Abstract
Signs of autonomic dysfunction, although at times seemingly mysterious, can contribute to diagnostic clarification and clinical investigation. Even when sophisticated autonomic testing equipment is not readily available, the experienced clinician, through educated observation and inductive reasoning—in conjunction with an intelligently obtained autonomic medical history—can discern much by a careful physical examination. Elements of the autonomic examination include variations in the pulse, postural measurements of blood pressure and heart rate, pupillary light reactions, skin coloration and temperature, patterns of sweating, and other organ-specific physical findings relevant to the individual patient’s presentation. Especially important is the often neglected practice of measuring the blood pressure standing up, for orthostatic hypotension cannot be diagnosed by symptoms alone and is a common source of potential morbidity. The examination should be carried out in the context of understanding the syndromic nature of abnormalities of components of the autonomic nervous system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the clinical evaluation of a patient with a known or suspected autonomic disorder, the history, based on the patient’s symptoms, is of paramount importance [1]. Signs of autonomic dysfunction, although at times seemingly mysterious, can contribute to diagnostic clarification and clinical investigation. Even when sophisticated autonomic testing equipment is not readily available, the experienced clinician, through educated observation and deductive and inductive reasoning, can discern much by a careful physical examination. As discussed below, the examination should be carried out in conjunction with an intelligently obtained autonomic medical history and in the context of understanding the syndromic nature of abnormalities of components of the autonomic nervous system (ANS).
Autonomic signs at the bedside invite clinical detective work but may escape notice unless the clinician adopts the inductive approach of the fictional detective Sherlock Holmes, who commented that “There is nothing more deceptive than an obvious fact” that has not been obvious to the unobservant [2]. We will give several examples of this sort of detective work.
Bedside autonomic assessment is not a superfluous activity, as autonomic disorders are neither rare nor inconsequential. The prevalence of orthostatic hypotension (OH), for example, in community-dwelling elderly persons is approximately 16% and increases with advancing age [3, 4]. Neurogenic OH occurs when there is inadequate release of norepinephrine from sympathetic vasomotor neurons and is a cardinal sign of sympathetic neurocirculatory failure. Neurogenic OH is seen frequently in patients with autonomic neuropathies [5] and ganglionopathies [6], as well as in neurodegenerative disorders involving abnormal accumulation of aggregates of alpha-synuclein, such as in Parkinson’s disease (PD) [7], pure autonomic failure (PAF) [8], and dementia with Lewy bodies [9]. In neuropathies and synucleinopathies, OH is associated with decreased survival [10,11,12,13]. Effective treatment strategies for OH are available, but implementation is dependent on recognition. For correct diagnosis, there is no adequate substitute for the physical examination.
Syndromic nature of autonomic disorders
When examining the patient with a known or suspected autonomic disorder, it is helpful to remember that the ANS is organized into anatomic and functional divisions. Dysautonomias often present as recognizable syndromic patterns of clinical involvement grouped according to the affected components of the ANS (Table 1). Components include the enteric nervous system (ENS), parasympathetic nervous system (PNS), and three subsystems of the sympathetic nervous system: the sympathetic noradrenergic system (SNS), sympathetic cholinergic system (SCS), and sympathetic adrenergic system (SAS) [1]. Each subsystem has a corresponding main chemical messenger: norepinephrine in the SNS, acetylcholine in the SCS, and epinephrine in the SAS.
In the ENS, for instance, Hirschsprung’s disease, which is caused by lack of development of enteric neurons, manifests entirely with signs of failure of propulsion of gastrointestinal contents. By contrast, increased SCS activity occurs in organophosphate poisoning, in which an excess of acetylcholine causes increased salivation, lacrimation, gastrointestinal motility, emesis, miosis, and urinary frequency.
SNS hyperactivity manifests with pallor, sweating, piloerection, vasoconstriction, mydriasis, trembling, and a tendency towards hypertension. Conversely, SNS hypoactivity manifests with OH, post-prandial hypotension, fatigue, ptosis, miosis, “coat hanger” nuchal pain phenomenon, and a tendency toward bradycardia.
PNS hyperactivity is suggested by miosis, a tendency toward bradycardia or heart block, increased salivation, diarrhea, and a tendency toward bronchoconstriction. Conversely, PNS hypoactivity manifests with sicca syndrome, light sensitivity, slow gastrointestinal transit, constipation, urinary retention, erectile failure, and a tendency toward tachycardia.
Other autonomic syndromes may be regional or distal, depending on localization of the lesion. Additionally, specific autonomic disorders may be accompanied by collateral signs distinct from the autonomic nervous system that nevertheless help to localize the pathology or identify the pattern of disease.
