Abstract
Most research concerning iontophoresis has focused on topical and transdermal drug delivery and in non-invasive skin sampling applications. Iontophoresis has been established as a safe, versatile and efficient enhancement technique, and several iontophoretic devices have been marketed for topical (lidocaine) and systemic (fentanyl, sumatriptan) delivery and for non-invasive sampling (glucose). Nevertheless, the last decade has seen an increased interest into the potential use of iontophoresis to deliver drugs through the nail and through the sclera and cornea, the two main barriers to eye drug delivery. This chapter aims to summarize the main progress achieved in these areas.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Rationale and Feasibility of Iontophoretic Drug Delivery
Transdermal drug delivery either by passive or iontophoretic means is indicated for drugs whose oral bioavailability is severely affected by first-pass effect. Avoidance of either enteric or hepatic metabolism allows dose reduction in some cases such as oestradiol and selegiline (Delgado-Charro and Guy 2001a; Azzaro et al. 2007), attaining a better drug/metabolite ratio. Transdermal administration is also convenient when oral absorption is erratic or low, for example, in patients suffering from nausea, diarrhoea or irregular gastrointestinal transit (Parkinson’s disease). In the case of topical administration, both modes of delivery allow targeting the drug locally and minimizing systemic side effects and drug interactions.
With respect to passive diffusion, iontophoresis expands the range of drugs administrable via the transdermal and topical routes to include some compounds with low passive permeability such as polar and charged compounds, i.e. those with a relatively high molecular weight and/or low partition coefficient (Kalia et al. 2004; Delgado-Charro 2009). Therefore, the physicochemical properties of the drug should be carefully considered before adopting a passive or an iontophoretic administration. Specifically, an ideal candidate for iontophoretic delivery will have sufficient aqueous solubility and electrical mobility to be delivered by electromigration with an optimum transport number (Phipps and Gyory 1992; Sage and Riviere 1992). The ionization properties of the drug are crucial, more precisely a pKa allowing sufficient ionization and charge/mass ratio at an acceptable pH (Nangia et al. 1996; Berner et al. 1988). Salts are typically preferred, and, in the case of cationic compounds, chloride salts will provide the chloride ions required for the Ag/AgCl anode electrochemistry without the need of additional competing salts (Scott et al. 2000). In the case of neutral, zwitterionic drugs to be delivered by electro-osmosis, good solubility is essential to maximize the drug concentration in the vehicle.
Concerning the therapeutic needs and pharmacokinetic properties of the drug, iontophoresis is particularly advantageous when there is a need for fast and pulsatile administration and individualized titrated doses or, as mentioned before, when oral absorption is erratic. It is not surprising therefore that iontophoretic applications have been found for hormonal therapy (LHRH analogues and fertility treatment); for Parkinson’s disease, migraine treatment (ZecuityTM, NuPathe Inc., USA) and antiemetic drugs; and for self-administered pain therapy (Ionsys® – fentanyl, Alza Corporation, USA) (Kalia et al. 2004; Delgado-Charro 2009).
Iontophoresis has been used primarily for drugs, the passive diffusion of which is very low, but this is not necessarily the case. For example, nicotine passive patches are widely available in the market, yet nicotine iontophoresis was investigated as a means to achieve a quick burst of the drug comparable to that provided by cigarettes (Brand and Guy 1995).
Additionally, in the case of topical administration, iontophoresis may be useful to target actives to hair follicles and sweat glands (Gelfuso et al. 2013). Skin appendages constitute a significant pathway for drugs transported both by electro-osmosis and electrorepulsion which, a priori, could favour active accumulation in these structures (Bath et al. 2000b, a; Scott et al. 1995; Turner and Guy 1997, 1998). Iontophoresis is also useful for providing a faster response, as shown by the earlier onset of local anaesthesia observed with lidocaine iontophoresis (Galinkin et al. 2002; Kearns et al. 2003; Rose et al. 2002; Squire et al. 2000) as compared to passive administration.
Finally, it has been shown that iontophoretic transport, at least the electrorepulsion contribution, is less dependent on the skin properties than passive diffusion. This is because transport numbers are primarily determined by the concentration and mobility of ions present in the system (Phipps and Gyory 1992; Berner et al. 1988; Mudry et al. 2006b, 2007). For example, the interspecies differences observed for the iontophoretic fluxes of some compounds were smaller than those observed in their passive diffusion; this feature helps data extrapolation (Mudry et al. 2006a; Phipps et al. 1989; Padmanabhan et al. 1990). Further, the iontophoretic flux of lidocaine HCl was practically the same across intact and tape-stripped skin (Sekkat et al. 2004). A priori, this data seems to support iontophoresis as a better (less variable) method to deliver drugs across barrier-deficient skin such as that of premature neonates, but caution should be exerted. At the end, the overall transdermal transport of a drug is the sum of the passive and iontophoretic contributions, and this advantage diminishes for compounds with a significant passive flux as recently reported (Djabri et al. 2012).
Even though iontophoresis enhances significantly the rate and extent of skin absorption of many drugs, it remains a technique to deliver relatively potent actives. Thus, careful consideration should be given to both the dose required and the attainable transdermal fluxes. Indeed, drug transport numbers (or fraction of the total charge transported by a specific ion during iontophoresis) are limited by endogenous ion competition and will be less than 0.4 for most therapeutic entities (Phipps and Gyory 1992; Mudry et al. 2006a; b, 2007). For example, the maximum transport number (i.e. measured in the absence of competing co-ions) for lithium is ~0.54, with the remaining charge being transported by endogenous, subdermal chloride ions. Lithium, a small inorganic cation, is very efficiently transported by iontophoresis, but this will not be the case for most therapeutic entities which typically have much smaller transport numbers. The maximum transport number for a series of cations (Mudry et al. 2007) decreased rapidly with molecular weight, and in practical terms, drugs with maximum transport numbers closer to those of lidocaine (~0.16) are considered as excellent candidates for iontophoresis. Therefore, the efficiency of an iontophoretic delivery, as expressed in moles of drug transported with respect to total charge delivered, is relatively low. For instance, lidocaine will transport a maximum 16 % of the total charge delivered to the iontophoretic circuit, with the remaining 84 % being transported by endogenous chloride mostly. Addition of other competing co-ions (stabilizers, buffers, salt bridges) to the donor vehicle will further decrease the efficiency of iontophoretic delivery (Mudry et al. 2006b; Phipps and Gyory 1992).
It follows that measurement of the maximum transport number achievable for a drug, even if the experimental conditions required would not be applicable in practice, is a fast method to predict the feasibility of an iontophoretic transdermal administration. Provided that the average concentration required in plasma (C ss) and the clearance of the drug (Cl) are known, Eq. 6.1 can be used to roughly estimate the intensity of current required for providing the drug input (J iontophoresis) which will match the elimination rate of the drug at the required concentration and will maintain a steady-state plasma concentration:
where t #.max.drug; z drug and F are the maximum transport number achievable for the drug, the valence of the drug and the Faraday constant, respectively. Alternatively, the input rate can be approximated from the daily dose. Please note that experimentally measured maximum transport numbers will include both the electromigration and electro-osmotic contributions for a charged drug and are more correctly termed transference numbers. In the case of an uncharged drug, only transported by electro-osmosis, Eq. 6.2 can be modified to:
where J solvent is the convective solvent flux and C donor is the drug concentration in the donor electrode chamber. Please note that J solvent is normally proportional to the current intensity (Delgado-Charro and Guy 2001b).
Once the intensity of current required is known, the current density (CD) resulting from such an administration can be determined using Eq. 6.3:
The maximum area per electrode will be that considered acceptable for the specific iontophoretic application and body site envisaged. Note that the total iontophoretic patch area would be, at least, double this value. Traditionally, the value of 0.4–0.5 mA.cm−2 has been considered as an upper limit for current density above in which sensations of tickling, warmth or discomfort experienced by the user become less tolerable (Ledger 1992). Figure 6.1 shows some simulations illustrating the discussion above.
Feasibility simulations in iontophoresis. Left panel: molar flux (μmol.h−1) achievable for model monovalent drugs for different transport numbers and intensity of current applied. Right panel: area per electrode (dashed lines, open symbols) and current intensity (solid lines, filled circles) required to deliver 10 mg of hypothetical monovalent drugs of 150 (squares), 300 (circles) and 450 (triangles) molecular weight in 24 h. The current density was fixed at 0.4 mA.cm−2 (The data was generated using Faraday’s law (Eq. 6.1))
The previous method allows a quick estimation of feasibility, that is, whether an iontophoretic administration merits further development. However, this method is primarily a steady-state calculation. Subsequent stages of the feasibility assessment should look into the kinetics of the process and the fact that iontophoretic fluxes require some time to reach steady values. The length of this time varies for different drugs and seems to be related to both the physicochemical properties of the drug and the presence of endogenous ions within the skin (Phipps and Gyory 1992). Thus, a more realistic approach should consider the magnitude of fluxes achieved during the length of current passage envisaged. Some of these concerns have been addressed by Nugroho et al. (2004).
Finally, the dose delivered in an iontophoretic administration can be estimated through Eq. 6.4:
Thus, at least theoretically, the same dose can be delivered by judicious manipulation of the application time and the iontophoretic fluxes (the latter being typically modified by changing the intensity of current applied for the same iontophoretic vehicle). This dosing flexibility is indeed an advantage of iontophoresis over other forms of controlled drug delivery. All the same, the concept of bioavailability encompasses both the extent and rate of drug absorption, and therefore, to achieve therapeutic efficacy, both the amount of drug absorbed and the rate with which it is absorbed must be appropriate to the pharmacodynamics and pharmacological properties of the drug.
2 Iontophoresis Drug Delivery for Local and Topical Therapies
The most widespread applications of iontophoresis are the treatment of palmoplantar hyperhidrosis and the diagnosis of cystic fibrosis. Other popular applications are the iontophoretic delivery of lidocaine, acyclovir and dexamethasone phosphate.
The treatment of palmoplantar hyperhidrosis is one of the oldest applications of iontophoresis (Kreyden 2004). Hyperhidrosis, an excessive rate of sweat secretion from the eccrine glands, is a disabling condition that affects both children and adults. Iontophoresis is one of the most effective, safest and inexpensive treatment options available. Although it has been applied for a long time in the treatment of this pathology, the mechanism of action of iontophoresis is unknown. Different options have been considered in the treatment of hyperhidrosis with iontophoresis, including the application of tap water, saline, botulinum toxin or anticholinergics. Anodal iontophoresis is more efficient than cathodal iontophoresis, and tap water is more effective than saline (Sato et al. 1993). Iontophoresis with anticholinergics is more effective than tap water iontophoresis, but may induce systemic side effects (Dolianitis et al. 2004). The administration of botulinum toxin by iontophoresis (the dose was administered in one 30-min session with a current intensity of 3 mA) has shown to reduce sweating more quickly and for a longer period than saline, without side effects (Davarian et al. 2008). Potentially, the iontophoretic administration of this toxin would avoid the painful injections required to this day even though the duration of effect observed is shorter. The apparent success in delivering this large toxin could be related to the high density of sweat glands in the palms and the very high potency of this active.
Iontophoresis is an integral part of the method used to diagnose cystic fibrosis. The disease results from a mutation in the gene encoding the cystic fibrosis transmembrane conductance regulator. Among other functional problems, this causes extensive dysfunction of the exocrine glands which constitutes the basis for the diagnosis of cystic fibrosis, basically a sweat test. First, pilocarpine is iontophoretically (5 min × 2.5–3.0 mA) delivered to a small area of the arm or leg to stimulate sweating. The sweat is then collected and analysed for volume and chloride content (Beauchamp and Lands 2005).
