Abstract
Introduction
Injuries to the distal tibiofibular syndesmosis are frequent and continue to generate controversy.
Methods
The majority of purely ligamentous injuries (“high ankle sprains”) is not sassociated with a latent or frank tibiofibular diastasis and may be treated with an extended protocol of physical therapy. Relevant instability of the syndesmosis with diastasis results from rupture of two or more ligaments that require surgical stabilization. Syndesmosis disruptions are commonly associated with bony avulsions or malleolar fractures. Treatment consists in anatomic reduction of the distal fibula into the corresponding incisura of the distal tibia and stable fixation. Proposed means of fixation are refixation of bony syndesmotic avulsions, one or two tibiofibular screws and suture button. There is no consensus on how long to maintain fixation. Both syndesmotic screws and suture buttons need to be removed if symptomatic.
Results/Complications
The most frequent complication is syndesmotic malreduction and may be minimized with open reduction and intraoperative 3D scanning. Other complications include hardware failure, heterotopic ossification, tibiofibular synostosis, chronic instability and posttraumatic arthritis.
Conclusion
The single most important prognostic factor is anatomic reduction of the distal fibula into the tibial incisura.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Injuries to the distal tibiofibular syndesmosis are estimated to occur in about 1–18 % of all ankle sprains [19, 34, 48] and up to 23 % of all ankle fractures [88, 133]. These injuries may be missed in the absence of a frank diastasis and if unrecognized lead to chronic instability and posttraumatic ankle arthritis [35, 77, 90]. The true prevalence of these injuries may, therefore, be higher than previously reported, as is also reflected in a high prevalence of late calcifications (up to 32 %) at the syndesmosis in professional football players [14, 124] and up to 50 % in patients with ankle fractures [113].
The syndesmotic complex provides a dynamic support to the ankle that is important for normal performance. While there is consensus that improper treatment of syndesmotic injuries is a negative prognostic factor in both sprains and fractures of the ankle, controversy prevails on many aspects of their management [89]. Over the last years, a plethora of articles has appeared that deals with the biomechanics, detection, reduction and fixation of syndesmotic injuries. This article reviews the current aspects of the management of syndesmotic injuries with an emphasis of studies that were published over the last 5 years.
Anatomy
The tibiofibular syndesmosis consists of a proximal part between the fibular head and the proximal tibial metaphysis that is formed by the Ligg. capitis fibulae anterior and posterior, the aponeurotic interosseous membrane, and the distal tibiofibular syndesmotic complex, for which the term syndesmosis is often used synonymously. The latter consists of five separate portions (Fig. 1).
Ankle specimen with the ligaments of the distal tibiofibular syndesmosis from anterior (a) and posterior (b): distal portion of the IOM interosseous membrane, AITFL anterior inferior tibiofibular ligament, PITFL posterior inferior tibiofibular ligament, TTFL transverse tibiofibular ligament. Photograph: Eddie Elsner, Dresden, Germany
The anterior–inferior tibiofibular ligament (AITFL) descends from the anterior tubercle of the tibia (Tillaux-Chaput) to the anterior tubercle of the distal fibula (Le Fort, Wagstaffe). It consists of 2–3 portions running parallel to each other. The posterior–inferior tibiofibular ligament (PITFL) descends posterolaterally from the posterior tubercle of the tibia (Earle) to the posterior margin of the distal fibula. It is more compact and runs more horizontally than the AITFL [6]. The transverse tibiofibular ligament (TTFL) lies distal to the posterior tibiofibular ligament and has a fibrocartilagineous appearance. It runs almost horizontally to the posterior tubercle of the fibula and is sometimes hard to discriminate from the posterior tibiofibular ligament. It has, therefore, synonymously been described as a deep portion of the PITFL, inferior transverse ligament (ITL), or a fibrocartilagineous reinforcement of the posterior capsule of the ankle joint [6, 28]. The interosseous tibiofibular ligament (IOL) contains short, strong collagenous and elastic fibers that fan out into a network almost completely filling the space between the tibial incisura and the corresponding medial margin of the fibula [41]. In the sagittal plane, it forms a triangle with its base 1–1.5 cm above the ankle joint level [6]. It lies in the pivot of the rotational plane of the distal fibula [45, 61]. Finally, the distal portion of the interosseous membrane (IOM) is considered by many as a separate part of the distal syndesmosis. It consists of aponeurotic fibers that are recruited from the cranial origins of the anterior and posterior tibiofibular ligaments in direct continuation of the apex of the pyramid-shaped IOL at 4–5 cm above the ankle joint level. Its fibers are thinner and longer than that of the IOL.
The shape of the fibular incision (incisura fibulae, peroneal groove) of the distal tibia at the level of the syndesmosis displays a considerable inter-individual variation [60, 74, 114]. The absolute depth of the incision varies between 1.0 and 7.5 mm [45, 60]. In anatomical studies, only 60–75 % of the specimens had a concave surface of the lateral aspect of the tibia, the remainder being shallow, irregularly shaped or slightly convex [24, 45]. The risk of malreduction of the distal fibula into the incision in cases of syndesmotic disruption may be increased with the latter configurations.
In a CT study of 107 normal ankles, Lepojärvi et al. [60] found the distal fibula to be situated either centrally or anteriorly within the incisura in 97 % of cases. They suggested that posterior translation indicates malreduction. They also found that the difference between anterior and posterior width of the incisura was significantly greater in males (2.7 mm) than in females (2.1 mm) and a high variation in the incisural width, as suggested earlier in radiographic studies [60, 114]. The authors cautioned that the larger joint size in males may lead to the false assumption of malreduction in some cases [60].
The anterior syndesmotic ligament is predominately or exclusively (63 %) supplied by the anterior branch of the peroneal artery, the anterior tibial artery providing additional branches in the remaining 37 %. The posterior syndesmotic ligaments are supplied by the posterior branch of the peroneal artery in 100 % [67]. The peroneal artery perforates the interosseous membrane at an average of 3 cm above the ankle joint level. The anterior tubercle of the tibia (Chaput) and underlying lateral tibial plafond are supplied by an anastomotic network between the perforating branch of the peroneal artery and the anterior tibial artery [20].
Biomechanical considerations
Because of the oblique axis of the ankle joint that ascends 8° in the frontal plane and 6° in the transverse plain, and the irregular shape of the talus, which is broader ventrally and laterally, the distal fibula performs a three-dimensional movement with respect to the distal tibia during physiological dorsiflexion and plantarflexion that is restricted by the tibiofibular syndesmosis [9, 19, 85, 92, 100, 112]. The deep portion of the deltoid ligament also contributes to syndesmotic stability acting as a restraint against lateral shift of the talus [96, 132].
