Abstract
Evaluation and management of syndesmosis fixation is challenging and controversial without a ‘one-approach fixes all.’ A relatively straightforward case of a failed ankle fixation, which underwent revision surgery, is presented herein. Several pertinent points are illustrated, and updated information on the diagnosis and treatment of these frequently intriguing injuries is presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
History of Previous Primary Treatment
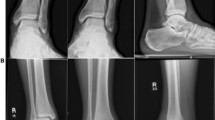
This is the case of a 20-year-old otherwise healthy man who had fallen inside a pothole and sustained an isolated, neurovascularly intact closed left ankle injury (Fig. 39.1a, b). He was transferred to an outside regional hospital for initial management.
The fracture was immediately reduced in the emergency room, and on the same day, the patient underwent open reduction and internal fixation of his fracture. The fibula was fixed using a lateral fibular locking plate (Newclip Technics) and the syndesmosis was stabilized using a partially threaded syndesmotic screw. The medial malleolus was also reduced and fixed with two fully threaded screws (Fig. 39.2a, b).
In view of the post-operative radiographs, 5 days following the fixation, the patient was referred to the authors’ tertiary centre for further management.
Evaluation of the Aetiology of Failure of Fixation
At this stage, the first step is to use several plain radiographic parameters to evaluate the status of the syndesmosis (Fig. 39.3a, b): tibiofibular clear space, tibiofibular overlap and medial clear space, length of the fibula (‘dime’ or ‘ball’ sign and talocrural angle) [1, 2]. The mortise view (Fig. 39.2a) shows that all of these parameters are disrupted, and on both the mortise and lateral views (Fig. 39.2b), there appears to be a non-congruent joint line. The aetiology of failure therefore is secondary to poor technique, i.e. poor reduction of the syndesmosis.
(a, b) Plain radiographic parameters for evaluation of the syndesmosis on the anteroposterior (AP) radiograph (a) and mortise view (b). Measurements should be: tibiofibular clear space (TFCS): <6 mm on either view, tibiofibular overlap (TFO): <6 mm (AP view) or <1 mm (mortise view), talocrural angle (TCA): 72°–86° (AP view), medial clear space (MCS): equal to the superior clear space and < 4 mm (mortise view). ‘Dime’ sign: ball (or circle should not be disrupted). (Obtained with permission from George D. Chloros, MD)
Clinical Examination
On examination, 5 days post-operatively, there was moderate swelling and no wound dehiscence, drainage or any signs of early infection (Fig. 39.4). The patient was otherwise completely neurovascularly intact.
Diagnostic-Biochemical and Radiological Investigations
In view of the radiographic evaluation, which prompted a high index of suspicion for syndesmosis malreduction, further imaging was ordered consisting of a computed tomography (CT) scan for pre-operative planning purposes (Fig. 39.5a-d).
(a–d) CT scan showing the status of the ankle joint and syndesmosis: (a) Transverse section showing that the fibula lies completely outside of the incisura. (b) Coronal section demonstrating significant joint incongruity. (c) Sagittal section showing anterior subluxation of the ankle joint. (d) Three-dimensional (3D) CT reconstruction showing in addition to malreduction of the medial malleolus
Based on the imaging, the list of problems is as follows (Fig. 39.6):
-
1.
Fibula malreduction – rotational defect.
-
2.
Syndesmotic anterior dislocation.
-
3.
Tibiotalar anterior subluxation (significant: more than 50% of the talar articular surface not articulating with the tibial plafond).
-
4.
Medial malleolus—malreduction.
-
5.
Posterior malfracture.
Preoperative Planning
At this point, the goal is to restore the ankle joint anatomic congruity by addressing the aforementioned problems: removal of the hardware, revision fixation of the fibula and the medial malleolus to correct the malreduction and appropriately establish the alignment of the joint surfaces and lastly, fixation of the syndesmosis; the appropriate length, alignment and rotation of the fibula must be addressed and second the syndesmosis needs to be fixed [3,4,5]. It is well established that malreducing the syndesmosis, either by failing to restore the aforementioned fibular parameters or by failure to fix the fibula in the appropriate position within the incisura, leads to poor outcomes [6].