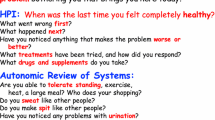
Approach to the patient with autonomic symptoms
The autonomic physical examination is best carried out in conjunction with the history. The effective clinician seeks signs that confirm or refute inductions from the history, and the physical findings may bring to mind additional questions to ask the patient. The examination carried out in isolation without this sort of give and take can be a rather meaningless exercise.
Examination of the patient begins as soon as the clinician enters the room. Important clues can be evident from the patient’s appearance and behavior during the interview. The patient who, for example, wears multiple layers of cozy clothing or a sweater when the ambient temperature is warm, or the patient who seems comfortable wearing less clothing in cold weather, may have a disorder of thermoregulation such as hypothyroidism or malnutrition (cold sensitivity), or erythromelalgia (heat sensitivity; Fig. 1). The patient who, before shaking hands, quickly wipes the palm across his or her clothing may have palmoplantar hyperhidrosis. The patient who brings a water bottle and takes sips between sentences may have xerostomia or chronic orthostatic intolerance. The odor of soiled clothing may be an indication of urinary or fecal incontinence, which are important aspects to some forms of autonomic failure. Dark sunglasses may indicate photosensitivity from tonically enlarged pupils.
As the examination proceeds, it is important to pay attention to how the patient moves. Legs that fidget, are crossed repetitively, or wrapped around one another like a pretzel can be a clue to orthostatic intolerance or OH [14, 15]. Decreased facial expression, slowness or irregularity of movement, or tremor in the patient with orthostatic intolerance may be important clues to an alpha-synucleinopathy. Are the head and neck bowed forward? This might indicate camptocormia, as in PD. What is the quality of the patient’s speech? Hypophonic or hypokinetic speech fits with PD, whereas ataxic or dysphonic speech fits with MSA. Is there rigidity at the wrist? This would be consistent with a parkinsonian synucleinopathy. Is there a grasp reflex, as one might find in dementia? Fine amplitude, high-frequency tremulousness may indicate a hyperadrenergic state. Increased sympathetic nervous system activity can be primary, as in pheochromocytoma, but more frequently is interrelated with the patient’s emotional, social, or spiritual context. A historical biblical example is Isaac’s trembling in Genesis 27:33.
Subtle behaviors during ordinary standing deserve close attention. Upon standing, the facial expression may convey a sense of apprehension. The patient with profound neurogenic OH may progressively flex the neck and trunk forward, a learned habit that lowers the head and reduces the vertical distance between the heart and the cerebral arterial circulation in order to sustain perfusion. Even when the systolic BP falls below 70 mmHg, the patient does not always complain of dizziness, perhaps because decreased cerebral perfusion impairs the perception of OH symptoms, but he or she will usually report an overwhelming need to sit down. The patient with milder orthostatic intolerance may shift weight from one leg to the other and back, which activates muscles that compress capacitance vessels and assists the return of venous blood to the heart.
Bodily physical characteristics should not go unnoticed. In a pediatric patient, the finding of a peculiar orange–gray hair color and twisted hair shafts suggests Menkes disease (Fig. 2). This is a rare X-linked recessive disease of copper metabolism. Since dopamine-beta-hydroxylase, the enzyme converting dopamine to norepinephrine in sympathetic nerves, is a copper enzyme, all patients with Menkes disease have a characteristic abnormal pattern of plasma catechols [16]. Further, the hands are potentially very informative. Are the hands and feet cool or cyanotic? In a patient with slow movement and orthostatic intolerance, this could be one of the signs of multiple system atrophy (MSA) [17]. Is there clubbing? This would suggest a paraneoplastic form of autonomic neuropathy. Is there skin tenting, as would occur in OH from dehydration? Are the fingers hyperextensible, as in Ehlers–Danlos syndrome, which can be associated with orthostatic intolerance (OI)? If so, then formal Beighton scoring would be appropriate.
The skin displays many potential autonomic signs. Is the skin moist, and, if this is uncertain, are there sweat droplets seen by otoscope examination of the skin of the face or trunk? In a patient complaining of decreased sweating, this would refute anhidrosis. Is there dry skin combined with angiokeratomas, which point to Fabry disease (Fig. 3)? Is there flushing? What is its symmetry and distribution? Is it present at rest or during standing? Pooling of blood on standing may cause the feet to appear flushed in a red, blue, or purple tone.