Numerous biomechanical studies have evaluated the exact amount of the relative movement of the distal fibula with respect to the distal tibia with various methods. From maximum plantarflexion to dorsiflexion, the fibula moves 0.82–3 mm laterally [1, 19, 28, 43, 51, 53, 85, 110], 0.9–1.34 mm posteriorly [1, 43, 85, 110], and rotates externally 0.5°–3.7° [1, 5, 9, 19, 43, 85]. The intermalleolar distance increases with dorsiflexion of the talus by 1.0–1.25 mm [19, 85]. In addition, a distal translation of the fibular tip of about 2.4 mm has been observed during normal gait [92, 100].
Several sectioning studies have looked at the contribution of the different portions of the syndesmosis for mechanical stability. Ogilvie-Harris and colleagues [78] found that the AITFL provided 35 %, the TTFL 33 %, the IOL 22 %, and the PITFL 9 % of the overall tibiofibular stability. Xenos et al. [132] performed serial sectioning of the syndesmosis from anterior to posterior with a constant external rotation load of 5 Nm on the foot. Tibiofibular diastasis increased by 2.3 mm with dissection of the AITFL, by an additional 2.2 mm with sectioning of the distal 8 cm of the IOM resulted and by another 2.8 mm with sectioning of the PITFL. Sarsam and Hughes [96] found a 30° and 40° increase in external rotation of the talus through sectioning the AITFL after an experimental fibular fracture above and below the syndesmosis, respectively. Two studies found greater strength of the PITFL as compared to the AITFL although not significant in ten specimens [9, 97].
More recent experiments have demonstrated the importance of an intact IOL for overall stability of the syndesmosis complex [90]. Hoefnagels et al. [46] found a significantly superior stiffness and load to failure of the IOL over the AITFL in cadaver feet. It may be concluded from the existing studies that with the rupture of two or more syndesmotic ligaments relevant mechanical instability will result, although biomechanical data do not necessarily reflect the clinical situation [90].
Mechanism of injury
Syndesmotic injury is predominately produced by forced external rotation of the talus in the ankle mortise [26]. With the foot in dorsiflexion, the broader posterior part of the talus is forced into the ankle mortise thus putting an additional strain on the syndesmotic ligaments [30, 59, 132]. Both fractures of the distal fibula and ruptures of the syndesmosis ligaments have been produced experimentally in the nineteenth century by Maisonneuve and Hönigschmied [62] through forced external rotation. Back then, authors such as Chaput, Earle, LeFort and Wagstaffe produced and described bony avulsions of the syndesmotic ligaments that still bear their names [135].
In a biomechanical cadaver study, Markolf et al. [64] confirmed that forced ankle dorsiflexion and external foot torque applied to a dorsiflexed, axially loaded ankle could produce high ankle sprains (syndesmotic injuries). They suggested that the most likely mechanism was falling forward on a weight-bearing foot while rotating the tibia internally, putting an external rotation strain on the ankle. However, several other trauma mechanisms such as inversion and plantarflexion have been described in the literature [48].
Syndesmosis injuries may occur in isolation, but the majority of syndesmotic disruptions are produced in the wake of ankle fractures and fracture-dislocations. The sequel of syndesmotic injuries and associated fractures has been described extensively in the clinical and biomechanical series of Lauge-Hansen [59]. The syndesmotic ligaments will most likely be disrupted in pronation type ankle fractures with the foot in dorsiflexion at the time of injury [91], while relevant injury to the tibiofibular syndesmosis is less likely to occur in supination type ankle fractures [83].
Diagnosis
Clinical examination
Patients with an injury to the tibiofibular syndesmosis typically present with pain in the anterolateral aspect of the ankle joint that is aggravated by forced dorsiflexion. Pain over the syndesmosis can be provoked with passive external rotation of the foot in neutral position against the fixed lower leg [30]. Compressing the tibia to the fibula above the midpoint of the calf (“squeeze test”) provokes pain at the level of the distal tibiofibular syndesmosis [30, 48]. For the “cross-legged test”, the patient is sitting and rests the mid-tibia of the injured leg on the knee. The patient himself produces pain in the region of the syndesmosis with a gentle downward force on the medial side of the knee [55]. A functional “stabilization test” may be used in athletes with suspected syndesmosis sprains [129, 131]. A stabilizing athletic tape applied tightly above the ankle joint substantially reduced pain after standing, walking and performing a toe raise and jump.
So far, only the external rotation test has been shown to correlate with a syndesmotic injury and longer return to preinjury activities in clinical series [3, 8]. Biomechanical evaluation of the four common clinical test showed no accurate prediction of the degree of mechanical injury [10]. De César et al. [21] compared the results of clinical examination with the MRI findings in 56 patients. The prevalence of syndesmotic injuries in the MRI was 17.8 %. Both the external rotation test and the calf squeeze test had a low sensitivity (30 and 20 %, respectively) and high specificity (94 and 85 %, respectively), suggesting that a negative test does not preclude syndesmotic injury but a positive test is highly indicative of an injury to the syndesmosis [21].
Radiographic examination
Standard radiographs of the ankle include the lateral and anteroposterior view with the foot in 20 degrees of internal rotation (“mortise view”). Chaput, in 1907 [17], described the “ligne claire” (tibiofibular clear space, TCS) as a measure for syndesmotic integrity (Fig. 2). Other radiographic landmarks include the tibiofibular overlap (TFO) and the medial clear space (MCS). An anteroposterior view of the complete lower leg is done in case of local tenderness to exclude a proximal fibular (Maisonneuve’s) fracture or dislocation of the superior tibiofibular syndesmosis.
Landmarks on standard mortise (a) and lateral (b) radiographs: tibiofibular overlap (TFO), tibiofibular clear space (ligne claire, TCS), medial clear space (MCS), anterior tibiofibular interval (ATF), anteroposterior tibiofibular ratio (APTF = A/B [36])
Generally, a TCS of <6 mm, a TFO of 6 mm or more (or 42 % of the fibular width) in the AP view or >1 mm in the mortise view are considered to be normal [40]. Ostrum et al. [80], in a cadaveric study, revealed gender-specific differences. According to their data, a TCS <5.2 mm in females and <6.47 mm in females and a TFO >2.1 mm in females and >5.7 mm in males should be considered normal. This corresponds to a TFO of >24 % and a TCS of <44 % of the fibular width [80]. Similarly, Dikos et al. [23] noted that the tibiofibular interval in the CT scans of 30 healthy volunteers was significantly greater in men than in women. When evaluating the ankle radiographs of 392 patients without known pathology at the ankle, Shah et al. [102] found a mean tibiofibular overlap of 8.3 mm in the true ap view and 3.5 mm in the mortise view. The mean TCS was 4.6 and 4.3 mm, respectively. Interestingly, the authors found a subset of patients with a complete lack of tibiofibular overlap in the mortise view as a normal variant. They found the TCS in the mortise view to be the most accurate measurement with a side-to-side difference of only 0.7 mm.
Latent diastasis is proved with stress radiographs, if necessary under regional anesthesia (Fig. 3). External rotation stress is applied manually under fluoroscopy or lateral shift with a standardized Telos device on radiographs [90, 136]. Widening of the TCS and MCS of 2 mm and more is considered to be pathological [132].