Therefore, a revision fixation is contemplated consisting of:
-
1.
Removal of the previous screws from the medial malleolus.
Equipment needed: small fragment set screwdriver
-
2.
Revision reduction and fixation of the medial malleolus using partially threaded cancellous screws.
Equipment needed: Tulloch-Brown clamp (special pointed reduction forceps); two partially threaded 4.0-mm cancellous screws
-
3.
Removal of the fibula plate.
Equipment needed: small fragment set screwdriver (Newclip Technics)
-
4.
Opening of the syndesmosis and evaluation under direct vision.
Equipment needed: dental pick, nibblers, lamina spreaders
-
5.
Visualization, reduction and revision fixation of the fibula to make sure that anatomic alignment including length, alignment and rotation is restored.
Equipment needed: 1.6 K-wires, one-third small fragment semi-tubular plate DepuySynthes
-
6.
Syndesmosis reduction fixation.
Equipment needed: fully threaded cortical 3.5-mm-long screw.
Revision Surgery
The patient was positioned supine in the operating table. Antibiotics were administered. The patient was prepped and draped in the usual sterile fashion and a thigh tourniquet was inflated to 350 mmHg. A medial incision was carried out, which was centred on the previous incision. The medial malleolus was exposed and the 4.0 screws were removed using the appropriate screwdriver. The fracture site was cleaned using a combination of dental picks and nibblers and subsequently reduced and held with a Tulloch-Brown clamp. Reduction was confirmed using biplanar fluoroscopy and was satisfactory. Two 1.6-K-wires were drilled in a parallel fashion and 4.0-mm partially threaded cannulated screws of appropriate length were inserted through the wires, which were then removed. The medial wound was closed using 3–0 subcutaneous sutures followed by 3–0 nylon skin sutures.
Attention was then drawn to the lateral side. The previous lateral incision was used and the hardware was exposed and removed using appropriate screwdrivers. The fracture site was taken down, mobilized and cleaned from the debris using a combination of instruments similar to the medial side. At this point, the lower syndesmosis was completely visualized and thoroughly debrided. The fibula was clearly posteriorly malreduced relative to the incisura, which was empty. The length, alignment and rotation of the fibula were re-established using standard reduction manoeuvre by reversing the mechanism of injury. Two crocodile reduction clamps were used to stabilize the fibula in place. A 12-hole third tubular plate was contoured to match the fibula, including distal contouring to ‘hook’ the lateral malleolus. Eight 3.5-mm cortical screws were subsequently inserted. Attention was turned on the syndesmosis, which was reduced under direct vision and temporarily pinned with a 1.6-mm K-wire. Fluoroscopy verified correct length, alignment and rotation of the fibula and reduction of the syndesmosis. Of note, there are mainly two methods of direct visualization and reduction of the syndesmosis, including the evaluation of the anterior incisura versus visualization of the anterior articular surface at the joint [7]. As the former method has proved less reliable (80%), the syndesmosis was reduced according the later method described by Tornetta et al., which is 93% accurate and is based on perfectly aligning the anterolateral tibial plafond cartilage and the anteromedial fibular cartilage [7]. The authors of this chapter recommend reducing the syndesmosis under direct vision as described and confirming the reduction fluoroscopically with contralateral side comparison. If the reduction is anatomic, then the projections should also be symmetrical. If this is not the case, then, re-attempt at reduction should be performed until everything ‘adds-up’. Post-operatively, the patient was put in a splint, no weightbearing for 6 weeks and given deep venous thrombosis (DVT) prophylaxis. He received initial follow-up at the clinic in 2 weeks and further imaging was obtained (Fig. 39.7a, b). At this point, the splint was replaced with a cam walker boot and the patient was encouraged to actively move his ankle using Therabands. At 8 weeks, full weightbearing was permitted and the patient started formal physical therapy. The syndesmotic screw was subsequently removed at 3 months. At 6 months, radiographs show maintenance of the post-operative result (Fig. 39.8a, b). The patient had an excellent range of motion, with a pain-free, stable ankle (Fig. 39.9a, b).
