Abstract
Purpose
To determine whether reaming of anterior cruciate ligament (ACL) reconstruction tibial tunnels with a 10-mm-diameter reamer would result in injury to the anterior roots of the medial and lateral menisci in an in vitro model when using a tibial aiming device at two settings (40° and 60°).
Methods
Three-dimensional footprints of the ACL and the anterior roots of the menisci were measured for 12 human cadaveric tibias. Measurements were taken before and after attempted reaming of an ACL tibial reconstruction tunnel in the calculated ACL centre using a tibial aiming device set at two angles (40° and 60°).
Results
Iatrogenic injury to the anterior root of the medial meniscus caused by overlap with the reamed tibial tunnel was found in 3/6 specimens in Group 1 (40°) and 0/6 specimens in Group 2 (60°). The average area of iatrogenic injury in Group 1 was 9.6 mm2 (8.6 % of the root). There was iatrogenic injury to the anterior root of the lateral meniscus in 4/6 specimens for both groups. The average area of iatrogenic injury was 20.5 mm2 (28.8 %) for Group 1 and 16.2 mm2 (25.9 %) for Group 2.
Conclusions
Reaming of ACL tibial reconstruction tunnels carries a risk of iatrogenic injury to the anterior meniscus roots, even when tunnels are reamed based on guide pin placement in the calculated centre of the ACL. Reaming at varying tibial aiming device angle settings can affect the obliquity of the tunnel aperture and cause iatrogenic injury to the anterior meniscal roots. Caution should be exercised clinically to avoid iatrogenic injury to both the anterior meniscal roots while reaming tibial tunnels during ACL reconstructions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of the meniscal root in joint function and the consequences of its loss have been well studied [2, 12, 17, 18, 28]. It has been reported that the meniscal roots serve as anchor points that allow the body of the meniscus to act as a shock absorber and transmit loads across the knee joint [11, 23, 25]. However, the loss of the meniscal attachments disrupts the circumferential fibres of the menisci and prevents the distribution of hoop stresses [2, 11, 23, 25]. This inability to transmit loads evenly across the knee may result in excessive loading and articular cartilage degeneration [2, 11, 23, 25].
Prior studies have examined the anatomy and biomechanics of the meniscal root attachments; however, the majority of this work has been regarding the posterior root attachments [2, 7, 8, 10, 16, 18, 22]. Relatively few investigations have studied the anatomy of the meniscal anterior root attachments, and many of these studies have only qualitatively defined the anatomic location of the root attachments or variable insertions [3, 11, 14, 20]. Few studies have defined the anterior roots in reference to pertinent surgical landmarks in the knee, and these studies only reported quantitative distances between the lateral or medial meniscal anterior root and the anterior cruciate ligament (ACL) [4, 11, 29, 30]. Presently, the relationship of the anterior meniscal roots with other important ligamentous and bony landmarks is understudied, and as a result, there is limited understanding of where these roots are located during arthroscopy.
At this point in time, there are only limited case reports describing anterior meniscal root avulsions [6, 15, 19, 26]. While these injuries may be relatively rare, the creation of anterior meniscal root avulsions has been reported to result in a level of meniscal extrusion that is a significant predictor of accelerated osteoarthritis in patients, with 89 % of patients in one study having meniscal extrusion twice that of the threshold for instigation of osteoarthritis [5, 17]. Due to the undefined quantitative anatomy of the anterior meniscal roots, there is also limited information regarding injury to the medial and lateral meniscus roots during ACL reconstruction, with only a recent case series demonstrating these injuries [15].
The purpose of this study was to determine whether reaming of ACL reconstruction tibial tunnels with a 10-mm-diameter reamer would result in injury to the anterior roots of the medial and lateral menisci in an in vitro setting when using a tibial aiming device at two settings (40° and 60°) in reference to the sagittal plane. It was hypothesized that reaming of the ACL reconstruction tibial tunnel over a guide pin centred over the anatomic footprint of the native ACL would result in damage to the anterior roots of the medial and lateral menisci at both tibial aiming device settings. In addition, decreased iatrogenic injury to the anterior horn of both medial and lateral meniscus roots was hypothesized to occur with a higher flexion angle setting of a tibial aiming guide.