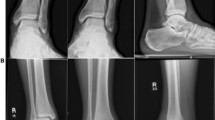
Computed tomography (CT) scanning is a more accurate method of detecting syndesmotic injuries, especially with diastases of 3 mm and less that may go undetected with plain radiographs [25, 32, 90]. CT scanning of both ankles allows determination of anteroposterior translation, rotation and shortening as well as the exact location of bony avulsions (Fig. 4). When obtaining CT scans in 30 healthy volunteers, Dikos et al. [23] found that tibiofibular intervals (the clear space as measured on CT scans) did not vary more than 2.3 mm and rotation of the fibula did not vary more than 6.5° between ankles of the same person.
CT scanning reveals tibiotalar subluxation in the coronal plane (a) and malposition of the distal fibula with respect to the incisura in the horizontal plane with a small bony avulsion of the PITFL (b). The case example shows an additional comminuted calcaneal fracture and talar body fracture in a complex foot trauma
Magnetic resonance imaging (MRI) has a 93 % specificity and 100 % sensitivity for injury of the AITFL and a 100 % specificity and sensitivity for injury of the PITFL when compared to arthroscopic findings in acute syndesmotic injuries [111]. It also detects injuries to the IOL (Fig. 5). Assessing syndesmotic injuries with MRI is associated with a high inter-observer agreement [73]. Sikka et al. [103] compared MRI findings to disability in professional football players. They found that an increasing grade of injury as judged with MRI was positively correlated with the number of missed games and practices.
Treatment
Indications for surgical fixation
Because the existing classification systems do not offer a clear therapeutic algorithm, clinical and radiographic examination should focus on detecting and documenting the amount of latent diastasis––as seen in stress radiographs and frank diastasis––which is obvious on plain radiographs [90]. As biomechanical studies with different setups have shown, lateral translation or shortening of 2 mm and external rotation of 5° of the distal fibula result in non-physiological pressure redistribution at the ankle joint [116, 134].
Instability of the distal tibiofibular syndesmosis with a frank or latent diastasis of more than 2 mm, either isolated or in conjunction with malleolar fractures, is treated with open reduction and fixation using one or two syndesmosis screws [41, 85, 90, 125]. For malleolar fractures, Boden and colleagues [12] concluded from biomechanical studies that a syndesmotic screw is warranted, if the fibular fracture extended more than 4.5 cm above the ankle joint line. These criteria have been confirmed by several clinical studies [19, 121]. However, all authors suggested that general radiographic criteria for syndesmotic fixation are of relatively low value compared with the intraoperative impression of syndesmotic stability or instability and should, therefore, only be used as a guide in the diagnosis and management of these injuries [121]. Nielson et al. [76] demonstrated that the level of the fibular fracture was not consistent with the level of disruption of the syndesmosis and the interosseous membrane in an MRI study and, therefore, concluded that the amount of syndesmotic injury cannot be detected by the radiographic level of the fibular fracture alone.
Patients without latent or frank diastasis (“high ankle sprains”) are treated with a short course of rest, ice, elevation and non-steroidal antiphlogistics (RICE) until subsidence of pain. This may include 1–3 weeks immobilization in a commercial brace or cast-boot followed by physical therapy to restore motion and strength and lastly sport-specific tasks in athletes [4, 129]. Patients have to be counseled that the time lost from sports is longer and residual complaints beyond 6 months are more frequent after syndesmotic sprains as compared to lateral ankle sprains [14, 34, 48, 113].
Intraoperative stress testing
When syndesmotic instability is suspected in malleolar fractures, stability of the syndesmotic complex is tested after open reduction and internal fixation of the fibular fracture. Most commonly, this is done by the hook test as described by Heim [41]. Under fluoroscopic control, the fibula is pulled laterally and dorsally. Because relevant disruption of the syndesmosis causes a three-dimensional instability, the fibula not only displaces laterally but also in the anteroposterior direction which can be tested clinically or in lateral radiographs [15, 78]. Alternatively, an intraoperative external rotation test is carried out. In cases of diastasis or anteroposterior instability of more than 2 mm fixation with a syndesmosis screw is indicated.
Relevant syndesmotic instability has to be expected in pronation injuries. However, Tornetta et al. [120] found that 45 % of operatively treated supination external rotation stage 4 (SER 4) injuries displayed syndesmotic instability on intraoperative stress examination. This underlines the general necessity of stressing the syndesmosis after internal fixation of malleolar fractures, because the osteoligamentous injury pattern is not always consistent with the predicted injury pattern according to the Lauge Hansen stages [31, 76, 89]. On the other hand, in a prospective-randomized study, Pakarinen et al. [82] found no differences between patients treated with syndesmotic fixation versus those treated without in SER 4 injuries with positive intraoperative external rotation stress testing. The authors concluded that in SER 4 injuries no relevant injury to the tibiofibular syndesmosis occurs. The numbers were small, because stress tests were positive in only 24 of 140 patients. The same was found by Kennedy et al. [54] in “low Weber C” fractures (i.e., within 5 cm of the ankle joint line).
Stoffel et al. [106], in a cadaveric experiment, found the lateral stress test (hook test) to be superior to the external rotation stress test for detecting syndesmotic instability. Pakarinen et al. [82] found good intraobserver agreement between the external rotation and hook tests but a poor sensitivity of both tests, suggesting that many syndesmotic injuries may go unnoticed. A cadaveric study suggested that 100 Nm of lateral force may be a benchmark for the hook test because no significant widening of the TCS occurs beyond that force [106].
Technique of reduction
In cases of relevant instability, the syndesmosis should be visualized directly via an anterolateral or lateral approach to clear the space between the distal tibia and fibula from avulsed ligaments and to facilitate reduction of bony avulsions [89]. Direct visual assessment of the alignment of the anterior tubercles of the distal tibia and fibula also helps avoiding malreduction [84].
Reduction of the distal fibula into the tibial incisura is best achieved with a pointed reduction clamp (Fig. 6). The clamp should be placed exactly in the axis of the ankle joint to minimize the risk of malreduction [87, 90]. The insertion points should be the lateral malleolar ridge on the fibula and the central part of the medial cortex at the tibia. Malposition of the reduction clamp, i.e., obliquely to the axis of the ankle joint, resulted in malreduction of the distal fibula in cadaveric experiments and the amount of malreduction increased with the degree of instability [87].
a Frank diastasis with widened TCS and MCS in a 20 year old skater. b MRI shows disruption of the AITFL; IOL and PITFL (arrows). c The syndesmosis is visualized via an anterolateral approach, showing a small avulsion of the AITFL at Chaput’s tubercle. The ruptured AITFL is marked with sutures. d–f Reduction is achieved with an overriding pointed clamp and fixation is achieved with two transsyndesmotic screws. g, h Postoperative CT scanning shows correct rotation, anteroposterior alignment and length of the distal fibula
Assessment of reduction
Several studies have shown that exact assessment of syndesmotic reduction cannot be achieved reliably with two-dimensional fluoroscopy or post reduction radiographs. The reported rates of malreduction when compared with three-dimensional fluoroscopy or postreduction CT lie between 22 and 52 % [29, 31, 65, 69, 90, 93, 95, 104, 122].