Detailed examination of the head, eyes, ears, nose, and throat is warranted. Is there unilateral ptosis, as in Horner’s syndrome? Is there nystagmus or dysphonia, as one might expect in the cerebellar form of MSA? Are the eyes and mouth dry (sicca syndrome, as in Sjögren’s syndrome)? Is the patient able to smell a standard odor, such as ground coffee? If not, then formal olfactory testing may be in order, since anosmia is a key finding in PD+OH. Is there a normal gag reflex? If not, one might suspect inadequate protection of the airway, as in MSA. The breath may have a particular odor, such as fetor hepaticus in a patient with liver failure or the uriniferous odor of renal failure. The neck should be examined with the patient supine (head on pillow). Is there jugular venous distention, a sign of right heart failure or pericardial restriction? Is there a carotid bruit, a sign of carotid occlusive disease, which in tandem with OH can further restrict cerebral perfusion? Is there thyroid enlargement or a thyroidal bruit, which would indicate Graves disease?
In examining the chest and abdomen, one should inspect first, looking for pectus excavatum or pectus carinatum, important findings in collagen vascular diseases. Is there auscultatory evidence for mitral valve prolapse or hypertrophic subaortic stenosis? Hepatosplenomegaly leads to suspicion of a host of conditions, including mononucleosis or other chronic infection, Gaucher disease, amyloidosis, myelofibrosis, and chronic alcoholism. Palpation and auscultation of the abdomen might point to aortic aneurysm, renal artery stenosis, or median arcuate ligament syndrome (Fig. 4).
The pulse provides many clues. Is the pulse bounding, as in hyperthyroidism, or barely palpable, as in presyncope? Is the pulse irregularly irregular, a finding indicating atrial fibrillation? Are there frequent extrasystoles, a common occurrence in chronic autonomic failure [18]? Is there respiratory sinus arrhythmia? If so, one can probably exclude arterial baroreflex failure [19]. Are the left and right radial pulses equal? Delay or reduction of the left radial pulse may indicate subclavian artery stenosis, an important cause of syncope during left arm exertion. Upon palpation of the radial pulse with two fingers, proximal and distal, does the pulse at the more distal finger disappear only with substantial pressure on the pulse by the more proximal finger? If so, then the patient may have systolic hypertension related to arterial stiffening.
The structured autonomic examination
Whereas standard physical examinations are specific to each medical specialty or subspecialty, the autonomic examination spans multiple organ systems, and its assessment requires a broad conceptual approach. A set of common elements to the autonomic examination may be defined (Table 2). At a minimum, the autonomic examination should assess orthostatic vital signs, the pulse (fullness, vascular stiffness, rhythm, respiratory sinus arrhythmia); skin color, temperature, and moisture; bowel sounds; and pupillary responses.
Pupilomotor
Pupillary size and reactivity are telling signs of ocular sympathetic (mydriasis) and parasympathetic (miosis) activity. In The Man with the Twisted Lip, Sherlock Holmes’s companion, Dr. Watson, recognizes the inhibitory effect on the sympathetic innervation of the irises in a man addicted to opium: “I can see him now, with yellow, pasty face, drooping lids, and pin-point pupils, all huddled in a chair” [20].
Pharmacologic inhibition of parasympathetic innervation, by contrast, enlarges the pupils. The classic herb that dilates the pupils is Atropa belladonna, which derives from the Italian phrase for “beautiful woman”, as eyedrops containing small amounts were used in antiquity to create a seductive appearance [21]. Also known as deadly nightshade, this plant is a potent anticholinergic toxin that contains atropine, scopolamine, and hyoscyamine, ingestion of which causes pupillary dilatation, tachycardia, anhidrosis, flushing, dry mouth, urinary retention, constipation, delirium, and hallucinations. This constellation of signs highlights the syndromic nature of a dysautonomia that may at first be evident in the size of the pupils.
The pupillary light reflex should be examined in a darkened room, to allow the pupils to optimally enlarge, with illumination directed from below in order to visualize their relative size and responsiveness. When assessing pupillary size, the patient should be asked to gaze into the distance to eliminate the pupillary constricting effect of ocular convergence.
One-fifth of the normal population has unequal pupils (anisocoria) with a diameter difference of 0.3 mm or more [22]. Anisocoria can also be a sign of unilateral oculosympathetic (cervical sympathetic chain) or oculoparasympathetic (ciliary ganglion) denervation. An oculosympathetic deficit causes the pupil to appear smaller and is typically accompanied by ipsilateral ptosis of the upper eyelid (Horner’s syndrome; Fig. 5). Congenital Horner’s syndrome is associated with heterochromia, in which the denervated iris differs in color from its counterpart. An oculoparasympathetic deficit causes the pupil to appear larger, and, in the case of Adie’s tonic pupil, segmental differences in contraction may be seen, giving the pupil an irregular shape. The difference in pupillary size will usually be more apparent for an oculosympathetic deficit in dim light and for an oculoparasympathetic deficit in bright light.
