Abstract
The autonomic nervous system controls the cardiovascular, gastrointestinal, urogenital, respiratory, thermoregulatory, and pupillary function and regulates sleep. Such a wide distribution is reflected by the protean manifestations of autonomic disorders, which range from generalized failure to isolated organ dysfunction, thus mimicking, among others, primary disorders of the innervated organs.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Autonomic Disorders
- Pure Autonomic Failure
- Hereditary Sensory Autonomic Neuropathy (HSAN)
- Composite Autonomic Scoring Scale (CASS)
- Acute Inflammatory Demyelinating Polyradiculoneuropathy (AIDP)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
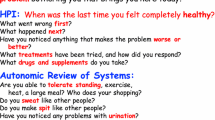
2.1 History Taking: You Need to Know What You’re Looking for
The autonomic nervous system controls the cardiovascular, gastrointestinal, urogenital, respiratory, thermoregulatory, and pupillary function and regulates sleep. Such a wide distribution is reflected by the protean manifestations of autonomic disorders, which range from generalized failure to isolated organ dysfunction, thus mimicking, among others, primary disorders of the innervated organs.
Loss of function as well as hypo-, hyper-, or deregulated activation may turn into autonomic symptoms. The clinical course may be likewise variable, from a paroxysmal or acute onset to subacute or chronic evolution. Comorbidities and other non-autonomic etiologies need to be taken into account as well. Clinical assessment of patients with suspected autonomic disorders therefore relies on a holistic approach to the patient, combined with a targeted autonomic history taking.
The present chapter is divided into three sections:
-
1.
Typical symptoms of each autonomic domain will be discussed together with possible causes and alternative, non-autonomic etiologies.
-
2.
Other important aspects to be considered: age, gender, time course, family history, and comorbidities.
-
3.
How to transfer symptoms into a feasible diagnostic hypothesis.
2.2 Key Autonomic Symptoms (Per Domain)
2.2.1 Cardiovascular Autonomic Dysfunction
2.2.1.1 How Does the Patient Complain About It
The key feature of cardiovascular autonomic impairment is “orthostatic intolerance,” eventually resulting in syncope. Syncope is defined as a transient, self-limited, loss of consciousness, which occurs when global cerebral perfusion is impaired [54].
The most frequent cause of syncope is vasovagal (reflex) syncope that is induced by a paroxysmal, abnormal cardiovagal outflow, coupled with sympathetic inhibition in otherwise healthy subjects, which results in cardioinhibition, vasodepression, or, more frequently, a combination of both. In vasovagal syncope, loss of consciousness is heralded by a 30–60s-lasting presyncopal phase in which signs of autonomic arousal and of cerebral and retinal hypoperfusion occur. In this premonitory phase, autonomic activation may cause warm feeling, cold sweat, yawning, drooling, abdominal discomfort, nausea, cramps, or the desire to sit down or leave the room [63]. If the subject reacts at this stage by sitting or lying down, onset of syncope can be prevented. Otherwise, symptoms of cerebral and retinal hypoperfusion like light-headedness, fatigue, blurred vision, graying out of colors, tinnitus, or palpitation develop. If cerebral perfusion remains under the critical level (below 60 mmHg) for longer than 7 s, the cerebral ischemic anoxia reserve is overruled, and loss of consciousness develops. Immediately before syncope occurs, subjects may turn pale and show pupil dilatation and inability to move. During syncope, postural tone is lost, and eyes are open: upward turning of the eyes, preceded by downbeat nystagmus, may occur. Loss of consciousness in syncope usually lasts 10–20s, but duration may be longer if cardioinhibition with prolonged asystole (up to 70s) develops. In this case, arrhythmic myoclonic jerks and loss of urine may be observed, whereas fecal incontinence is rare. Tongue biting, especially if sided, is also unusual in syncope and is rather indicative of seizures [54]. Immediately after cessation of syncope, flushing may occur, as well as moaning or growling. Recovery is typically quick in syncope (minutes), although fatigue, retrograde amnesia, sleepiness, or, to the contrary, euphoria or agitation may persist longer, especially in elderly patients.
Common triggers of vasovagal syncope are represented by prolonged standing position, warm ambient temperature, pain, vision of blood, needle phobia, or intense emotions. Autonomic activation may be also triggered by specific stimuli which originate in the gastrointestinal (swallowing, rectal examination, defecation), urogenital (micturition), or respiratory (cough, sneezing) tract, leading to a so-called situational syncope. Reflex vasovagal syncope may, rarely, have an atypical presentation, i.e., without the abovementioned prodroma. These are, in general, reported more frequently by female and younger subjects, probably due to more severe autonomic activation in the presyncopal phase, while older subjects may fail to recall premonitory symptoms, since they are more susceptible to retrograde amnesia.
Syncope occurring in aging individuals during neck manipulation or even upon mild stimuli such as head turning is suggestive of carotid sinus syndrome, that is, syncope associated with asystole >3 s or systolic blood pressure drop >50 mmHg upon carotid sinus stimulation, and should prompt further investigations, including carotid sinus massage [54].
Orthostatic hypotension (OH) is defined as an orthostatic blood pressure fall >20 mmHg systolic or >10 mmHg diastolic within 3 min of head-up tilt or standing [17]. It may also manifest with syncope, but since blood pressure fall is progressive and not abrupt in this case, patients more frequently complain of prolonged symptoms of cerebral and/or generalized hypoperfusion, including light-headedness, dizziness, fatigue, nausea, and cognitive slowing upon standing. Visual problems ranging from blurring to tunnel vision are also a common complaint, as well as, more rarely, scotomas and visual hallucinations due to occipital hypoperfusion [63]. Hypoperfusion in shoulder and neck muscles may result in head and neck pain with a characteristic “coat hanger” distribution. Altered blood supply may also trigger orthostatic dyspnea and angina in the absence of pulmonary and coronary artery disease. OH symptoms are typically alleviated by sitting or recumbent position and are exacerbated in the morning, after large meals, or with heat exposure [16].
If OH develops in the context of a primary autonomic disease (i.e., due to neurodegeneration of the ANS, like in α-synucleinopathies), this may be accompanied by supine and nocturnal hypertension in 30–50% of the patients [9, 11, 24]. Supine hypertension is mostly asymptomatic or manifests with supine headache, angina, or nocturia, but is important to be recognized, since pharmacological interventions for OH may exacerbate hypertensive crises and cause end-organ damage on the long term [10].
A peculiar form of OH is delayed OH, that is, OH manifesting during prolonged standing (i.e., after 3 min of orthostatic challenge). Delayed OH is not uncommon in the elderly, otherwise healthy, population: it presents with OH-typical symptoms after prolonged standing or walking and may trigger syncope due to reflex bradycardia. Recent studies suggest that delayed OH may otherwise represent a milder, initial form of classical OH, especially if associated with parkinsonism or diabetes [21, 42].