Discussion
There is considerable controversy in the diagnosis and detection of syndesmosis injuries, with the literature being constantly updated with new imaging for technological advances. Sufficient and updated knowledge of the currently available imaging modalities including their strengths and limitations and their appropriate application is essential and crucial in the clinical decision-making of the individual patient.
In this particular case presented, the initial syndesmosis malreduction was easily diagnosed in a straightforward manner using the usual imaging parameters, as described previously (Figs. 39.3a, b and 39.6).
However, it is important to note that nowadays, those ‘classic’ measurements are surrounded with significant controversy and uncertainty, and therefore should be taken with a grain of salt [2]. First and foremost, they are dependent on the magnification, rotation and position of the limb as far as plantar flexion and dorsiflexion and they have been challenged by recent CT studies [2]. Second, as outlined below, there is significant interindividual variation, and therefore the bottom line is that x-rays should be interpreted with caution and always within the clinical context, on a case-by-case basis [2]. Frequently, stress radiographs are important in the assessment in equivocal cases [8].
Intra-Operative Imaging
As there is considerable anatomical variability among patients [9], but little intraindividual variation [10], the simple technique of templating the contralateral (uninjured) ankle with intra-operative fluoroscopy is shown to be very effective in assessing the syndesmosis, and is briefly shown in Fig. 39.10 [9, 11,12,13]. Furthermore, intra-operative cone beam CT may also be used to accurately assess reduction [14]; however, its major current limitation is availability.
Intra-operative reduction using the contralateral extremity as template [11]. Prior to prepping and draping, a coronal plane template is obtained by a perfect mortise view. Fibular length and rotation, by virtue of the usual radiographic parameters, as described previously, including the medial clear space, the tibiofibular clear space and the tibiofibular overlap as well as the ‘ball’ or ‘dime’ sign, is evaluated. Subsequently, for reduction in the sagittal plane, a perfect lateral of the ankle with superimposition of the medial and lateral talar domes is obtained. Posterior tibiofibular distance (A-B): The distance between the posterior aspect of the posterior malleolus of the tibia and the posterior cortex of the fibula is measured on the contralateral extremity and the image is saved for future templating. The injured limb is then reduced in both planes. The posterior tibiofibular distance should match the previously templated contralateral extremity both measured at the same level, and subsequently the surgeon may proceed with their preferred method of syndesmosis fixation. Of note, the distance between the limb and image intensifier should be kept constant to minimize magnification errors and measurements should take place at the same level for both injured and uninjured limbs. (Obtained with permission from George D. Chloros, MD)
Further Advanced Imaging
Bilateral computed tomography (CT) of the ankles may be checked either pre-operatively (to diagnose syndesmosis injury) or post-operatively (to assess fixation) [10].
Pre-operative assessment is crucial in determining subtle, i.e. less than 3-mm diastases, and is superior to plain radiographs in diagnosing syndesmosis injuries [10], as about 40% of those may be overlooked based on plain radiographic evaluation even in experienced hands [15]. Figures 39.11 and 39.12 show the different parameters that can be evaluated based on the bilateral ankle CT.
(a–d): Various CT scan measurements, based on Nault et al. [1]. Note the line joining the anterior and posterior edges of the colliculi (connecting point a to point c): (a) Anterior tibiofibular distance (a, b), posterior tibiofibular distance (c, d), distance between tibia and fibula in the middle of the incisura (e, f). (b) Distance between the anterior part of the fibula (g, h) and the posterior part of the fibula (h-i), respectively, perpendicular to line a-c. (c) Distance between the anterior part of the incisura and the anterior part of the fibula (b-j). (d) Angle theta (θ), drawn between line a-c and a line representing the orientation of the fibula (i.e. along the longest axis of the fibula). (Obtained with permission from George D. Chloros, MD)
[1] Nault ML, Hébert-Davies J, Laflamme GY, Leduc S. CT scan assessment of the syndesmosis: A new reproducible method. Journal of Orthopaedic Trauma. 2013;27 [11]:638–641.