Delivery of topical anaesthetics prior to dermal surgery remains one of the most common applications of iontophoresis. The iontophoresis of hydrochloride salts of anaesthetics of the amide type, such as lidocaine (Maloney et al. 1992), bupivacaine, etidocaine, mepivacaine, prilocaine and ropivacaine, has been frequently reported (Brouneus et al. 2001). Several studies demonstrated that lidocaine iontophoresis and the eutectic mixture of lidocaine and prilocaine (EMLA®, AstraZeneca PLC, UK) were of a similar efficacy in providing the analgesia necessary for cannulation and CO2 laser surgery of superficial skin lesions (Phahonthep et al. 2004; Galinkin et al. 2002). Purpose designed, disposable electrodes (Numby Stuff® from Iomed Clinical Systems, Salt Lake City, USA) containing lidocaine HCl and epinephrine were the first available to be used in combination with a Phoresor power supply. The Phoresor II Auto PM850 is a programmable, direct current delivery device which can apply up to 4 mA and uses a 9-volt battery. Later on, the LidoSite® Topical System (lidocaine topical anaesthetic system) was developed by Vyteris, Inc. (Fair Lawn, NJ), and approved by the US FDA in 2004. The LidoSite® was a small, easy-to-use, preprogrammed iontophoretic lidocaine delivery system composed of a drug-filled patch connected to a controller (Kalia et al. 2004). Several trials have investigated the safety and effectiveness of lidocaine iontophoresis and compared it with either placebo or with EMLA cream in adults and children (Galinkin et al. 2002; Kearns et al. 2003; Rose et al. 2002; Squire et al. 2000). Briefly, the results indicate that both techniques provide similar pain relief; however, the application time is greatly reduced for iontophoresis (5–15 min) in comparison to the 50–90 min required by the EMLA cream. Therefore, the faster delivery of lidocaine via iontophoresis provides a faster onset of analgesia. Regrettably, the LidoSite® System was later discontinued. Despite this, lidocaine iontophoresis still attracts interest and is object of ongoing clinical research according to ClinicalTrials.gov. For example, clinical trials sponsored by Dharma Therapeutics, Inc., USA, currently look into the same application (lidocaine/epinephrine to provide local anaesthesia for venepuncture), whereas other trials sponsored by Acclarent, Inc., USA, investigate the anaesthetic effect of lidocaine/epinephrine iontophoretically delivered to the external auditory apparatus to treat otitis. This new application can be implemented using the Tula® Iontophoresis System also by Acclarent, Inc., USA, which is object of another clinical trial. Unfortunately, no results have been posted in any case.
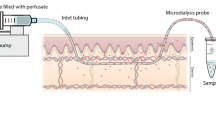
The efficacy of topical creams and ointments in the treatment of herpes labialis remains a controversial issue, more precisely their relative benefit with respect to spontaneous healing. This poor outcome has been attributed to the low penetration of the drug across intact skin and its insufficient delivery to the basal epidermis, the targeted site of infection. The possibility of enhancing the skin permeability of acyclovir via an electric current was investigated in several occasions. Morrel et al. demonstrated that a single dose of a conventional formulation of acyclovir (ACV) via iontophoresis was a convenient and effective treatment for cold sores (Morrel et al. 2006). ACV is an ampholyte drug with two pKa values (2.27 and 9.25); thus, it is primarily cationic below pH 2, neutral between pH 3 and 8.5 and anionic at pH greater 9.5. Thus, depending on the pH of the vehicle, ionized ACV can be delivered both by anodal or cathodal iontophoresis and neutral ACV by electro-osmotic flow (Padula et al. 2005). Shukla et al. (2009) tested the iontophoretic delivery of ACV from different formulations (neutral creams and pH 11 gels); according to these authors, only the neutral drug solubilized in the water phase of the creams was available for transport. On the other hand, delivery of the negatively charged ACV from the pH 11 gels increased the dermis exposure to the drug. For example, the AUC0–60 (area under the curve ACV interstitial fluid concentration versus time) measured by microdialysis were 8.8 ± 1.5 mg.min.L−1, 174 ± 078 mg.min.L−1 and 13.3 ± 4.8 mg.min.L−1 for the neutral cream, pH 11 gel iontophoresis and pH 11 gel passive, respectively. Apparently, the high pH did not cause skin irritation. At the time of this review, two phase II clinical trials sponsored by Transport Pharmaceuticals, Inc. (USA), on the effectiveness of iontophoretic delivery of ACV to treat herpes labialis are listed in ClinicalTrials.gov, unfortunately with no results posted yet.
The efficacy of iontophoresis to deliver other antiviral agents used against herpes labialis has also been reported. Iontophoresis was used to deliver the antiviral drug idoxuridine to 14 recurrent herpes labialis lesions in a clinical trial involving six patients. Results were characterized by immediate relief of discomfort and swelling, rapid appearance and coalescence of vesicles, minimal or no spread of the lesions and accelerated healing with minimal or no scab (Gangarosa et al. 1979). Gangarosa et al. (1986) compared iontophoresis of vidarabine monophosphate (ara-AMP) and acyclovir for efficacy against herpes orolabialis. Patients with vesicular orolabial herpes participated in a double-blind, placebo-controlled clinical study comparing iontophoresis of vidarabine monophosphate (ara-AMP, n = 9), of acyclovir (ACV, n = 9) and of NaCl (placebo group, n = 9). Ara-AMP-treated lesions yielded lower titres of virus after 24 h compared with lesions treated with NaCl or ACV. Ara-AMP significantly decreased the duration of shedding of virus compared to the placebo group (Gangarosa et al. 1986).
The iontophoretic administration of dexamethasone sodium phosphate (DP) to treat local pain and soft tissue inflammation in sports medicine remains a popular application. The disodium salt DP is water-soluble and, at a physiological pH, is present mainly in its dianionic form (pKa, 1.9 and 6.4). DP is relatively well delivered to the skin by cathodal iontophoresis, and, in this case, the challenge is to ensure that a sufficient DP reaches the target tissue beneath the skin despite of the drug’s systemic clearance. Iontophoretic treatment of various musculoskeletal problems with DP has been the subject of clinical studies employing a great variety of protocols, many of which have reported beneficial effects (Nirschl et al. 2003; Li et al. 1996), though improvement in the patient’s condition has not been always observed (Reid et al. 1994; Runeson and Haker 2002). Again, it has been demonstrated that, to achieve optimal iontophoretic delivery, DP must be delivered from the cathode and formulated rationally, excluding mobile competing co-ions, such as chloride ions (Fig. 6.2) (Sylvestre et al. 2008a,b). When properly implemented, iontophoresis enhances significantly the delivery of DP; for example, the combined amounts of dexamethasone sodium phosphate and dexamethasone in the treated SC (0.78 cm2) were estimated via tape stripping to be 9.9 ± 3.3 nanomoles and 0.69 ± 0.29 nanomoles after 3 h of iontophoresis and 3 h of passive diffusion, respectively (Sylvestre et al. 2008a).
Donor composition, primarily the presence of competing co-ions, has a significant impact on the cathodal iontophoretic flux of dexamethasone phosphate (DP). The formulations tested were A (1:2 injectable DP 0.4 %, Faulding (Mayne Pharma PLC, UK) + lidocaine 4 % (AstraZeneca, UK)), B (injectable DP 0.4 % (American Regent, USA)), C (injectable DP 0.4 %, Faulding), D (DP 0.4 % in potassium citrate), E (DP 0.4 % in 0.9 % NaCl), F (injectable DP 0.5 %, Organon, UK) and G (DP 0.4 % in water). The current intensity was 0.3 mA (0.38 mA.cm−2). Numbers on top of the columns indicate the average transport number of the drug expressed as percentage (Data taken and redrawn from Sylvestre et al. 2008b)
The topical iontophoresis of non-steroidal anti-inflammatory drugs (NSAIDs) is attractive in that this alternative, local delivery method would reduce the risk of GI-related side effects commonly encountered after oral administration. The cathodal iontophoresis (0.625 mA.cm−2 for 90 min) of a series of NSAIDs (salicylic acid, ketoprofen, naproxen and indomethacin) suggested an important effect of the drug lipophilicity on their in vivo delivery in rats (Tashiro et al. 2001). NSAID skin concentrations were higher for the most lipophilic drugs, whereas the cutaneous plasma concentrations decreased for the most lipophilic actives. According to the authors, the rate of transfer of NSAIDs from the skin to the cutaneous vein decreased with increasing lipophilicity. These results underline the key role which drug partitioning between the stratum corneum (SC) and the viable epidermis may have in determining the local bioavailability of drugs (Tashiro et al. 2001).
A double-blind study compared the efficacy and tolerability of pirprofen and lysine soluble aspirin (Flectadol®, Maggioni-Winthrop S.p.A., Milan, Italy) administered by iontophoresis to 80 patients with various painful rheumatic diseases. The treatment lasted 2 weeks and consisted of five administrations a week, each lasting 20 min. After five administrations, patients showed significant improvement in pain at rest, and on movement, no significant differences were observed between the pirprofen and aspirin groups. The final outcome was described as excellent or good for ~75 % of the treated patients with a satisfactory functional improvement being reported for ~80 % (Garagiola et al. 1988).
A commercially available gel containing piroxicam was used to administer this drug both passively and with iontophoresis to human volunteers (Curdy et al. 2001). The total amount of drug recovered from the SC via tape stripping was significantly higher post-iontophoresis (48.6 ± 18.8 μg.cm−2) than after passive diffusion (5.4 ± 2.0 μg.cm−2).
The iontophoresis of ketoprofen was efficacious and safe in the treatment of acute osteoarthritic diseases also in high-risk patients (Salli 1993). Three hundred and twelve patients with osteoarthritic diseases were admitted to this multicentre clinical trial and received ketoprofen by iontophoresis twice a day for ten consecutive days. Pain relief was almost complete in 94.6 % of the patients, improvement of active motility in 83.6 %, disappearance of swelling in more than half of the patients and functional improvement in about all the cases. Two allergic skin reactions of a mild degree (in 0.6 % of patients) were registered.
Ketorolac has also been successfully delivered by iontophoresis to human volunteers. The drug was delivered using silver electrodes with a current of 2 mA for five treatment sessions for 20 min every day (Saggini et al. 1996).
A double-blind randomized study compared ionization with diclofenac sodium and ionization with saline solution in two groups of patients with scapulohumeral periarthritis or elbow epicondylitis. Both groups were treated with 20 ionization sessions each lasting 30 min during a 1-month period. There was a significantly greater improvement in pain at rest, pain on pressure, pain on movement and joint swelling in the 11 patients treated with diclofenac sodium compared with the 13 placebo-treated patients, but no significant differences between the two treatments as regards functional impairment were observed (Vecchini and Grossi 1984). However, other studies have reported side effects including a systemic adverse reaction (Macchia et al. 2004) and allergic contact dermatitis (Foti et al. 2004).
The iontophoretic administration of antineoplastic agents to treat skin cancer has been proposed to avoid the scarring associated with surgery, the long-term complications of radiation therapy and the adverse effects associated with the systemic administration of these actives. Chang et al. (1993) investigated whether iontophoretic delivery of cisplatin could be used to treat basal and squamous cell carcinomas in a group of patients who refused surgery. Cisplatin was delivered from the anode together with the vasoconstrictor epinephrine hydrochloride; the dose of drug and current applied depended on the size of the lesion. Eleven of the 15 patients showed either a partial reduction in the lesion area or a complete response. There were no incidences of systemic side effects (nausea or vomiting) although a minor burning sensation at the cathode was reported. The authors concluded that small lesions responded better and suggested a treatment schedule involving a daily iontophoretic therapy of 20–30 min for 5 days followed by a 2-week recovery period.
Smith et al. (1992) investigated the iontophoresis of vinblastine sulphate as a possible treatment for the cutaneous lesions associated with Kaposi sarcoma in human immunodeficiency virus-positive patients. The first step involved the iontophoretic delivery (4 mA, 10 min) of both lidocaine and epinephrine; after which vinblastine sulphate was delivered (4 mA, 10–90 min) on the same skin site. A non-HIV-infected group showed signs of local erythema which cleared up within 2 weeks. However, less inflammation was observed in the HIV-1 patients treated over a period of 6 months. This difference could be explained by the immunosuppression at advanced stages of the illness experienced by the patient group. All patients showed a significant clearing of the lesions.
Cathodal iontophoresis enhanced the transdermal flux of methotrexate as compared to passive diffusion (Alvarez-Figueroa et al. 2001); it was not clear whether therapeutic local concentrations could be achieved given that target values are unknown. A topical dosage form of this drug for the treatment of psoriasis would be of great interest, as the systemic administration use of this drug results in numerous side effects.
Iontophoretic delivery of 5-fluorouracil (5-FU) appears to be a safe, effective and well-tolerated therapy for Bowen’s disease. Twenty-six patients with biopsy-proven Bowen’s disease received eight 5-FU iontophoretic treatments in 4 weeks (Welch et al. 1997). A local excision procedure took place 3 months after the last treatment, and the specimens were step-sectioned and evaluated for any histologic evidence of bowenoid changes. Only one of the 26 patients showed histologic evidence of Bowen’s disease 3 months after treatment. A case report described a cutaneous allergic reaction in one patient after 5-FU iontophoretic treatment (Anderson et al. 1997).