Initial OH is characterized by a transient blood pressure decrease immediately on standing >40 mmHg systolic and/or >20 mmHg diastolic. Afterwards blood pressure quickly normalizes, so that duration of presyncopal symptoms is short (<30 s), but may still cause syncope in some occasions (e.g., during heat exposure) [17].
Finally, palpitations, anxiety, panic attacks, chest discomfort, dyspnea, and migraine-like headache are typical symptoms that may be reported by patients suffering from postural orthostatic tachycardia syndrome (POTS) [33], another syndrome of orthostatic intolerance, characterized by a disproportionate increase in heart rate in response to orthostatic stress (>30 bpm within 10 min of standing with respect to baseline or standing heart rate >120 bpm), whereas little or no change in blood pressure occurs. A vasovagal reflex may superimpose in one third of patients, causing syncope or presyncope.
For physiology see Sect. 1.2.1, for clinical testing and management see Sect. 3.2.11
2.2.1.2 Can I Be Sure? Alternative Etiologies to Take into Account
Dizziness, fatigue, and neck pain are rather vague symptoms, but the occurrence with postural changes, followed by a prompt resolution with recumbency, is highly suggestive of orthostatic hypotension. In this clinical scenario, non-neurogenic causes of orthostatic intolerance should be ruled out. These include hypovolemia, as a consequence of diarrhea, emesis, or blood loss, among others, and use of drugs, such as diuretics, neuroleptics, antihypertensives, and other vasoactive agents. Adrenal insufficiency, systemic mastocitosis, and carcinoid syndrome are other less common causes of hypovolemia, either due to chronic volume depletion or vasodilation [16] (Table 2.1). In this case, simultaneous evaluation of blood pressure and heart rate during postural changes supports the diagnosis. Indeed, when hypovolemia occurs, the blood pressure drop upon standing is usually coupled with a compensatory increase in heart rate, which is usually blunted (<10 bpm) or absent in case of neurogenic OH.
Syncope is one cause of transient loss of consciousness (T-LOC), but other causes of T-LOC may represent a diagnostic challenge in clinical practice. Assessing the ultimate cause of syncope may also prove difficult. The diagnostic mainstay is a careful clinical history which should focus on triggers, e.g., sudden postural changes or prolonged standing, and warning symptoms. If an abrupt onset, without prodromal symptoms, is reported, cardiopulmonary causes of syncope should be promptly investigated. A variety of heart diseases such as tachy- or bradyarrhythmia, ischemia, and valvular or structural cardiopathy may manifest with syncope [3].
It may be particularly difficult to rule out generalized seizures, since myoclonic jerks may appear also in the setting of syncope, especially in case of prolonged asystole due to cardioinhibitory vasovagal activation [57]. However, myoclonic jerks tend to be few in number and arrhythmic in syncope, while they may last over minutes and show rhythmicity in generalized epileptic seizures.
Psychogenic disorders, like psychogenic non-epileptic seizures or psychogenic pseudosyncope, should be also taken into consideration in the differential diagnosis, especially if psychiatric comorbidities or emotional triggers can be pointed out at history taking, duration of unconsciousness is exaggeratedly long (up to 60 min), frequency of syncopal episodes is high, and atypical features are observed during the episode (e.g., eyelid flatter, swallowing).
Metabolic causes, like hypoglycemia, or more rare causes and mimicries of T-LOC like drop attacks or cataplexy should be also taken into account in the case of atypical presentation.
In elderly patients, history taking may be unclear or misleading, and a fall, due to postural instability, with consequent concussion and loss of consciousness, may be mistaken for a syncopal event. On the other hand, in older patients, fragile or with polypharmacy, orthostatic hypotension is also a frequent, treatable, cause for unexplained falls to be excluded.
Exercise intolerance due to cardiac autonomic neuropathy results from reduced response in heart rate and blood pressure during the strains. In this context, pre-existing left ventricular systolic dysfunction and silent ischemic coronary disease are to be ruled out. In particular, patients suffering from diabetic neuropathy may experience painless cardiac ischemia, because of reduced pain sensitivity [58].
In patients diagnosed with POTS, clinical workup should rule out iatrogenic causes (newly prescribed antihypertensive drugs other than β-blockers; high-dose antidepressants, especially SNRI and TCA; neuroleptics), hyperthyroidism, anemia, or more rare causes, like pheochromocytoma, or the presence of accessory conduction pathways as in Wolff-Parkinson-White syndrome [19].
2.2.2 Dermatological (Sweating and Vasomotor Disorders)
2.2.2.1 How Does the Patient Complain About Them
Thermoregulatory and sweating dysfunctions are often encountered in the setting of autonomic disorders. Both hypo- and hyperhidrosis (reduced and increased sweat production, respectively) may occur with a variable distribution.
Patients may complain of hypohidrosis as reduced tolerance to heat exposure and skin dryness. If global anhidrosis occurs, the inability of dissipating heat may, in turn, lead to hyperthermia with potentially fatal consequence [6].
Hyperhidrosis may manifest as drenching sweat, if the whole body is affected, or as localized sweating in the axillae, palms, soles of feet, and face. Secretomotor dysfunction may also cause gustatory sweating, which is a pathological sweating in response to stimuli that usually activate salivation, such as eating or food aroma [15].
Seborrhea may be reported, but causes other than dysautonomia, e.g., endocrinological, may be more relevant in its pathogenesis [37].
Alterations in skin vasomotor control are responsible for altered venous return, which results in peripheral edema, cold hands/feet, and Raynaud-like phenomena, with blueish or blanched extremities. Inappropriate vasodilation may manifest as paroxysmal cutaneous flushes.
In complex regional pain syndrome (formerly known as reflex sympathetic dystrophy), regional sweating and vasomotor abnormalities may occur together with sensory deficits, dystonic postures, and myoclonic jerks, following traumatic limb injury or without an apparent cause [8].
2.2.2.2 Can I Be Sure? Alternative Etiologies to Take into Account
Hypohidrosis occurs as a common side effect of drugs with anticholinergic properties such as tricyclic antidepressants, oxybutynin, and botulinum toxin, the latter being the treatment of choice for local hyperhidrosis. Sweating disturbances may be also caused by a variety of conditions, from alcohol or drug withdrawal to thyroid dysfunction. Hyperthyroidism is usually characterized by excessive sweating, while a reduced thyroid function is responsible for hypohidrosis and reduced heat tolerance. Drenching sweats may be a common sign of hypercatabolic states linked to systemic infections or neoplasms. Sweat glands may be involved in the course of primary dermatological disorders, vasculitis (Sjogren’s syndrome), or burns and radiation therapy, resulting in regional or global anhidrosis. Congenital dysplasia of ectodermal-derived tissues may be a fairly rare cause of anhidrosis in children [6].