Materials and methods
Specimens consisted of 12 fresh-frozen human cadaveric knees (eight males and four females) with an average age of 54 years (median 56, range 44–67). This work was performed at the (blinded for review) where research involving de-identified cadaveric specimens is exempted from IRB review. Exclusion criteria prior to obtaining the specimens excluded knees with significant degenerative changes or absence of cruciate ligaments or menisci. The skin, muscle, collateral ligaments and capsular tissue were removed from all specimens. The tibial attachments of the ACL and posterior cruciate ligament (PCL) were left intact, while the femoral attachments were resected to leave the maximum amount of the ACL and PCL fibres intact. The fibula was disarticulated from the tibia by incision through the proximal and distal tibiofibular ligament attachments. A full-length tibia remained, and its articular surface was inspected for arthritic changes and degeneration of the menisci or cruciate ligaments. The tibia was then rigidly secured in a custom fixture (Fig. 1) and randomly assigned into one of two separate groups. One group utilized a point-to-shoot tibial aiming guide set at 40° (Acufex Director, Smith and Nephew, Inc., Memphis, TN) for tibial tunnel reaming, and the other used the same guide with the angle set to 60°. These angles were in reference to the sagittal plane with the superior surface of the guide parallel to the tibial plateau.
Representation of the testing set-up with the knee securely positioned in a custom clamp to prevent any movement during testing. The coordinate measuring device (in blue) was used to measure interspatial relationships between the anterior meniscus root attachments and ACL native footprint and reamed tibial tunnels
Measuring distances in millimetres in X, Y and Z coordinates using a coordinate measuring device (MicroScribe-MX, GoMeasure3D, Amherst, VA), the outer circumference of the ACL footprint was marked with 40 coordinate points. The outer circumference of the anterior roots of the medial and lateral menisci was then outlined with 30 coordinate points. The footprints of the meniscal root attachments were determined by varying tension on the fibres of the meniscal roots to determine exactly where the fibres attached to the tibial plateau, thereby modelling a previous study [10]. As an assessment of accuracy for the coordinate measuring device, a single-point articulation performance test (SPAT) was performed by the manufacturer (GoMeasure3D, Amherst, VA) based on the B89.4.22 American Society of Mechanical Engineers (ASME) standard. The average SPAT result was reported to be ±0.126 mm, which describes the repeatability and reproducibility of the measurements [10].
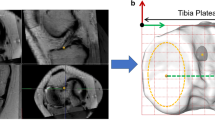
The ACL was then transected at its insertion site, and the centre of the footprint was calculated using the coordinate measuring device. For Group 1, a point-to-shoot tibial aiming guide was set at 40° and placed parallel to the tibial plateau 1 cm medial to the medial edge of the patellar tendon insertion at the tibial tuberosity. The tip of the tibial aiming device was then placed in the calculated centre of the ACL footprint. The anterior point of guide pin entry on the tibial plateau was then measured in X, Y and Z coordinates. The pin was then over-reamed with a 10-mm-diameter reamer (Cannulated Headed Reamer, Arthrex, Naples, FL) according to common clinical reamed ACL tunnel diameters [1]. The reaming procedure is described in Fig. 2. Next, using the coordinate measuring device, the borders of the tibial tunnel aperture were mapped out with 20 coordinate points and repeat measurements around the circumference of the anterior root attachments of the medial and lateral menisci were taken with 30 coordinate points each. The distances to the centre of the tibial tunnel entry point were measured in both medial–lateral and superior–inferior directions using an electronic calliper with reported accuracy of ±0.03 mm (Swiss Precision Instruments Inc., Garden Grove, CA). Medial–lateral distances to the tibial tunnel entry point were measured from the medial edge of the patellar tendon, and superior–inferior distances were measured from the superior-most portion of the articular surface of the lateral tibial plateau. The area of the anterior roots of the medial and lateral menisci and the reamed tibial tunnel was calculated using Heron’s formula as described by a previous study [10]. These areas were used to determine the percentage overlap of the tibial tunnel with the meniscal anterior root attachment footprints, therefore determining the percentage of the root that was removed with reaming. For Group 2, six specimens were tested by changing the angle of the tibial aiming device to 60° and repeating the same measurements as for Group 1. The measurements were taken as described above by the same individual (initials blinded for review) and collected on a standardized collection sheet. All measurement calculations were performed with a custom program utilizing MATLAB software (R2013a, The Mathworks, Natick, MA).