Not to be confused with anisocoria is hippus, a normal phenomenon in which the pupillary size is unstable and is more easily visualized in younger patients whose pupils normally are larger than those of older patients.
Vasomotor
“I do not think that I have ever seen such deadly paleness in a woman’s face”, remarked Dr. Watson in The Adventure of the Beryl Coronet. “Her lips, too, were bloodless, but her eyes were flushed with crying” [23]. To Watson and Holmes, facial pallor and flushing were significant clues to someone’s emotional state or character. Facial flushing can be a sign of autonomic arousal, anticholinergic or antiestrogen medication, narcotic antagonist medication, niacin, carcinoid tumor, mastocytosis or other forms of histamine release, rosacea, polycythemia vera, allergy, or sunburn, among many other potential causes. Heat-induced flushing may occur in patients with global anhidrosis who lack the capacity to produce a thermoregulatory sweating response [24].
Unilateral facial flushing is a feature of harlequin syndrome, which is frequently accompanied by a contralateral oculosympathetic deficit with ptosis, miosis, and absence of flushing [25]. Facial flushing or sweating, lacrimation, nasal stuffiness, or ptosis ipsilateral to a paroxysmal headache can signify a trigeminal autonomic cephalalgia [26]. Presyncopal bilateral facial pallor, by contrast, is a hallmark sign of neurally mediated syncope [27].
Purplish discoloration of the toes or feet, which is often more pronounced in the upright posture, is frequently seen in patients with distal vasomotor instability, which can result from arteriolar vasoconstriction or venous pooling. The feet may be warm or cool to the touch.
Sherlock Holmes’s guest who warmed his wet feet by the fire in The Five Orange Pips likely would have had wrinkled toes, a detail inconsequential in the context of the story as compared to the distinctive traces of clay on his toecaps [28]. Wrinkling of the fingers and toes within several minutes of immersion in water is a normal autonomic phenomenon caused by peripheral adrenergic vasoconstriction in the digital pulp [29].
Secretomotor
The patient who frequently rubs or blinks the eyes may suffer from xerophthalmia (dry eyes). This can result from inadequate lacrimation causing a decreased volume of tear film production, for example, in Sjögren syndrome. Other patients may have decreased eye-blinking from prolonged gazing at a computer screen or from facial bradykinesia in Parkinson’s disease, as each blink of the eyes compresses the lacrimal gland and disperses new tears to replace moisture lost to evaporation. The conjunctivae may appear slightly red, and contact lenses may not remain in place.
The patient with a dry tongue and cracked lips may have xerophthalmia (dry mouth). This can result from Sjögren syndrome or more commonly from anticholinergic medication.
Had Conan Doyle written for a medical readership, he might have challenged Sherlock Holmes to solve cases punctuated with medical clues such as aberrant reinnervation. Gustatory facial sweating (auriculotemporal syndrome) following injury to the facial nerve develops when severed parasympathetic fibers that originally supplied the salivary glands regrow in the wrong direction and innervate facial sweat glands. When eating, droplets of sweat appear on the cheek. Other salivary fibers may reinnervate the lacrimal gland and cause unilateral tears when eating (crocodile tears).
Sudomotor
In The Adventure of the Blue Carbuncle, Sherlock Holmes examined a hat “as an intellectual problem”, and concluded that the marks of moisture on the inside were “proof positive that the wearer perspired very freely” [30]. By contrast, dry leather shoe insoles or dry socks can suggest a small fiber neuropathy significant enough to abolish distal postganglionic sudomotor neuronal function.
Chronic anhidrosis may present with dry, parched or cracked skin, or there may be no remarkable physical findings. Hyperhidrosis is more easily detected than anhidrosis and is more often noticed by patients. Detection of subtle asymmetry of sweating is important because it has potential localizing value. The best way to visualize active sweating at the bedside is to dim the room lights and shine a bright light held just above the examiner’s eyes perpendicularly to the patient’s skin to elicit reflections from sweat droplets [31]. Tiny sweat droplets on the skin surface may be visualized through an otoscope.
More sensitive than visualization is palpation of the skin, which feels smoother to the touch when normal sweating is present. Asymmetry of baseline sweating, when suspected, can be assessed quickly by a gentle stroke of the fingers against the skin, at the same time taking note of any asymmetry of temperature. The same principle is the basis for the spoon test, in which sliding a moderately heavy spoon over the surface of sympathetically denervated skin encounters greater resistance [32].
