deformity (p=0.027). Out of all the knees that underwent TKA, 78.17 % of patients under 60 years had meniscal root tear [7] (Fig. 5.2).
5.5 Diagnosis
5.5.1 Physical Examination
In order to effectively assess a potential meniscal root tear, both a physical exam and imaging methods should be performed since root tears are not always evident when a partial examination is done [13]. Additionally, when performing a physical exam, it is important to identify if the patient has varus alignment or a high BMI since these are some of the risk factors for medial meniscal root tears [25]. Meniscal root tears are often not associated with traumatic events, with one study reporting that 70 % of patients with meniscal root injuries could recall a minor traumatic event such as squatting, and the rest couldn’t recall any specific event leading up to the injury [4]. The most common presenting symptoms in meniscal root tears are posterior knee pain and joint line tenderness which are nonspecific symptoms [20]. Another common but not always present symptom is a popping sound which is heard while doing light activities like going upstairs or squatting [37]. Seil et al. [51] described a test that has proven useful in diagnosing a medial meniscal root avulsion. It involves applying varus stress to the knee while it is relaxed and in full extension and palpating the anteromedial joint line [51]. When there is a medial meniscal root avulsion, the meniscal extrusion is reproduced and disappears when the knee is moved back to its normal alignment [51].
5.5.2 Imaging
Magnetic resonance imaging (MRI) is noninvasive and should be a part of the diagnostic workout of meniscal root tears due to the challenges associated with a clinical diagnosis [4, 18]. Prior studies suggested that MRI is 93 % sensitive, is 100 % specific, and has a positive predictive value of 100 % [8, 12, 24]; however, other authors reported that meniscal root tears could only be identified in approximately 73 % [46]. Of note, an accurate diagnosis of a meniscal root tear through an MRI is very reliant on the skill of the radiology and the quality of the images [4].
The posterior medial meniscus is most easily visualized as a band of fibrocartilage, which anchors the posterior horn to the tibial plateau in two consecutive coronal MRI images [4]. Lateral meniscal root tears are most easily visualized on coronal and sagittal sequences that show both the apex and posterior slope of the lateral tibial eminence [4, 12]. T2-weighted sequences are considered the best option for visualizing tears due to their maximum specificity and sensitivity values [39]; additionally, many believe that axial images produce the highest specificity and sensitivity [8]. When a posterior meniscal root tear is suspected, three locations should be assessed on MRI: (1) between the intercondylar tubercles, (2) at the level of the lateral tubercle, and (3) on the lateral edge of the tibial eminence adjacent to the lateral tubercle. Additionally, both coronal and sagittal planes should be evaluated to improve sensitivity [13].
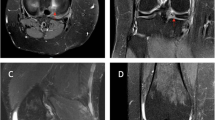
Since visualizing a meniscal root tear is difficult due to the root’s small size, the presence of meniscal extrusion has a high correlation with meniscal root tears [6, 41], although not all knees with meniscal extrusion have meniscal root tears [4]. Medial meniscal extrusions of more than 3 mm are strongly associated with severe meniscal degeneration and meniscal root tears [11, 40]. Another common and important sign associated with meniscal root tears is a ghost sign [4]. A ghost sign is defined to be the absence of an identifiable meniscus in the sagittal plane or an increased signal replacing the normally dark meniscal tissue signal [40, 48]. In addition to ghost signs, vertical linear defects on coronal imaging and radial linear defects at the bony insertion of the meniscal roots are also signs of meniscal root tears [29] (Fig. 5.3).
Magnetic resonance imaging of the right knee demonstrating (a) meniscal extrusion (>3 mm) and an edema of the medial femoral condyle on a coronal cut. (b) Sagittal view showing the absence of the posterior horn of the meniscus (“ghost sign”) and (c) sagittal view of a medial meniscus posterior root tear
5.6 Classification Systems
Our group developed an arthroscopically based classification system for both posterior root tears based on tear morphology. Root tears were divided in partial stable root tear (type 1), complete radial tear within 9 mm from the root attachment (type 2), bucket-handle tear with complete root detachment (type 3), complex oblique or longitudinal tear with complete root detachment (type 4), and bony avulsion of the root attachment (type 5) (Fig. 5.1) [33]. Of these types, type 2 was the more frequently encountered which can be subclassified in type 2A, defined as complete radial meniscal tears 0 to < 3 mm from the center of the root attachment; type 2B, defined as complete radial meniscal tears 3 to < 6 mm from the center of the root attachment; and type 2C, defined as complete radial meniscal tears 6–9 mm from the root attachment.
Forkel et al. [21] described a lateral posterior root tear classification (three subcategories). Type 1 is the avulsion of the root at the attachment on the tibial plateau with an intact meniscofemoral ligament. Type 2 is a radial tear of the posterior horn with an intact meniscofemoral ligament. Type 3 is a complete injury of the posterior horn of the lateral meniscus with rupture of the meniscofemoral ligament (Fig. 5.4).
