Abstract
Today, cardiovascular diseases (CD) are the overall leading cause of mortality worldwide. The most prevalent cardiovascular forms of diseases can be linked to adaptive selective forces acting during the evolution of cardiovascular systems from invertebrate animals to mammals, i.e., for 4 billion years, that have become maladaptive during the post-agricultural period, in humans following the changes in civilization, environment, and habits. Key among these is the association of arterial hypertension with increased dietary salt intake. Atherosclerotic disease has also been linked to meat and fat consumption. Policies to treat CD must be twofold: (1) to remove the maladaptive changes, e.g., high dietary salt, obesity, and high cholesterol and (2) to use our understanding of the molecular aspects of CD to develop targeted therapeutics, e.g., diuretics to increase salt excretion and to reduce lipids.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Lay summaryProminent cardiovascular pathologies, including hypertension and atherosclerosis, may have evolutionary underpinnings. For example, selection for survival with a low-salt diet in early man may underlie salt-sensitivity and hypertension in modern civilization with high dietary salt consumption. Similarly, the evolutionary process may not have had sufficient time to adapt to a shift to high-fat and meat diets in contemporary society. Thinking in these terms results in an approach to these diseases focused on changes in environmental factors.
1 Introduction
The standard approach to the treatment of cardiovascular disease is based on empirical studies and does not consider the implications or imprint of evolution, which may provide insight into the pathogenesis of heart and vascular disease in contemporary times.
The cardiovascular system has evolutionary roots in invertebrate animals when simple absorption of nutrients, as by cells, is gradually replaced by an open circulatory system in which blood, or more appropriately termed hemolymph, is not contained in vessels (or a very few) and flows freely through the organism making direct contact with organs and cells. Subsequently, vessels with focal areas of contracting muscle to move the blood as seen in the earthworm. A two-chamber heart consisting of a single atrium and ventricle with a closed circulatory system, which exposes the blood to oxygen in the gills and then transport it throughout the organs, emerged in fish. With the evolution of amphibians, e.g., frog, which exist in both water and land, a three-chamber heart developed with two atria and a single ventricle allowing oxygenated and deoxygenated blood to be separated as they enter the heart. With the advent of reptiles, e.g., turtles, a partial ventricular septum occurs to form a “three and one-half”-chamber heart. The human or mammalian heart and cardiovascular system are the most advanced, consisting of four chambers and highly developed arterial and venous circulations (reviewed in [1]). Thus, the cardiovascular system has evolved over approximately 4 billion years (see also Chap. 10).
The classical Darwinian concept of evolution is that environmental selection, along with other evolutionary forces (i.e., genetic drift, gene flow, mutation) has shaped what we are today and will, presumably, shape what we will become… slowly reducing the frequency of maladaptive traits to give way to one’s that confer a reproductive advantage. However, cardiovascular disease is the number one cause of mortality in the world today [2] The question is why, if the system is constantly being optimized by selection.
A central theory is that many of the selective forces that have acted on the cardiovascular system are now being replaced by new forces to which the cardiovascular system is not adapted [3, 4]. Human agriculture is about 12,000 years old,
only a minimal part throughout the history of human development, but its occurrence turns the human world upside down… [and] there has not been enough time for natural selection to change this design of the body to adapt us to the lifestyle of modern society [5].
Additionally, in general, cardiovascular diseases (CD) progress with aging and post-reproductive years so that the force of selection is weaker (see also Chap. 21). In this chapter, two leading causes of cardiovascular mortality, i.e., hypertension and atherosclerosis, are analyzed from this evolutionary perspective.
2 Research Findings
2.1 Hypertension
Arterial hypertension is a leading cause of heart failure, stroke, and renal failure.
It is reasoned that Darwinian selection has led to a highly regulated and complex system to maintain blood pressure for an optimal perfusion of organs and tissues, with delivery of nutrients and oxygen under all varieties of situations, such that there is scant evidence of hypertension in non-human organisms.
