Abstract
Ten percent of all ankle fractures sustain an associated syndesmotic injury. Syndesmosis injuries have been reported in conjunction with ankle sprains to ankle fractures, with an incidence between 1% and 18%. Isolated ligamentous syndesmosis sprains are rare and consequently are often undiagnosed, progressing to chronic ankle symptoms such as pain and disability, until arthritic joint changes indicate the original pathology. Syndesmotic injuries, even isolated, are not always easy to diagnose because they range from a simple sprain to frank diastasis. Among the most important predictors of functional results, on treatment of syndesmotic injuries, is the accurate restoration of the syndesmotic space. The suspension technique can achieve flexible fixation of the syndesmosis and permit full range of motion of the tibiofibular joint, thanks to starting rehabilitation exercise at an early stage after surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Ten percent of all ankle fractures sustain an associated syndesmotic injury. Syndesmosis injuries have been reported in conjunction with ankle sprains to ankle fractures, with an incidence between 1% and 18%. Isolated ligamentous syndesmosis sprains are rare and consequently are often undiagnosed, progressing to chronic ankle symptoms such as pain and disability, until arthritic joint changes indicate the original pathology. Syndesmotic injuries, even isolated, are not always easy to diagnose because they range from a simple sprain to frank diastasis. Among the most important predictors of functional results, on treatment of syndesmotic injuries, is the accurate restoration of the syndesmotic space. The suspension technique can achieve flexible fixation of the syndesmosis and permit full range of motion of the tibiofibular joint, thanks to starting rehabilitation exercise at an early stage after surgery.
1 Anatomy and Biomechanical Background
The distal tibiofibular syndesmosis is a joint with a low degree of mobility between tibia and fibula. The fibula lies on the “incisura fibularis” of the tibia. In 75% of the cases a true articulation is present, with articular cartilage on the two contact facets, forming a synovial joint with a fat-containing synovial fold interposed between the synovial lining and the fibula: this synovial fold contains loose connective tissue with an abundance of blood vessels and occasionally some small nerves [1]. The syndesmotic ligament complex consists of the following. (a) The anterior inferior tibiofibular (AITF) ligament has a triangular aspect with multiple tight fibers interspersed with some fat. The fibers start at the broad-based anterior tibial tubercle (Chaput) and converge toward the fibular tubercle (Wagstaffe–Le Fort) [2]. (b) The posterior inferior tibiofibular (PITF) ligament is a strong ligament that extends from the posterior tibial malleolus to the posterior tubercle of the fibula and runs from proximal-medial to distal-lateral, forming a 20–40° angle with the horizontal plane [2]. It is a thick and strong ligament: very high rotational stress force more often results in a fracture of the posterior tibial malleolus than in a rupture of the ligament. (c) The interosseous ligament (IL) is a thick and round ligament that runs horizontally between the proximal margin of the fibular malleolar fossa and the dorsodistal rim of the tibia. It can be considered a distal continuation of the interosseous membrane at the level of the tibiofibular syndesmosis [3]. The interosseous membrane is not a true ligament, but it is essential in maintaining connection between tibia and fibula and acts as a reinforcement structure.
Another indirect stabilizer is the deltoid ligament, which acts on the medial side to hold the syndesmosis stabilizing the talus to the tibial malleolus. The AITFL limits the fibular external rotation, the PITFL limits the posterior translation, whereas the IOL prevents the lateral translation of the fibula [4, 5]. On the other side of the joint, the deltoid has a critical function in limiting talar abduction, pronation, and external rotation [5]. The resistance to diastasis comes from the PITFL and IT for 40–45%, the AITFL for 35%, and the interosseous membrane for 20–25% of cases [6].
The most widely accepted mechanism resulting in injury of the syndesmotic ligaments is external rotation and hyperdorsiflexion. Distal tibiofibular syndesmosis is essential for the stability of the ankle mortise. In normal situations, the ankle mortise widens only 1 mm during gait [7]. During the stance phase of the gait cycle, weight-bearing determines a lateral thrust of the talus against the fibular malleolus. When syndesmotic and deltoid ligaments are disrupted, the talus is functionally disconnected from the leg, and the patient complains of instability during weight-bearing. The incidence of ankle syndesmosis injuries is higher in athletes [8, 9] because of their movements: planting the foot and then performing cutting motions, as well as the possibility of direct associated blows to the lateral ankle [10], can progress to a sprain. The reported percentage of syndesmotic injuries is variable because of difficulties of a correct diagnosis, but it varies from 1% to 18% of all ankle sprains [7, 11], excluding the cases of ankle fractures.