Photodynamic therapy (PDT) is now considered as a valuable alternative treatment of cancer. PDT involves the administration of a tumour-localizing photosensitizer or photosensitizer prodrug (5-aminolevulinic acid [ALA], a precursor in the heme biosynthetic pathway) and the subsequent activation of the photosensitizer by light (Peng et al. 1997). Using iontophoresis, a rapid and quantifiable system for topical ALA delivery, with measurement of subsequent protoporphyrin IX (PpIX) fluorescence and phototoxicity, has been reported (Rhodes et al. 1997). ALA was iontophoretically delivered from a 2 % solution into the upper inner arm skin of 13 healthy volunteers with the delivery being sufficient to induce tumour necrosis. Iontophoretic transport of ALA across human SC was studied quantitatively in vitro by Bodde et al. (2002). The results showed that the amount of ALA that passively diffuses through the SC in several hours, leading to therapeutic levels of PpIX in the epidermis, can be delivered by iontophoresis in 10 min or less. However, because the formation of sufficient PpIX also requires several hours and also because the SC overlying skin lesions such as basal cell carcinoma (BCC) is not intact, the clinical benefit of topical ALA delivery by iontophoresis for PDT of BCC is yet to be established.
Finally, the delivery of calcitonin gene-related peptide (CGRP) and vasoactive intestinal polypeptide (VIP) has shown potential to treat venous stasis ulcers (Gherardini et al. 1998). The anodal electrodes (40 cm2) contained drug reservoirs filled with 1 mL of a 3-nM CGRP or of a 0.3-μM VIP; the cathodal electrode reservoirs contained sodium phosphate buffer. This iontophoretic set-up was applied to intact skin in the proximity of the ulcer in 66 patients, and pulsed electric current was delivered for 20 min. The clinical results suggested that both peptides’ delivery was enhanced and that the electric current passage close to the ulcer area had a positive influence on the healing process.
3 Iontophoretic Transdermal Drug Delivery
Until very recently, only the fentanyl iontophoretic system (Ionsys®, Alza Corporation, USA) had been marketed as a transdermal drug delivery system. In January 2013, the sumatriptan iontophoretic delivery system, ZecuityTM by NuPathe Inc., USA, was approved by the FDA for the acute treatment of migraine.
The Ionsys® System was indicated for the short-term management of acute postoperative pain in adult patients requiring opioid analgesia during hospitalization. Fentanyl physicochemical and pharmacological properties together with its pharmacokinetics – short half-life and high first-pass effect – make it an ideal candidate for transdermal administration (Chelly et al. 2004). Passive transdermal fentanyl patches for the treatment of chronic pain have been marketed for nearly 20 years but cannot provide the rapid bolus of drug input required to treat acute pain. The feasibility of fentanyl iontophoresis was demonstrated in vitro and in vivo (see Fig. 6.3) (Thysman and Preat 1993; Ashburn et al. 1995) and led to the development of the Ionsys® System (using E-TRANS® electrotransport technology, Alza Corporation, USA) – a preprogrammed, self-contained, on-demand drug delivery system activated by the patient which can deliver 80 doses of 40 μg of fentanyl in a 24-h period. The Ionsys® was designed to operate for 24 h after the first activation and allowed 6 doses per hour up to a maximum of 80 doses, after which the system shut off. Subsequently, a new transdermal system is required if the fentanyl administration is to be continued. The transdermal system used a 10-min transdermal infusion for each 40-μg dose (Gupta et al. 1999; Gupta et al. 1998). Clinical studies showed that the Ionsys® System was well tolerated by patients suffering postoperative pain and was equivalent to a standard intravenous morphine pump (Viscusi et al. 2006; Minkowitz et al. 2007; Ahmad et al. 2007; Hartrick et al. 2006). Ionsys was marketed in Europe by Janssen-Cilag, an affiliate of Alza; however, a defect involving corrosion of a component within the system was found by Janssen-Cilag in 2008. There had been neither complains linked to the defect nor evidence of patient harm; nevertheless the device was recalled as a precautionary measure. Because the root cause of the defect was not identified, the marketing authorization was finally suspended by the European Medicines Agency (EMA) (EMA 2008). The current marketing status of the device at the Food and Drug Administration (FDA) website is also discontinued. In January 2013, The Medicines Company (Parsippany, NJ, USA) acquired Incline Therapeutics, Inc., which had previously acquired the rights to Ionsys from Alza, with intention to resubmit the product marketing approval in the USA and Europe.
Current intensity controlled the extent of fentanyl absorbed as shown by changes in AUC (area under the curve plasma concentration vs. time, filled diamonds), C max (maximum plasma concentration, filled squares) and the amount of fentanyl absorbed per 10-min dose, A abs (open circles), but did not modified t max (time to reach C max, filled triangles). Fentanyl HCl was delivered using a patient-controlled transdermal system, 16–35 volunteers received each treatment (Data taken and redrawn from Sathyan et al. 2005)
Other opioid analgesics are good candidates for iontophoresis from both physicochemical and pharmacological standpoints. A prospective, randomized, single-blind study investigated the effectiveness of iontophoretically delivered morphine hydrochloride to control postoperative pain in 38 patients who underwent total knee or hip replacement. Postoperative pain was initially controlled with IV meperidine and, thereafter, with a patient-controlled analgesia (PCA) device also administering meperidine. The following morning, either morphine hydrochloride or lactate ringer’s solutions (control) were delivered iontophoretically for 6 h. Because of the red wheal and flare observed under the anodal compartment, apparently due to the local histamine release provoked by morphine, the investigators were aware of the patients who received morphine, and only the patients were blinded. PCA analgesia remained available to patients during this period and for 12 h after iontophoresis. The morphine group usesd significantly less PCA meperidine both during iontophoresis and for the following 12-h post-iontophoretic treatment as compared to the lactate group (Ashburn et al. 1992).
The iontophoretic delivery of apomorphine for the treatment of idiopathic Parkinson’s disease was evaluated in human subjects. Although some encouraging results were obtained, they will require further confirmation, especially as the skin required pretreatment with surfactants (Bodde et al. 1998; Li et al. 2005) to further improve delivery of the drug. In vivo studies in rats suggest that therapeutic levels of ropinirole hydrochloride could be achieved via iontophoresis (Luzardo-Alvarez et al. 2003). However, the results will need further confirmation in humans and after formulation of a suitable electrode patch.
The iontophoretic delivery of tacrine, the first centrally acting cholinesterase inhibitor approved for the treatment of Alzheimer’s disease, in healthy adult volunteers was investigated in two occasions. One study used Iogel® silver/silver chloride electrodes (Chattanooga Group, Inc., USA), whereas the second one employed a novel two-compartment electrode system in which the drug reservoir was separated from the electrode by a membrane; this arrangement maximized the drug transport efficiency by avoiding competition with co-ions. A 0.4-mA.cm−2 current was applied for 3 h using patches with an active surface area of 10 cm2. Apparently, both types of electrodes would be able to provide tacrine blood levels similar to those observed following oral administration of the drugs (Kankkunen et al. 2002).
The treatment of migraine also represents an interesting application for iontophoresis. Several in vitro (Femenia-Font et al. 2005) and in vivo studies carried out with sumatriptan in human volunteers (Siegel et al. 2007) suggested that iontophoresis could provide adequate drug plasma levels for migraine treatment. Similar results have been obtained with zolmitriptan (Patel et al. 2009). A phase III randomized, double-blind, placebo-controlled trial evaluated the efficacy and tolerability of a sumatriptan iontophoretic transdermal system for the acute treatment of migraine in 469 patients. Patients on sumatriptan iontophoresis experienced less nausea, photophobia and phonophobia than those on placebo iontophoresis; further they had a rapid and sustained headache pain relief and used less rescue medication than the placebo group. About 50 and 44 % of patients treated with the sumatriptan iontophoresis and placebo iontophoresis experienced treatment-related adverse reactions, most of which were transient and mild-to-moderate application side effects. Therefore, sumatriptan iontophoresis was effective and well tolerated and particularly advantageous in migraine patients with nausea (Goldstein et al. 2012). In January 2013, the FDA (Drugs@FDA 2013) cleared the Zecuity iontophoretic transdermal delivery system by NuPathe Inc., USA, which delivers 6.5 mg of sumatriptan over 4 h.
The following paragraphs summarize the key progress in peptide and protein delivery by iontophoresis. Comprehensive and recent reviews on this topic field are available elsewhere (Gratieri et al. 2011). Early work demonstrated that iontophoresis could deliver peptides systemically, more specifically the tripeptide, threonine-lysine-proline (Thr-Lys-Pro) after topical application onto hairless rat skin (Green et al. 1992). In vivo results were consistent with the measured flux of the peptide in vitro. Iontophoretic pretreatment of rats resulted in enhanced delivery of the peptide subsequently applied passively. No important changes in skin morphology were observed following the current passage.
Currently, there is wide evidence supporting that iontophoresis can successfully deliver peptides and proteins in their active form. However, the therapeutic and commercial usefulness of the technique will depend on the dose and input profiles required for each application and on which alternative routes of delivery are available for the peptide considered. An increase in delivery rates of the somatostatin analogue, octreotide, was obtained in vivo in rabbits when mild current densities (50–150 μA.cm−2) were applied (Lau et al. 1994). Peptide plasma levels increased proportionally with the intensity of the current applied and drug input declined quickly upon current cessation. Several iontophoretical studies have investigated calcitonin, a 32-amino acid peptide with a molecular weight of ~3500 Da which, under physiological conditions, is positively charged. For example, human calcitonin was delivered into hairless rats, although lowering of serum calcium was not linearly dependent upon either the current density or time of current application (Thysman et al. 1994). The possibility of delivering calcitonin topically to the dentin in order to treat invasive cervical resorption (Kitchens et al. 2007) and systemically to treat osteoporosis and Paget’s disease has been reported as well. Nevertheless, no studies have been carried so far in humans. Salmon calcitonin, which is more potent than the human form, has been iontophoretically delivered in animal skin models with the blood levels attained being comparable to those achieved by intravenous infusion (Santi et al. 1997; Chaturvedula et al. 2005). Iontophoresis of LHRH has been investigated in vivo in pigs (Heit et al. 1993). Elevated LHRH concentrations were measured in the blood and concomitant increases in LH (luteinizing hormone), and FSH (follicle-stimulating hormone) levels were observed, demonstrating that the hormone had been delivered as a pharmacologically active species. Further, the circulating levels of LHRH fell rapidly upon the termination of iontophoresis. A larger peptide, growth hormone-releasing factor, GRF (1–44) (MW 5040), was delivered by iontophoresis into hairless guinea pigs, resulting in steady-state plasma levels of ~0.2 ng.mL−1 which were associated to a ~3.16-μg.h−1 transdermal flux (Kumar et al. 1992).
The iontophoretic delivery of the LHRH analogue leuprolide has been investigated in humans (Meyer et al. 1990; Lu et al. 1993). The application of a low current intensity (0.2 mA) over 70 cm2 resulted in LH levels comparable to those obtained after subcutaneous injection (Meyer et al. 1990). These results are remarkable, considering the low current density (~3.1 μA.cm−2) employed. Only 15 % of the subjects reported a tingling sensation during current passage, and 46 % observed at the electrode sites some erythema which resolved quickly after current termination. The effect of formulation variables on the iontophoretic delivery of leuprolide was also studied in humans (Lu et al. 1993). The lowest leuprolide concentration provided the highest transport. Vehicles formulated with different ionic strengths were evaluated. Systemic leuprolide levels differed, but there was little effect on the LH and testosterone concentration. This observation was attributed to differences in the pharmacological response of the subjects included in the study.
Despite the many in vitro and in vivo studies performed on peptide iontophoresis (Kochhar and Imanidis 2004; Nair and Panchagnula 2004; Chaturvedula et al. 2005), the prediction of iontophoretic fluxes and blood levels attainable for a given compound remains difficult. Computational studies of 3D quantitative structure-permeation relationships suggest that iontophoresis is favoured by peptide hydrophilicity and hindered by voluminous, localized hydrophobicity (Schuetz et al. 2005, 2006). An especially interesting situation is presented when the bulky lipophilic moiety is directly adjacent to a positively charged residue as it is the case, for example, of nafarelin and leuprolide. It has been demonstrated that these two peptides reduce the magnitude of the electro-osmotic solvent flow typically observed in the anode-to-cathode direction at physiological pH and, in doing so, dramatically affect their own iontophoretic transport (Schuetz et al. 2006; Lau et al. 1994).
Insulin has attracted significant attention from researchers in the field of iontophoresis. It is generally accepted that hexameric insulin is too large for being delivered via iontophoresis; however, the flux of monomeric human insulin (mean MW ~6000 Da, negatively charged) was increased significantly by current application as compared to passive diffusion. Nevertheless, the iontophoretic administration of insulin is hindered by numerous challenges including the instability of the peptide. A considerable number of in vitro studies have investigated the effect of iontophoretic parameters on insulin delivery and have demonstrated the physiological effect of iontophoretically delivered insulin on blood glucose levels in different small animal models, particularly mice, rats and rabbits (Pillai et al. 2003, 2004a; b; Pillai and Panchagnula 2003a; b; Kari 1986; Liu et al. 1988; Rastogi and Singh 2005; Langkjaer et al. 1998). More recently, different approaches, combining iontophoresis with other techniques such as chemical enhancers, ultrasound, liposomes or microneedles, have been tested (Singh et al. 2012). While some of these studies have successfully delivered insulin in these small animal models, a delivery method which involves compromising the SC may not be appropriate for chronic use in humans. Further, it is uncertain whether the results can be extrapolated to humans, who will require significantly greater doses of the hormone to be delivered and provide the pharmacologic effect.