While the fibular length can be assessed reliably in mortise radiographs of the ankle using Weber’s classical landmarks, rotational and anteroposterior displacement cannot be detected with the same reliability. The position of the distal fibula with respect to the tibia can be assessed on lateral radiographs [125]. The anterior tibiofibular interval on lateral ankle radiographs is one measure of syndesmotic integrity and fibular position within the tibial incisura [109, 127, 132]. More recently, Grenier et al. [36] found the anteroposterior tibiofibular ratio (APTF) measured on lateral fluoroscopic view to have a good inter- and intraobserver reliability. The APTF in their 30 patients (60 ankles without pathology) averaged 0.94 with a range of 0.63–1.31. The side-to-side differences were not significant.
Measuring rotation on either anteroposterior or lateral views is particularly difficult. As much as 30° of external rotation of the fibula may go undetected with standard 2D intraoperative fluoroscopy [65]. On the other hand, 10° of internal fibular rotation could be detected reliably with standard fluoroscopy. There is no consensus on how to measure fibular rotation within the tibial incisura on axial CT scans. Knops et al. [57] compared four different methods in a cadaver experiment. They found the angle between the tangent to the anterior tibial surface at its most anterior point and the bisection of the vertical midline of the fibula as described by Zwipp [136] are fairly reliable and accurate with a greater ease of measurement and less anatomic variability as compared to the other methods.
Direct visualization of the syndesmosis is helpful in reducing the rates of malreduction. To avoid anteroposterior displacement, the alignment of the anterior margin of the fibula and tibia (Tubercule de Chaput) should be assessed clinically via the existing approach [90]. In a small comparative study of 12 patients, Pelton et al. [84] showed an unacceptable rate of malreduction when treating Maisonneuve Type syndesmotic injuries in a closed manner, while open reduction with direct visualization of the syndesmosis lead to anatomic or near-anatomic reduction in all cases. Still, Miller et al. [69] reported a 16 % rate of malreduction with direct visualization. Similarly, Sagi et al. [95], in a study of 107 syndesmotic injuries, reported a 15 % malreduction rate with open reduction compared to a 44 % malreduction rate with closed reduction of the syndesmosis.
Although the inter-individual variation of the morphology of the distal tibiofibular joint is considerable [45, 74], the intra-individual differences between the two ankles of one individual are minimal [23, 36, 109]. Therefore, the contralateral, uninjured ankle may serve as a template for reduction of the distal tibiofibular joint. Summers et al. [109] obtained anatomic reduction of the distal fibula into the tibial incisura while comparing the relationship of the distal tibia to the fibula on both the anteroposterior and lateral fluoroscopic images to the contralateral, uninjured side in 17 of 18 patients. Correct reduction was confirmed with 3D fluoroscopy.
Technique of fixation
The classical fixation of syndesmosis ruptures accompanied by a malleolar fracture is a single 3.5 mm cortical screw positioned between 1 and 4 cm above the ankle joint level (Fig. 7) after fixation of the distal fibula [41, 125]. The screw is not over drilled to avoid lagging. The anterior tibiofibular ligament is sutured separately or reattached with a small or mini-fragment screw in cases of bony avulsion at the distal tibia or fibula. In cases of pure ligamentous syndesmosis rupture––including Maisonneuve injuries, in the authors’ practice a second screw is introduced parallel to and above the first one to assure rotational stability [90]. The two screws can be connected by a small two-hole plate to increase torque resistance, e.g., in osteoporotic bone [33].
a, b In ankle fracture-dislocations with syndesmotic disruption, internal fixation of the distal fibula and medial malleolus is followed by transsyndesmotic screw fixation (same patient as in Fig. 4). c, d At 1 year follow-up and complete implant removal at the ankle, the mortise is stable without signs of posttraumatic arthritis. Salvage of the ankle joint was particularly important in this case because the subtalar joint had to be fused after a comminuted calcaneal fracture
Several biomechanical and clinical studies revealed no relevant differences regarding stability and functional outcome measurements, respectively, between one or two syndesmotic screws [47, 128], titanium or stainless steel screws [7], tri- or quadricortical screws [7, 72], transsyndesmotic or suprasyndesmotic screws [58], metal or bioabsorbable screws [2, 49, 117]. Biomechanical testing of 4.5 vs. 3.5 mm screws revealed conflicting results [39, 115]. In a finite element analysis, Verim et al. [123] found the lowest von Mises stress in the screws placed 30–40 mm above the ankle joint line and, therefore, suggested this position for syndesmotic screw placement. McBryde et al. [66], in a biomechanical study, found that placement of the screw within 2 cm of the tibiotalar joint line was associated with less widening of the TCS than screw placement 3.5 cm above the joint line.
The use of suture button repair aims at allowing a more physiological motion of the distal fibula with respect to the tibia while maintaining adequate stability [101]. This technique was shown to be biomechanically equivalent to both a 3.5 mm tricortical [56] and a 4.5 mm quadricortical screw [119] and associated with faster rehabilitation in a clinical study [118]. The functional outcomes at the short term (12–28 months) do not show significant differences with respect to the AOFAS scores as compared to syndesmotic screw placement [98]. Patients with suture button fixation required less implant removal than those fixed with a syndesmotic screw. However, the need for screw removal is questioned in the literature, as detailed below. When comparing syndesmotic screw fixation to tightrope fixation in a clinical study, the only variable that had a significant influence on functional outcome was anatomic reduction of the distal fibula into the incisura [75].
In ankle fractures and fracture-dislocations, direct fixation of the posterior tibial fragment (“posterior malleolus”) firmly reattaches the posterior tibiofibular ligament and, therefore, significantly contributes to syndesmotic stabilization [70, 91]. In a cadaver study, posterior malleolus fixation was superior to transsyndesmotic fixation in restoring stiffness to the ankle joint [31]. In this experiment, posterior malleolus fixation restored stiffness of the cadaver ankle specimens to 70 %, while syndesmotic screw fixation only restored stiffness to 40 %. Direct fixation with either screws or an antiglide plate from posteriorly ensures anatomic fixation and provides more stability as compared to indirect fixation from anteriorly [91, 126]. After fixation of the malleolar fractures and the posterior tibial fragment, the need for an additional transsyndesmotic screw should be tested intraoperatively as outlined above (Fig. 8).
a, b Multifragmentary fracture of the posterior tibial plafond in a trimalleolar ankle fracture c necessitating a direct posterior approach for restoring joint congruity. d, e Fixation of the posterior tubercle of the tibia restores syndesmotic stability after internal fixation of the distal fibula and medial malleolus, obviating the need for an additional transsyndesmotic screw. f, g Postoperative radiographs
To retain or to remove the syndesmotic screw?