Photographs demonstrating the reaming of tibial tunnels during ACL reconstruction. a Demonstration of using the coordinate measuring device stylus to calculate the centre of the ACL footprint. The tibial aiming guide was then placed at this exact site. b The guide pin was then drilled through the centre of the ACL footprint. A 10-mm reamer was then positioned on the anteromedial surface of the tibia. c Overhead view of the reamer exiting through the centre of the ACL footprint on the tibial plateau
Statistical analysis
Matched comparisons of quantitative distances between the ACL and menisci between pre- and post-reaming conditions were performed with Wilcoxon signed-rank tests. Mann–Whitney U tests were used to compare the pre- to post-reaming change between groups 1 and 2 in terms of these same quantitative distances. A p value of less than 0.05 was considered statistically significant, and all statistical analyses were performed using IBM SPSS Statistics, version 20 (Armonk, NY). For the reporting of the pre- and post-reaming measurements of the meniscal footprints, as well as the meniscal root–ACL reconstruction tunnel overlap calculations, a qualitative approach to reporting values was utilized. This was chosen because the observation of two qualitative measures (hitting or not hitting the root) would not result in a clear numerical comparison that would be required for reporting significance.
Results
ACL footprint and meniscal root quantitative relationship
After tunnel reaming, the ACL tunnels were observed to be more anterior than the native ACL footprint (Table 1). The post-reaming distances between the ACL tunnel and anterior root of the medial meniscus were significantly smaller than the pre-reaming distances for Group 1 (p = 0.027) and Group 2 (p = 0.003) (Fig. 3).
Distances measured from the meniscus root footprint centre to the ACL reconstruction tibial tunnel footprint centre. The ACL tibial tunnel centre to the centre of the anterior root attachment of the lateral meniscus measurement (A), and the ACL tibial tunnel centre to the anterior root attachment of the medial meniscus measurement (B) are labelled. The menisci were transected after these measurements to allow for accurate measurement of their root attachment
Before and after tunnel reaming, measurements were taken from the centre of the native ACL and ACL tunnel to the anterior root of the lateral meniscus. Group 1 was not significantly different between pre- and post-reaming distances, but in Group 2, the post-reaming distance was significantly closer than the pre-reaming distance (p = 0.021).
Qualitative measurement of the meniscal roots
The anterior root attachments of the medial meniscus pre-reaming footprints were 125.5 mm2 (95 % CI 107.9, 143.0) and 117.2 mm2 (95 % CI 83.7, 150.7) for groups 1 and 2, respectively. Post-reaming footprints were 119.6 mm2 (95 % CI 98.1, 141.1) for Group 1 and 118.9 mm2 (95 % CI 90.9, 147.0) for Group 2. The anterior root attachments of the lateral meniscus pre-reaming footprints were 72.1 mm2 (95 % CI 59.7, 84.6) and 75.1 mm2 (95 % CI 53.4, 96.9) for groups 1 and 2, respectively. Post-reaming footprints were 73.0 mm2 (95 % CI 64.4, 81.7) for Group 1 and 61.2 mm2 (95 % CI 44.9, 77.5) for Group 2.
ACL reconstruction tunnel and anterior meniscal root qualitative overlap
There was overlap between the calculated footprints of the anterior root of the medial meniscus and the reamed tibial tunnel, which suggests an iatrogenic injury to the root, in three of six specimens in Group 1 and zero of six specimens in Group 2. The average amount of iatrogenic overlap in Group 1 was calculated in terms of the area (9.6 mm2, range 2.3–18.4 mm2) and percentage of the root attachment (8.6 %). Concerning the anterior root of the lateral meniscus, there was iatrogenic overlap between the footprint of the root and the reamed tibial tunnel in four of six specimens for both groups. In Group 1, the average iatrogenic overlap between the lateral meniscus and reamed tibial tunnel was 20.5 mm2 (range 1.1–36.2 mm2) and 28.8 %. For Group 2, the average iatrogenic overlap was 16.2 mm2 (range 4.1–31.8 mm2) and 25.9 %.