4 Iontophoresis Applications in Ocular Drug Delivery
The treatment of ocular diseases, particularly those afflicting the anterior and posterior camera of the eye, represents an important challenge. Drug delivery by topical formulations is typically ineffective due to both precorneal obstacles (drainage, blinking, tear film and induced lacrimation) and anatomical barriers (lipophilic corneal epithelium, hydrophilic corneal and scleral stroma and tight junctions) presented by the eye. It has been suggested that ocular iontophoresis may overcome some of the above-mentioned challenges, and therefore, the technique has been tested for the delivery of antibacterials, antivirals, antifungals, steroids, antimetabolites and genes.
Ocular iontophoresis can be classified into transcorneal and transscleral iontophoresis, according to treatment location. Transcorneal iontophoresis aims to deliver the drug to the anterior segment of the eye (cornea, aqueous humour, ciliary body, iris and lens) for the potential treatment of keratitis, glaucoma, dry eyes, corneal ulcers and ocular inflammation (Eljarrat-Binstock and Domb 2006).
Transscleral iontophoresis delivers the drug directly into the vitreous and retina. For this purpose, the iontophoretic device is placed on the conjunctiva, over the pars plana area, to avoid potential damage to the retina by current passage. Transscleral iontophoresis represents a potential alternative to intravitreal injections and to systemic administration in the treatment of endophthalmitis, uveitis, retinitis, optic nerve atrophy, paediatric retinoblastoma and age-related macular degeneration (Eljarrat-Binstock and Domb 2006).
Like the skin, the sclera has an isoelectric point between 3.5 and 4 and therefore a net negative charge at physiological pH; thus, transport by electro-osmosis will be possible depending on the pH. The key parameters controlling the iontophoretic transport of low molecular weight compounds are very similar to those controlling transdermal iontophoresis, i.e. the current intensity, duration of the application and composition of the iontophoretic vehicle (buffers and competing ions) (Gungor et al. 2010). On the other hand, the iontophoretic flux of some high molecular weight cationic compounds was not proportional to their concentration in the donor (Gungor et al. 2010). Similar observations were made in an in vitro study which delivered a marker, a hydrophilic 40-kDa dextran, across the isolated porcine sclera and across the trilayer sclera-choroid-Bruch’s membrane. It was observed that drug depots built up inside the sclera during in vitro iontophoresis and that this reservoir provides for a sustained transscleral flux for up to 3 h after iontophoresis (Pescina et al. 2011) (see Fig. 6.4).
Concentration of a dextran of 40 kDa (FD-40) in the choroid, retina and vitreous after its application onto excised eye bulb (no dynamic barrier). *Significantly different to the passive 30-min application (Redrawn from Pescina et al. 2011)
Although generally considered as a safe technique if properly implemented, some complications including epithelial oedema, decrease in endothelial cell inflammatory infiltration and burns can occur depending on the site of application, current density and duration. Because the corneal tissue and sclera present important differences, the passage of current affects them differently. For example, damage to the cornea surface affects vision, whereas the sclera is very sensitive to pain and hypoxia. In the case of humans, a transscleral exposure to 0–3.0 mA for 20 min and to 1.5 mA for 40 min was well tolerated, while passage of 4.0 mA for 20 min produced a burning sensation in half of the subjects treated (Parkinson et al. 2003).
Several studies have been conducted to demonstrate that iontophoresis can efficiently enhance the passage of various molecules across the eye membranes. Most of these studies have been performed in vivo in rabbits, while fewer in vitro studies and human trial are being reported.
The transcorneal and transscleral penetration of dexamethasone after short-term iontophoresis was investigated in rabbits, using drug-loaded disposable HEMA hydrogel sponges and a portable iontophoretic device. The drug levels measured in the cornea after a single transcorneal iontophoresis (1 mA for 1 min) were up to 30-fold higher than those obtained after repeated eye drop instillation. Further, high drug concentrations were measured in the retina and sclera 4 h post transscleral iontophoresis (Eljarrat-Binstock et al. 2005).
Antibiotics such as gentamicin, ciprofloxacin and vancomycin have been delivered with iontophoresis either transcorneally or transsclerally. A study in rabbits compared transcorneal iontophoresis (1 min, 1 mA) of gentamicin sulphate with topical eye drops of fortified gentamicin (1.4 %) applied every 5 min for 1 h and with subconjunctival injection of 0.25 mL of a 40-mg.mL-1 gentamicin solution. The peak gentamicin concentrations after a single iontophoresis treatment were 12–15 times higher than those obtained after gentamicin injection or after topical eye drop instillation; moreover, iontophoresis maintained the therapeutic drug levels in the cornea for more than 8 h (Eljarrat-Binstock et al. 2004). In another study, the concentration of ciprofloxacin in the aqueous humour just after 5 min of transcorneal iontophoresis was not significantly higher than in the no-current control. However, 6 and 12 h post-iontophoresis, the concentrations of drug in the aqueous humour were approximately six- and fivefold higher than in the control group, respectively (Vaka et al. 2008).
Methotrexate iontophoresis was investigated in rabbits using drug-loaded hydrogels mounted on a portable iontophoretic device. Following (1.6 and 5 mA.cm−2 for 4 min) the iontophoretic applications, the therapeutic drug levels were maintained for at least 8 h at the sclera and retina and for 2 h at the aqueous humour. Increasing the current density from 1.6 to 5 mA.cm−2 led to a twice-higher concentration at the vitreous and to 8 and 20 times higher concentrations at the retina and sclera, respectively (Eljarrat-Binstock et al. 2007).
The recombinant humanized monoclonal antibody bevacizumab used in ophthalmology for the treatment of neovascularization in diseases such as diabetic retinopathy and age-related macular degeneration is currently administrated by repeated intravitreal injection, which can cause severe complications. Pescina et al. investigated in vitro whether anodal iontophoresis could enhance the transscleral transport of this antibody (Pescina et al. 2010). This preliminary study showed that anodal iontophoresis significantly enhanced (~7.5-fold) bevacizumab transport through isolated human sclera even though the drug is essentially uncharged.
The EyeGate® II Delivery System (Eyegate Pharmaceuticals, Inc., USA) was used to deliver EGP-437 (dexamethasone phosphate, DP, formulated for iontophoresis) in a phase I/II clinical trial in patients with uveitis. After a single iontophoresis treatment, approximately two thirds of the patients reached an anterior chamber cell score of zero within 28 days. Lower doses seemed to be more effective and the treatments were well tolerated. Concurrent pharmacokinetic data indicated a low short-term systemic exposure to dexamethasone after ocular iontophoresis; further, no systemic corticosteroid-mediated effects were observed (Cohen et al. 2012).
The same drug and device were employed in a phase II clinical trial in patients with dry eye. Patients were placed in a controlled adverse environment and randomized into one of the three iontophoresis treatment groups: 7.5 mA-min at 2.5 mA (DP 7.5), 10.5 mA-min at 3.5 mA (DP 10.5) or 10.5 mA-min at 3.5 mA (placebo iontophoresis). Primary efficacy endpoints were corneal staining and ocular discomfort. Secondary endpoints included tear film break-up time, ocular protection index and symptomatology. While the DP 7.5 and DP 10.5 treatment groups showed statistically significant improvements in signs and symptoms of dry eye at various time points, the primary endpoints were not achieved (Patane et al. 2011).
Ocular iontophoresis has been implemented using several devices differing primarily on the design of the drug reservoir. A very common approach, primarily used for transcorneal drug delivery, consists on an eye cup with a drug solution in which the electrode is immersed. The eye cup is placed over the eye and then a slightly negative pressure is created to keep the applicator in its place. A range of size and shape of eye cups adapt to different animal species and humans. The return electrode is placed close to the eye, typically on the forehead. The EyeGate® II Delivery System, originally designed at the Bascom Palmer Eye Institute at the University of Miami and optimized by EyeGate Pharma (Eyegate Pharmaceuticals, Inc., USA), is based on this design and consists of two parts: a reusable battery-powered generator and a disposable applicator which contains the drug.
A second approach in the design of eye iontophoresis devices involves hydrogels in which the drug is dispersed. The hydrogels also modulate drug release, thus facilitating drug handling and minimizing tissue hydration (Eljarrat-Binstock et al. 2010). Two companies, Iomed Inc. (Salt Lake City, Utah, USA) and Aciont Inc. (Salt Lake City, Utah, USA), have developed hydrogel-based applicators, OcuPhor and Visulex. These systems are under investigation for transscleral iontophoresis with different drugs (Kompella et al. 2010).
5 Cosmetic Applications of Iontophoresis
Iontophoresis has become a tool to deliver skin care and cosmetic agents. Nevertheless, the therapeutic and cosmetic fields of application are very different in their regulatory aspects, product research and development methods and markets targeted. Yet there have been some interesting advances in this area which are worth discussing; this concerns primarily the iontophoresis of vitamin C and its derivatives and of botulin toxin and the treatment of scar tissue and acne scars.
As discussed earlier, the iontophoresis of botulinum toxin has aimed primarily to treat palmar hyperhidrosis, and there is no peer-reviewed literature on the use of iontophoresis to deliver botulinum toxin for cosmetic purposes (e.g. treatment of wrinkles).
The iontophoresis of vitamin C, vitamin C derivatives and multivitamins has aimed primarily to treat melasma and to promote collagen regeneration. The magnesium salt of the L-ascorbic acid 2-phosphate (Asc-2-P) is usually preferred due to the poor stability of ascorbic acid. A wide variety of iontophoretic devices, formulations and experimental conditions has been used, and while the information provided is not always complete, it is clear that the delivery conditions were far from optimal in some cases. Some, although incomplete, evidence for efficacy in vivo is provided by colorimetric measurements in the case of melasma and by photography and by self-assessment. Some reports describe studies in which iontophoresis was combined with other procedures (laser, depigmentation creams) or are case reports which complicate data interpretation. Two representative studies in humans are described below.
A group of 29 (24–49 years old) females with melasma participated in a randomized double-blind, within-group comparison, placebo-controlled trial (Huh et al. 2003). One side of the face was treated with iontophoresis of 3.75 % Asc-2-P magnesium salt, and the other side was treated with placebo iontophoresis. The Vitaliont II System (Indiba-Japan Co., Ltd., Japan), employed to apply a 0.5-mA current for 8 min, has a “neutral” handpiece or positive electrode holder by the patient’s hand and a metal negative electrode which was slowly moved along the skin surface. Some of the effects reported (21 % reported a mild sense of electric shock, 7 % itching, 7 % erythema, 3 % burning sensation and 3 % skin dryness) could be due to the method followed to implement iontophoresis. The results, evaluated by photographic assessment, self-assessment and colorimetry measurements of the melasma lesion, allowed the authors to conclude that iontophoresis of Asc-2-P magnesium salt could be a useful treatment for melasma.
Choi et al. (2010) compared the effects of vitamin C either on its own or included in a multivitamin (B1, B2, B6, C, nicotinamide and dexpanthenol) formulation in a randomized, split-face, double-blind trial involving 20 women with melasma. A Vitaliont II device was used to implement 6-min iontophoretic applications, twice a week for 12 weeks, using multivitamins on one side of the face and only vitamin C on the other. Application of sunscreen was allowed on both sides. Self-assessment and colorimetric measurement were used to assess the efficacy of the treatments. While the condition was improved after 12 weeks in both sides, there were no significant differences between the two formulations tested. Side effects such as burning sensations, erythema and itching were reported more frequently for the vitamin C sites. According to the authors, both treatments were equally effective for melasma, but the multivitamin iontophoresis was better tolerated. However, some details concerning the specific experimental method and, crucially, the polarity of the current applied on each site are not completely clear.
