Abstract
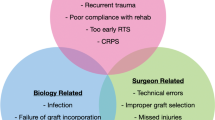
Knee instability following anterior cruciate ligament reconstruction often represents a problematic outcome. When compared to traumatic re-tears, a symptomatic unstable knee with a structurally intact graft is a less common, yet potentially more puzzling cause of ACL reconstruction failure. A number of scenarios can result in such a presentation, including (a) graft laxity in the setting of properly positioned tunnels; (b) non-anatomic tunnel placement resulting in improper graft position/orientation; and (c) additional factors contributing to instability, such as lower extremity malalignment, high tibial slope, meniscal deficiency, and damage to other ligamentous structures. In this chapter, we review the causes, diagnosis, and surgical management of these issues.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diagnosis of Structurally Intact but Abnormally Lax ACL Graft
Firstly, it’s important to differentiate between laxity on exam and true symptomatic instability. Inadequate rehabilitation and lack of lower extremity neuromuscular control can result in symptoms of instability, even without any objective evidence of laxity after ACL reconstruction [1]. In contrast, some asymptomatic and fully functional patients may demonstrate positive exam findings of laxity on such tests as the Lachman, anterior drawer, pivot shift tests, and arthrometer measurements.
For patients who have exhausted rehabilitative measures and continue to exhibit symptomatic instability, a follow-up MRI must be obtained to assess integrity of the ACL graft and evaluate for other pathologies. In the setting of an intact graft, the following most common scenarios that can lead to residual instability must be considered:
-
1.
Proper graft position, but insufficient graft tension
-
2.
Improper graft position/orientation
-
3.
Unrecognized or unaddressed additional injuries/conditions
Below, we discuss a step-by-step approach to recognizing and surgically addressing each of the above factors.
Scenario 1: Properly Positioned Graft with Insufficient Tension
One potential cause of an unstable knee with a structurally intact ACL graft is laxity of the graft itself. Detailed physical examination and dedicated imaging are important to rule out additional contributing factors (discussed below), such as erroneous tunnel placement, other ligamentous injuries, and malalignment. Arthroscopic evaluation of the graft will reveal an intact graft in correct position/orientation, with abnormal laxity to probing (case 1, Fig. 6.2). In this case, the graft may be lax for the following reasons: (a) inadequate initial tension, (b) failure of rigid fixation, and (c) graft stretching over time.
Inappropriate Intraoperative Tension
Inadequate initial intraoperative tension on an ACL graft may result from: (a) failure to pre-tension the graft prior to implantation, (b) failure to place the knee into correct position during graft fixation, and (c) failure to apply adequate tension during graft fixation.
Pre-tensioning the graft is important in order to remove the creep (i.e., plastic deformation) prior to implantation. Biomechanical studies show that higher loads and longer application times leave the graft with higher residual tension and lower potential for stretching [2, 3]. In the clinical setting, application of 80–90 N load to the graft for a minimum of 15 minutes is recommended. Surgical tip: be sure to re-check and adjust the tension on the graft a few minutes after the initial load is applied – as plastic deformation occurs, the graft stretches slightly, and the tension experienced decreases.
For a single-bundle ACL reconstruction, the graft should be fixed with the knee in full extension, while a reverse Lachman force is applied [4]. Failure to apply this force may result in graft fixation with the tibia in the excessively anterior position (case 1, Fig. 6.1b).
Applying adequate force to the ACL graft during fixation represents a balance between preventing laxity and avoiding over-tightening, with a minimum of 20 N of force recommended [5]. It is essential to verify appropriate graft tension at the conclusion of the case by checking knee stability manually via Lachman, anterior drawer, and pivot shift tests and by probing the graft under direct arthroscopic visualization.
Loss of Rigid Graft Fixation (i.e. Graft Slippage)
A wide variety of options for securing the ACL graft exist, broadly divided into the main types of aperture fixation and suspensory fixation. Aperture fixation at the intra-articular opening of the tunnel results in the shortest possible distance of the unfixed graft. Suspensory fixation leaves more of the graft unsecured, allowing a “windshield-wiper effect” and possible tunnel widening, which can theoretically allow the graft to shift into a suboptimal position, potentially producing graft laxity [6, 7]. Additionally, laxity can result when fixation mode itself fails, such as button pull through, adjustable loop lengthening, suture failure, and graft slippage past the interference screw [8, 9].