Discussion
The most important finding of the present study is that iatrogenic injury to the anterior roots of the medial and lateral menisci can occur while reaming ACL tibial reconstruction tunnels. Indeed, the fact that iatrogenic overlap was found after tunnels were reamed based on a guide pin placed in the centre of the ACL footprint lends concern about any tunnel placed more anteriorly, which may lead to increased iatrogenic overlap of the ACL tunnel footprint and the anterior meniscus root footprints. Iatrogenic injury to the anterior roots of the medial and lateral menisci was seen in 25 and 67 % of reamed tunnels across both testing groups, respectively, even though the guide pin was placed directly in the calculated centre of the ACL footprint. This provides evidence to the hypothesis that it is possible to cause iatrogenic injury to either meniscal root when reaming an ACL reconstruction tibial tunnel. A higher qualitative incidence of medial meniscal anterior root injury using a tibial aiming guide set at 40° was found compared with the same guide set at 60°. This gives credence to the hypothesis that a higher flexion angle on a tibial aiming device for ACL reconstruction tibial tunnel reaming may result in decreased iatrogenic injury to the anterior root of the medial meniscus. However, both guide angles resulted in iatrogenic injury to the anterior root of the lateral meniscus in four of six specimens. Therefore, the results from this study appear to indicate that while both anterior roots may be prone to iatrogenic injury during ACL reconstructions, the lateral meniscus may be more susceptible to inadvertent damage, regardless of the setting of the tibial aiming guide.
Another essential finding of this study was the recognition that the centre of the ACL reconstruction tibial tunnels may potentially shift anterior in comparison with the native ACL tibial footprint. The authors acknowledge that the anterior edge of the reamer is what first enters the joint as the acorn reamer travels over the guide pin, and the reamer may move slightly anterior during reaming unless a solid reamer is used or a fixed pin is used. This is hypothesized to be the reason why the reamed tunnels for Group 1 and Group 2 resulted in tibial tunnels that were centred significantly more anterior and closer to the anterior medial meniscal roots than the native ACL tibial footprint. In addition, the Group 2 reamed tunnels also moved significantly anterior and closer to the lateral meniscus as well. The authors believe that this anterior movement of the reamed tunnels in comparison with the native ACL represents the true risk of reaming the tibial tunnels during ACL reconstructions, especially when using an acorn tipped reamer. In addition, due to the obliquity of the tibial tunnel, the actual aperture was oblique and not perfectly round at the point of exiting into the joint. This implies that the leading edge of the oval is a few millimetres anterior to the actual guide pin entry, not because the guide pin was errant but because the aperture was oblique. Once again, knowledge of this mechanical finding is important because the larger the aperture, the greater the risk of anterior meniscal root injury and/or anterior movement of the tibial tunnel.
In this study, the distance from the centre of the ACL attachment area to the medial meniscus attachment centre was an average of 20.6 and 21.3 mm for groups 1 and 2, respectively. In the only known previous anatomic studies relating the ACL and medial meniscus anterior root, the posterior aspect of the medial meniscus root has been reported to insert an average of 7 mm anterior to the anterior aspect of the ACL tibial insertion and approximately 11.5 mm from the centre of the ACL footprint [4, 11]. In addition, the distance from the lateral meniscus attachment centre to the centre of the ACL attachment area was an average of 8.5 and 8.4 mm for the two groups in this study. Recently, Ziegler et al. [30] quantified the relationship between the ACL and different bony and soft tissue landmarks, including the lateral meniscus. They reported that the ACL centre was an average of 7.5 mm medial to the centre of the anterior root of the lateral meniscus, 10.2 mm posteromedial to the anteromedial aspect of the anterior horn and 8.5 mm anteromedial to the posteromedial aspect of the anterior horn of the lateral meniscus. As seen with the paucity of studies regarding the relationship between the medial and lateral meniscal roots and the ACL, the authors propose that the minimal literature regarding anterior meniscus root injury after ACL reconstructions is likely due to lack of recognition rather than lack of damage to the roots. However, with two studies illustrating increased levels of radiographic osteoarthritis after concurrent meniscal tears and ACL injury in comparison with isolated ACL tears [21, 27], the possibility of iatrogenic injury to the anterior meniscal roots should be a concern for surgeons to avoid stimulating any possible osteoarthritis in the future after ACL reconstruction.