Gastrointestinal
The biblical story of the trial by ordeal conducted in the case of the “sotah”, the woman accused of adultery by her husband, teaches about one of the most important—and underappreciated—signs of distress-related activation of the SAS.
The woman would be brought to the priest, who would conduct the trial according to a specific ritual. The key sign of guilt was when the accused woman was forced to drink “waters of bitterness”, consisting of water and dust from the floor of the tabernacle. The priest would incant, “If thou has gone aside, being under thy husband, and if thou be defiled… this water that causeth the curse shall go into thy bowels, and make thy belly to swell” (Numbers 5:19–21). The accused woman would have to reply, “Amen, Amen” (the first use of the term in the Bible). The woman would then drink the test potion. If she had been unfaithful, her belly would swell.
Why would abdominal distention be a sign of distress and, therefore, in biblical lie detection, of guilt? Adrenaline potently relaxes smooth muscle of the gastrointestinal tract. Indeed, this relaxation provided the basis for the first successful method, introduced by Walter B. Cannon, for detecting adrenaline release during emotional distress. Cannon drew blood from a cat exposed to a barking dog. This evoked release into the cat’s blood of a substance that relaxed a strip of gut tissue (Fig. 6). Exposure of the strip to blood from the adrenal veins produced the same relaxing effect, and tying off the adrenal veins eliminated the effect, indicating that distress released a substance from the adrenal glands into the bloodstream. The woman in distress would have a form of functional ileus (decreased propulsion of gut contents). In this setting, a non-palatable liquid would not pass through the gut, and the belly would swell.
Tracings by Walter B. Cannon showing in vitro intestinal relaxation upon exposure to blood from a cat exposed to a barking dog. This was the first demonstration of distress-induced release of a hormone (epinephrine). Following baseline (A), alternate application of excited blood (at B and D) and quiet blood (at C), from the same animal, to an intestinal strip initially beating in Ringer’s solution
It is not widely appreciated that high circulating levels of catecholamines can produce ileus. The distended loops of bowel would result in abdominal swelling. Ileus without intestinal obstruction is called pseudo-obstruction. Intestinal pseudo-obstruction can be a manifestation of pheochromocytoma, a tumor that secretes catecholamines into the bloodstream [33,34,35,36].
Urinary
Palpation and percussion of the suprapubic region can detect a greatly distended bladder. If there is no evidence of urinary outlet obstruction, for example, an enlarged prostate gland in men or prolapse of the bladder or rectum in women [37], then neurogenic atony of bladder wall contraction should be suspected and sacral sensation should be carefully examined. Loss of sensation to pinprick in sacral dermatomes S2–S5, reduced anal sphincter tone, or loss of the anal wink reflex should alert suspicion for a lesion of the cauda equina or conus medullaris.
More common than an atonic bladder that retains urine is an overactive or hypercontractile bladder, which, if neurogenic, may be accompanied by lower extremity hyperreflexia, a spastic gait, and extensor toe responses to plantar stimulation (Babinski sign).
Urinary retention requiring intermittent catheterization or indwelling bladder cannulation is an important sign of MSA. Urinary retention is much more typical of MSA than PD+OH. The reason is degeneration in a region called Onuf’s nucleus, which is in the anterior horn of the sacral spinal cord. Onuf’s nucleus receives descending input from the “continence center” in the pons of the brainstem, and it projects to the urethral sphincter by way of the pudendal nerve (Fig. 7). Stretch receptors in the bladder wall send afferent information to the spinal cord, and the signal is transmitted both to the brainstem and to Onuf’s nucleus, completing long-distance and local negative feedback loops.
Heart rate
“One of the most interesting, but also, if I do not mistake, one of the least noticed facts of the symptomatology of cervical spinal lesions”, wrote Jean-Martin Charcot in 1881, is “the permanent retardation of the pulse” [38]. His description proceeds to describe paroxysmal bradycardia, flushing, headache, and syncope: “The state of syncope always opens the scene; the apoplectic state with stertorous sleep then supervenes, at the moment when the pulse, which had been for an instant suppressed, reappears, and when the pallor of the features gives place to redness of the countenance” [38]. Charcot was correct to suspect that these phenomena did not arise in the heart, but rather in the spinal cord or medulla oblongata, even though knowledge of autonomic neuroanatomy at that time was insufficiently detailed to explain this disrupted connection between the brain and the heart. A century later, it is understood that interruption of cardiac sympathetic innervation at T1–T4 when cardiac vagal innervation is intact can lead to unopposed cardiac parasympathetic activity causing bradycardia as well as orthostatic hypotension [39, 40].