Blood pressure is a complex quantitative trait with both environmental and genetic components. Genome-wide associations and targeted gene studies have generated an expanding list of common and uncommon genetic variants linked to blood pressure (reviewed in [6]). Biometric strategies in the past have suggested 20–30 % of inter-individual variation in blood pressure is attributed to genes [7]. However, more recent and refined phenotyping from family studies suggest that 15–40 % of clinical systolic blood pressure and 50–60 % of ambulatory blood pressure are heritable [8–10]. Although blood pressure is heritable, “essential” hypertension does not follow a clear pattern of inheritance and is assumed to, in part, be due to the numerous interacting networks of molecular pathways, genes/protein modifications, and environmental confounders. Thus, it is reasoned that most of the genes associated with blood pressure were adaptive across human evolutionary history and may have had little phenotypic detriment until changes in human civilization occurred.
A key environmental factor in hypertension has been assigned to an increase in dietary sodium [11, 12]. The epidemiologic, clinical, and experimental support for this is overwhelming. First, in the INTERSALT Study conducted in 32 countries, the risk of developing hypertension over three decades of adult life was linearly and very tightly related to 24-hour urine sodium excretion, the best measure of dietary sodium intake. Second, reduced dietary sodium intake and diuretics have proven to be among the most effective treatments for primary hypertension. However, both normotensive and hypertensive persons show tremendous inter-individual variability in their blood pressure responses to dietary sodium loading and sodium restriction. This variability indicates a strong genetic underpinning. Third, the handful of rare Mendelian forms of human hypertension all involve excessive renal retention of salt and water, leading to severe salt-dependent hypertension.
A prevailing theory is that hypertension in human society, especially Western civilization, is the by-product of the selection for salt retention (reviewed in [13]). It has been speculated that the human diet, up until 10,000–25,000 years ago, consisted of 80 % meat with the rest being wild vegetables and fruits for an estimated daily intake of 600–770 mg sodium. With this diet, genes were selected for salt and water retention to the challenges of volume-depleting illnesses. Moreover, recent data show that dietary salt increases arterial stiffness, suggesting that the vasculature also has evolved in the context of a low-salt diet [14–16].
These genes are hypothesized to have become maladaptive when dietary salt intake increased with the agricultural revolution, harvested by solar evaporation and boiling, used to preserve and cure meats or used as a commodity of trade; and when an acquired taste for salt developed, e.g., salted fish [13, 17]. Now the average daily consumption of salt is 10–12 g/day in the USA and 24 g/day in Japan, representing 10–20 times the consumption estimated prior to the agricultural revolution [12]. Even a low-salt diet today is 6 g/day, representing a 350 % increase in about 10,000 years.
2.2 Atherosclerosis
Atherosclerosis, frequently referred to as “hardening of the arteries” is the principal cause of heart attack, stroke, and peripheral vascular disease. Heritability of atherosclerotic disease is well established and a family history of coronary artery disease is a risk factor included in established criteria for preventative treatment for cardiovascular disease [18–20]. The range of genetic variance in coronary artery disease is between 40 and 60 % based on family pedigree in twins [21, 22].
Rodents and other lower organisms do not normally develop and are resistant to developing atherosclerotic lesions even when subjected to pro-atherogenic interventions. Induction of atherosclerotic changes in vessels has not been reported in amphibians or lower species. Under non-experimental conditions, atherosclerosis is not observed in rodents on “normal” rat diets and severe interventions are required even to evoke mild atherosclerosis in rodents. In order to induce significant atherosclerosis, genetic manipulations, e.g., ApoE knockout [23, 24] are required to use these for research studies. Providing Western-style diets with high levels of saturated fats (approx. 35 % kcal %fat), cholesterol (0.5–1 % w/w), and cholic acid (0.1–5 % w/w) induces mild atherosclerosis in some mouse strains [25]. Guinea pigs, unlike other rodents, have a cholesterol profile similar to humans and develop diet-induced atherosclerotic lesions [26].