Several studies have confirmed the importance of preservation of the posterior meniscal roots. Two studies have reported that medial meniscal posterior root tears resulted in peak contact pressures that were not significantly different from a total medial meniscectomy [2, 18]. Clinical studies also have found that in the long term, partial meniscectomies are correlated with increased prevalence of osteoarthritis, while meniscal repair resulted in significantly less progression of osteoarthritis [9, 13, 24]. Other studies have shown that posterior root avulsions result in significant increases in peak contact pressure and decreased contact areas in comparison with the intact knee [7, 16, 22]. Two studies also found a significant increase in clinically significant meniscal extrusion and gap formation with medial meniscus root tears compared to native and post-repair conditions [8, 18]. Costa et al. [5, 17] also reported that all anterior horn roots examined in their study resulted in >3 mm of meniscal extrusion, and this amount of extrusion has been significantly associated with degenerative changes to the articular cartilage and theorized to precede and influence future articular cartilage damage. Therefore, biomechanical, clinical and radiographic studies indicate intact meniscal roots are essential for avoidance of articular cartilage damage in the knee. Although the clinically significant amount of meniscal root disruption has not been quantified, it is shown from this study that even with guide pin placement in the centre of the ACL footprint, the ACL reconstruction tibial tunnels may move anteriorly and meniscal root injury may also result. In addition, this study indicates that the ACL tibial tunnels have a slim margin for error for placement before they could result in iatrogenic anterior meniscal root injury, with increasing misaligned tibial tunnel placement theoretically leading to the possibility of complete anterior meniscal root avulsions.
The authors acknowledge some limitations in this study. The specimens were dissected free of all soft tissue attachments, so the angle used for the tibial guide was very consistent. However, this situation was different than in vivo given the slight angular alterations needed to insert the guide through the portals and onto the desired spot on the tibial plateau; however, this method was chosen to standardize the tunnel reaming. In this study, the tibial tunnels were also reamed in the anterior portion of the ACL footprint, as discussed previously, although the guide pin was placed in the calculated centre of the ACL footprint. However, the authors believe that this finding represents a true risk of ACL reconstruction tibial tunnel reaming, especially when using an acorn reamer, and proposes that future studies investigate whether this anterior displacement occurs in vivo.
In this study, clinical relevance was related to the finding that even when the tunnels were attempted to be reamed in the centre of the ACL footprint, meniscal damage frequently occurred. With the close proximity of the anterior meniscal roots to the ACL footprint and the inherent difficulty of reaming tibial tunnels directly in the centre of the ACL footprint during surgery, it is theorized that an iatrogenic mechanism of injury may be a potential risk to the anterior meniscal roots. Even though anterior root avulsion may be a rare injury post-ACL reconstruction, it is possible that disrupting the anterior root could have deleterious consequences similar to posterior root avulsions. This study utilized a coordinate measuring device to place the tibial guide pin in the exact centre of the ACL footprint and still reported frequent meniscal damage and anterior movement of the ACL reconstruction tunnels, which shows that there is very little room for error for placement of the ACL tunnel. The authors propose that future studies investigate the effect of nonanatomic ACL reconstruction tunnel reaming on the incidence of iatrogenic anterior meniscus root injury.
Conclusions
This study demonstrates that even with a guide pin positioned in the calculated anatomic centre of the ACL footprint, the attachments of the anterior meniscal roots can be damaged. In addition, this study illustrated that even when ACL reconstruction tibial tunnels are reamed according to a guide pin placed at the calculated centre of the ACL, the centre of the tibial tunnels may move anteriorly and closer to the anterior meniscal roots. Caution should be exercised clinically to avoid iatrogenic injury to both anterior meniscal roots while reaming tibial tunnels during ACL reconstructions.