The integrity of parasympathetic innervation of the heart can be estimated at the bedside by two simple methods. First, by palpating the pulse while the patient is asked to take a single deep breath or a series of slow deep breaths, variations in cardiac frequency may be discerned. This respiratory sinus arrhythmia is a normal response that consists of acceleration of heart rate during inspiration and slowing of heart rate during expiration. Under resting conditions, the heart varies; in patients with baroreflex–cardiovagal failure, such as in MSA, the heart rate is more metronomic, and there is very little variability (Fig. 8). Second, the normal release of parasympathetic tone upon standing may cause an immediate, transient increase in heart rate during the first 15–30 s [41].
Because these responses attenuate with increasing age, their absence in older patients is less informative. When present, they represent a qualitative, though imprecise, indication that cardiovagal function is present.
Blood pressure
Last, but by no means least, bedside examination of the autonomic nervous system should assess the hemodynamic response to orthostatic stress. No reasonable clinician would diagnose hypertension on the basis of symptoms without measuring blood pressure. Similarly, the diagnosis of OH or OI requires measurement of blood pressure (BP) and heart rate during postural change.
For routine screening in a busy clinical practice, we recommend measuring BP and heart rate while the patient is supine, having rested in the supine position for at least 2 min, then while standing at 1 min. Measuring the standing BP before a full minute has passed is of little value except in cases where there is a history of syncope or falling immediately upon standing. A substantial fall in BP at 1 min of standing will capture most cases of neurogenic OH [42]. If the fall in BP is borderline, or if it is within normal limits when the clinician suspects OH, then repeating the standing BP measurement at 2–5 min may be appropriate.
OH is defined, not by symptoms—which can be nonspecific or even absent—but by a sustained reduction in systolic BP of at least 20 mmHg or diastolic BP of 10 mmHg within 3 min of standing [3, 43]. The absence of compensatory tachycardia (when pharmacologic beta blockade is not present) is suggestive of neurogenic OH. In some cases, postural tachycardia is preserved in neurogenic OH. Excessive postural tachycardia in the absence of OH is a defining feature of postural tachycardia syndrome [43].
Various automated devices, some of which are designed for inexperienced users, are increasingly replacing the traditional auscultatory technique using a stethoscope and mercurial or aneroid sphygmomanometer for clinical assessment of BP [44]. In general, wrist devices are less accurate than upper arm devices [45], and all indirect methods are less accurate than intra-arterial recordings [46]. These devices are usually sufficient, however, for assessing changes in BP [46], which is of greater importance than static BP measurements when evaluating autonomic disorders.
Automated oscillometric devices are user-friendly and purported to eliminate observer bias but have the unintended consequence of making it seem unnecessary to think about the physiology of BP when assessing the patient. All that is necessary to document BP in the medical record is to place a cuff on the patient’s arm, press a button, wait 30–40 s, and write down the numbers. When evaluating the patient with orthostatic syncope whose BP drops precipitously within the first 20–30 s of standing and then recovers, an automated device may not function quickly enough to detect the relevant abnormality, whereas the clinician who knows the patient’s baseline BP, can, with a stethoscope and experience, detect the drop in time.
Accuracy of BP measurement depends on arm position. The detection device should be kept at the level of the heart (the right atrium), especially when the patient changes posture, to avoid the confounding effect of the hydrostatic pressure of the arm blood column. If the device shifts to a lower level when the patient stands up, a falsely higher BP result will occur. The difference can be as much as 2 mmHg for every inch (2.5 cm) above or below the heart [44]. Equally important is that the patient be comfortable, relaxed, and not speaking or tensing limb muscles. The mercury column or equivalent should be deflated at a rate of 2–3 mm/s (more slowly if bradycardia is present, more quickly if the patient at that moment is presyncopal), and the BP recorded to the nearest 2 mmHg [44].
The absence of OH at a given point in time does not exclude the presence of noradrenergic failure with the potential for intermittent neurogenic OH. The hemodynamic response to orthostatic stress will vary by the time of day, the length of the preceding supine rest period, hydration status, pharmacologic effects of medications, ambient temperature, meals, and many other factors [47]. In a study of 40 outpatients with documented symptomatic OH, the abnormal drop in BP was reproducible at subsequent times during the same day in only about 70% of patients [48]. For these reasons, morning assessments may be more sensitive, and, when the results are uncertain, repeated measurements on separate days may be necessary.
Detection of OH in the patient who is unable to stand up represents a special diagnostic challenge. In most cases, the transition from supine to seated will cause some degree of a drop in BP, especially if the legs are passively lowered.