Controversy prevails on how long to retain syndesmotic screws and the overall need for removal [89, 99]. As per AO recommendation, syndesmosis screws are kept in place for 6–8 weeks with the patient restricted to 15 kg partial weight-bearing in a below knee cast or special boot [41, 129]. Many authors advocate removal of the screw(s) not before 3 months or in symptomatic patients only [25, 40, 63, 69, 104].
The syndesmosis screw restricts normal ankle motion [50, 85]. If the screw is left in place with the patient fully weight-bearing, screw breakage occurs in 7–29 % [99, 108] and osteolysis around the screw in 68–91 % [37, 41], while the ankle joint regains its physiological tibiofibular clearance. Screw breakage appears to be dependent on the screw diameter and the time of fixation. Stuart and Panchbhavi have found that 3.5 mm screws are significantly more likely to break than 4.0 or 4.5 mm screws [108]. The clinical relevance of screw breakage remains to be further elucidated. Hamid et al. [37] found superior functional results as measured with the AOFAS score in patients with retained broken screws (92.4) than in patients with retained intact screws (83.1). Manjoo et al. [63] found superior results with broken, loosened or removed screws compared with intact screws. The authors suggested removal of intact screws only. It can be speculated that screw breakage restores the normal physiological movement between the distal tibia and fibula.
Miller et al. [71] found superior ankle motion and functional outcome scores at 2 weeks after locked screw removal compared with retained screws. However, these improvements plateaued in the further course with no significant differences remaining after 12 weeks. Schepers et al. [99] reported a 22 % complication rate following screw removal, including infection in 9 % and recurrent diastasis in 7 % of cases. Song et al. [104], in a prospective radiographic study, found that syndesmosis malunions detected on postoperative CT scans corrected spontaneously in 8 of 9 patients 1 month after removal of the syndesmotic screw and full weight-bearing.
Implant removal may also be necessary after suture endobutton fixation of syndesmotic injuries. DeGroot et al. [22] reported that 6 of 24 treated with suture button repair required removal due to local irritation or lack of motion. Storey et al. [107] reported removal of the suture button in 8 of 102 cases for the following reasons: osteomyelitis, aseptic osteolysis, failure of stabilization, and unexplained pain over the implant.
Complications
The most common problem in the treatment of syndesmotic disruptions is malreduction of the distal fibula into the tibial incisura which has been addressed extensively above. Treatment consists of anatomic reduction as early as possible. When analyzing 5,123 consecutive ankle fractures, Ovaska et al. [81] found a 1.6 % reoperation rate. The majority of patients undergoing surgical revision had malreduction of the syndesmosis (47 of 79, 59 %), most commonly malposition of the distal fibula in the tibial incisura. Secondary correction was successful in 84 %. Heineck et al. [42] showed in a cadaver model that secondary correction can be performed reproducibly within 1.9° of rotation and 1.5 mm of translation when using K-wires for marking the deformity as assessed with CT scans. Correction of syndesmotic malreduction should be carried out as early as possible to avoid late complications such as chronic ankle instability and posttraumatic arthritis [90].
The overall rate of wound infections after ankle fractures with or without syndesmotic disruption is <2 % [105]. High rates of infection and nonunion (17 %) have recently been reported with high-energy transsyndesmotic ankle fracture-dislocations (“logsplitter fracture”) [11]. The rate of posttraumatic arthritis was 70 % in a series of 23 of these high-energy injuries, reflecting the amount of soft tissue injury (more than half of the patients had open fractures) and marginal involvement of the tibial plafond.
Failure of syndesmosis fixation is twelve times more likely to occur in obese patients than in patients with normal weight when adjusting the data for injury severity [68]. Patients with complicated diabetes are 3.4× more likely to develop complications such as malunion or nonunion after malleolar fractures than those without [89]. Multiple tibiofibular screws, augmented fixation with bone cement and fibular plate fixation with multiple screws have been suggested to avoid failure of fixation in these patients [33, 89].
With tightrope fixation, wound problems and irritations at the knot over the fibula have been described in 17 % of cases [75]. Burying the knot in a recess beneath the fibular periosteum has been suggested to eliminate this problem. DeGroot et al. [22] observed osteolysis and subsidence of the device into the bone in 4 of 24 cases and heterotopic ossification in 3 of 24 cases after suture button repair.
Heterotopic ossifications at the distal tibiofibular joint (Fig. 9) have been observed in up to 50 % of patients with follow-up radiographs after syndesmotic injury [113]. The prevalence has been reported to be higher with the use of bioabsorbable screws [13]. The prevalence of a tibiofibular synostosis has been reported in 1.7–18.2 % [16, 86, 130]. Recently, Hinds et al. [44], in a study of 564 ankle fractures, identified male sex (OR = 2.82), syndesmotic screw fixation (OR = 2.46) and tibiofibular dislocation (OR = 1.74) as independent risk factors for the development of a complete synostosis (as seen in 16.1 % of all patients) and incomplete bony bridging (seen in 8.2 %). Plantarflexion, dorsiflexion and inversion were significantly reduced in patients with radiographic tibiofibular synostosis [40]. Karapinar et al. [52] noted a higher rate of tibiofibular synostosis after quadricortical screw fixation compared with tricortical screw fixation. However, there was no difference in the functional outcomes after 2 years. Symptomatic synostosis requires surgical removal.
For reduced range, ankle of motion due to intra-articular adhesions following syndesmotic injury, arthroscopic debridement and chondroplasty, if indicated, relieves symptoms in the short term [77, 78]. Han and colleagues [38] reported significant functional improvement from arthroscopic marginal resection of chronically injured syndesmosis ligaments irrespective of additional screw fixation, and suggested that hypertrophy and impingement are the main causes of pain in chronic syndesmotic injury.
Chronic syndesmotic instability results from inadequate detection or fixation of syndesmosis disruptions. It is characterized by continued pain, limited ankle range of motion and the inability to perform on a preinjury level after syndesmosis injuries with or without malleolar fractures. Typically, patients report a sensation of giving way and pain while walking on uneven grounds [90, 136]. Treatment consists in a secondary, near-anatomic syndesmoplasty, preferably with one half of the peroneus longus tendon [35].
Olson et al. [79] reported favorable results of tibiofibular arthrodesis in ten patients at a minimum follow-up of 2 years. Two patients required reoperation but no secondary ankle fusion became necessary. However, the potential problems of tibiofibular synostosis as discussed above should be borne in mind.
Results
The results of non-operative, functional treatment of syndesmosis sprains without diastasis are favorable with good to excellent outcomes reported in 86–100 % and full return to sports in almost all cases [4, 34, 113].
The pioneers of operative fracture treatment, Chaput and Quénu, already found that malleolar fractures with diastasis carry a worse prognosis than those without [17]. In recent clinical studies, the mere presence of a syndesmotic injury is a negative prognostic factor in malleolar fractures [27, 127].