References
Aga C, Rasmussen MT, Smith SD, Jansson KS, LaPrade RF, Engebretsen L, Wijdicks CA (2013) Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissue anterior cruciate ligament reconstruction on the tibial side. Am J Sports Med 41:841–848
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Berlet GC, Fowler PJ (1998) The anterior horn of the medial meniscus: an anatomic study of its insertion. Am J Sports Med 26:540–543
Bhatia S, Korth K, Van Thiel GS, Gupta D, Cole BJ, Bach BR Jr, Verma NN (2013) Effect of reamer design on the posteriorization of the tibial tunnel during endoscopic transtibial anterior cruciate ligament reconstruction. Am J Sports Med 41:1282–1289
Costa CR, Morrison WB, Carrino JA (2004) Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? Am J Roentgenol 183:17–23
Feucht MJ, Minzlaff P, Saier T, Lenich A, Imhoff AB, Hinterwimmer S (2013) Avulsion of the anterior medial meniscus root: case report and surgical technique. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2462-7
Harner CD, Mauro CS, Lesniak BP, Romanowski JR (2009) Biomechanical consequences of a tear of the posterior root of the medial meniscus. J Bone Joint Surg Am 91(Suppl 2):257–270
Hein CN, Gurske-Deperio J, Ehrensberger MT, Marzo JM (2011) Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee 18:189–192
Hoser C, Fink C, Brown C, Reichkendler M, Hackl W, Bartlett J (2001) Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage. J Bone Joint Surg Br 83-B:513–516
Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF (2012) Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med 40:2342–2347
Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD (1995) Insertion-site anatomy of the human menisci: gross, arthroscopic and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 11:386–394
Jones AO, Houang MTW, Low RS, Wood DG (2006) Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol 50:306–313
Jørgensen U, Sonne-Holm S, Lauridsen F, Rosenklint A (1987) Long-term follow-up of meniscectomy in athletes. A prospective longitudinal study. J Bone Joint Surg Br 69-B:80–83
Kohn D, Moreno B (1995) Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy 11:96–103
LaPrade CM, James EW, Engebretsen L, LaPrade RF (2014) Anterior medial meniscal root avulsions due to malposition of the tibial tunnel during anterior cruciate ligament reconstruction: two case reports. Knee Surg Sports Traumatol Arthrosc 22:1119–1123
LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF (2014) Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 96:471–479
Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 33:569–574
Marzo JM, Gurske-DePerio J (2009) Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med 37:124–129
Navarro-Holgado P, Cuevas-Perez A, Aguayo-Galeote M, Carpintero-Benitez P (2007) Anterior medial meniscus detachment and anterior cruciate ligament tear. Knee Surg Sports Traumatol Arthrosc 15:587–590
Ohkoshi Y, Takeuchi T, Inoue C, Hashimoto T, Shigenobu K, Yamane S (1997) Arthroscopic studies of variants of the anterior horn of the medial meniscus. Arthroscopy 13:725–730
Øiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38:2201–2210
Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, LaPrade RF (2014) Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in-situ pullout repair restores derangement of joint mechanics. Am J Sports Med 42:699–707
Shepard MF, Hunter DM, Davies MR, Shapiro MS, Seeger LL (2002) The clinical significance of anterior horn meniscal tears diagnosed on magnetic resonance images. Am J Sports Med 30:189–192
Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal repairs. Am J Sports Med 38:1542–1548
Shrive NG, O’Connor JJ, Goodfellow JW (1978) Load-bearing in the knee joint. Clin Orthop Relat Res 131:279–287
Toy JO, Feeley BT, Gulotta LV, Warren RF (2011) Arthroscopic avulsion repair of a pediatric ACL with an anomalous primary insertion into the lateral meniscus. HSS J 7:190–193
Von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Vyas D, Harner CD (2012) Meniscus root repair. Sports Med Arthrosc 20:86–94
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36:65–72
Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF (2011) Arthroscopically pertinent landmarks for tunnel positioning in single bundle and double bundle anterior cruciate ligament reconstructions. Am J Sports Med 39:743–752
Acknowledgments
This study was funded by the Steadman Philippon Research Institute and did not receive any external funding. The authors would like to acknowledge Grant Dornan, MSc, for his statistical expertise and Max Michalski, MD, MSc, for his assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watson, J.N., Wilson, K.J., LaPrade, C.M. et al. Iatrogenic injury of the anterior meniscal root attachments following anterior cruciate ligament reconstruction tunnel reaming. Knee Surg Sports Traumatol Arthrosc 23, 2360–2366 (2015). https://doi.org/10.1007/s00167-014-3079-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3079-1