The iontophoresis of estriol and, especially, of tretinoin could be useful for the treatment of acne scars. Yet, the experimental methods have not always been optimized for the delivery of these actives, and the role of current passage has not always been clearly isolated. The three studies below are representative examples of this application. Iontophoresis has been employed to deliver estriol and tretinoin for the treatment of atrophic acne scars (Schmidt et al. 1995). The first group (18 women) received estriol iontophoresis using a 0.3 % acid aqueous solution of the active as donor whereas the second group (28 women and men) tretinoin iontophoresis which used a 0.025 % tretinoin gel. Twice weekly iontophoretic treatments (15 min, 3 mA) were applied for 3 months. There are some ambiguities concerning whether the polarity of iontophoresis was appropriate for the ionization status of the actives, the pH and the characteristics of the “mesh” electrode used. An impressive improvement of the scars was reported but there were neither passive nor placebo iontophoresis controls (Fig. 6.5). Local effects included post-iontophoresis erythema in all patients. No other side effects were reported for the estriol group, but three patients complained of dry skin, and one developed typical retinoid dermatitis in the tretinoin group. The same group (Schmidt et al. 1999) explored further the use of tretinoin iontophoresis in a study involving 32 patients (19 women (15–39 years) and 13 men (18–48 years)). The iontophoresis procedure used a tretinoin gel (0.025 %) and involved 20-min 3- mA current sessions applied twice weekly using a Minisan (Medizintechnik, Austria) low-frequency instrument and a metal facial mask covered with a sponge material that provided openings for the nostrils and mouth. Once again, a significant improvement was reported although, in this case, the efficiency of the treatment is assessed through subjective evaluations of scar depth, skin firmness and elasticity, pore size and skin moisture.
Treatment of atrophic acne scars. The protocol involved 15-min sessions of 3 mA iontophoresis applied twice weekly for a 3-month period using either an acid aqueous solution of 0.3 % estriol or a 0.025 % tretinoin gel as donor formulation (Data taken and redrawn from Schmidt et al. 1995)
The third study involved twice weekly iontophoretic (20 min of 6 mA) sessions over a ~3.5-month period and a 0.05 % tretinoin gel as donor (Knor 2004). Thirty-eight patients with different scar types (ten superficial, ten macula atrophic, seven depressed fibrotic and 11 ice pick) and scar ages (nine (0–1 years), nine (1–2 years), 13 (2–4 years) and seven (4–10 years)) participated. The assessment included clinical examination (scar depth, skin colour, skin vascularization, pore size, skin firmness and elasticity), photographs and measurements of skin moisture, sebum and pH values. Complete or partial flattening of scars was achieved in 79 % of the cases studied; most interestingly, the outcome was highly dependent on the type and age of the scar. Best results were observed for scars with small diameter (superficial and ice pick), whereas the most disappointing results were observed for depressed fibrotic scars and old scars.
6 Iontophoretic Drug Delivery to the Nail
The iontophoresis of prednisolone sodium phosphate in vivo across the nail was reported in 1986, possibly the earliest proof of concept for iontophoretic nail delivery (James et al. 1986). Yet, it was only in the last decade that significant advance was observed in this area as recently summarized (Delgado-Charro 2012). The efficiency of iontophoresis to enhance the nail transport of therapeutic drugs varies; in vitro the enhancement fold ranges from 5 to 10 (Murthy et al. 2007b; a; Hao et al. 2009; Amichai et al. 2010a). Iontophoresis enhances the delivery of terbinafine into and across the nail plate both in vitro and in vivo. However, there are large differences in the level of enhancement observed, a fact partially explained by the different experimental conditions used and the relatively complex formulations required to provide sufficient drug solubility (Amichai et al. 2010a, b; Nair et al. 2009a, b, c; 2011). For example, the delivery of terbinafine in vitro across human nail and porcine hoof from a pH 4 formulation (1 % terbinafine, 37–40 % ethoxydiglycol, 1.5 % hydroxyethyl cellulose, 0–3 % dimethyl sulfoxide (DMSO) and 1 % NaCl or KCl) has been reported (Amichai et al. 2010a). The cumulative deliveries of terbinafine after 24 h were 0.3 ± 0.9; 0, and 4.6 ± 6.3 μg.cm−2 for the passive, 0.3 mA.cm−2, and 0.4 mA.cm−2 experiments, respectively. Further release of the drug into the receptor was measured after the donor was removed suggesting the formation of a drug reservoir in the nail plate.
It is now generally believed that iontophoretic transport across the nail can occur both by electro-osmosis and electrorepulsion mechanisms. The permselective properties of the nail have been clearly demonstrated by Murthy et al. (2007a) who characterized the transport of glucose and griseofulvin in the pH range 3–7. Anodal and cathodal fluxes were higher at pH 7 and 3, respectively. Similar anodal and cathodal transport was measured at pH 5 suggesting that the nail’s isoelectric point is around this value. Further, nail permselectivity affects the iontophoretic transport of small inorganic ions such as sodium, the transport number of which increased from 0.35 to 0.88 in the pH range 4–7 (symmetric pH experiments) (Dutet and Delgado-Charro 2010b) and from 0.25 to 0.6 as the donor pH increased from 3 to 11 (asymmetric pH experiments) (Smith et al. 2010). Despite the nail’s well-established permselectivity, it remains to be seen whether drug delivery solely based on electro-osmosis will be a useful approach. For example, the iontophoretic transport of mannitol and urea across the nail has been extremely variable and not always greater than the passive controls (Hao and Li 2008; Dutet and Delgado-Charro 2010a).
The contribution of electromigration to transport in transungual iontophoresis seems more efficient. In vitro experiments showed the transport numbers of sodium and lithium to be directly proportional to their molar fractions; further the gradient of the linear regression increased with pH, reflecting changes in nail permselectivity, and could be used to predict the maximum transport number (absence of competing co-ions) (Dutet and Delgado-Charro 2010b). According to these results, transport numbers during nail iontophoresis are primarily determined by molar fraction and mobility, very similarly to what occurs during transdermal iontophoresis (Fig. 6.6).
Cation transport numbers during transungual iontophoresis. The donor formulation was 50-mM NaCl + 50-mM LiCl in 5-mM HEPES (4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid); a 0.2 mA (1 mA.cm−2). Direct current was passed across fingernail tips (Data taken and redrawn from Dutet and Delgado-Charro 2010b)
The role of other factors such as current intensity, competing ions and pH is illustrated by work on the nail iontophoresis of salicylic acid (SA) (Murthy et al. 2007b). SA cathodal transport was proportional to the intensity of current, increased linearly with SA concentration and decreased with increasing concentration of competing co-ions. Another series of experiments investigated the effect of pH; SA cathodal fluxes respond, as expected, to changes in the drug ionization (pKa = 3.1) and in the nail permselectivity (Murthy et al. 2007b).
The feasibility of nail iontophoresis, in vivo, has been clearly demonstrated. Constant current iontophoresis (0.2 mA, 0.5 mA.cm−2) was well tolerated by healthy volunteers; further, changes in TOWL (transonychial water loss) (Dutet and Delgado-Charro 2009) were similar after passive and iontophoretic experiments and had disappeared in approximately 1 h. A recent work based on Fourier Transform InfraRed spectrometry (FT-IR) and impedance spectroscopy (Benzeval et al. 2013) also suggests the TOWL changes observed after nail iontophoresis to be mostly due to hydration. Reverse iontophoresis across the nail has also been reported albeit for small inorganic ions only; the in vivo sodium transport number was 0.51 ± 0.1 (Dutet and Delgado-Charro 2009).
A clinical study concerning terbinafine nail iontophoresis involved 38 patients with toe onychomycosis (Amichai et al. 2010b). The 0.1-mA constant current was applied using graphite active and Ag/AgCl return electrodes, respectively, and a 1-cm2 patch containing 1 % terbinafine HCl. The patches also contained 25 % ethylene oxide/propylene oxide block copolymer (Pluronic® F127, Uniqema, USA), 2 % absolute ethanol, 5 % propylene glycol, 0.8 % Sharomix 824 (a blend containing pethylparaben, ethylparaben, propylparaben and phenoxyethanol) and 0.12 % triethanolamine in water at a pH 4.6. Passive and iontophoretic patches were applied to the toenail for 6–8 h overnight, 5 days a week for 4 weeks. The iontophoresis group had significant improvement and higher amounts of terbinafine (5.69 ± 2.15 μg.cm−2) in the nail plate compared to the passive group (1.34 ± 0.54 μg.cm−2); the patch was well tolerated.
Overall, the in vivo data available suggest that nail iontophoresis is both efficient and well tolerated. Nevertheless, the clinical potential of iontophoresis to treat nail diseases and the relative advantages of this enhancement technique with respect to other methods for drug delivery have not been fully established.
7 Reverse Iontophoresis: Non-invasive Sampling Applications
Iontophoresis is a symmetric process that can be used both for drug delivery and sampling applications. Many molecules including drugs and markers of therapeutic and clinical interest are extracted to the surface from both the subdermal compartment and from within the skin. The potential for non-invasive clinical chemistry was soon noticed, and applications tested include general blood chemistry, glucose monitoring, the detection of diagnostic markers and therapeutic drug monitoring. This field, extensively reviewed in the past (Delgado-Charro 2011; Leboulanger et al. 2004d), has seen relatively few new developments lately; therefore, this section aims to summarize only the basic principles underlying the methodology and applications of reverse iontophoresis.
-
1.
Iontophoretic sampling can be mediated by both electromigration and electro-osmosis, allowing extraction of both charged and neutral compounds. Nevertheless, as illustrated by phenytoin (Leboulanger et al. 2004c), charged analytes are more efficiently extracted.
-
2.
Molar fraction, competing ions, pH, ionization status and current intensity affect the efficiency of iontophoretic transport similarly in sampling applications and drug delivery (Leboulanger et al. 2004d; Delgado-Charro 2011). Nevertheless, with the exception of current intensity, these factors cannot be easily manipulated in reverse iontophoresis, being primarily controlled by physiological values (pH, ionic composition) and by the clinical concentration range of markers and drugs. Transport numbers of drugs and markers are normally small because of the competition with the more mobile and concentrated endogenous ions. That is, sodium and chloride ions will transport most of the charge towards the cathodal and anodal compartments, respectively (Leboulanger et al. 2004a; Sieg et al. 2004a). All the same, manipulation of the collector formulation allowed some optimization of the extraction process, as shown for the electro-osmotic extraction of mannitol and glucose (Santi and Guy 1996a, b; Tamada and Comyns 2005).
-
3.
Because proteins and other large molecules are not efficiently transported across the skin, reverse iontophoretic samples provide a relatively “clean” matrix for measuring free drug concentrations typically requiring little processing. It follows that only the free fraction of a drug is available for iontophoretic sampling as demonstrated for phenytoin (Leboulanger et al. 2004c) and that extraction fluxes will decrease for heavily bound drugs, adding to the analytical challenge.
-
4.
Small, fully charged, highly concentrated and not significantly protein-bound compounds are probably the best candidates to be extracted by reverse iontophoresis by electromigration. For example, the feasibility of a non-invasive iontophoretic therapeutic monitoring of lithium has been demonstrated (Leboulanger et al. 2004a). In the case of neutral compounds, those found in relatively high concentration are preferred, as it is the case of glucose (Tamada et al. 1999, DirecNet, 2004). Other critical issues are the clinical application and potential market envisaged which explains why the first and only reverse iontophoretic device so far marketed has been the GlucoWatch Biographer® (Cygnus, Inc., USA) (Tamada et al. 1999, DirecNet, 2004). The GlucoWatch Biographer®, no longer in the market, was a glucose monitoring device which was worn on the wrist like a watch (see Fig. 6.7) and took non-invasive glucose measurements through the skin every 10 min for up to 13 h.
-
5.
Iontophoretic extraction is generally more efficient and reproducible than passive transdermal sampling, even though the extracted quantities of analyte are typically very small. The sensitivity of the analytical method determines the minimum amount of analyte to be extracted to allow for an accurate quantification and, as a result, the duration of the iontophoretic sampling procedure. It should be noticed that not all applications require the same continuous sampling and sophisticated technology that glucose monitoring does. For example, the assessment of an average drug exposure could be sufficient for the therapeutic drug monitoring of some drugs, and this would require less frequent sampling and could be performed by simpler iontophoretic devices without integrated analytical capabilities.
-
6.
The iontophoretic fluxes of extraction of some analytes are high at the beginning of the extraction period and decline afterwards. This has been observed in vitro and in vivo for endogenous analytes such us glucose (Rao et al. 1993), urea (Wascotte et al. 2004, 2007), lactate (Nixon et al. 2007) and many amino acids (Sieg et al. 2009; Sylvestre et al. 2010) and in vivo (Leboulanger et al. 2004a) for the case of patients following chronic lithium therapy. The iontophoretic fluxes of extraction for these compounds only correlate with the systemic levels after this initial phase, or “warm-up” period. This observation has been explained by the presence of a skin reservoir for these substances, which either exists naturally as it is the case of glucose and components of the natural moisturizing factor or builds up upon the chronic administration of lithium. This first short phase provides an opportunity to extract markers of skin health or with cosmetic significance and potentially, to assess historical chemical exposure (e.g. adherence to treatment drugs). Once the reservoir is exhausted, the analytes are extracted from the subdermal interstitial fluid which is in equilibrium with plasma, and therefore the fluxes of extraction provide “real-time” information as it has been shown for glucose, urea and lithium (Leboulanger et al. 2004a; Sieg et al. 2004a; Tamada et al. 1999; Wascotte et al. 2007).