Like hypertension, atherosclerosis is considered as a function of environmental and genetic components. The difficulty in discerning these two components has been presented as evidence that the risk of the genetic variants is dependent on environmental influences [27]. Genome-wide association studies (GWAS) have identified at least 150 suggestive loci associated with coronary artery disease [28]. However, over 50 % of the associated variants occur in half of the population, and a quarter occur in 75 % of the population [29]. Thus, it is likely that on the average, each variant confers a minimal to modest risk and it has been estimated that the contribution of these to coronary artery disease and similar complex diseases is less than 10 % [27]. Many of these genes implicated in coronary artery disease are involved in inflammation and stem cell biology, and a lesser number are associated with known pathways for lipid variants [30].
Atherosclerotic disease is widely believed to be a disease of Western societies and changes in lifestyle brought about in the post-agricultural era. Major established environmental risk factors include high cholesterol, cigarette smoking, obesity, physical inactivity, and diabetes (review [31]).
A primary genetic focus of the link between increased cholesterol and genetics in the pathogenesis of atherosclerosis is the gene coding for apolipoprotein (ApoE) [32–35]. Among the principal variants, the alleles epsilon 2 (E2), epsilon 3 (E3), and epsilon 4 (E4) are the most common and have been shown to affect lipoproteins through regulation of hepatic binding, chylomicron catabolism, and uptake. Epidemiological studies have demonstrated that the epsilon 4 allele (coding for the protein ApoE4) most predisposes to atherosclerosis [36]. This allele is an “evolutionary relic from the pre-agricultural history of Homo sapiens and has not adapted to a nutrient-rich culture” [35, 37] (see also Chaps. 19 and 21). It remains at a high frequency; however, populations living in regions where agricultural economies have first been established, e.g., in the Mediterranean basin, have the lowest frequencies (0.05–0.13), while the frequency of this allele remains high among foragers, e.g., Pygmies (0.41), aborigines of Malaysia (0.24), and Papuans (0.37) [38].
A central question in evolutionary terms is whether ApoE and other proteins/gene variants linked to the lipid handling and the inflammatory response have persisted simply because they were neutral, or are under bidirectional selection (positive and negative). Both lipid handling and the inflammatory response are complex processes of interacting molecular signaling pathways and are central to cell and organ survival. The handling of fats and lipids, which include sterols, vitamins, phospholipids, and triglycerides, is key to dietary emulsification, digestion, absorption of nutrients, cell membranes, and metabolism required for cell and organ survival. The evolutionary paradigm suggests that the constellation of genes/proteins controlling lipid metabolism was selected to handle a pre-agricultural diet [39]. Inflammation plays a pathogenic role in a variety of other modern human diseases, including hypertension [40]. Inflammation has classically been defined as an evolutionary response to injury and infection; however, it is now associated with many post-agricultural human diseases, not including cardiovascular ones but also articular, inflammatory digestive, degenerative, and oncological disorders (see Chap. 18). A detailed analysis of the relevant theories has recently been address by Okin et al. [41].
A new twist in the atherosclerotic story and its link with a post-agricultural meat diet is the role of gut flora-mediated formation of pro-atherogenic compounds from meat, e.g., trimethylamine-N-oxide (TMAO) [42]. This is especially intriguing in an evolutionary context since vegetarian diets shift the microbiome to produce less TMAO, suggesting that dietary meat may have altered the gut flora to make it more pro-atherogenic.
3 Implications for Policy and Practice
Evolutionary underpinnings of contemporary CD in the post-agricultural period are based on selective pressures that have shifted from adaptive to maladaptive, or possess both adaptive and maladaptive features. In other words, “created by evolutionary hangovers… [and] biological evolution to cure hangovers can be very slow” [43]. Additionally, most CD are, in large part, age-related, occurring mostly in post-productive life, i.e., when the effect of selective pressures is markedly reduced. Thus, we cannot depend on natural selection to correct these over any predictable, albeit long time period. Policies and practices must be directed both (1) toward reducing or preventing the adverse effects of the cardiovascular risk factors derived from and associated with the post-agricultural period and (2) to use our understanding of the specific evolved genetic underpinning to develop molecular and genetics-targeted therapeutics. These strategies have already been engaged for hypertension and atherosclerosis.