2.2.3 Urogenital
2.2.3.1 How Does the Patient Complain About Them
Normal urinary function consists of a storage phase, in which the bladder detrusor is inactivated and activation of urethral sphincter muscles prevents urine leak, and a voiding phase, in which bladder detrusor contraction and urethral sphincter relaxation promote passing of urine. Both the storage and the voiding phase are under involuntary and voluntary control. Neurogenic disorders may result in a variable combination of detrusor overactivity or underactivity, with or without sphincter dysfunction [46, 60].
Impairment of the urinary storage phase results in nocturia, urinary frequency, and urgency, with or without incontinence.
Symptoms of voiding phase dysfunction are reported as feeling of incomplete bladder emptying and need for a double voiding, along with hesitancy and interrupted or poor stream. Since post-void urine residual volume increases in case of voiding impairment, retention and overflow incontinence may superimpose.
The abovementioned lower urinary tract symptoms usually worsen during the course of chronic autonomic disorders and may even shift, e.g., from a storage dysfunction to a voiding or mixed one over time [60]. Recurrent lower urinary tract infections, retrograde pyelonephritis, and eventually urosepsis are frequent complications of neurogenic bladder disturbances. In case of large post-void residual urine volume, hydronephrosis and bladder and kidney stones may also occur.
Sexual dysfunction frequently accompanies urological autonomic failure. Erectile dysfunction in men often remains undiagnosed, but it has been reported that isolated erectile dysfunction may precede urinary symptoms over years in atypical parkinsonian symptoms like multiple system atrophy, actually belonging to the earliest, though unspecific, premotor disease signs [14]. Ejaculatory disorders may also be reported, including premature or delayed ejaculation or complete absence of semen emission if retrograde ejaculation takes place. Women may complain either of genital hyposensitivity with anorgasmia or pain during sexual activity due to poor vaginal lubrication [39].
2.2.3.2 Can I Be Sure? Alternative Etiologies to Take into Account
Lower urinary tract symptoms are a frequent complaint in the aging population of both genders, resulting from structural to functional disorders of the pelvic district, and clinical manifestations may overlap with those of urogenital autonomic failure.
Laboratory tests to exclude urinary tract infections are mandatory in case of acute onset of lower urinary tract symptoms, especially if dysuria is present, since infection is the most common, reversible cause. On the other hand, when recurrent infections occur, an underlying urodynamic disturbance should be excluded.
The most common etiology for lower urinary tract symptoms in men is represented by benign prostatic hyperplasia, whose prevalence has an exponential rise from the sixth decade of life. Obstructive symptoms, like poor or interrupted stream with hesitancy, are the most frequent complaints, but frequency and urgency can occur, as well as incomplete emptying and retention, in the case of superimposing atonic bladder [18].
In women, urinary symptoms may develop as a consequence of pelvic floor relaxation and prolapses, especially after multiple labors, or in the presence of pelvic masses and scars.
Major pelvic surgery or pelvic radiation may produce urogenital symptoms in both sexes.
Bladder dysfunction occurring together with low-back pain, saddlelike sensory deficit, and variable motor and sensory loss in the lower extremities, is highly suspicious for a cauda equina syndrome and should prompt further investigation to rule out caudal entrapment (vertebral disc prolapses, fractures, neoplasms).
Aging is accompanied by an exponential increase in sexual disturbances as a result of multiple pathophysiological mechanisms. Poor vaginal lubrication or pain during sexual intercourse in a postmenopausal woman may reflect genital atrophy due to the physiological reduction in hormone levels. Chronic diseases, medications, and atherosclerotic changes may underlie an erectile dysfunction in older men. Thyroid disorders, prolactinomas, and gonadic hormone deficiency may manifest with sexual dysfunction, among others. Classical cardiovascular risk factors like smoking, hypertension, and dyslipidemia are further risk factors for erectile dysfunction of vascular origin. Failure in both erection and ejaculation phases may also occur as a consequence of prostate surgery or radiotherapy. Retrograde ejaculation is a recognized side effect of many drugs, especially sympatholytic agents.
2.2.4 Gastrointestinal
2.2.4.1 How Does the Patient Complain About Them
Symptoms of gastrointestinal autonomic dysfunction may arise at every level of the gastrointestinal tract and are divided into symptoms of the upper and of the lower gastrointestinal tract. Autonomic dysfunction of the upper gastrointestinal tract may manifest with:
-
1.
Xerostomia, which is a complaint of dry mouth, due to reduced saliva production.
-
2.
Drooling, an excessive pooling of saliva that flows out of the mouth. Drooling is often reported by patients suffering from parkinsonian syndromes, but in this context, it is mainly related to impaired deglutition, and it can even coexist with xerostomia in up to 30% of the patients [5].
-
3.
Delayed bolus transit in esophagus, which may manifest with regurgitation and dysphagia.
-
4.
Delayed gastric emptying, presenting with bloating, belching, and early satiety. Gastroparesis may also cause nausea, postprandial vomiting, and anorexia.
Symptoms of the lower gastrointestinal tract may produce a variety of symptoms. Constipation and colic pain are by far the most reported. A long-standing constipation may, in turn, promote bacterial overgrowth, which results in intermittent diarrhea. Apart from constipation, dissynergic contraction of pelvic muscles and anal sphincter may contribute to evacuation difficulties or to involuntary loss of stool [13]. Rarely, focal dystonia of the striated anal sphincter may result in refractory constipation [26].
2.2.4.2 Can I Be Sure? Alternative Etiologies to Take into Account
A detailed pharmacological anamnesis is the first step in the evaluation of salivary disturbances. Dry mouth is a common side effect of anticholinergic drugs, whereas benzocaine (contained in cough drops and over-the-counter medications for mouth ulcers) may cause sialorrhea. Xerostomia is a key feature of Sjögren’s disease and associated connective tissue disorders. Dryness may involve also the eyes both in Sjogren’s disease and autonomic failure. Reduced salivary production may follow surgery and radiotherapy for head and neck tumors. Drooling is frequently encountered in the setting of altered neuromuscular control of swallowing, such as bulbar form of amyotrophic lateral sclerosis, myasthenia gravis, or cerebral palsy.