Images of the five different types of meniscal root tears based on morphology: partial stable root tear (type 1), compete radial tear within 9mm of the bony root attachment (type 2), bucket-handle tear with complete root detachment (type 3), complex oblique or longitudinal tear with complete root detachment (type 4), and bony avulsion fracture of the root attachment (type 5). Types 2A, 2B, and 2C are marked on the image for type 2
5.7 Treatment
Although recently recognized as an important pathology, several treatment options have been described in the literature including nonoperative treatment, partial or subtotal meniscectomies, and root repair. Nonoperative treatment is advocated in the elderly population or those with advanced degenerative changes in the same compartment. Symptomatic treatment with rest, ice, nonsteroidal anti-inflammatory drug, and/or an unloader brace can help alleviate the symptoms in some cases. In this subset of patients (advanced degenerative changes), if mechanical symptoms are present such as locking, a partial or subtotal meniscectomy can improve the overall knee function.
Indications for meniscal repair are acute, traumatic root tears in patients with nearly normal or normal cartilage surface (Outerbridge less than grade 2) or chronic symptomatic root tears in young or middle-aged patients without significant preexisting osteoarthritis [4]. These injuries can develop subtly over time.
5.7.1 Transtibial Pullout Repair for Posterior Meniscus Root Tears
The transtibial pullout technique allows for anatomic reduction and fixation of the meniscal root. Padalecki et al. [47]) reported that a pullout repair of radial tears restored the joint contact pressure and area similar to the intact state. Drilling tibial tunnels may enhance healing due to the presence of growth factors and potentially bone marrow mesenchymal stem cells. The fixation construct has been reported to have significantly weaker fixation to the tibia compared to the native root [17, 31]. Feucht et al. [17] reported a 2.2 mm displacement of the meniscal root repair with transtibial pullout under cyclic loading in a pig model caused by the long length of the meniscus suture repair construct (bungee effect). Several authors have validated this technique the root transosseous repair [1, 30, 45, 50]. Starke et al. [52] reported that nonanatomic positioning of the posterior meniscal horn attachment had a significant effect on the resultant tension. Placing the horn attachment 3 mm medially decreased the tension at the horn attachment by 49–73 %, depending on knee flexion angle and femorotibial load. Conversely, fixation of the root in a lateral position resulted in a relative increase in the tension by 28–68 %. Lower levels of meniscal hoop tension caused increased cartilage stress.
The senior author’s current preferred technique for fixation of a posterior horn meniscal root tear involves transosseous suture repair tied over a button on the anteromedial tibia. For this technique, standard anterolateral and anteromedial portals are created adjacent to the patellar tendon. It is important to be as close as possible to the patellar tendon to improve visualization for the posterior roots (Fig. 5.5).
A diagnostic arthroscopy is performed to assess for any associated lesions. The damaged meniscal root should be probed to assess for severity and tear pattern [33]. An accessory arthroscopic portal (anteromedial or anterolateral) can be made to help access the posterior root. The bony bed of the planned root repair anatomic location should then be carefully decorticated using a curved curette (Fig. 5.6).
A grasper can be used to position the torn meniscal root and determine the ideal location to perform the repair. If the root can be positioned at the desired location, peripheral release of the posterior horn should be carried out to allow the root for additional excursion (Fig. 5.7).
Once the desired position of the root has been confirmed, an incision is made for the transtibial tunnels just medial to the tibial tubercle (medial root). For a posterior lateral meniscal root repair, the incision will be made on the anterolateral tibia, just distal to the medial aspect of Gerdy’s tubercle. In order to best restore the footprint of the repair, two transtibial tunnels are created at the location of the root attachment. A custom root aiming device with a cannulated sleeve is used to position a drill pin. A tibial tunnel guide is then used to ream the first tunnel (along the posterior aspect of the posterior root attachment site) (Fig. 5.8).
The second tunnel is placed approximately 5 mm anterior to the first tunnel using an offset guide. The tunnels are visualized arthroscopically to verify correct tunnel placement, and the drill pins are removed leaving the two cannulas in place for passing the sutures. An accessory anteromedial or anterolateral portal can be created if necessary depending on the root to be repaired (if not done previously) to allow an arthroscopic grasper to firmly hold the torn meniscal root and facilitate passing the sutures. A suture-passing device is utilized to pass a simple suture through the far posterior portion of the detached meniscal root, approximately 5 mm medial to its lateral edge for the medial meniscus, or 5 mm lateral to its medial edge for the lateral meniscus, passing from the tibial to the femoral side. Sutures are then pulled out through the anteromedial portal (through a cannula) as the device is removed. Prior to passing the second suture through the meniscus, the first suture is shuttled down through the more posteriorly placed tibial tunnel in order to avoid intra-articular suture tangling with the aid of a looped passing wire placed up the posteriorly placed tunnel cannula. The steps are repeated with the second suture positioned through the midportion of the meniscal root, anterior to the first suture placed into the meniscus. The second suture is then pulled down through the anterior positioned tibial cannula (Fig. 5.9).