2 Classification
A classification of syndesmosis injuries has been proposed by Porter [10] as follows:
-
Grade 1. Injury to the anterior deltoid ligament, to the AITF ligament, and sometimes to the interosseous ligament, but without tearing of the interosseous membrane or the deep deltoid ligament. This kind of lesion is by definition stable because there is no widening of the syndesmosis.
-
Grade 2. The anterior and deep deltoid ligament is involved so far as the syndesmosis in the AITF and interosseous ligament. Distal tibiofibular syndesmosis is unstable but the ankle is normally aligned on nonstress radiographs. This kind of occult instability is often difficult to recognize.
-
Grade 3. The injury involves the entire deltoid ligament and syndesmosis is widely disrupted: the fibula is often fractured above the syndesmosis, sometimes at its proximal part (Maisonneuve lesion). A more recent classification has been proposed distinguishing acute isolated syndesmotic injury as stable or unstable [12].
3 Diagnosis
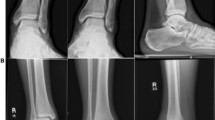
Diagnosis is achieved at the clinical examination for patients sustaining an instable syndesmotic injury who complain of persistent ankle pain, sensations of giving way, proximal palpation pain superiorly to the mortise, and difficulty when walking on uneven ground [13, 14]. As concerns the diagnosis of syndesmotic lesions, many clinical tests have being described: the Cotton test and the fibula translation test are the most reliable for diagnosis [12, 15], by comparing to the opposite side. Many imaging signs are described in the literature for the diagnosis of ankle syndesmosis disruption: the tibiofibular clear space and the tibiofibular overlap sign are the most often described, paying attention to false images caused by the joint rotation [16]. The medial clear space, between the lateral border of the medial malleolus and the medial border of the talus, is a valid radiographic sign. In the mortise view this measure should be equal to or less than the superior clear space between the talar dome and the tibial plafond [17].
Weight-bearing radiographs are very useful in disclosing occult lesions. Magnetic resonance imaging (MRI) can be very useful in visualizing disruption of syndesmotic ligaments [18], and computed tomography (CT) can identify displacement of the distal tibiofibular syndesmosis using the tibiofibular line [19].
4 Treatment
Treatment of syndesmotic lesions depends on the degree of the lesion [20]. Stable lesions (grade 1) must not be treated surgically [10, 12]. The RICE protocol is recommended in the first 7–10 days, with complete weight-bearing with crutches in the first 1–2 weeks. The rehabilitation program permits an average time to return to the sport in 4–8 weeks. Unstable lesions (grade 2–3) are treated surgically, but the choice of the type of surgery depends on the type of instability, whether acute, subacute, or chronic. In acute cases, the treatment is preferably performed with trans-syndesmotic screw fixation. In the subacute setting (6 weeks to 6 months), the focus is to restore the normal anatomy by repairing the elongated ligaments and by placing a positioning screw [14]. If the remnants of the AITF are inadequate, a free tendon graft (plantaris tendon, peroneus longus tendon, or fascia lata) can be used to replace it. For chronic lesions [15, 19], those more than 6 months old, the treatment should be fusion of the distal tibiofibular syndesmosis. In subacute lesions, this type of reconstruction must be associated with an arthroscopic debridement of the syndesmosis and always with a syndesmotic screw fixation. In the past decade, suture-button devices have been used instead of screws, alone in acute cases or associated with other techniques (graft, anatomic reconstruction of AITF ligament) in subacute or chronic settings. In a recent systematic review [21] of suture-button versus syndesmotic screw techniques, the suture-button fixation group showed similar American Orthopaedic Foot & Ankle Society (AOFAS) outcome scores (91.06 points) compared to the conventional screw fixation (87.78 points) group, and the rate of implant removal and poor reduction was lower in the suture-button fixation group.