CT for evaluation of the syndesmosis, based on Lee et al. The surface area of the syndesmosis (SAS) [16] is the surface area enclosed by the anterior colliculus (a), the most anterior part of the fibula (b), the posterior colliculus (c) and the most posterior aspect of the fibula (d). The SAS on the right side is significantly larger, compared to the left indicating disruption. (Obtained with permission from George D. Chloros, MD)
[Lee SW, Lee KJ, Park CH, Kwon HJ, Kim BS. The Valid Diagnostic Parameters in Bilateral CT scan to Predict Unstable Syndesmotic Injury with Ankle Fracture. Diagnostics (Basel). 2020;10 [10].]
Of note plain radiographs are unreliable in quantifying the status of the posterior malleolus including determining the size of the fragment and if any incarcerated fragments and in these cases a CT scan has been shown to change operative planning in 44% of cases [17]. Therefore the authors of this chapter suggest that every ankle fracture with a posterior malleolar component (unless extremely small i.e. a flake) should get a pre-operative CT scan to truly assess the injury. In the case described herein the posterior malleolus was broken but the fragment was small and fixing the syndesmosis with a screw restores the function of the posterior inferior tibiofibular ligament
Weightbearing CT
The emergence of weightbearing CT is promising, and in recent studies the diastasis in unstable ankles is significantly greater compared to conventional CT [18]. In a recent systematic review, the surface area of the syndesmosis (SAS) has been shown to be the most reliable measurement in the diagnosis of syndesmotic instability using a weightbearing CT scan [19].
MRI
Magnetic resonance imaging (MRI) has 93% specificity and 100% sensitivity for anterior inferior tibiofibular ligament (AITFL) and 100% sensitivity and specificity for posterior inferior tibiofibular ligament (PITFL) disruptions [4]; however, it is an expensive investigation and usually not required in the acute assessment of the syndesmosis.
Although this case is straightforward, in general, the decision regarding performing a revision surgery of the syndesmosis based on radiographic parameters, for example on an ankle that shows some degree of asymmetry compared to the contralateral extremity in an otherwise nonpainful patient, remains tough and controversial as it would entail a relatively important surgery with prolonged no weightbearing in an asymptomatic patient. In these tough situations, the authors of this chapter would routinely obtain a post-operative bilateral CT scan to further assess the situation, for example whether the fixation was problematic to begin with and inform the patient that they may have a higher chance of getting ankle arthritis in the future. The decision is always tough one, and recommendations are based on multiple factors, and always on a case-by-case basis. In this patient presented herein, there was obvious distortion of the radiographic parameters, and it was clearly felt that the benefit of a revision surgery to address the syndesmosis and reduce the talus back into the mortise would be the appropriate management as the risk of not having surgery would definitely lead to early-onset debilitating arthritis.
Summary: Lessons Learned
-
Evaluation and treatment of ‘failed’ syndesmosis fixation is difficult and controversial.
-
There is no unified universal approach and each case should be individualized.
-
The case presented here shows successful treatment of a failed syndesmosis and mortise fixation in a patient due to obvious initial technical errors.
-
However, the moto ‘get it right the first time’ and correctly addressing the syndesmosis is crucial in ankle fractures, but not always feasible, as unpredictable factors, including the nature and severity of the injury, as well as patient factors may compromise outcome.
-
Good knowledge of the various imaging modalities and parameters, including pre-operative, intra-operative and post-operative imaging, is critical and those should complement a thorough history and examination of the individual patient in order to lead to optimal outcomes.
References
Kellett JJ, Lovell GA, Eriksen DA, Sampson MJ. Diagnostic imaging of ankle syndesmosis injuries: a general review. J Med Imaging Radiat Oncol. 2018;62(2):159–68.
White T, Bugler K. Ankle fractures. In: Tornetta P, Ricci W, Court-Brown C, McQueen M, McKee MM, editors. Rockwood and Green's fractures in adults. 9th ed. Lippincot Williams & Wilkins; 2020. p. 2822–76.