The sutures are tied down over a cortical fixation device on the anteromedial tibia for the medial meniscal root repair, or the anterolateral tibia for the lateral meniscal root repair, while the posterior root of the respective meniscus is visualized and probed arthroscopically (Fig. 5.10).
5.8 Postoperative Rehabilitation
Patients should be non-weight-bearing for at least 6 weeks. Physical therapy should start as soon as possible after surgery, which should include early passive range of motion exercises in a safe zone of 0–90 degrees of flexion for the initial 2 weeks. After 2 weeks, patients can work on further increases in knee flexion as tolerated. Progressive advancement to full weight-bearing begins at 8 weeks. Deep leg presses and squats greater than 70 degrees of knee flexion should be avoided for at least four months after surgery (Fig. 5.11).
5.9 Outcomes
The optimal treatment of meniscal root tears is still debated due to the conflicting clinical and radiologic results that are being reported. Chung et al. [9, 10] reported in a recent meta-analysis on medial meniscal root tear repair that although there were significant improvements in postoperative clinical scores, the progression of arthrosis was not prevented and meniscal extrusion was not reduced. Feucht et al. [18] reported in a systematic review that there were improved outcomes when arthroscopic transtibial pullout repair was used for posterior medial meniscal root tears. The systematic review reported that 84 % of the patients showed no progression of osteoarthritis on the Kellgren-Lawrence grading scale, and Lysholm scores improved from a mean of 52 preoperatively to a mean of 86 postoperatively [18]. Additionally, in 82 % of the patients, MRI did not show progression of cartilage degeneration, and in 56 % of patients, MRI showed a reduction of medial meniscus extrusion [18]. Overall the healing status was complete in 62 % of patients, partial in 34 %, and failed in only 3 % based on MRI and second-look arthroscopy [9, 10, 18]. A retrospective study by Ozkoc et al. [46] looked at patients with a medial meniscus posterior root tear (MMPRT) who were treated with a partial meniscectomy and had a mean follow-up of 4.7 years. This study found that the Lysholm scores of the patients had improved significantly although degenerative changes as defined by the Kellgren-Lawrence radiologic grade had increased postoperatively [46]. Another study done by Chung et al. [9, 10] compared the radiologic and clinical outcomes between a partial meniscectomy cohort and a medial meniscus root repair cohort at a 5-year minimum follow-up. The repair group reported significantly higher Lysholm and International Knee Documentation Committee (IKDC) scores although both groups showed a progression of Kellgren-Lawrence grade and medial joint space narrowing with the repair cohort showing less progression in comparison to the partial meniscectomy cohort [9, 10]. Finally, the repair cohort had a 0 % rate of conversion to total knee replacement, whereas the partial meniscectomy cohort had a 35 % rate [9, 10].
The median age of patients in meniscal root repair studies is around 50 years, meaning that the outcomes on meniscal root repairs are based on poorly designed studies with potentially skewed data [8, 27–29, 38, 44]. Although the majority of studies have reported subjective improvement of symptoms, the prevention of progression of arthrosis has not been adequately documented [9, 10, 16, 18, 19, 20, 46]. Additionally, the poor reduction of meniscal extrusion or the failure to do so and low reported healing rates coupled with the age of the patients may help explain the poor radiographic results [9, 10, 18, 19]. Meniscal root tears are technically challenging procedures, with an anatomic repair being crucial to the success and outcome of the surgery. This type of procedure may be better left to more experienced surgeons with enough volume. Overall there is still a great deal of need for better designed studies to explore some of the unanswered questions regarding meniscal root repairs.
References
Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1510–3.
Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–31.
Benjamin M, Evans EJ, Rao RD, Findlay JA, Pemberton DJ. Quantitative differences in the histology of the attachment zones of the meniscal horns in the knee joint of man. J Anat. 1991;177:127–34.
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–30.
Bonasia DE, Pellegrino P, D’Amelio A, Cottino U, Rossi R. Meniscal root tear repair: why, when and how? Orthop Rev (Pavia). 2015;7(2):5792.
Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–6.
Choi ES, Park SJ. Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg Relat Res. 2015;27(2):90–4.
Choi SH, Bae S, Ji SK, Chang MJ. The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2098–103.
Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol: Arthrosc; 2015.
Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH, Kim JG. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–50.
Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23.