Conclusion
“It is a mistake to confound strangeness with mystery”, said Sherlock Holmes in A Study in Scarlet. Continuing, he points out that “These strange details, far from making the case more difficult, have really had the effect of making it less so” [49]. Autonomic signs likewise may at first seem mysterious to the patient or to the inexpert clinician, but with understanding of the underlying concepts and attention to detail, a careful study of physical signs can begin to elucidate the most perplexing of autonomic disorders.
Abbreviations
- ANS:
-
Autonomic nervous system
- BP:
-
Blood pressure
- ENS:
-
Enteric nervous system
- MSA:
-
Multiple system atrophy
- OH:
-
Orthostatic hypotension
- OI:
-
Orthostatic intolerance
- PAF:
-
Pure autonomic failure
- PD:
-
Parkinson’s disease
- PNS:
-
Parasympathetic nervous system
- POTS:
-
Postural tachycardia syndrome
- SAS:
-
Sympathetic adrenergic system
- SCS:
-
Sympathetic cholinergic system
- SNS:
-
Sympathetic noradrenergic system
References
Goldstein DS, Cheshire WP (2017) The autonomic medical history. Clin Auton Res 27:223–233
Doyle AC (1891) The Boscombe Valley mystery. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 88
Wu JS, Yang YC, Lu FH, Wu CH, Chang CJ (2008) Population-based study on the prevalence and correlates of orthostatic hypotension/hypertension and orthostatic dizziness. Hypertens Res 31:897–904
Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS (1992) Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 19:508–519
Freeman R (2014) Diabetic autonomic neuropathy. Handb Clin Neurol 126:63–79
Goldstein DS, Holmes C, Dendi R, Li ST, Brentzel S, Vernino S (2002) Pandysautonomia associated with impaired ganglionic neurotransmission and circulating antibody to the neuronal nicotinic receptor. Clin Auton Res 12:281–285
Orimo S, Uchihara T, Nakamura A, Mori F, Kakita A, Wakabayashi K, Takahashi H (2008) Axonal alpha-synuclein aggregates herald centripetal degeneration of cardiac sympathetic nerve in Parkinson’s disease. Brain 131:642–650
Kaufmann H, Hague K, Perl D (2001) Accumulation of alpha-synuclein in autonomic nerves in pure autonomic failure. Neurology 56:980–981
Baba M, Nakajo S, Tu PH, Tomita T, Nakaya K, Lee VM, Trojanowski JQ, Iwatsubo T (1998) Aggregation of alpha-synuclein in Lewy bodies of sporadic Parkinson’s disease and dementia with Lewy bodies. Am J Pathol 152:879–884
Gaspar L, Kruzliak P, Komornikova A, Celecova Z, Krahulec B, Balaz D, Sabaka P, Caprnda M, Kucera M, Rodrigo L, Uehara Y, Dukat A (2016) Orthostatic hypotension in diabetic patients-10-year follow-up study. J Diabetes Complicat 30:67–71
Goldstein DS, Holmes C, Sharabi Y, Wu T (2015) Survival in synucleinopathies: a prospective cohort study. Neurology 85:1554–1561
Kyle RA, Greipp PR, O’Fallon WM (1986) Primary systemic amyloidosis: multivariate analysis for prognostic factors in 168 cases. Blood 68:220–224
Spallone V, Ziegler D, Freeman R, Bernardi L, Frontoni S, Pop-Busui R, Stevens M, Kempler P, Hilsted J, Tesfaye S, Low P, Valensi P, Toronto Consensus Panel on Diabetic N (2011) Cardiovascular autonomic neuropathy in diabetes: clinical impact, assessment, diagnosis, and management. Diabetes Metab Res Rev 27:639–653
Cheshire WP (2000) Hypotensive akathisia: autonomic failure associated with leg fidgeting while sitting. Neurology 55:1923–1926
Adiyaman A, Tosun N, Elving LD, Deinum J, Lenders JWM, Thien T (2007) The effect of crossing legs on blood pressure. Blood Press Monit 12:189–193
Goldstein DS, Holmes CS, Kaler SG (2009) Relative efficiencies of plasma catechol levels and ratios for neonatal diagnosis of Menkes disease. Neurochem Res 34:1464–1468
Augustis S, Saferis V, Jost WH (2017) Autonomic disturbances including impaired hand thermoregulation in multiple system atrophy and Parkinson’s disease. J Neural Transm (Vienna) 124:965–972
Goldstein DS (2010) Cardiac ectopy in chronic autonomic failure. Clin Auton Res 20:85–92
Moak JP, Goldstein DS, Eldadah BA, Saleem A, Holmes C, Pechnik S, Sharabi Y (2007) Supine low-frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Heart Rhythm 4:1523–1529
Doyle AC (1891) The man with the twisted lip. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 99
Tombs S, Silverman I (2004) Pupillometry: a sexual selection approach. Evol Hum Behav 25:221–228