Symptoms of chronic, delayed bolus transit may result from anatomical obstructions and should prompt exclusion of malignancies. Mesenteric vascular insufficiency should also be considered as a likely cause of gastroparesis in the elderly. Medications (Ca2+ blockers, antidepressants) and metabolic disturbances (hypothyroidism and hypercalcemia) should be excluded as common causes of chronic constipation. Rare etiologies for obstructive colonic symptoms are represented by Chagas’ disease and Hirschsprung’s disease, respectively, an infective and hereditary cause of enteric nervous system degeneration. Systemic sclerosis with visceral involvement may also be a rare case of gastrointestinal obstruction, especially at esophageal level.
2.2.5 Respiration and Sleep
2.2.5.1 How Does the Patient Complain About Them
Respiratory symptoms may be an early manifestation of autonomic failure in patients with multiple system atrophy (MSA), though commonly associated with advanced stages and, overall, constituting a poor prognostic predictor [25]. Obstructive sleep apnea is generally an early manifestation, while central sleep apnea may develop later on, when degeneration of brainstem breathing relays occurs [48]. Sleep-related breathing disorders are typically reported by the patient’s bed partner, while the patient himself may be less aware of them. These include enhanced or new-onset snoring and stridor, a harsh and strained high-pitched inspiratory sound that occurs especially, but not only, at nighttime, which is due to pathological adduction of the vocal cords and is typically accompanied by chronic dysphonia. Sleep is not restorative in these patients, who also complain about sleepiness and sleep attacks during daytime.
In patients with severely impaired central respiratory drive, awake breathing rhythm alterations, like periodic inspiratory gasps or agonic respiratory patterns, may occur, as well as respiratory insufficiency of “pump failure” type [35].
2.2.5.2 Can I Be Sure? Alternative Etiologies to Take into Account
When sleep-related disorders precede other autonomic or motor manifestations, they cannot be distinguished from idiopathic sleep-related disordered breathing. Anecdotal reports of surgical intervention for snorers, who were eventually diagnosed with multiple system atrophy (MSA), underline the importance of a careful differential diagnosis [25].
Chronic stridor and other inspiratory disorders result from a partial obstruction of the upper respiratory tract, usually at glottic or supraglottic levels [38]. Clinical examination by the otorhinolaryngologist is required to exclude neoplastic, cystic, or inflammatory lesions of the larynx. Extrinsic stenosis may be caused by disorders of the adjacent structures, such as thyroid goiter or cancer, or result from neck surgery and radiotherapy. Soft tissue swelling secondary to acromegaly is a less common cause of obstruction and sleep apnea. Unilateral vocal cord palsy may be caused by chest or mediastinal neoplasm entrapping the recurrent laryngeal nerve or by accidental lesion of the recurrent laryngeal nerve during thyroid surgery.
2.2.6 Ophthalmological Autonomic Dysfunction
2.2.6.1 How Does the Patient Complain About It
Autonomic disorders may affect both lacrimation and pupillomotor function. Patients may complain of xerophthalmia, dry eyes, which results from impaired cholinergic stimulation of lacrimal glands.
Reduced nocturnal visual acuity and blurred vision, photophobia, and involuntary eyelid closure to light are typical symptoms of altered pupillomotor function due to impaired iris dilation and pupil light reflex, respectively [67]. Basal alterations of pupil diameter or altered pupillary response to cholinomimetic or sympathomimetic drugs are usually not noted by the patients [65].
2.2.6.2 Can I Be Sure? Alternative Etiologies to Take into Account
Eye dryness is a cardinal feature of Sjögren’s disease. Autonomic failure is not frequent in Sjogren’s disease, although cases with severe cardiovascular autonomic failure have been described [49]. Incomplete eyelid closure, e.g., after facial nerve palsy or previous injuries with scarring, is a mechanical cause of eye dryness to be excluded. Xerophthalmia is a classical manifestation of vitamin A deficiency, by now a rare finding in developed countries.
Diminished night vision is frequently reported as a consequence of cataract, typically in elderly subjects, but other causes include a variety of retinal disorders, like diabetic retinopathy, among others. Photophobia may occur in association with cataract and corneal or vitreous disturbances or as a side effect of refractive surgery.
2.2.7 Useful Screening Tools: Autonomic Questionnaires
Standardized questionnaires represent a useful tool to assess and rate the severity of autonomic symptoms. The most suitable one should be chosen among the validated available scales on the basis of physician’s purpose. The Composite Autonomic Symptom Scale (COMPASS) and the Composite Autonomic Scoring Scale (CASS) have been developed to introduce a scoring system of autonomic symptoms’ severity and a correlation with autonomic function tests, respectively. The COMPASS is a self-administered survey, consisting of 84 items, and has been validated in a variety of autonomic disorders. A shorter version, the COMPASS-31, has been also developed [50].
The orthostatic hypotension questionnaire (OHQ) is a ten-item scale, purposely developed to assess severity of symptoms due to orthostatic hypotension and their impact on daily activity [27].
Specific questionnaires have been developed to evaluate autonomic symptoms in different diseases. The Scales for Outcomes in Parkinson’s Disease-Autonomic (SCOPA-AUT), a self-administered, brief questionnaire which covers cardiovascular, gastrointestinal, urinary, thermoregulatory, pupillomotor, and sexual domains, is recommended for patients with Parkinson’s disease [41]. The Unified Multiple System Atrophy Rating Scale (UMSARS) evaluates severity of motor and autonomic symptoms in patients with multiple system atrophy and can be used to monitor disease progression as well. Questions about disease-specific autonomic symptoms are included in UMSARS part I, a broader historical review, and results of quick orthostatic challenge test are reported in UMSARS part III [61].
2.3 Other Important Clues from History Taking
2.3.1 Time Course: Episodic/Situational, Acute, Subacute, and Chronic Symptoms
The mode of onset and the time course of autonomic symptoms provide essential clues for an etiological diagnosis. An episodic time course is, for example, typical of orthostatic and situational vasovagal syncope, where triggering or exacerbating factors can be pointed out at history taking. An acute or subacute onset of autonomic disturbances usually prompts to an immune etiology, such as acute inflammatory demyelinating polyradiculoneuropathy (AIDP), acute autonomic ganglionopathy, or a paraneoplastic syndrome. An AIDP, also known as Guillain-Barré syndrome, manifests with ascending flaccid paralysis and areflexia, frequently after an infectious illness. It has a monophasic evolution, usually without recurrence, and severe autonomic disturbances, such as arrhythmia and marked hypo- and hypertensive peaks, may occur in up to 20% of the patients during the disease course [68].
An acute monophasic time course, frequently followed by spontaneous remission or stabilization, as well as a premorbid report of infectious illnesses is suggestive of acute autonomic ganglionopathy, while in paraneoplastic syndromes, a subacute onset, often preceding the diagnosis of malignancies, is common.