There is evidence from numerous clinical series that anatomic reduction of the distal fibula within the incision at the distal tibia is the single most important prognostic factor in the treatment of malleolar fracture with syndesmotic disruption [18, 26, 54, 75, 95, 127, 128]. Chissel and Jones, in a study of 43 patients with Weber type C ankle fractures, of which 31 were treated with a syndesmosis screw, found that a syndesmotic widening of more than 1.5 mm was associated with an unacceptable outcome at 2–8 years follow-up [18]. Sagi et al. [94] when comparing severe with non-severe ankle fractures requiring syndesmotic stabilization still found syndesmotic malreduction to give significantly worse outcomes in both groups. Wikerøy et al. [128] at a follow-up of 8.4 years noted poorer functional scores in patients with a difference in the syndesmotic width between the operated and the non-operated ankle of 1.5 mm or more. Although several studies suggested an overuse of the syndesmosis screw, this did not adversely affect the functional result [18, 90].
References
Ahl T, Dalen N, Lundberg A, et al. Mobility of the ankle mortise. A roentgen stereophotogrammetric analysis. Acta Orthop Scand. 1987;58:401–2.
Ahmad J, Raikin SM, Pour AE, et al. Bioabsorbable screw fixation of the syndesmosis in unstable ankle injuries. Foot Ankle Int. 2009;30:99–105.
Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27:276–84.
Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14:232–6.
Barnett CH, Napier JR. The axis of rotation at the ankle joint in man; its influence upon the form of the talus and the mobility of the fibula. J Anat. 1952;86:1–9.
Bartoniček J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25:379–86.
Beumer A, Campo MM, Niesing R, et al. Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury. 2005;36:60–4.
Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73:667–9.
Beumer A, Valstar ER, Garling EH, et al. Kinematics of the distal tibiofibular syndesmosis: radiostereometry in 11 normal ankles. Acta Orthop Scand. 2003;74:337–43.
Beumer A, Van Hemert WL, Swierstra BA, et al. A biomechanical evaluation of clinical stress tests for syndesmotic ankle instability. Foot Ankle Int. 2003;24:358–63.
Bible JE, Sivasubramaniam PG, Jahangir AA, et al. High-energy transsyndesmotic ankle fracture dislocation–the “Logsplitter” injury. J Orthop Trauma. 2014;28:200–4.
Boden SD, Labropoulos PA, Mccowin P, et al. Mechanical considerations for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am. 1989;71:1548–55.
Böstman OM. Distal tibiofibular synostosis after malleolar fractures treated using absorbable implants. Foot Ankle. 1993;14:38–43.
Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–8.
Candal-Couto JJ, Burrow D, Bromage S, et al. Instability of the tibio-fibular syndesmosis: have we been pulling in the wrong direction? Injury. 2004;35:814–8.
Cedell CA. Supination-outward rotation injuries of the ankle. A clinical and roentgenological study with special reference to the operative treatment. Acta Orthop Scand. 1967;110:113.
Chaput V. Les fractures malleolaires du cou-de-pieds et les accidents du travail. Paris: Masson; 1907.
Chissell HR, Jones J. The influence of a diastasis screw on the outcome of Weber type-C ankle fractures. J Bone Joint Surg Br. 1995;77:435–8.
Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am. 1956;38:761–81.
Cronier P, Steiger V, Rammelt S. Early open reduction and internal fixation of Pilon fractures. Fuß Sprunggel. 2012;10:12–26.
De Cesar PC, Avila EM, De Abreu MR. Comparison of magnetic resonance imaging to physical examination for syndesmotic injury after lateral ankle sprain. Foot Ankle Int. 2011;32:1110–4.
DeGroot H, Al-Omari AA, El Ghazaly SA. Outcomes of suture button repair of the distal tibiofibular syndesmosis. Foot Ankle Int. 2011;32:250–6.
Dikos GD, Heisler J, Choplin RH, et al. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma. 2012;26:433–8.
Ebraheim NA, Lu J, Yang H, et al. The fibular incisure of the tibia on CT scan: a cadaver study. Foot Ankle Int. 1998;19:318–21.
Ebraheim NA, Mekhail AO, Gargasz SS. Ankle fractures involving the fibula proximal to the distal tibiofibular syndesmosis. Foot Ankle Int. 1997;18:513–21.
Edwards GS Jr, Delee JC. Ankle diastasis without fracture. Foot Ankle. 1984;4:305–12.
Egol KA, Pahk B, Walsh M, et al. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma. 2010;24:7–11.
Fick R Handbuch der Anatomie und Mechanik der Gelenke unter Berücksichtigung der bewegenden Muskeln. Part I: Anatomie der Gelenke Fischer; Jena 1904.
Franke J, Von Recum J, Suda AJ, et al. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am. 2012;94:1386–90.
Frick H. Diagnosis, therapy and results of acute instability of the syndesmosis of the upper ankle joint (isolated anterior rupture of the syndesmosis) [in German]. Orthopäde. 1986;15:423–6.
Gardner MJ, Brodsky A, Briggs SM, et al. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res. 2006;447:165–71.
Gardner MJ, Demetrakopoulos D, Briggs SM, et al. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788–92.
Gardner R, Yousri T, Holmes F, et al. Stabilization of the syndesmosis in the Maisonneuve fracture–a biomechanical study comparing 2-hole locking plate and quadricortical screw fixation. J Orthop Trauma. 2013;27:212–6.
Gerber JP, Williams GN, Scoville CR, et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19:653–60.
Grass R, Rammelt S, Biewener A, et al. Peroneus longus ligamentoplasty for chronic instability of the distal tibiofibular syndesmosis. Foot Ankle Int. 2003;24:392–7.
Grenier S, Benoit B, Rouleau DM, et al. APTF: anteroposterior tibiofibular ratio, a new reliable measure to assess syndesmotic reduction. J Orthop Trauma. 2013;27:207–11.
Hamid N, Loeffler BJ, Braddy W, et al. Outcome after fixation of ankle fractures with an injury to the syndesmosis: the effect of the syndesmosis screw. J Bone Joint Surg Br. 2009;91:1069–73.
Han SH, Lee JW, Kim S, et al. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28:336–42.
Hansen M, Le L, Wertheimer S, et al. Syndesmosis fixation: analysis of shear stress via axial load on 3.5-mm and 4.5-mm quadricortical syndesmotic screws. J Foot Ankle Surg. 2006;45:65–9.
Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10:156–60.
Heim U. Malleolar fractures [in German]. Unfallheilkunde. 1983;86:248–58.
Heineck J, Serra A, Haupt C, et al. Accuracy of corrective osteotomies in fibular malunion: a cadaver model. Foot Ankle Int. 2009;30:773–7.
Henkemeyer U, Püschel R, Burri C. Experimentelle Untersuchungen zur Biomechanik der Syndesmose. Langenbecks Arch Chir Suppl Forum. 1975; 369–371.