-
7.
A critical issue concerning reverse iontophoresis has been the calibration of the efficiency of extraction. Ideally, the fluxes of extraction would be linearly proportional to the systemic concentration of the analyte, and the proportionality constant which reflects the efficiency of the extraction process would be constant from the beginning of the extraction and would suffer from little inter- and intra-variability. However, this has not been always the case. Firstly, the extraction fluxes observed for a constant subdermal concentration require some time to become steady, and the lag time varies between 0.5 and 10 h depending on the analyte considered (Leboulanger et al. 2004b, c, d; Delgado-Charro 2011; Santi and Guy 1996a, b). Evidently, the interpretation of the extraction data becomes further complicated when the subdermal levels change reflecting a drug or a marker disposition (Leboulanger et al. 2004b). Secondly, the efficiency of glucose extraction showed wide inter- and intra-variability so that the GlucoWatch® Biographer had to be calibrated via a conventional finger stick prior to each use; this was perceived as an important limitation (Sieg et al. 2004a; Tamada et al. 1999, DirecNet, 2004). Conversely, the efficiency of lithium extraction has shown little variability, and in fact, the constant determined in a training set of patients could be used to predict the serum levels of the drug in another patient group (Leboulanger et al. 2004a). It is not clearly established whether the variability is related to the mechanism of extraction (electro-osmosis versus electrorepulsion) or to the properties of the analyte. While some work has attempted to solve this issue via an internal standard calibration procedure, a good internal standard for glucose has not been identified yet (Sieg et al. 2004a, b; Leboulanger et al. 2004b).
-
8.
Other areas in which reverse iontophoresis has been frequently tried and several in vivo studies reported are the assessment of renal function (Wascotte et al. 2004; Ching et al. 2011; Djabri 2015; Degim et al. 2003) and of skin health, primarily the extraction of components of the natural moisturizing factor (Wascotte et al. 2004, 2007; Sieg et al. 2004b, 2009; Nixon et al. 2007; Sylvestre et al. 2010).
To summarize, although the potential of reverse iontophoresis as a non-invasive sampling tool has been demonstrated, only one device the GlucoWatch Biographer® has been marketed for sampling purposes. Reverse iontophoresis can offer non-invasive therapeutic monitoring and clinical chemistry for drugs and markers with the adequate clinical, pharmacokinetic and physicochemical properties, thus addressing the needs of patient populations for which repetitive blood sampling represents a significant burden.
Conclusions
Transdermal iontophoresis has demonstrated to be a useful tool both to deliver and to sample drugs and markers. The efficiency of iontophoresis to enhance topical and transdermal drug delivery has been clearly established through abundant in vivo and in vitro data for multiple drugs; further iontophoresis is non-invasive and considered as safe, with several iontophoresis devices having reached the market for both topical and transdermal applications. Nevertheless, a judicious choice of the drug and application is crucial for the successful implementation of iontophoresis. Nail and ocular iontophoresis have progressed significantly in the last decade. Despite the relatively low number of iontophoretic devices marketed, the area continues to be actively researched and tested in clinical trials. The key benefits of iontophoresis are its ability to modulate drug input, its safety profile and the enhancement observed with respect to passive diffusion for judiciously selected candidates.
References
Ahmad S, Hewitt DJ, Damaraju CV (2007) Fentanyl HCl iontophoretic transdermal system versus intravenous morphine pump after gynecologic surgery. Arch Gynecol Obstet 276:251–258
Alvarez-Figueroa MJ, Delgado-Charro MB, Blanco-Mendez J (2001) Passive and iontophoretic transdermal penetration of methotrexate. Int J Pharm 212:101–107
Amichai B, Mosckovitz R, Trau H et al (2010a) Iontophoretic terbinafine HCL 1.0% delivery across porcine and human nails. Mycopathologia 169:343–349
Amichai B, Nitzan B, Mosckovitz R et al (2010b) Iontophoretic delivery of terbinafine in onychomycosis: a preliminary study. Br J Dermatol 162:46–50
Anderson LL, Welch ML, Grabski WJ (1997) Allergic contact dermatitis and reactivation phenomenon from iontophoresis of 5-fluorouracil. J Am Acad Dermatol 36:478–479
Ashburn MA, Stephen RL, Ackerman E, Petelenz TJ, Hare B, Pace NL et al (1992) Iontophoretic delivery of morphine for postoperative analgesia. J Pain Symptom Manage 7:27–33
Ashburn MA, Streisand J, Zhang J, Love G, Rowin M, Niu S et al (1995) The iontophoresis of fentanyl citrate in humans. Anesthesiology 82:1146–1153
Azzaro AJ, Ziemniak J, Kemper E, Campbell BJ, VanDenBerg C (2007) Pharmacokinetics and absolute bioavailability of selegiline following treatment of healthy subjects with the selegiline transdermal system (6 mg/24 h): a comparison with oral selegiline capsules. J Clin Pharmacol 47:1256–1267
Bath BD, Scott ER, Phipps JB, White HS (2000a) Scanning electrochemical microscopy of iontophoretic transport in hairless mouse skin. Analysis of the relative contributions of diffusion, migration, and electroosmosis to transport in hair follicles. J Pharm Sci 89:1537–1549
Bath BD, White HS, Scott ER (2000b) Visualization and analysis of electroosmotic flow in hairless mouse skin. Pharm Res 17:471–475
Beauchamp M, Lands LC (2005) Sweat-testing: a review of current technical requirements. Pediatr Pulmonol 39:507–511
Benzeval I, Bowen CR, Guy RH, Delgado-Charro MB (2013) Effects of iontophoresis, hydration and permeation enhancers on human nail plate: infrared and impedance spectroscopy assessment. Pharm Res. doi:10.1007/s11095-013-1010-y
Berner B, Wilson DR, Guy RH, Mazzenga GC, Clarke FH, Maibach HI (1988) The relationship of pKa and acute skin irritation in man. Pharm Res 5:660–663
Bodde HE, Roemele PE, Star WM (2002) Quantification of topically delivered 5-aminolevulinic acid by lontophoresis across ex vivo human stratum corneum. Photochem Photobiol 75:418–423
Bodde HE, Van Laar T, Van der Geest R, Danhof M (1998) An integrated pharmacokinetic-pharmacodynamic approach to optimization of R-apomorphine delivery in Parkinson’s disease. Adv Drug Deliver Rev 33:253–263
Brand RM, Guy RH (1995) Iontophoresis of nicotine in-vitro: pulsatile drug-delivery across the skin. J Control Release 33:285–292
Brouneus F, Karami K, Beronius P, Sundelof L (2001) Diffusive transport properties of some local anesthetics applicable for iontophoretic formulation of the drugs. Int J Pharm 218:57–62
Chang BK, Guthrie TH Jr, Hayakawa K, Gangarosa LP Sr (1993) A pilot study of iontophoretic cisplatin chemotherapy of basal and squamous cell carcinomas of the skin. Arch Dermatol 129:425–427
Chaturvedula A, Joshi DP, Anderson C, Morris RL, Sembrowich WL, Banga AK (2005) In vivo iontophoretic delivery and pharmacokinetics of salmon calcitonin. Int J Pharm 297:190–196
Chelly JE, Grass J, Houseman TW, Minkowitz H, Pue A (2004) The safety and efficacy of a fentanyl patient-controlled transdermal system for acute postoperative analgesia: a multicenter, placebo-controlled trial. Anesth Analg 98:427–433
Ching CTS, Chou TR, Sun TP, Huang SY, Shieh HL (2011) Simultaneous, noninvasive, and transdermal extraction of urea and homocysteine by reverse iontophoresis. Int J Nanomed 6:417–423
Choi YK, Rho YK, Yoo KH, Lim YY, Li K, Kim BJ et al (2010) Effects of vitamin C vs. multivitamin on melanogenesis: comparative study in vitro and in vivo. Int J Dermatol 49:218–226
Cohen AE, Assang C, Patane MA, From S, Korenfeld M (2012) Evaluation of dexamethasone phosphate delivered by ocular iontophoresis for treating noninfectious anterior uveitis. Ophthalmology 119:66–73
Curdy C, Kalia YN, Naik A, Guy RH (2001) Piroxicam delivery into human stratum corneum in vivo: iontophoresis versus passive diffusion. J Control Release 76:73–79
Davarian S, Kalantari KK, Rezasoltani A, Rahimi A (2008) Effect and persistency of botulinum toxin iontophoresis in the treatment of palmar hyperhidrosis. Aust J Dermatol 49:75–79
Degim IT, Ilbasmis S, Dundaroz R, Oguz Y (2003) Reverse iontophoresis: a non-invasive technique for measuring blood urea level. Pediatr Nephrol 18:1032–1037
Delgado-Charro MB (2009) Recent advances on transdermal iontophoretic drug delivery and non-invasive sampling. J Drug Del Sci Tech 19:75–88
Delgado-Charro MB (2011) Sampling substrates by skin permeabilization. In: Murthy M (ed) Dermatokinetics of therapeutic agents. Taylor and Francis Publishers, Boca Raton, pp 149–174
Delgado-Charro MB (2012) Iontophoretic drug delivery across the nail. Expert Opin Drug Del 9:91–103
Delgado-Charro MB, Guy RH (2001a) Transdermal drug delivery. In: Hillery AM, Lloyd AW, Swarbrick J (eds) Drug delivery and targeting for pharmacists and pharmaceutical scientists. Taylor & Francis Inc, London, pp 207–235
Delgado-Charro MB, Guy RH (2001b) Transdermal iontophoresis for controlled drug delivery and non-invasive monitoring. Stp Pharma Sci 11:403–414
Djabri A, Guy RH, Delgado-Charro MB (2012) Passive and iontophoretic transdermal delivery of Phenobarbital: implications in paediatric therapy. Int J Pharm 435:76–82
Djabri A, van’t Hoff W, Brock P, Wong IAC, Guy RH, Delgado-Charro MB (2015) Iontophoretic transdermal sampling of iohexol as a non-invasive tool to assess glomerular filtration rate. Pharm Res 32:590–603.
Dolianitis C, Scarff CE, Kelly J, Sinclair R (2004) Iontophoresis with glycopyrrolate for the treatment of palmoplantar hyperhidrosis. Australas J Dermatol 45(4):208–212
Drugs@FDA. 2013. Zecuity TM label Information. Drugs@FDA. FDA approved products. Available from: http://www.accessdata.fda.gov/scripts/cder/drugsatfda.
Dutet J, Delgado-Charro MB (2009) In vivo transungual iontophoresis: effect of DC current application on ionic transport and on transonychial water loss. J Control Release 140:117–125
Dutet J, Delgado-Charro MB (2010a) Electroosmotic transport of mannitol across human nail during constant current iontophoresis. J Pharm Pharmacol 62:721–729
Dutet J, Delgado-Charro MB (2010b) Transungual iontophoresis of lithium and sodium: effect of pH and co-ion competition on cationic transport numbers. J Control Release 144:168–174
Eljarrat-Binstock E, Domb AJ (2006) Iontophoresis: a non-invasive ocular drug delivery. J Control Release 110:479–489
Eljarrat-Binstock E, Domb AJ, Orucov F, Frucht-Pery J, Pe’er J (2007) Methotrexate delivery to the eye using transscleral hydrogel iontophoresis. Curr Eye Res 32:639–646
Eljarrat-Binstock E, Pe’er J, Domb AJ (2010) New techniques for drug delivery to the posterior eye segment. Pharm Res 27:530–543
Eljarrat-Binstock E, Raiskup F, Frucht-Pery J, Domb AJ (2005) Transcorneal and transscleral iontophoresis of dexamethasone phosphate using drug loaded hydrogel. J Control Release 106:386–390
Eljarrat-Binstock E, Raiskup F, Stepensky D, Domb AJ, Frucht-Pery J (2004) Delivery of gentamicin to the rabbit eye by drug-loaded hydrogel iontophoresis. Invest Ophthalmol Vis Sci 45:2543–2548
EMA 2008. Questions and answers on the recommendation to suspend the marketing authorization of Ionsys. European Medicines Agency. London. 2008. Doc.Ref.EMEA/CHMP/609856/2008.; Available from: http://www.emea.europa.eu/docs/en_GB/document_library/Medicine_QA/2009/11/WC500014766.pdf.