Isolated attacks with generalized or organ-specific autonomic dysfunction may occur as a consequence of drug or toxin exposure, such as organophosphate pesticides. Autonomic crises are also a typical feature of some rare diseases with autonomic nerve involvement such as Riley-Day syndrome and porphyria.
A chronic, progressive course of autonomic symptoms points towards a degenerative pathology of the autonomic nervous system which may occur alone, as in pure autonomic failure, or in combination with additional neurological features as in MSA, Parkinson’s disease, and dementia with Lewy bodies. Autonomic failure is typically progressive and ranges from milder manifestation in Parkinson’s disease to severe dysautonomia in pure autonomic failure and multiple system atrophy [55].
2.3.2 Age and Gender
With the exception of vasovagal syncope, which may also occur in otherwise healthy children, disease onset in the childhood or teenage points toward a genetic cause.
In the age range from 10 to 30 years, up to 47% of the females and 31% of the males experience at least one syncopal episode, vasovagal syncope being by far the most common etiology. Syncope shows a second peak of incidence after the age of 65, with cardiopulmonary causes playing a key role in this age cluster [54].
POTS and vasovagal syncope show a striking female prevalence, usually affecting young women in childbearing age [19].
Primary forms of autonomic failure are characterized by a sporadic adult onset in the sixth or seventh decade [56, 62]. MSA and pure autonomic failure have a similar incidence in both genders, while Parkinson’s disease has a 1.5 times higher male prevalence. Recent evidence suggests that some autonomic symptoms in Parkinson’s disease may be more frequent and progredient in male patients [52]. In secondary autonomic failure, the gender prevalence and the age of onset depends on the underlying causative disease. Thus, like other autoimmune disorders, AAG may more frequently affect female patients in their young or middle adulthood, while diabetic and uremic neurogenic OH typically affect older individuals.
The presentation of autonomic disturbances itself may be also influenced by age. For instance, orthostatic intolerance more often features light-headedness in the young and cognitive slowing in the elderly [32].
2.3.3 Family History
Autonomic failure may occur in a number of rare genetic diseases including familial amyloidosis, Fabry disease, hereditary sensory autonomic neuropathies, and porphyrias [15]. The main presentation is a peripheral neuropathy with both autonomic and sensory deficits. Additional manifestations and familial recurrence pattern are helpful clues to address genetic testing.
Familial amyloidosis is an autosomal dominant inherited disease, caused by mutations in the gene coding for transthyretin. Like in acquired forms of amyloidosis, the aberrant form of transthyretin accumulates in different organs. Peripheral nerves are the second most common site of deposition after cardiovascular system, and this accounts for the frequent autonomic and sensitive neuropathic manifestations.
Fabry disease is due to an X-linked mutation in the enzyme α-galactosidase A that leads to lysosomal accumulation of glycosphingolipids. It manifests with early-onset heart failure, renal failure, and stroke. Neuropathic involvement results in painful crises and sweating disorders. According to its X-linked genetics, Fabry disease affects predominantly male patients, but heterozygous female carriers may also become symptomatic [44].
Hereditary sensory autonomic neuropathies (HSAN) are currently classified in five forms on the basis of the genetic substrate and clinical presentation. They usually feature mixed autonomic and sensory manifestations with the exception of HSAN III. This form, also known as Riley-Day syndrome or familial dysautonomia, shows a selective absence of unmyelinated fibers and manifests as isolated autonomic crises with onset in the childhood [40].
Isolated sympathetic noradrenergic failure is the unique manifestation of dopamine β-hydroxylase deficiency, a rare genetic disorder with autosomal recessive transmission [45]. It selectively impairs conversion of dopamine into noradrenaline in peripheral nerves; thus, parasympathetic and sympathetic cholinergic functions (sweating) are normally preserved. The usual presentation is a combination of orthostatic hypotension and eyelid ptosis in children.
2.3.4 Comorbidities: Main Suspects
In patient with polypharmacy, the first step is to review drug schedules for potential offending drugs, especially if recent changes have been applied. As mentioned before, high-dose antihypertensive or psychotropic drugs are the main cause of new-onset OH. Anticholinergic drugs, either for treatment of bladder detrusor overactivity or for symptomatic treatment of parkinsonism and dystonia, may in turn induce xerostomia, accommodation difficulties, gastrointestinal dysmotility, and atonic bladder.
Secondary involvement of ANS is far more common than primary autonomic disorders; thus, exclusion of metabolic or immunologic etiologies is a key step in the diagnostic workup.
Fasting blood glucose and glycated hemoglobin levels should always be checked as diabetes mellitus is a leading cause of autonomic neuropathy, and an altered glycemic control represents its strongest predictor [58]. Autonomic neuropathy may also arise in the setting of uremia, liver disorders, chemotherapy, neck or thoracic radiotherapy, and nutritional deficiencies.
A panel of immunological test may be performed to exclude autoimmune conditions with secondary dysautonomia, such as Sjögren’s disease, rheumatoid arthritis, and systemic lupus erythematosus.
Borreliosis, leprosy, botulism, syphilis, and HIV infection may also present with autonomic neuropathy. Autonomic involvement during infectious illness may be a consequence of direct microbial neurotropism, neurotoxin production, or autoimmunity triggered by molecular mimicry. The latter is the likely mechanism which underlies post-infectious acute autoimmune demyelinating polyneuropathy.
Subacute onset of autonomic symptoms without other apparent causes in middle-aged individuals should rise suspicion for an occult neoplasm. Different mechanisms may account for ANS involvement in cancer, including direct infiltration, chemotherapy-related toxicity, nutritional alterations, or, in the absence of the previous, paraneoplastic manifestation [2] . Paraneoplastic autonomic syndromes frequently present together with sensory neuropathy. The autoantibody most commonly associated is anti-Hu; others are anti-PCA-2 and anti-CRMP-5 [16]. Small-cell lung cancer is present in more than 80% of the seropositive patients, but autonomic and sensory deficits may antedate the tumor diagnosis, which, when found, tends to be localized and treatment responsive. History taking should focus on suggestive features like tobacco consumption, nocturnal sweating, or unexplained weight loss, and a total body scan should be performed.
2.3.5 Additional Neurological Signs
Autonomic dysfunction may occur isolated or, more often, as a part of a disorder with a broader neurologic presentation. As mentioned above, sensory neuropathy accompanies autonomic failure in hereditary sensory autonomic neuropathies and, frequently, in paraneoplastic syndromes.
Diabetic peripheral neuropathy usually presents with a mixed autonomic and distal sensorimotor phenotype. Sweating and vasomotor abnormalities occur along with pain, numbness, paresthesia, areflexia, and weakness which spread from the extremities in a length-dependent fashion [4].