Hinds RM, Lazaro LE, Burket JC, et al. Risk factors for posttraumatic synostosis and outcomes following operative treatment of ankle fractures. Foot Ankle Int. 2014;35:141–7.
Höcker K, Pachucki A. The fibular incisure of the tibia. The cross-sectional position of the fibula in distal syndesmosis [in German]. Unfallchirurg. 1989;92:401–6.
Hoefnagels EM, Waites MD, Wing ID, et al. Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int. 2007;28:602–4.
Høiness P, Stromsøe K. Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma. 2004;18:331–7.
Hopkinson WJ, St Pierre P, Ryan JB, et al. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325–30.
Hovis WD, Kaiser BW, Watson JT, et al. Treatment of syndesmotic disruptions of the ankle with bioabsorbable screw fixation. J Bone Joint Surg Am. 2002;84-A:26–31.
Huber T, Schmoelz W, Bolderl A. Motion of the fibula relative to the tibia and its alterations with syndesmosis screws: A cadaver study. Foot Ankle Surg. 2012;18:203–9.
Jend HH, Ney R, Schottle H. Movements of the fibula [German]. Unfallchirurg. 1987;90:144–7.
Karapinar H, Kalenderer O, Karapinar L, et al. Effects of three- or four-cortex syndesmotic fixation in ankle fractures. J Am Podiat Med Assoc. 2007;97:457–9.
Kärrholm J, Hansson LI, Selvik G. Mobility of the lateral malleolus. A roentgen stereophotogrammetric analysis. Acta Orthop Scand. 1985;56:479–83.
Kennedy JG, Soffe KE, Dalla Vedova P, et al. Evaluation of the syndesmotic screw in low Weber C ankle fractures. J Orthop Trauma. 2000;14:359–66.
Kiter E, Bozkurt M. The crossed-leg test for examination of ankle syndesmosis injuries. Foot Ankle Int. 2005;26:187–8.
Klitzman R, Zhao H, Zhang LQ, et al. Suture-button versus screw fixation of the syndesmosis: a biomechanical analysis. Foot Ankle Int. 2010;31:69–75.
Knops SP, Kohn MA, Hansen EN, et al. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. 2013;34:1403–10.
Kukreti S, Faraj A, Miles JN. Does position of syndesmotic screw affect functional and radiological outcome in ankle fractures? Injury. 2005;36:1121–4.
Lauge-Hansen N. Fractures of the ankle II: combined experimental/surgical and experimental roentgenologic investigation. Arch Surg. 1950;60:957–85.
Lepojärvi S, Pakarinen H, Savola O, et al. Posterior translation of the fibula may indicate malreduction: CT study of normal variation in uninjured ankles. J Orthop Trauma. 2014;28:205–9.
Lutz W. Zur Struktur der unteren Tibiofibularverbindung und der Membrana interossea cruris. Anat Entwicklungsgesch. 1942;111:315.
Maisonneuve MJG. Recherches sur la fracture du peroné. Arch Gén de Med. 1840;7:165–87.
Manjoo A, Sanders DW, Tieszer C, et al. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma. 2010;24:2–6.
Markolf KL, Jackson S, Mcallister DR. Force and displacement measurements of the distal fibula during simulated ankle loading tests for high ankle sprains. Foot Ankle Int. 2012;33:779–86.
Marmor M, Hansen E, Han HK, et al. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32:616–22.
McBryde A, Chiasson B, Wilhelm A, et al. Syndesmotic screw placement: a biomechanical analysis. Foot Ankle Int. 1997;18:262–6.
McKeon KE, Wright RW, Johnson JE, et al. Vascular anatomy of the tibiofibular syndesmosis. J Bone Joint Surg Am. 2012;94:931–8.
Mendelsohn ES, Hoshino CM, Harris TG, et al. The effect of obesity on early failure after operative syndesmosis injuries. J Orthop Trauma. 2013;27:201–6.
Miller AN, Carroll EA, Parker RJ, et al. Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int. 2009;30:419–26.
Miller AN, Carroll EA, Parker RJ, et al. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res. 2010;468:1129–35.
Miller AN, Paul O, Boraiah S, et al. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma. 2010;24:12–6.
Moore JA Jr, Shank JR, Morgan SJ, et al. Syndesmosis fixation: a comparison of three and four cortices of screw fixation without hardware removal. Foot Ankle Int. 2006;27:567–72.
Muhle C, Frank LR, Rand T, et al. Tibiofibular syndesmosis: high-resolution MRI using a local gradient coil. J Comput Assist Tomogr. 1998;22:938–44.
Mukhopadhyay S, Metcalfe A, Guha AR, et al. Malreduction of syndesmosis–are we considering the anatomical variation? Injury. 2011;42:1073–6.
Naqvi GA, Cunningham P, Lynch B, et al. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40:2828–35.
Nielson JH, Gardner MJ, Peterson MG, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;436:216–21.
Ogilvie-Harris DJ, Gilbart MK, Chorney K. Chronic pain following ankle sprains in athletes: the role of arthroscopic surgery. Arthroscopy. 1997;13:564–74.
Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10:558–60.
Olson KM, Dairyko GH Jr, Toolan BC. Salvage of chronic instability of the syndesmosis with distal tibiofibular arthrodesis: functional and radiographic results. J Bone Joint Surg Am. 2011;93:66–72.
Ostrum RF, De Meo P, Subramanian R. A critical analysis of the anterior-posterior radiographic anatomy of the ankle syndesmosis. Foot Ankle Int. 1995;16:128–31.
Ovaska MT, Makinen TJ, Madanat R, et al. A comprehensive analysis of patients with malreduced ankle fractures undergoing re-operation. Int Orthop. 2014;38:83–8.
Pakarinen H, Flinkkila T, Ohtonen P, et al. Intraoperative assessment of the stability of the distal tibiofibular joint in supination-external rotation injuries of the ankle: sensitivity, specificity, and reliability of two clinical tests. J Bone Joint Surg Am. 2011;93:2057–61.
Pakarinen HJ, Flinkkila TE, Ohtonen PP, et al. Syndesmotic fixation in supination-external rotation ankle fractures: a prospective randomized study. Foot Ankle Int. 2011;32:1103–9.
Pelton K, Thordarson DB, Barnwell J. Open versus closed treatment of the fibula in Maissoneuve injuries. Foot Ankle Int. 2010;31:604–8.
Peter RE, Harrington RM, Henley MB, et al. Biomechanical effects of internal fixation of the distal tibiofibular syndesmotic joint: comparison of two fixation techniques. J Orthop Trauma. 1994;8:215–9.
Phillips WA, Schwartz HS, Keller CS, et al. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67–78.
Phisitkul P, Ebinger T, Goetz J, et al. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg Am. 2012;94:2256–61.
Purvis GD. Displaced, unstable ankle fractures: classification, incidence, and management of a consecutive series. Clin Orthop Relat Res. 1982;165:91–8.
Rammelt S, Heim D, Hofbauer LC, et al. Problems and controversies in the treatment of ankle fractures [German]. Unfallchirurg. 2011;114:847–60.