For hypertension, current recommendations are to reduce salt intake to 1500–2000 mg/day [44, 45]. It should be noted that there is significant inter-individual variability and the generalized recommendation for indiscriminate reduction of salt in all populations has been a subject of recent debate [46]. Drugs targeted to reducing sodium retention and promoting salt/water excretion, including thiazides and furosemide, are among the most effective in reducing blood pressure and associated cardiovascular morbidity and mortality.
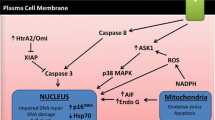
For atherosclerotic disease, there is convincing data showing that targeting both inflammatory process and genes/proteins in cholesterol/lipid metabolism associated with atherosclerosis is highly effective in reducing the incidence of coronary artery disease and stroke. Low-dose aspirin is anti-inflammatory and has proven to be one of the most efficacious treatments for coronary artery disease. Prominent among proven agents targeted to lipid metabolism are those which target HMG CoA reductase, e.g., statins, linked to atherosclerosis (reviewed in [47]). Agents are being developed to target ApoE, which is also believed to play a role in Alzheimer’s disease [48] (see Chaps. 19 and 21). Again, the situation appears much more complex. Common clinical guidelines are to reduce red meat and saturated fat consumption; however, the empirical data indicate that the relationship is “complicated” [49]. Cardiovascular risk can be reduced by decreasing saturated fats and replacing them with polyunsaturated and monounsaturated fats. Although most doctors also recommend a diet rich in plant proteins rather than in meat and poultry, the evidence for a benefit is scant [47]. Reduction of total dietary protein itself has not been shown to be of significant benefit in the prevention of coronary heart disease [50].
References
Bishopric NH (2005) Evolution of the heart from bacteria to man. Ann N Y Acad Sci 1047:13–29
Archer E, Blair SN (2011) Physical activity and the prevention of cardiovascular disease: from evolution to epidemiology. Prog Cardiovasc Dis 53:387–396
deGoma EM, Knowles JW, Angeli F, Budoff MJ, Rader DJ (2012) The evolution and refinement of traditional risk factors for cardiovascular disease. Cardiol Rev 20:118–129
Yang D, Liu Z (2013) An evolutionary perspective on cardiovascular disease. Phylogenet Evol Biol 1:1–2
Ai X, Jiang A, Ke Y, Solaro RJ, Pogwizd SM (2011) Enhanced activation of p21-activated kinase 1 in heart failure contributes to dephosphorylation of connexin 43. Cardiovasc Res 92:106–114
Sing CF, Boerwinkle E, Turner ST (1986) Genetics of primary hypertension. Clin Exp Hypertens A 8:623–651
Bochud M, Bovet P, Elston RC, Paccaud F, Falconnet C, Maillard M, Shamlaye C, Burnier M (2005) High heritability of ambulatory blood pressure in families of East African descent. Hypertension 45:445–450
Hottenga JJ, Boomsma DI, Kupper N, Posthuma D, Snieder H, Willemsen G, de Geus EJ (2005) Heritability and stability of resting blood pressure. Twin Res Hum Genet 8:499–508
Kupper N, Willemsen G, Riese H, Posthuma D, Boomsma DI, de Geus EJ (2005) Heritability of daytime ambulatory blood pressure in an extended twin design. Hypertension 45:80–85
Elliott P, Marmot M, Dyer A, Joossens J, Kesteloot H, Stamler R, Stamler J, Rose G (1989) The INTERSALT study: main results, conclusions and some implications. Clin Exp Hypertens A 11:1025–1034
Stamler J (1997) The INTERSALT study: background, methods, findings, and implications. Am J Clin Nutr 65:626S–642S
Lev-Ran A, Porta M (2005) Salt and hypertension: a phylogenetic perspective. Diabetes Metab Res Rev 21:118–131
Kusche-Vihrog K, Schmitz B, Brand E (2015) Salt controls endothelial and vascular phenotype. Pflugers Arch 467:499–512
Edwards DG, Farquhar WB (2015) Vascular effects of dietary salt. Curr Opin Nephrol Hypertens 24:8–13