Arthroscopic debridement of syndesmosis and arthroscopically assisted insertion of the suture-button device is today’s technique. The patient is assessed in a supine position, with the leg in a noninvasive traction device. In addition to the two usual portals, an ancillary anterosuperior portal is used for a more accurate removal of the scar tissue inside the syndesmotic space (Fig. 20.1). After the complete cleanup of the scar tissue and an evaluation of the lesion including the medial compartment (Fig. 20.2), the pathological mobility of the joint is assessed (see Videos 20.1 and 20.2). The K-wire of the suture-button device is then passed along both the fibular and tibial shaft, choosing the exact level at which to insert by fluoroscopy. The wire is pulled ahead until its tip emerges from the cortical bone inside the syndesmosis, under direct scope visualization. The wire is then completely drilled out the contralateral side of the leg, until the button engages the cortical bone. When both buttons are regularly placed on the two sides of the syndesmosis, on the lateral cortical side of the fibula and on the medial side of the tibia, it is possible to reduce the syndesmotic lesion under direct scope visualization (Fig. 20.3) by simply tightening the sutures.
Traps | Tricks |
|---|---|
Uncertain decision about treatment | Make an accurate classification of the lesion |
Low visualization with scope | Clean up the scar tissue in the syndesmosis with shaver and radiofrequency wand |
Difficult to move instruments and visualize syndesmosis together | Provide opening an anterosuperior accessory portal for shaver using anterior for scope |
Doubts about the placement of the K-wire guide for suture button | Use both scope and fluoroscopy at the same time |
References
Bartonicek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25:379–86.
Hermans J, Beumer A, de Jong TAW, Kleinrensink J. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. Anatomy. 2010;217:633–45.
Golanó P, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557.
Brown KW, et al. MRI findings associated with distal tibiofibular syndesmosis injury. Am J Roentgenol. 2004;182(1):131–6.
Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am. 1956;38(4):761–81.
Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10(5):558–60.
Lin CF, Gross MT, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36:272–384.
Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17:282–5.
Van den Bekerom MPJ, Lamme B, Hogervorst M, Bolhuis HW. Which ankle fractures require syndesmotic stabilization? J Foot Ankle Surg. 2007;46:456–63.
Porter DA. Evaluation and treatment of ankle syndesmosis injury. Instruction course lectures. Foot and ankle. Rosemont, IL: AAOS; 2010. p. 159–65.
Clanton T, Paulos P. Syndesmosis injuries in athletes. Foot Ankle Clin N Am. 2002;7:529–54.
van Dijk CN, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthr. 2016;24:1200–16.
Beumer A, van Hemert WL, Niesing R, et al. Kinematics before and after reconstruction of anterior syndesmosis of the ankle: a prospective radiostereometric and clinical study in 5 patients. Acta Orthop. 2005;76(5):713–20.
Van Dijk CN. Syndesmotic injuries. Tech Foot Ankle Surg. 2006;5(1):34–7.
Van Dijk CN. Acute syndesmosis injury. In: Chan KM, Karlsson J, editors. ISAKOS-FIMS world consensus conference on ankle instability. Rome: International Federation of Sports Medicine; 2005.
Garner MJ, Demetrakopoulos D, Briggs SM, Lorich DG. Malreduction of tibifibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788–92.
Beumer A, van Hemert WL, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227–34.
Oae K, Takao M, Naito K, et al. Injury of tibiofibular syndesmosis: value of MRI imaging for the diagnosis. Radiology. 2003;227(1):155–61.
Gifford PB, Lutz ML. The tibiofibular line: an anatomical feature to diagnose syndesmosis malposition. Foot Ankle Int. 2014;35(11):1181–6.
Van den Bekerom MPJ, de Leuw PAJ, van Dijk CN. Delayed operative treatment of syndesmotic instability: current concept review. Injury. 2009;40:1137–42.
Zhang P, et al. A systematic review of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury. BMC Musculoskel Disord. 2017;18:286.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Syndesmosis (MP4 148,961 kb)
Syndesmotic joint instability arthroscopic repair (MP4 354,644 kb)
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Allegra, F., Lijoi, F. (2020). Syndesmotic Joint Instability Arthroscopic Repair. In: Allegra, F., Cortese, F., Lijoi, F. (eds) Ankle Joint Arthroscopy. Springer, Cham. https://doi.org/10.1007/978-3-030-29231-7_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-29231-7_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29230-0
Online ISBN: 978-3-030-29231-7
eBook Packages: MedicineMedicine (R0)