Corbet JJ (2003) The bedside and office neuro-ophthalmology examination. Semin Neurol 23:63–76
Doyle AC (1892) The adventure of the beryl coronet. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 132
Cheshire WP (2016) Thermoregulatory disorders and illness related to heat and cold stress. Auton Neurosci 196:91–104
Cheshire WP, Low PA (2006) Harlequin syndrome: still only half understood. J Neuroophthalmol 28:169–170
Newman LC (2015) Trigeminal autonomic cephalalgias. Continuum 21:1041–1057
Cheshire WP (2017) Syncope. Continuum 23:335–358
Doyle AC (1891) The five orange pips. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 94
Wilder-Smith EP, Chow A (2003) Water-immersion wrinkling is due to vasoconstriction. Muscle Nerve 27:307–311
Doyle AC (1892) The adventure of the blue carbuncle. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 106
Cheshire WP (2008) Clinical evaluation of the patient with an autonomic disorder. In: Low PA, Benarroch EE (eds) Clinical autonomic disorders, 3rd edn. Wolters Kluwer, Lippincott Williams & Wilkins, Philadelphia, pp 112–129
Tsementzis SA, Hitchcock ER (1985) The spoon test: a simple bedside test for assessing sudomotor function. J Neurol Neurosurg Psychiatry 48:378–380
Kek PC, Ho ET, Loh LM (2015) Phaeochromocytoma presenting with pseudo-intestinal obstruction and lactic acidosis. Singap Med J 56:e131–e133
Salazar A, Naik A, Rolston DD (2001) Intestinal pseudoobstruction as a presenting feature of a pheochromocytoma. J Clin Gastroenterol 33:253–254
Sawaki D, Otani Y, Sekita G, Kobayakawa N, Fukushima K, Takeuchi H, Aoyagi T (2003) Pheochromocytoma complicated with refractory paralytic ileus dramatically improved with intravenous administration of alpha-adrenergic receptor antagonist, phentolamine. J Clin Gastroenterol 37:194
Wu HW, Liou WP, Chou CC, Chen YH, Loh CH, Wang HP (2008) Pheochromocytoma presented as intestinal pseudo-obstruction and hyperamylasemia. Am J Emerg Med 26(971):e971–e974
Selius BA, Subedi R (2008) Urinary retention in adults: diagnosis and initial management. Am Fam Physician 77:643–650
Charcot JM (1881) Lectures on the diseases of the nervous system delivered at La Salpêtrière trans. trans. By George Sigerson. The New Sydenham Society, J. El Adlard, London. Reprinted by The landmark library of neurology and neurosurgery. New York: 1994, vol II, pp 117–120
Mathias CJ (2006) Orthostatic hypotension and paroxysmal hypertension in humans with high spinal cord injury. Prog Brain Res 152:231–243
Clayton VE, Krassioukov AV (2006) Orthostatic hypotension and autonomic pathways after spinal cord injury. J Neurotrauma 23:1713–1725
De Leeuw PW (1988) Testing parasympathetic function at the bedside. Neth J Med 33:257–259
Soysal P, Aydin AE, Okudur SK, Isik AT (2016) When should orthostatic blood pressure changes be evaluated in elderly: 1st, 3rd or 5th minute? Arch Gerontol Geriatr 65:199–203
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz I, Schondorf R, Stewart JM, van Dijk JG (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21:69–72
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ (2005) Recommendations for blood pressure measurement in humans and experimental animals. Part 1: blood pressure measurement in humans. A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 45:142–161
Casiglia E, Tikhonoff V, Albertini F, Palatini P (2016) Poor reliability of wrist blood pressure self-measurement at home: a population-based study. Hypertension 68:896–903
Hunyor SN, Flynn JM, Cochineas C (1978) Comparison of performance of various sphygmomanometers with intra-arterial blood pressure readings. Br Med J 2:159–162
Smith JJ, Porth CM, Erickson M (1994) Hemodynamic responses to the upright posture. J Clin Pharmacol 34:375–386
Ward C, Kenny RA (1996) Reproducibility of orthostatic hypotension in symptomatic elderly. Am J Med 100:418–422
Doyle AC (1887) A study in scarlet. In: The complete Sherlock Holmes (2002). Gramercy, New York, p 24
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The research reported here was supported by the Division of Intramural Research, NINDS, NIH.
Rights and permissions
About this article
Cite this article
Cheshire, W.P., Goldstein, D.S. The physical examination as a window into autonomic disorders. Clin Auton Res 28, 23–33 (2018). https://doi.org/10.1007/s10286-017-0494-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-017-0494-7