In neurodegenerative disorders of the central nervous system, autonomic failure is part of a complex presentation which may include parkinsonism, ataxia, pyramidal signs, and dementia. A combination of these features along with the severity of dysautonomia guides the differential diagnosis, which may be particularly difficult prior to develop a full-blown clinical picture (Fig. 2.1).
2.4 From Autonomic Symptoms to a Diagnostic Hypothesis
2.4.1 Primary Autonomic Diseases
Autonomic failure is a key feature of a group of sporadic neurodegenerative disorders, whose pathological hallmark is represented by α-synuclein inclusions. α-synuclein accumulates within oligodendroglial cytoplasmic inclusion in MSA, and within neuronal cytoplasmic inclusions, the so-called Lewy bodies, in PD, dementia with Lewy bodies and pure autonomic failure. α-synuclein accumulates within oligodendroglial cytoplasmic inclusion in MSA and inside neuronal somas, Lewy bodies, or Lewy neurites, among others.
MSA is a progressive, fatal disorder which features parkinsonism, cerebellar and pyramidal symptoms, and autonomic failure in various combinations. Autonomic failure is an early and prominent manifestation which is underlain by a likewise conspicuous neurodegeneration over hypothalamus, noradrenergic and serotoninergic brainstem nuclei, and intermediolateral columns in the spinal cord [12].
A diagnosis of probable MSA requires the presence of urogenital dysautonomia (urinary incontinence plus erectile dysfunction in men) or an orthostatic fall by at least 30 mmHg in systolic or 15 mmHg in diastolic blood pressure within 3 min of standing or head-up tilt [23]. Further features of dysautonomia in MSA are represented by generalized hypo- or anhidrosis, stridor, and sleep-related breathing disturbances [31]. The association of these features with a poorly levodopa-responsive parkinsonism or a sporadic adult-onset cerebellar ataxia is highly suggestive of MSA.
The parkinsonian variant of MSA may be easily mistaken for idiopathic PD, especially at disease onset [31]. Autonomic failure in PD is milder and usually a later manifestation. Neuropathological changes involve both central autonomic nuclei and, to a greater extent, peripheral autonomic relays. Constipation is a common premotor manifestation of PD [1] and one of the most reported non-motor symptoms. A variety of urinary complaints, and particularly nocturia, may be present in up to 75% of the patients with PD [46]. Prevalence of OH is 30% in PD, ranging from 14% in drug-naïve patients to 52% in advanced stage of the disease [10].
Dementia with Lewy bodies is defined by the presence of progressive dementia with fluctuating cognition and parkinsonism [34]. The burden of autonomic dysfunction is considered intermediate between MSA and Parkinson’s disease [55]. A high prevalence of carotid sinus hypersensitivity has been reported in patients with dementia with Lewy bodies [28].
Pure autonomic failure is a rare α-synucleinopathy which is defined by the presence of isolated autonomic disturbances, mainly severe OH, without additional neurological features. α-Synuclein mainly accumulates in peripheral autonomic nerves in pure autonomic failure [20]. Many cases of pure autonomic failure may develop parkinsonism or cognitive impairment during the disease course, eventually evolving into PD, MSA, or dementia with Lewy bodies. Pure autonomic failure is settled at the extremity of a spectrum in α-synuclein distribution pattern, since it selectively involves peripheral ANS and spares the central nervous system.
Autonomic failure has been also reported in τ-pathies like progressive supranuclear palsy and frontotemporal dementia.
Progressive supranuclear palsy is an atypical parkinsonism, characterized by poor L-dopa responsiveness, vertical gaze palsy, and frequent falls. Three years after disease onset, urinary urge or incontinence has been reported in 54% of the patients [7]. Occurrence of OH in progressive supranuclear palsy is debated, with some studies reporting similar prevalence of OH like in PD, but others not confirming this observation [29, 47].
The presence of cardiovascular autonomic failure was recently reported in patients with frontotemporal dementia, another τ-pathy characterized by severe cognitive impairment, behavioral abnormalities, and signs of first and second motor neuron degeneration in different combinations. In these patients, the presence of OH may remain underdiagnosed, due to inability of the patient to communicate symptoms [51].
A new entity, the cerebellar ataxia, neuropathy, and vestibular areflexia syndrome (CANVAS), has been recently described and is pointed as a further cause of autonomic dysfunction [64]. The presentation with cerebellar ataxia and autonomic symptoms may mislead to a diagnosis of MSA cerebellar variant, but the presence of a sensory neuronopathy such as a more benign course may be supportive. Both autonomic and sensory symptoms probably result from a degenerative ganglionopathy, as suggested by neuropathological studies [53].
2.4.2 Secondary Autonomic Diseases
A variety of systemic illnesses may affect the peripheral nervous system and produce autonomic symptoms. Chronic alcohol consumption, metabolic disorders, autoimmunity, or toxins are among the implicated factors.
One of the main causes of secondary autonomic dysfunction, as mentioned above, is represented by diabetes mellitus. Autonomic neuropathy is one of the multifaceted manifestations of peripheral nervous system involvement in diabetes, which also includes distal sensory motor neuropathy and mononeuropathies. Reports on prevalence and time onset are contrasting; even if autonomic neuropathy is usually a complication of a long-standing diabetes, it may appear within a year from the diagnosis in type 2 and within 2 years in type 1 diabetes patients [43]. Poor glycemic control seems to be crucial in its development [22, 69]. The manifestations may range from a global autonomic failure to an asymptomatic dysfunction which may be detected when autonomic tests are performed. When autonomic involvement appears in the context of a classical distal neuropathy, hypo- or anhidrosis and vasomotor disturbances develop together with sensory disturbances in the extremities. Visceral involvement manifests as gastroparesis, which may be particularly severe, alternating constipation and diarrhea, cystopathy, and erectile dysfunction [58]. Strict glucose and glycated hemoglobin targets should be avoided in these patients, since loss of sympathetic activation during hypoglycemia may result in hypoglycemia unawareness and a higher risk of hypoglycemic coma. Cardiovascular autonomic neuropathy may also develop, carrying along a higher overall mortality and morbidity [59]. Symptoms of cardiovascular dysfunction in diabetes are represented by resting tachycardia, orthostatic hypotension, reduced tolerance to exercise, and painless myocardial ischemia.
Sjögren’s syndrome is often associated with neuropathic autonomic manifestations, the most prevalent being pupillomotor abnormalities, sweating reduction, and orthostatic hypotension. These may appear in the setting of a pure autonomic neuropathy or as an additional feature of sensory ataxia and painful or trigeminal neuropathies. Interestingly, these manifestations may frequently precede the diagnosis of sicca syndrome [36].