Femenia-Font A, Balaguer-Fernandez C, Merino V, Lopez-Castellano A (2005) Iontophoretic transdermal delivery of sumatriptan: effect of current density and ionic strength. J Pharm Sci 94:2183–2186
Foti C, Cassano N, Conserva A, Vena GA (2004) Allergic contact dermatitis due to diclofenac applied with iontophoresis. Clin Exp Dermatol 29:91
Galinkin JL, Rose JB, Harris K, Watcha MF (2002) Lidocaine iontophoresis versus eutectic mixture of local anesthetics (EMLA) for IV placement in children. Anesth Analg 94:1484–1488
Gangarosa LP, Merchant HW, Park NH, Hill JM (1979) Iontophoretic application of idoxuridine for recurrent herpes labialis: report of preliminary clinical trials. Method Find Exp Clin Pharmacol 1:105–109
Gangarosa LP Sr, Hill JM, Thompson BL, Leggett C, Rissing JP (1986) Iontophoresis of vidarabine monophosphate for herpes orolabialis. J Infect Dis 154:930–934
Garagiola U, Dacatra U, Braconaro F, Porretti E, Pisetti A, Azzolini V (1988) Iontophoretic administration of pirprofen or lysine soluble aspirin in the treatment of rheumatic diseases. Clin Ther 10:553–558
Gelfuso GM, Gratieri T, Delgado-Charro MB, Guy RH, Fonseca Vianna Lopez R (2013) Iontophoresis-targeted, follicular delivery of minoxidil sulphate for the treatment of alopecia. J Pharm Sci 102(5):1488–1494. doi:10.1002/jps.23485
Gherardini G, Gurlek A, Evans GR, Milner SM, Matarasso A, Wassler M et al (1998) Venous ulcers: improved healing by iontophoretic administration of calcitonin gene-related peptide and vasoactive intestinal polypeptide. Plast Reconstr Surg 101:90–93
Goldstein J, Smith TR, Pugach N, Griesser J, Sebree T, Pierce M (2012) A sumatriptan iontophoretic transdermal system for the acute treatment of migraine. Headache 52:1402–1410
Gratieri T, Kalaria D, Kalia YN (2011) Non-invasive iontophoretic delivery of peptides and proteins across the skin. Expert Opin Drug Deliv 8:645–663
Green PG, Shroot B, Bernerd F, Pilgrim WR, Guy RH (1992) In vitro and in vivo iontophoresis of a tripeptide across nude rat skin. J Control Release 20:209
Gungor S, Delgado-Charro MB, Ruiz-Perez B, Schubert W, Isom P, Moslemy P et al (2010) Trans-scleral iontophoretic delivery of low molecular weight therapeutics. J Control Release 147:225–231
Gupta SK, Sathyan G, Phipps B, Klausner M, Southam M (1999) Reproducible fentanyl doses delivered intermittently at different time intervals from an electrotransport system. J Pharm Sci 88:835–841
Gupta SK, Southam M, Sathyan G, Klausner M (1998) Effect of current density on pharmacokinetics following continuous or intermittent input from a fentanyl electrotransport system. J Pharm Sci 87:976–981
Hao JS, Li SK (2008) Transungual iontophoretic transport of polar neutral and positively charged model permeants: effects of electrophoresis and electroosmosis. J Pharm Sci 97:893–905
Hao J, Smith KA, Li SK (2009) Iontophoretically enhanced ciclopirox delivery into and across human nail plate. J Pharm Sci 98:3608–3616
Hartrick CT, Bourne MH, Gargiulo K, Damaraju CV, Vallow S, Hewitt DJ (2006) Fentanyl iontophoretic transdermal system for acute-pain management after orthopedic surgery: a comparative study with morphine intravenous patient-controlled analgesia. Reg Anesth Pain Med 31:546–554
Heit MC, Williams PL, Jayes FL, Chang SK, Riviere JE (1993) Transdermal iontophoretic peptide delivery: in vitro and in vivo studies with luteinizing hormone releasing hormone. J Pharm Sci 82:240–243
Huh CH, Seo KI, Park JY, Lim JG, Eun HC, Park KC (2003) A randomized, double-blind, placebo-controlled trial of vitamin C iontophoresis in melasma. Dermatology 206:316–320
James MP, Graham RM, English J (1986) Percutaneous iontophoresis of prednisolone–a pharmacokinetic study. Clin Exp Dermatol 11:54–61
Kalia YN, Naik A, Garrison J, Guy RH (2004) Iontophoretic drug delivery. Adv Drug Deliv Rev 56:619–658
Kankkunen T, Sulkava R, Vuorio M, Kontturi K, Hirvonen J (2002) Transdermal iontophoresis of tacrine in vivo. Pharm Res 19:704–707
Kari B (1986) Control of blood glucose levels in alloxan-diabetic rabbits by iontophoresis of insulin. Diabetes 35:217–221
Kearns GL, Heacook J, Dally SAJ, Singh H, Alander SW, Qu S (2003) Percutaneous lidocaine administration via a new iontophoresis system in children: tolerability and absence of systemic bioavailability. Pediatrics 112:578–582
Kitchens JA, Schwartz SA, Schindler WG, Hargreaves KM (2007) Iontophoresis significantly increases the trans-dentinal delivery of osteoprotegerin, alendronate, and calcitonin. J Endod 33:1208–1211
Knor T (2004) Flattening of atrophic acne scars by using tretinoin by iontophoresis. Acta Dermatovenerol Croat 12:84–91
Kochhar C, Imanidis G (2004) In vitro transdermal iontophoretic delivery of leuprolide under constant current application. J Control Release 98:25–35
Kompella UB, Kadam RS, Lee VH (2010) Recent advances in ophthalmic drug delivery. Ther Deliv 1:435–456
Kreyden OP (2004) Iontophoresis for palmoplantar hyperhidrosis. J Cosmet Dermatol 3:211–214
Kumar S, Char H, Patel S, Piemontese D, Malick AW, Iqbal K et al (1992) In vivo transdermal iontophoretic delivery of growth-hormone releasing-factor GRF (1–44) in hairless guinea-pigs. J Control Release 18:213–220
Langkjaer L, Brange J, Grodsky GM, Guy RH (1998) Iontophoresis of monomeric insulin analogues in vitro: effects of insulin charge and skin pretreatment. J Control Release 51:47–56
Lau DT, Sharkey JW, Petryk L, Mancuso FA, Yu Z, Tse FL (1994) Effect of current magnitude and drug concentration on iontophoretic delivery of octreotide acetate (Sandostatin) in the rabbit. Pharm Res 11:1742–1746
Leboulanger B, Aubry JM, Bondolfi G, Guy RH, Delgado-Charro MB (2004a) Lithium monitoring by reverse iontophoresis in vivo. Clin Chem 50:2091–2100
Leboulanger B, Fathi M, Guy RH, Delgado-Charro MB (2004b) Reverse iontophoresis as a non-invasive tool for lithium monitoring and pharmacokinetic profiling. Pharm Res 21:1214–1222
Leboulanger B, Guy RH, Delgado-Charro MB (2004c) Non-invasive monitoring of phenytoin by reverse iontophoresis. Eur J Pharm Sci 22:427–433
Leboulanger B, Guy RH, Delgado-Charro MB (2004d) Reverse iontophoresis for non-invasive transdermal monitoring. Physiol Meas 25:R35–R50
Ledger P (1992) Skin biological issues in electrically enhanced transdermal delivery. Adv Drug Deliver Rev 9:289–307
Li GL, de Vries JJ, van Steeg TJ, van den Bussche H, Maas HJ, Reeuwijk HJ et al (2005) Transdermal iontophoretic delivery of apomorphine in patients improved by surfactant formulation pretreatment. J Control Release 101:199–208
Li LC, Scudds RA, Heck CS, Harth M (1996) The efficacy of dexamethasone iontophoresis for the treatment of rheumatoid arthritic knees: a pilot study. Arthritis Care Res 9:126–132
Liu J, Sun Y, Siddiqui O, Chien Y, Shi W, Li J (1988) Blood glucose control in diabetic rats by transdermal iontophoretic delivery of insulin. Int J Pharm 44:197–204
Lu MF, Lee D, Carlson R, Rao GS, Hui HW, Adjei L et al (1993) The effects of formulation variables on iontophoretic transdermal delivery of leuprolide to humans. Drug Dev Ind Pharm 19:1557–1571
Luzardo-Alvarez A, Delgado-Charro MB, Blanco-Mendez J (2003) In vivo iontophoretic administration of ropinirole hydrochloride. J Pharm Sci 92:2441–2448
Macchia L, Caiaffa MF, di Gioia R, Tursi A (2004) Systemic adverse reaction to diclofenac administered by transdermal iontophoresis. Allergy 59:367–368
Maloney JM, Bezzant JL, Stephen RL, Petelenz TJ (1992) Iontophoretic administration of lidocaine anesthesia in office practice: an appraisal. J Dermatol Surg Oncology 18:937–940
Meyer BR, Kreis W, Eschbach J, O’Mara V, Rosen S, Sibalis D (1990) Transdermal versus subcutaneous leuprolide: a comparison of acute pharmacodynamic effect. Clin Pharmacol Ther 48:340–345
Minkowitz HS, Rathmell JP, Vallow S, Gargiulo K, Damaraju CV, Hewitt DJ (2007) Efficacy and safety of the fentanyl iontophoretic transdermal system (ITS) and intravenous patient-controlled analgesia (IV PCA) with morphine for pain management following abdominal or pelvic surgery. Pain Med 8:657–668
Morrel EM, Spruance SL, Goldberg DI (2006) Topical iontophoretic administration of acyclovir for the episodic treatment of herpes labialis: a randomized, double-blind, placebo-controlled, clinic-initiated trial. Clin Infect Dis 43:460–467
Mudry B, Carrupt PA, Guy RH, Delgado-Charro MB (2007) Quantitative structure-permeation relationship for iontophoretic transport across the skin. J Control Release 122:165–172
Mudry B, Guy RH, Delgado-Charro MB (2006a) Prediction of iontophoretic transport across the skin. J Control Release 111:362–367
Mudry B, Guy RH, Delgado-Charro MB (2006b) Transport numbers in transdermal iontophoresis. Biophys J 90:2822–2830
Murthy SN, Waddell DC, Shivakumar HN et al (2007a) Iontophoretic permselective property of human nail. J Dermatol Sci 46:150–152
Murthy SN, Wiskirchen DE, Bowers CP (2007b) Iontophoretic drug delivery across human nail. J Pharm Sci 96:305–311
Nair AB, Kim HD, Chakraborty B et al (2009a) Ungual and trans-ungual iontophoretic delivery of terbinafine for the treatment of onychomycosis. J Pharm Sci 98:4130–4140
Nair AB, Kim HD, Davis SP et al (2009b) An ex vivo toe model used to assess applicators for the iontophoretic ungual delivery of terbinafine. Pharm Res 26:2194–2201
Nair AB, Vaka SR, Sammeta SM et al (2009c) Trans-ungual iontophoretic delivery of terbinafine. J Pharm Sci 98:1788–1796
Nair AB, Kiran Vaka SR, Murthy SN (2011) Transungual delivery of terbinafine by iontophoresis in onychomycotic nails. Drug Dev Ind Pharm 37:1253–1258
Nair VB, Panchagnula R (2004) Influence of electrical parameters in the iontophoretic delivery of a small peptide: in vitro studies using arginine-vasopressin as a model peptide. Farmaco 59:583–593
Nangia A, Andersen PH, Berner B, Maibach HI (1996) High dissociation constants (pKa) of basic permeants are associated with in vivo skin irritation in man. Contact Dermatitis 34:237–242
Nirschl RP, Rodin DM, Ochiai DH, Maartmann-Moe C (2003) Iontophoretic administration of dexamethasone sodium phosphate for acute epicondylitis. A randomized, double-blinded, placebo-controlled study. Am J Sport Med 31:189–195
Nixon S, Sieg A, Delgado-Charro MB, Guy RH (2007) Reverse iontophoresis of L-lactate: in vitro and in vivo studies. J Pharm Sci 96:3457–3465
Nugroho AK, Della Pasqua O, Danhof M, Bouwstra JA (2004) Compartmental modeling of transdermal iontophoretic transport: I. In vitro model derivation and application. Pharm Res 21:1974–1984
Padmanabhan RV, Phipps JB, Lattin GA, Sawchuk RJ (1990) In vitro and in vivo evaluation of transdermal iontophoretic delivery of hydromorphone. J Control Release 11:123–135
Padula C, Sartori F, Marra F, Santi P (2005) The influence of iontophoresis on acyclovir transport and accumulation in rabbit ear skin. Pharm Res 22:1519–1524
Parkinson TM, Ferguson E, Febbraro S, Bakhtyari A, King M, Mundasad M (2003) Tolerance of ocular iontophoresis in healthy volunteers. J Ocul Pharmacol Ther 19:145–151
Patane MA, Cohen A, From S, Torkildsen G, Welch D, Ousler GW 3rd (2011) Ocular iontophoresis of EGP-437 (dexamethasone phosphate) in dry eye patients: results of a randomized clinical trial. Clin Ophthalmol 5:633–643