De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480–6.
De Smet AA, Mukherjee R. Clinical, MRI, and arthroscopic findings associated with failure to diagnose a lateral meniscal tear on knee MRI. AJR Am J Roentgenol. 2008;190(1):22–6.
Ellman MB, James EW, LaPrade CM, LaPrade RF. Anterior meniscus root avulsion following intramedullary nailing for a tibial shaft fracture. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1188–91.
Ellman MB, LaPrade CM, Smith SD, Rasmussen MT, Engebretsen L, Wijdicks CA, LaPrade RF. Structural properties of the meniscal roots. Am J Sports Med. 2014;42(8):1881–7.
Feucht MJ, Bigdon S, Mehl J, Bode G, Muller-Lantzsch C, Sudkamp NP, Niemeyer P. Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):140–5.
Feucht MJ, Grande E, Brunhuber J, Rosenstiel N, Burgkart R, Imhoff AB, Braun S. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med. 2014;42(1):187–93.
Feucht MJ, Kuhle J, Bode G, Mehl J, Schmal H, Sudkamp NP, Niemeyer P. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–16.
Feucht MJ, Minzlaff P, Saier T, Lenich A, Imhoff AB, Hinterwimmer S. Avulsion of the anterior medial meniscus root: case report and surgical technique. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):146–51.
Feucht MJ, Salzmann GM, Bode G, Pestka JM, Kuhle J, Sudkamp NP, Niemeyer P. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):119–25.
Forkel P, Foehr P, Meyer JC, Herbst E, Petersen W, Brucker PU, Burgkart R, Imhoff AB. Biomechanical and viscoelastic properties of different posterior meniscal root fixation techniques. Knee Surg Sports Traumatol Arthrosc. 2016 Jul 11. [Epub ahead of print]. PMID: 27401006.
Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH, Yoo SH, Nha KW. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326–32.
Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):257–70.
Harper KW, Helms CA, Lambert 3rd HS, Higgins LD. Radial meniscal tears: significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185(6):1429–34.
Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, Jung KA. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–10.
Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342–7.
Jung YH, Choi NH, Oh JS, Victoroff BN. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40(6):1406–11.
Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–53.
Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, Lee MY. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–54.
Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22(7):795. e791-794
Kopf S, Colvin AC, Muriuki M, Zhang X, Harner CD. Meniscal root suturing techniques: implications for root fixation. Am J Sports Med. 2011;39(10):2141–6.
LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, Wijdicks CA, LaPrade RF. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912–20.
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–9.
Laprade CM, James EW, Engebretsen L, Laprade RF. Anterior medial meniscal root avulsions due to malposition of the tibial tunnel during anterior cruciate ligament reconstruction: two case reports. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1119–23.
LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–9.
LaPrade CM, Jisa KA, Cram TR, LaPrade RF. Posterior lateral meniscal root tear due to a malpositioned double-bundle anterior cruciate ligament reconstruction tibial tunnel. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3670–3.
Lee DW, Ha JK, Kim JG. Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res. 2014;26(3):125–34.
Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–8.
Lee SY, Jee WH, Kim JM. Radial tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol. 2008;191(1):81–5.
Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–74.
Magee T. MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging. 2008;28(2):466–70.
Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–31.
Moatshe G, Chahla J, Slette E, Engebretsen L, Laprade RF. Posterior meniscal root injuries. Acta Orthop. 2016:1–7.
Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40(5):1138–43.
Nicholas SJ, Golant A, Schachter AK, Lee SJ. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1433–6.
Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–54.
Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, Laprade RF. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699–707.
Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106:91–115.
Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, Prado Novoa M, Espejo-Reina A, Quintero Lopez C, Ezquerro Juanco F. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32(4):624–33.
Raustol OA, Poelstra KA, Chhabra A, Diduch DR. The meniscal ossicle revisited: etiology and an arthroscopic technique for treatment. Arthroscopy. 2006;22(6):687. e681-683
Seil R, Duck K, Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2072–5.
Starke C, Kopf S, Grobel KH, Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy. 2010;26(3):358–65.
Watson JN, Wilson KJ, LaPrade CM, Kennedy NI, Campbell KJ, Hutchinson MR, Wijdicks CA, LaPrade RF. Iatrogenic injury of the anterior meniscal root attachments following anterior cruciate ligament reconstruction tunnel reaming. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2360–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 ISAKOS
About this chapter
Cite this chapter
Phocas, A., Chahla, J., LaPrade, R.F. (2017). Meniscal Root Tears: A Missed Epidemic? How Should They Be Treated?. In: LaPrade, R., Arendt, E., Getgood, A., Faucett, S. (eds) The Menisci. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53792-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-662-53792-3_5
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53791-6
Online ISBN: 978-3-662-53792-3
eBook Packages: MedicineMedicine (R0)