Fort NM, Aiyer AA, Kaplan JR, Smyth NA, Kadakia AR. Management of acute injuries of the tibiofibular syndesmosis. Eur J Orthop Surg Traumatol. 2017;27(4):449–59.
Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. 2015;41(6):601–14.
Walsh AS, Sinclair V, Watmough P, Henderson AA. Ankle fractures: getting it right first time. Foot (Edinb). 2018;34:48–52.
Kubik JF, Rollick NC, Bear J, Diamond O, Nguyen JT, Kleeblad LJ, et al. Assessment of malreduction standards for the syndesmosis in bilateral CT scans of uninjured ankles. Bone Joint J. 2021;103(1):178–83.
Tornetta P 3rd, Yakavonis M, Veltre D, Shah A. Reducing the syndesmosis under direct vision: where should i look? J Orthop Trauma. 2019;33(9):450–4.
Tornetta P 3rd, Axelrad TW, Sibai TA, Creevy WR. Treatment of the stress positive ligamentous SE4 ankle fracture: incidence of syndesmotic injury and clinical decision making. J Orthop Trauma. 2012;26(11):659–61.
Chu X, Salameh M, Byun SE, Hadeed M, Stacey S, Mauffrey C, et al. The utilization of intraoperative contralateral ankle images for syndesmotic reduction. Eur J Orthop Surg Traumatol. 2022;32(2):347–51.
Rammelt S, Md P, Boszczyk A, Md P. Computed tomography in the diagnosis and treatment of ankle fractures: a critical analysis review. JBJS Rev. 2018;6(12):e7.
Harwin SF, Schreiber JJ, McLawhorn AS, Dy CJ, Goldwyn EM. Intraoperative contralateral view for assessing accurate syndesmosis reduction. Orthopedics. 2013;36(5):360–1.
Summers HD, Sinclair MK, Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma. 2013;27(4):196–200.
Koenig SJ, Tornetta P 3rd, Merlin G, Bogdan Y, Egol KA, Ostrum RF, et al. Can we tell if the syndesmosis is reduced using fluoroscopy? J Orthop Trauma. 2015;29(9):e326–30.
Vetter SY, Euler J, Beisemann N, Swartman B, Keil H, Grützner PA, et al. Validation of radiological reduction criteria with intraoperative cone beam CT in unstable syndesmotic injuries. Eur J Trauma Emerg Surg. 2021;47(4):897–903.
Szymański T, Zdanowicz U. Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures-How much do we miss? Foot Ankle Surg. 2022;28(2):263–8.
Lee SW, Lee KJ, Park CH, Kwon HJ, Kim BS. The valid diagnostic parameters in bilateral CT scan to predict unstable syndesmotic injury with ankle fracture. Diagnostics (Basel). 2020;10(10):812.
Donohoe S, Alluri RK, Hill JR, Fleming M, Tan E, Marecek G. Impact of computed tomography on operative planning for ankle fractures involving the posterior malleolus. Foot Ankle Int. 2017;38(12):1337–42.
Del Rio A, Bewsher SM, Roshan-Zamir S, Tate J, Eden M, Gotmaker R, et al. Weightbearing cone-beam computed tomography of acute ankle syndesmosis injuries. J Foot Ankle Surg. 2020;59(2):258–63.
Raheman FJ, Rojoa DM, Hallet C, Yaghmour KM, Jeyaparam S, Ahluwalia RS, et al. Can weightbearing cone-beam CT reliably differentiate between stable and unstable syndesmotic ankle injuries? A systematic review and meta-analysis. Clin Orthop Relat Res. 2022;480(8):1547–62.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chloros, G.D., Santolini, E., Davidson, A.E., Vasilopoulou, A., Giannoudis, P.V. (2024). Ankle Syndesmosis Injury Failed Fixation. In: Giannoudis, P.V., Tornetta III, P. (eds) Failed Fracture Fixation. Springer, Cham. https://doi.org/10.1007/978-3-031-39692-2_39
Download citation
DOI: https://doi.org/10.1007/978-3-031-39692-2_39
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-39691-5
Online ISBN: 978-3-031-39692-2
eBook Packages: MedicineMedicine (R0)