Peripheral neuropathies with autonomic manifestations may also arise in the absence of obvious underlying disorders. The frequent detection of autoantibodies, as well as the clinical overlap with acute inflammatory demyelinating polyneuropathy or paraneoplastic syndromes, has pointed towards an immunological etiology of these conditions. Different entities have been described on the basis of clinical presentation, which may range from an exclusive autonomic dysfunction to mixed autonomic and sensory or sensory motor manifestations [30]. The best characterized entity is represented by autoimmune autonomic ganglionopathy (AAG), previously known as acute pandysautonomia [66]. AAG is associated in up to 50% of the patients with an antiganglionic acetylcholine receptor antibody, which probably plays a direct pathogenetic role as autoantibody levels are closely related to disease severity and remission. The disease usually features an almost exclusive autonomic presentation with orthostatic intolerance and gastrointestinal dysmotility as a prominent manifestations [30].
Take Home Messages
-
Autonomic disorders have a multifaceted presentation which may overlap with common non-autonomic medical conditions. A careful history taking and examination is the first milestone to guide clinical work-up.
-
The early onset of a progressive, severe autonomic failure in the setting of a parkinsonian or a cerebellar syndrome is highly suggestive for multiple system atrophy
-
Autonomic disturbances feature in a variety of peripheral neuropathies secondary to acquired or congenital metabolic disorders (e.g. diabetes, Fabry’ disease), autoimmune diseases (Sjogren’s syndrome, systemic lupus erythematosus), toxic or infectious causes.
-
An acute or subacute onset of autonomic symptoms should prompt exclusion of a paraneoplastic cause. An autoantibodies panel and ad hoc imaging studies should be performed.
References
Adams-Carr KL, Bestwick JP et al (2015) Constipation preceding Parkinson’s disease: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 87(7):710–716
Antoine JC, Camdessanche JP (2007) Peripheral nervous system involvement in patients with cancer. Lancet Neurol 6(1):75–86
Brignole M (2007) Diagnosis and treatment of syncope. Heart 93(1):130–136
Callaghan BC, Cheng HT et al (2012) Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol 11(6):521–534
Cersosimo MG, Raina GB et al (2011) Dry mouth: an overlooked autonomic symptom of Parkinson’s disease. J Parkinsons Dis 1(2):169–173
Cheshire WP, Freeman R (2003) Disorders of sweating. Semin Neurol 23(4):399–406
Colosimo C, Morgante L et al (2010) Non-motor symptoms in atypical and secondary parkinsonism: the PRIAMO study. J Neurol 257(1):5–14
de Boer RD, Marinus J et al (2011) Distribution of signs and symptoms of complex regional pain syndrome type I in patients meeting the diagnostic criteria of the International Association for the Study of Pain. Eur J Pain 15(8):830 e831–830 e838
Fanciulli A, Gobel G et al (2016) Supine hypertension in Parkinson’s disease and multiple system atrophy. Clin Auton Res 26(2):97–105
Fanciulli A, Strano S et al (2013) The potential prognostic role of cardiovascular autonomic failure in alpha-synucleinopathies. Eur J Neurol 20(2):231–235
Fanciulli A, Strano S et al (2014) Detecting nocturnal hypertension in Parkinson’s disease and multiple system atrophy: proposal of a decision-support algorithm. J Neurol 261(7):1291–1299
Fanciulli A, Wenning GK (2015) Multiple-system atrophy. N Engl J Med 372(14):1375–1376
Fasano A, Visanji NP et al (2015) Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol 14(6):625–639
Fowler CJ (2007) Update on the neurology of Parkinson’s disease. NeurourolUrodyn 26(1):103–109
Freeman R (2005) Autonomic peripheral neuropathy. Lancet 365(9466):1259–1270
Freeman R (2008) Clinical practice. Neurogenic orthostatic hypotension. N Engl J Med 358(6):615–624
Freeman R, Wieling W et al (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21(2):69–72
Gacci M, Eardley I et al (2011) Critical analysis of the relationship between sexual dysfunctions and lower urinary tract symptoms due to benign prostatic hyperplasia. Eur Urol 60(4):809–825
Garland EM, Celedonio JE et al (2015) Postural tachycardia syndrome: beyond orthostatic intolerance. Curr Neurol Neurosci Rep 15(9):60
Garland EM, Hooper WB et al (2013) Pure autonomic failure. Handb Clin Neurol 117:243–257
Gibbons CH, Freeman R (2015a) Clinical implications of delayed orthostatic hypotension: a 10-year follow-up study. Neurology 85(16):1362–1367
Gibbons CH, Freeman R (2015b) Treatment-induced neuropathy of diabetes: an acute, iatrogenic complication of diabetes. Brain 138(Pt 1):43–52
Gilman S, Wenning GK et al (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71(9):670–676
Goldstein DS, Pechnik S et al (2003) Association between supine hypertension and orthostatic hypotension in autonomic failure. Hypertension 42(2):136–142
Jecmenica-Lukic M, Poewe W et al (2012) Premotor signs and symptoms of multiple system atrophy. Lancet Neurol 11(4):361–368
Jost WH, Muller-Lobeck H et al (1998) Involuntary contractions of the striated anal sphincters as a cause of constipation: report of a case. Dis Colon Rectum 41(2):258–260
Kaufmann H, Malamut R et al (2012) The Orthostatic Hypotension Questionnaire (OHQ): validation of a novel symptom assessment scale. Clin Auton Res 22(2):79–90
Kenny RA, Shaw FE et al (2004) Carotid sinus syndrome is common in dementia with Lewy bodies and correlates with deep white matter lesions. J Neurol Neurosurg Psychiatry 75(7):966–971
Kimber J, Mathias CJ et al (2000) Physiological, pharmacological and neurohormonal assessment of autonomic function in progressive supranuclear palsy. Brain 123(Pt 7):1422–1430
Koike H, Watanabe H et al (2013) The spectrum of immune-mediated autonomic neuropathies: insights from the clinicopathological features. J Neurol Neurosurg Psychiatry 84(1):98–106
Kollensperger M, Geser F et al (2008) Red flags for multiple system atrophy. Mov Disord 23(8):1093–1099
Low PB, Benarroch EE (2008) Clinical autonomic disorders. Wolters Kluver-Lippincott- Williams & Wilkins, Philadelphia