Patel SR, Zhong H, Sharma A, Kalia YN (2009) Controlled non-invasive transdermal iontophoretic delivery of zolmitriptan hydrochloride in vitro and in vivo. Eur J Pharm Biopharm 72:304–309
Peng Q, Warloe T, Berg K, Moan J, Kongshaug M, Giercksky KE et al (1997) 5-Aminolevulinic acid-based photodynamic therapy. Clinical research and future challenges. Cancer 79:2282–2308
Pescina S, Ferrari G, Govoni P, Macaluso C, Padula C, Santi P et al (2010) In-vitro permeation of bevacizumab through human sclera: effect of iontophoresis application. J Pharm Pharmacol 62:1189–1194
Pescina S, Padula C, Santi P, Nicoli S (2011) Effect of formulation factors on the trans-scleral iontophoretic and post-iontophoretic transports of a 40 kDa dextran in vitro. Eur J Pharm Sci 42:503–508
Phahonthep R, Sindhuphak W, Sriprajittichai P (2004) Lidocaine iontophoresis versus EMLA cream for CO2 laser treatment in seborrheic keratosis. J Med Assoc Thailand 87(Suppl 2):S15–S18
Phipps J, Gyory G (1992) Transdermal ion migration. Adv Drug Deliver Rev 9:137–176
Phipps JB, Padmanabhan RV, Lattin GA (1989) Iontophoretic delivery of model inorganic and drug ions. J Pharm Sci 78:365–369
Pillai O, Borkute SD, Sivaprasad N, Panchagnula R (2003) Transdermal iontophoresis of insulin. II. Physicochemical considerations. Int J Pharm 254:271–280
Pillai O, Kumar N, Dey CS, Borkute, Sivaprasad N, Panchagnula R (2004a) Transdermal iontophoresis of insulin: III. Influence of electronic parameters. Method Find Exp Clin 26:399–408
Pillai O, Nair V, Panchagnula R (2004b) Transdermal iontophoresis of insulin: IV. Influence of chemical enhancers. Int J Pharm 269:109–120
Pillai O, Panchagnula R (2003a) Transdermal delivery of insulin from poloxamer gel: ex vivo and in vivo skin permeation studies in rat using iontophoresis and chemical enhancers. J Control Release 89:127–140
Pillai O, Panchagnula R (2003b) Transdermal iontophoresis of insulin. V. Effect of terpenes. J Control Release 88:287–296
Rao G, Glikfeld P, Guy RH (1993) Reverse iontophoresis: development of a noninvasive approach for glucose monitoring. Pharm Res 10:1751–1755
Rastogi SK, Singh J (2005) Effect of chemical penetration enhancer and iontophoresis on the in vitro percutaneous absorption enhancement of insulin through porcine epidermis. Pharm Dev Technol 10:97–104
Reid KI, Dionne RA, Sicard-Rosenbaum L, Lord D, Dubner RA (1994) Evaluation of iontophoretically applied dexamethasone for painful pathologic temporomandibular joints. Oral Surg Oral Med Oral Pathol 77:605–609
Rhodes LE, Tsoukas MM, Anderson RR, Kollias N (1997) Iontophoretic delivery of ALA provides a quantitative model for ALA pharmacokinetics and PpIX phototoxicity in human skin. J Invest Dermatol 108:87–91
Rose JB, Galinkin JL, Jantzen EC, Chiavacci RM (2002) A study of lidocaine iontophoresis for pediatric venipuncture. Anesth Analg 94:867–871
Runeson L, Haker E (2002) Iontophoresis with cortisone in the treatment of lateral epicondylalgia (tennis elbow)–a double-blind study. Scan J Med Sci Sports 12:136–142
Sage B, Riviere J (1992) Model systems in iontophoresis—transport efficacy. Adv Drug Deliver Rev 9:265–268
Saggini R, Zoppi M, Vecchiet F, Gatteschi L, Obletter G, Giamberardino MA (1996) Comparison of electromotive drug administration with ketorolac or with placebo in patients with pain from rheumatic disease: a double-masked study. Clin Ther 18:1169–1174
Salli L (1993) Efficacy and tolerability of ketoprofene administered through iontophoresis in rheumatoid arthritis. Results from a multicentric study. Clin Ther 142:533–537
Santi P, Guy RH (1996a) Reverse iontophoresis-parameters determining electro-osmotic flow. II: electrode chamber formulation. J Control Release 42:29–36
Santi P, Guy RH (1996b) Reverse iontophoresis: parameters determining electroosmotic flow: I. pH and ionic strength. J Control Release 38:159–165
Santi P, Volpato NM, Bettini R, Catellani PL, Massimo G, Colombo P (1997) Transdermal iontophoresis of salmon calcitonin can reproduce the hypocalcemic effect of intravenous administration. Farmaco 52:445–448
Sathyan G, Jaskowiak J, Evashenk M, Gupta S (2005) Characterization of the Pharmacokinetics of the fentanyl HCl patient controlled transdermal system (PCTS). Clin Pharmacokin 44:7–15
Sato K, Timm DE, Sato F, Templeton EA, Meletiou DS, Toyomoto T et al (1993) Generation and transit pathway of H+ is critical for inhibition of palmar sweating by iontophoresis in water. J Appl Physiol 75:2258–2264
Schmidt JB, Binder M, Macheiner W, Bieglmayer C (1995) New treatment of atrophic acne scars by iontophoresis with estriol and tretinoin. Int J Dermatol 34:53–57
Schmidt JB, Donath P, Hannes J, Perl S, Neumayer R, Reiner A (1999) Tretinoin-iontophoresis in atrophic acne scars. Int J Dermatol 38:149–153
Schuetz YB, Carrupt PA, Naik A, Guy RH, Kalia YN (2006) Structure-permeation relationships for the non-invasive transdermal delivery of cationic peptides by iontophoresis. Eur J Pharm Sci 29:53–59
Schuetz YB, Naik A, Guy RH, Kalia YN (2005) Effect of amino acid sequence on transdermal iontophoretic peptide delivery. Eur J Pharm Sci 26:429–437
Scott ER, Phipps JB, Gyory JR, Padmanabhan. Electrotransport systems for transdermal delivery: a practical implementation of iontophoresis. In: Wise DL (ed) Handbook of pharmaceutical controlled release technology. Basel, Swizterland: Marcel Dekker Inc.; 2000. p. 617–659
Scott ER, Phipps JB, White HS (1995) Direct imaging of molecular transport through skin. J Invest Dermatol 104:142–145
Sekkat N, Kalia YN, Guy RH (2004) Porcine ear skin as a model for the assessment of transdermal drug delivery to premature neonates. Pharm Res 21:1390–1397
Shukla C, Friden P, Juluru R, Stagni G (2009) In vivo quantification of acyclovir exposure in the dermis following iontophoresis of semisolid formulations. J Pharm Sci 98:917–925
Sieg A, Guy RH, Delgado-Charro MB (2004a) Noninvasive glucose monitoring by reverse iontophoresis in vivo: application of the internal standard concept. Clin Chem 50:1383–1390
Sieg A, Guy RH, Delgado-Charro MB (2004b) Simultaneous extraction of urea and glucose by reverse iontophoresis in vivo. Pharm Res 21: 1805–1810
Sieg A, Jeanneret F, Fathi M, Hochstrasser D, Rudaz S, Veuthey JL, Guy RH, Delgado-Charro MB (2009) Extraction of amino acids by reverse iontophoresis in vivo. Eur J Pharm Biopharm 72:226–231
Siegel SJ, O’Neill C, Dube LM, Kaldeway P, Morris R, Jackson D et al (2007) A unique iontophoretic patch for optimal transdermal delivery of sumatriptan. Pharm Res 24:1919–1926
Singh N, Kalluri H, Herwadkar A, Badkar A, Banga AK (2012) Transcending the skin barrier to deliver peptides and proteins using active technologies. Crit Rev Ther Drug Carrier Syst 29:265–298
Smith KA, Hao J, Li SK (2010) Influence of pH on transungual passive and iontophoretic transport. J Pharm Sci 99:1955–1967
Smith KJ, Konzelman JL, Lombardo FA, Skelton HG 3rd, Holland TT, Yeager J et al (1992) Iontophoresis of vinblastine into normal skin and for treatment of Kaposi’s sarcoma in human immunodeficiency virus-positive patients. The Military Medical Consortium for Applied Retroviral Research. Arch Dermatol 128: 1365–1370
Sylvestre JP, Bouissou C, Guy RH, Delgado-Charro MB (2010) Extraction and quantification of amino acids in human stratum corneum in vivo. Br J Dermatol 163:158–465
Sylvestre JP, Díaz-Marín C, Delgado-Charro MB, Guy RH (2008a) Iontophoresis of dexamethasone phosphate: competition with chloride ions. J Control Release 131:41–46
Sylvestre JP, Guy RH, Delgado-Charro MB (2008b) In vitro optimization of dexamethasone phosphate delivery by iontophoresis. Phys Ther 88:1177–1185
Squire SJ, Kirchhoff KT, Hissong K (2000) Comparing two methods of topical anesthesia used before intravenous cannulation in paediatric patients. J Pediatr Health Care 14:68–72
Tamada JA, Comyns K (2005) Effect of formulation factors on electroosmotic glucose transport through human skin in vivo. J Pharm Sci 8:1839–1849
Tamada JA, Garg S, Jovanovic L, Pitzer KR, Fermi S, Potts RO (1999) Noninvasive glucose monitoring: comprehensive clinical results. Cygnus Res Team JAMA 282:1839–1844
Tashiro Y, Shichibe S, Kato Y, Hayakawa E, Itoh K (2001) Effect of lipophilicity on in vivo iontophoretic delivery. I NSAIDs Biol Pharm Bull 24:278–283
The diabetes research in children network (DirecNet) study group (2004) Accuracy of the GlucoWatch G2 Biographer and the continuous glucose monitoring system during hypoglycemia: experience of the Diabetes Research in Children Network. Diabetes Care 27:722–726
Thysman S, Hanchard C, Preat V (1994) Human calcitonin delivery in rats by iontophoresis. J Pharm Pharmacol 46:725–730
Thysman S, Preat V (1993) In vivo iontophoresis of fentanyl and sufentanil in rats: pharmacokinetics and acute antinociceptive effects. Anesth Analg 77:61–66
Turner NG, Guy RH (1997) Iontophoretic transport pathways: dependence on penetrant physicochemical properties. J Pharm Sci 86:1385–1389
Turner NG, Guy RH (1998) Visualization and quantitation of iontophoretic pathways using confocal microscopy. J Investig Dermatol Symp Proc 3:136–142
Vaka SR, Sammeta SM, Day LB, Murthy SN (2008) Transcorneal iontophoresis for delivery of ciprofloxacin hydrochloride. Curr Eye Res 33:661–667
Vecchini L, Grossi E (1984) Ionization with diclofenac sodium in rheumatic disorders: a double-blind placebo-controlled trial. J Int Med Res 12:346–350
Viscusi ER, Reynolds L, Tait S, Melson T, Atkinson LE (2006) An iontophoretic fentanyl patient-activated analgesic delivery system for postoperative pain: a double-blind, placebo-controlled trial. Anesth Analg 102:188–194
Wascotte V, Caspers P, de Sterke J, Jadoul M, Guy RH, Preat V (2007) Assessment of the “Skin reservoir” of urea by confocal raman microspectroscopy and reverse iontophoresis in vivo. Pharm Res 24:1897–1901
Wascotte V, Delgado-Charro MB, Guy RH, and Preat V. Monitoring renal function by reverse iontophoresis. Eur J Pharm Sci 2004;23:S57–S57
Welch ML, Grabski WJ, McCollough ML, Skelton HG, Smith KJ, Menon PA et al (1997) 5-fluorouracil iontophoretic therapy for Bowen’s disease. J Am Acad Dermatol 36:956–958
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Disclaimer
Since the submission of this chapter, a supplemental new drug application (sNDA) Ionsys System was approved by the FDA (April 2015); further this fentanyl iontophoretic system was approved by the EMA (EPAR November 2015).
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Merino, V., Castellano, A.L., Delgado-Charro, M.B. (2017). Iontophoresis for Therapeutic Drug Delivery and Non-invasive Sampling Applications. In: Dragicevic, N., I. Maibach, H. (eds) Percutaneous Penetration Enhancers Physical Methods in Penetration Enhancement. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53273-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-662-53273-7_6
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53271-3
Online ISBN: 978-3-662-53273-7
eBook Packages: MedicineMedicine (R0)