Kullo IJ, Leeper NJ (2015) The genetic basis of peripheral arterial disease: current knowledge, challenges, and future directions. Circ Res 116:1551–1560
Eaton SB, Konner M (1985) Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med 312:283–289
Kullo IJ, Trejo-Gutierrez JF, Lopez-Jimenez F, Thomas RJ, Allison TG, Mulvagh SL, Arruda-Olson AM, Hayes SN, Pollak AW, Kopecky SL, Hurst RT (2014) A perspective on the New American College of Cardiology/American Heart Association guidelines for cardiovascular risk assessment. Mayo Clin Proc 89:1244–1256
Nasir K, Budoff MJ, Wong ND, Scheuner M, Herrington D, Arnett DK, Szklo M, Greenland P, Blumenthal RS (2007) Family history of premature coronary heart disease and coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 116:619–626
Marenberg ME, Risch N, Berkman LF, Floderus B (1994) de FU: Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med 330:1041–1046
Marenberg ME, Risch N, Berkman LF, Floderus B (1994) de FU: Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med 330:1041–1046
Bjorkegren JL, Kovacic JC, Dudley JT, Schadt EE (2015) Genome-wide significant loci: how important are they? Systems genetics to understand heritability of coronary artery disease and other common complex disorders. J Am Coll Cardiol 65:830–845
Jawien J (2012) The role of an experimental model of atherosclerosis: apoE-knockout mice in developing new drugs against atherogenesis. Curr Pharm Biotechnol 13:2435–2439
Imaizumi K (2011) Diet and atherosclerosis in apolipoprotein E-deficient mice. Biosci Biotechnol Biochem 75:1023–1035
Nishina PM, Verstuyft J, Paigen B (1990) Synthetic low and high fat diets for the study of atherosclerosis in the mouse. J Lipid Res 31:859–869
Fernandez ML, Volek JS (2006) Guinea pigs: a suitable animal model to study lipoprotein metabolism, atherosclerosis and inflammation. Nutr Metab (Lond) 3:17
Schadt EE, Bjorkegren JL: NEW: network-enabled wisdom in biology, medicine, and health care. Sci Transl Med 2012;4:115rv1
Bjorkegren JL, Kovacic JC, Dudley JT, Schadt EE (2015) Genome-wide significant loci: how important are they? Systems genetics to understand heritability of coronary artery disease and other common complex disorders. J Am Coll Cardiol 65:830–845
Roberts R (2015) A genetic basis for coronary artery disease. Trends Cardiovasc Med 25:171–178
Goldschmidt-Clermont PJ, Dong C, Seo DM, Velazquez OC (2012) Atherosclerosis, inflammation, genetics, and stem cells: 2012 update. Curr Atheroscler Rep 14:201–210
McGill HC Jr (1978) Risk factors for atherosclerosis. Adv Exp Med Biol 104:273–280
Davignon J, Gregg RE, Sing CF (1988) Apolipoprotein E polymorphism and atherosclerosis. Arteriosclerosis 8:1–21
Phillips MC (2014) Apolipoprotein E isoforms and lipoprotein metabolism. IUBMB Life 66:616–623
Davignon J, Cohn JS, Mabile L, Bernier L (1999) Apolipoprotein E and atherosclerosis: insight from animal and human studies. Clin Chim Acta 286:115–143
Mertens G (2010) Gene/environment interaction in atherosclerosis: an example of clinical medicine as seen from the evolutionary perspective. Int J Hypertens 2010:654078
Eichner JE, Dunn ST, Perveen G, Thompson DM, Stewart KE, Stroehla BC (2002) Apolipoprotein E polymorphism and cardiovascular disease: a HuGE review. Am J Epidemiol 155:487–495
Mahley RW, Rall SC Jr (1999) Is epsilon4 the ancestral human apoE allele? Neurobiol Aging 20:429–430
Corbo RM, Scacchi R (1999) Apolipoprotein E (APOE) allele distribution in the world. Is APOE*4 a ‘thrifty’ allele? Ann Hum Genet 63:301–310
Kuipers RS, Luxwolda MF, Dijck-Brouwer DA, Eaton SB, Crawford MA, Cordain L, Muskiet FA (2010) Estimated macronutrient and fatty acid intakes from an East African Paleolithic diet. Br J Nutr 104:1666–1687
De MC, Rudemiller NP, Abais JM, Mattson DL (2015) Inflammation and hypertension: new understandings and potential therapeutic targets. Curr Hypertens Rep 17:507
Okin D, Medzhitov R (2012) Evolution of inflammatory diseases. Curr Biol 22:R733–R740