Rammelt S, Zwipp H, Grass R. Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. Foot Ankle Clin. 2008;13:611–33.
Rammelt S, Zwipp H, Mittlmeier T. Operative treatment of pronation fracture–dislocations of the ankle [German]. Operat Orthop Traumatol. 2013;25:273–91.
Reimann R, Anderhuber F. Kompensationsbewegungen der Fibula, die durch die Keilform der Torchlea tali erzwungen werden. Acta Anat. 1980;108:60–7.
Ruan Z, Luo C, Shi Z, et al. Intraoperative reduction of distal tibiofibular joint aided by three-dimensional fluoroscopy. Technol Health Care. 2011;19:161–6.
Sagi C, Shah A. In response. J Orthop Trauma. 2013;27:e247–8.
Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26:439–43.
Sarsam IM, Hughes SP. The role of the anterior tibio-fibular ligament in talar rotation: an anatomical study. Injury. 1988;19:62–4.
Sauer HD, Jungfer E, Jungbluth KH. Experimentelle Untersuchungen zur Reißfestigkeit des Bandapparates am menschlichen Sprunggelenk. Hefte Unfallheilkd. 1978;131:37–42.
Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36:1199–206.
Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. 2011;131:879–83.
Scranton PE Jr, Mcmaster JG, Kelly E. Dynamic fibular function: a new concept. Clin Orthop Relat Res. 1976;118:76–81.
Seitz WH Jr, Bachner EJ, Abram LJ, et al. Repair of the tibiofibular syndesmosis with a flexible implant. J Orthop Trauma. 1991;5:78–82.
Shah AS, Kadakia AR, Tan GJ, et al. Radiographic evaluation of the normal distal tibiofibular syndesmosis. Foot Ankle Int. 2012;33:870–6.
Sikka RS, Fetzer GB, Sugarman E, et al. Correlating MRI findings with disability in syndesmotic sprains of NFL players. Foot Ankle Int. 2012;33:371–8.
Song DJ, Lanzi JT, Groth AT, et al. The effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint: a prospective radiographic study. Foot Ankle Int. 2014;35:543–8.
SooHoo NF, Krenek L, Eagan MJ, et al. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91:1042–9.
Stoffel K, Wysocki D, Baddour E, et al. Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis. A cadaveric study. J Bone Joint Surg Am. 2009;91:2646–52.
Storey P, Gadd RJ, Blundell C, et al. Complications of suture button ankle syndesmosis stabilization with modifications of surgical technique. Foot Ankle Int. 2012;33:717–21.
Stuart K, Panchbhavi VK. The fate of syndesmotic screws. Foot Ankle Int. 2011;32:S519–25.
Summers HD, Sinclair MK, Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma. 2013;27:196–200.
Svensson OK, Lundberg A, Walheirn G, et al. In vivo fibular motions during various movements of the ankle. Clin Biomech. 1989;4:155–60.
Takao M, Ochi M, Oae K, et al. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324–9.
Tang CW, Roidis N, Vaishnav S, et al. Position of the distal fibular fragment in pronation and supination ankle fractures: a CT evaluation. Foot Ankle Int. 2003;24:561–6.
Taylor DC, Englehardt DL, Bassett FH 3rd. Syndesmosis sprains of the ankle. The influence of heterotopic ossification. Am J Sports Med. 1992;20:146–50.
Teramoto A, Kura H, Uchiyama E, et al. Three-dimensional analysis of ankle instability after tibiofibular syndesmosis injuries: a biomechanical experimental study. Am J Sports Med. 2008;36:348–52.
Thompson MC, Gesink DS. Biomechanical comparison of syndesmosis fixation with 3.5- and 4.5-millimeter stainless steel screws. Foot Ankle Int. 2000;21:736–41.
Thordarson DB, Motamed S, Hedman T, et al. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am. 1997;79:1809–15.
Thordarson DB, Samuelson M, Shepherd LE, et al. Bioabsorbable versus stainless steel screw fixation of the syndesmosis in pronation-lateral rotation ankle fractures: a prospective randomized trial. Foot Ankle Int. 2001;22:335–8.
Thornes B, Shannon F, Guiney AM, et al. Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res. 2005;431:207–12.
Thornes B, Walsh A, Hislop M, et al. Suture-endobutton fixation of ankle tibio-fibular diastasis: a cadaver study. Foot Ankle Int. 2003;24:142–6.
Tornetta P 3rd, Axelrad TW, Sibai TA, et al. Treatment of the stress positive ligamentous SE4 ankle fracture: incidence of syndesmotic injury and clinical decision making. J Orthop Trauma. 2012;26:659–61.
Van Den Bekerom MP, Haverkamp D, Kerkhoffs GM, et al. Syndesmotic stabilization in pronation external rotation ankle fractures. Clin Orthop Relat Res. 2010;468:991–5.
Vasarhelyi A, Lubitz J, Gierer P, et al. Detection of fibular torsional deformities after surgery for ankle fractures with a novel CT method. Foot Ankle Int. 2006;27:1115–21.
Verim O, Er MS, Altinel L, et al. Biomechanical evaluation of syndesmotic screw position: a finite-element analysis. J Orthop Trauma. 2014;28:210–5.
Vincelette P, Laurin CA, Lévesque HP. The footballer’s ankle and foot. Can Med Assoc J. 1972;107:872–7.
Weber BG. Verletzungen des oberen Sprunggelenkes. In: Aktuelle Probleme in der Chirurgie. Bern: Huber; 1966.
Weber M. Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int. 2004;25:716–27.
Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19:102–8.
Wikerøy AK, Høiness PR, Andreassen GS, et al. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. 2010;24:17–23.
Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35:1197–207.
Wilson FC Jr, Skilbred LA. Long-term results in the treatment of displaced bimalleolar fractures. J Bone Joint Surg Am. 1966;48:1065–78.
Wolf BR, Amendola A. Syndesmosis injuries in the athlete: when and how to operate. Curr Opin Orthop. 2002;31:151–4.
Xenos JS, Hopkinson WJ, Mulligan ME, et al. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77:847–56.
Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15:330–9.
Zindrick MR, Hopkins DE, Knight GW, et al. The effect of lateral talar shift upon the biomechanics of the ankle joint. Orthop Trans. 1985;9:332–3.
Zwipp H. Chirurgie des Fußes. New York: Springer-Verlag; 1994.
Zwipp H, Rammelt S, Grass R. Ligamentous injuries about the ankle and subtalar joints. Clin Podiatr Med Surg. 2002;19:195–229.
Conflict of interest
Stefan Rammelt and Petr Obruba declare that they have no conflict of interest.
Compliance with ethical requirements
Stefan Rammelt and Petr Obruba declare that this is a review article that includes no studies on humans or animals. Therefore, an approval by an ethics committee was not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rammelt, S., Obruba, P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg 41, 601–614 (2015). https://doi.org/10.1007/s00068-014-0466-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-014-0466-8