Mathias CJ, Low DA et al (2012) Postural tachycardia syndrome--current experience and concepts. Nat Rev Neurol 8(1):22–34
McKeith IG, Dickson DW et al (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65(12):1863–1872
Meissner WG, Vital A et al (2010) Dyspnea as first sign of autonomic failure in postmortem confirmed multiple system atrophy. Mov Disord 25(12):1997–1998
Mori K, Iijima M et al (2005) The wide spectrum of clinical manifestations in Sjogren’s syndrome-associated neuropathy. Brain 128(Pt 11):2518–2534
Mostile G, Jankovic J (2009) Treatment of dysautonomia associated with Parkinson’s disease. Parkinsonism Relat Disord 15(Suppl 3):S224–S232
Novakovic D, MacKay S (2015) Adult obstructive sleep apnoea and the larynx. Curr Opin Otolaryngol Head Neck Surg 23(6):464–469
Oertel WH, Wachter T et al (2003) Reduced genital sensitivity in female patients with multiple system atrophy of parkinsonian type. Mov Disord 18(4):430–432
Pareyson D, P Saveri, et al (2014) Charcot-Marie-Tooth disease and related hereditary neuropathies: from gene function to associated phenotypes. Curr Mol Med. PMID: 25323870
Pavy-Le Traon A, Amarenco G et al (2011) The Movement Disorders task force review of dysautonomia rating scales in Parkinson’s disease with regard to symptoms of orthostatic hypotension. Mov Disord 26(11):1985–1992
Pavy-Le Traon A, Piedvache A et al (2015) New insights into orthostatic hypotension in multiple system atrophy: a European multicentre cohort study. J Neurol Neurosurg Psychiatry 87(5):554–561
Pfeifer MA, Weinberg CR et al (1984) Autonomic neural dysfunction in recently diagnosed diabetic subjects. Diabetes Care 7(5):447–453
Ranieri M, Bedini G et al (2016) Fabry disease: recognition, diagnosis, and treatment of neurological features. Curr Treat Options Neurol 18(7):33
Robertson D, Haile V et al (1991) Dopamine beta-hydroxylase deficiency. A genetic disorder of cardiovascular regulation. Hypertension 18(1):1–8
Sakakibara R, Panicker J et al (2015) A guideline for the management of bladder dysfunction in Parkinson’s disease and other gait disorders. NeurourolUrodyn 35(5):551–563
Schmidt C, Herting B et al (2008) Autonomic dysfunction in patients with progressive supranuclear palsy. Mov Disord 23(14):2083–2089
Shimohata T, Shinoda H et al (2007) Daytime hypoxemia, sleep-disordered breathing, and laryngopharyngeal findings in multiple system atrophy. Arch Neurol 64(6):856–861
Shimoyama M, Ohtahara A et al (2002) Isolated autonomic cardiovascular neuropathy in a patient with primary Sjogren syndrome: a case of successful treatment with glucocorticoid. Am J Med Sci 324(3):170–172
Sletten DM, Suarez GA et al (2012) COMPASS 31: a refined and abbreviated Composite Autonomic Symptom Score. Mayo Clin Proc 87(12):1196–1201
Struhal W, Javor A et al (2014) The phoenix from the ashes: cardiovascular autonomic dysfunction in behavioral variant of frontotemporal dementia. J Alzheimers Dis 42(3):1041–1046
Szewczyk-Krolikowski K, Tomlinson P et al (2014) The influence of age and gender on motor and non-motor features of early Parkinson’s disease: initial findings from the Oxford Parkinson Disease Center (OPDC) discovery cohort. Parkinsonism Relat Disord 20(1):99–105
Szmulewicz DJ, McLean CA et al (2014) Dorsal root ganglionopathy is responsible for the sensory impairment in CANVAS. Neurology 82(16):1410–1415
Task Force for the Diagnosis and Management of Syncope et al (2009) Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 30(21):2631–2671
Thaisetthawatkul P, Boeve BF et al (2004) Autonomic dysfunction in dementia with Lewy bodies. Neurology 62(10):1804–1809
Twelves D, Perkins KS, Counsell C. Systematic review of incidence studies of Parkinson’s disease. Mov Disord. 2003;18(1):19–31.
van Dijk JG, Thijs RD et al (2014) The semiology of tilt-induced reflex syncope in relation to electroencephalographic changes. Brain 137(Pt 2):576–585
Vinik AI, Maser RE et al (2003) Diabetic autonomic neuropathy. Diabetes Care 26(5):1553–1579
Vinik AI, Ziegler D (2007) Diabetic cardiovascular autonomic neuropathy. Circulation 115(3):387–397
Vodusek DB (2014) Lower urinary tract and sexual dysfunction in neurological patients. Eur Neurol 72(1–2):109–115
Wenning GK, Tison F et al (2004) Development and validation of the Unified Multiple System Atrophy Rating Scale (UMSARS). Mov Disord 19(12):1391–1402
Wickremaratchi MM, Perera D, O’Loghlen C, Sastry D, Morgan E, Jones A, Edwards P, Robertson NP, Butler C, Morris HR, Ben-Shlomo Y. Prevalence and age of onset of Parkinson’s disease in Cardiff: a community based cross sectional study and meta-analysis. J Neurol Neurosurg Psychiatry. 2009;80(7):805–7.
Wieling W, Thijs RD et al (2009) Symptoms and signs of syncope: a review of the link between physiology and clinical clues. Brain 132(Pt 10):2630–2642
Wu TY, Taylor JM et al (2014) Autonomic dysfunction is a major feature of cerebellar ataxia, neuropathy, vestibular areflexia ‘CANVAS’ syndrome. Brain 137(Pt 10):2649–2656
Yamashita F, Hirayama M et al (2010) Pupillary autonomic dysfunction in multiple system atrophy and Parkinson’s disease: an assessment by eye-drop tests. Clin Auton Res 20(3):191–197
Young RR, Asbury AK et al (1975) Pure pan-dysautonomia with recovery. Description and discussion of diagnostic criteria. Brain 98(4):613–636
Yuan D, Spaeth EB et al (2014) Disproportionate pupillary involvement in diabetic autonomic neuropathy. Clin Auton Res 24(6):305–309
Yuki N, Hartung HP (2012) Guillain-Barre syndrome. N Engl J Med 366(24):2294–2304
Ziegler D, Behler M et al (2015) Near-normoglycaemia and development of neuropathy: a 24-year prospective study from diagnosis of type 1 diabetes. BMJ Open 5(6):e006559
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Fanciulli, A., Indelicato, E., Wenning, G.K. (2017). Autonomic History Taking and Key Symptoms: Where Is the Autonomic Disease?. In: Struhal, W., Lahrmann, H., Fanciulli, A., Wenning, G. (eds) Bedside Approach to Autonomic Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-05143-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-05143-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-05142-0
Online ISBN: 978-3-319-05143-7
eBook Packages: MedicineMedicine (R0)