Tang WH, Hazen SL (2014) The contributory role of gut microbiota in cardiovascular disease. J Clin Invest 124:4204–4211
Ehrlich P (2001) The human natures: genes, cultures, and the human prospect. Penguin Books, New York, p 36
Kotchen TA, Cowley AW Jr, Frohlich ED (2013) Salt in health and disease–a delicate balance. N Engl J Med 368:1229–1237
Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N, Dunbar SB, Frohlich ED, Hall JE, Jessup M, Labarthe DR, MacGregor GA, Sacks FM, Stamler J, Vafiadis DK, Van Horn LV (2012) Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 126:2880–2889
Stolarz-Skrzypek K, Staessen JA (2015) Reducing salt intake for prevention of cardiovascular disease–times are changing. Adv Chronic Kidney Dis 22:108–115
Darioli R (2011) Dietary proteins and atherosclerosis. Int J Vitam Nutr Res 81:153–161
Liao F, Hori Y, Hudry E, Bauer AQ, Jiang H, Mahan TE, Lefton KB, Zhang TJ, Dearborn JT, Kim J, Culver JP, Betensky R, Wozniak DF, Hyman BT, Holtzman DM (2014) Anti-ApoE antibody given after plaque onset decreases Abeta accumulation and improves brain function in a mouse model of Abeta amyloidosis. J Neurosci 34:7281–7292
Michas G, Micha R, Zampelas A (2014) Dietary fats and cardiovascular disease: putting together the pieces of a complicated puzzle. Atherosclerosis 234:320–328
Haring B, Gronroos N, Nettleton JA, von Ballmoos MC, Selvin E, Alonso A (2014) Dietary protein intake and coronary heart disease in a large community based cohort: results from the Atherosclerosis Risk in Communities (ARIC) Study. PLoS ONE 9:e109552
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ (2003) The Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289:2560–2572
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Glossary
- Atherosclerosis
-
Atherosclerotic plaques are aggregates of plasma lipids (especially cholesterol) cells (smooth muscle cells and monocytes/macrophages), and connective tissue matrix (collagen fibers and proteoglycans). Inflammation is the “dominant process” with atherosclerotic plaques characterized by increased cellular proliferation, lipids accumulation, calcification, ulceration, hemorrhage, and thrombosis. Typically, a major acute coronary syndrome occurs when an atherosclerotic plaque in a coronary artery ruptures with subsequent thrombosis. Chronic ischemia caused by reduced blood flow in the coronary artery due to narrowing of the vessels by atherosclerosis triggers chronic stable angina and may cause heart failure. The most common form of stroke arises when blood clots form on atherosclerotic plaques in carotid and cerebral arteries and blocks flow (reviewed in [30]).
- Hypertension
-
Over 500 million people experience hypertension worldwide and its prevalence increases with age especially in Western civilization. There is overwhelming evidence that reducing hypertension reduces cardiovascular morbidity and mortality. Antihypertensive therapy has been associated with reductions in stroke incidence averaging 35–40 %, myocardial infarction 20–25 %, and heart failure >50 %. It is estimated that in patients with stage 1 hypertension and additional cardiovascular risk factors, achieving a sustained 12 mmHg reduction in systolic blood pressure over 10 years will prevent 1 death for every 11 patients treated [51]. The origins of current standard and effective treatment of hypertension can be derived from evolutionary insights.
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Danziger, R.S. (2016). Evolutionary Imprints on Cardiovascular Physiology and Pathophysiology. In: Alvergne, A., Jenkinson, C., Faurie, C. (eds) Evolutionary Thinking in Medicine. Advances in the Evolutionary Analysis of Human Behaviour. Springer, Cham. https://doi.org/10.1007/978-3-319-29716-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-29716-3_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29714-9
Online ISBN: 978-3-319-29716-3
eBook Packages: MedicineMedicine (R0)