Graft Stretch
Due to intrinsic properties, some grafts are predisposed to greater likelihood of stretching over time. Studies have shown higher risk of re-rupture with allografts than with autografts [9,10,11]; additionally, hamstring grafts are more likely to experience stretch than bone-patellar tendon-bone (BPTB) grafts are [8, 9]. Although differences in overall clinical outcomes are debatable, a number of studies have demonstrated greater anterior knee laxity with hamstring grafts, compared to that of BPTB grafts [12,13,14]. Chapter 5 focuses specifically on graft options for ACL revision reconstruction.
Surgical Approach to a Properly Positioned Graft with Insufficient Tension
For a symptomatic patient with an ACL graft that is properly positioned but lax on clinical and arthroscopic examination, revision ACL reconstruction is required, as there is currently no clinically proven way to “tighten” such a graft in situ. In this situation, the surgeon must consider and address all possible contributing issues, discussed above, as follows (Table 6.1).
-
1.
If possible, choose a stiffer graft, with lower intrinsic likelihood of stretching. If an allograft was used at index surgery, an autograft should be considered for revision. With a previously used hamstring, consider BPTB or quadriceps tendon (QT).
-
2.
Ensure appropriate graft tension during preparation and implantation. Maintain the graft under at least 80–90N of tension for at least 15 minutes prior to implantation, re-checking the tension every 4–5 minutes. While the graft is being secured, ensure full knee extension and a reverse Lachman force. Consider using a tensiometer to ensure adequate force application at the time of graft fixation, and verify elimination of the Lachman, anterior drawer, and pivot shift tests afterwards.
-
3.
For securing the graft, choose implants that will ensure optimal tension and rigid fixation and have the least likelihood of any postoperative slippage. Aperture fixation produces the shortest and stiffest grafts, while many currently used suspensory devices allow adding graft tension even after fixation is set. In a revision setting, consider employing two modes of fixation on either the femoral or tibial side or even on both sides. For example, you can secure the graft with a button-loop device on the femur and interference screw on the tibia, add tension as needed from the femoral side, finalize femoral fixation by adding an interference screw, and back up tibial fixation by securing the graft sutures distally (to a post or an anchor).
Scenario 2: Improperly Positioned Graft
If the graft has been malpositioned, residual knee laxity and instability may occur, even with a graft that’s properly tensioned, well fixed, and intrinsically stiff. Proper graft function depends on anatomic tunnel position [15,16,17], and thus, erroneous tunnel placement, which is the most common technical error during ACL reconstruction [18], can result in a graft that is structurally intact but functionally insufficient (i.e., lax).
Femoral Tunnel Too Anterior
A femoral tunnel placed too anteriorly has been found to be an important factor leading to graft failure, occurring in ~30% of revision ACL reconstructions [18]. A too anterior tunnel produces a graft that becomes excessively tight in flexion and loose in extension [19].
Tibial Tunnel Too Posterior
The most common mistake of tibial tunnel placement is a too posterior location, which has been shown to result in higher rates of rotational instability and worse subjective outcomes [20]. In contrast, a too-anteriorly placed tibial tunnel may cause graft impingement on the roof of the intercondylar notch in extension and may lead to loss of terminal extension [17].
Vertical Graft
The classically described vertical graft can be stable in the anterior to posterior plane, but has a rotationally unstable component, as seen with a positive pivot shift phenomenon (case 2, Fig. 6.3). Vertical grafts can result from the femoral tunnel placed too anteriorly, the tibial tunnel placed too posteriorly, or a combination of the two [16, 18].
Surgical Approach to an ACL Graft with Non-anatomic Tunnel Placement
Preoperative confirmation of suspected graft/tunnel malposition as cause for residual laxity should be done with imaging, including plain radiographs (which can show too-anterior femoral and/or too-posterior tibial tunnels), MRI (which can show an intact but vertically oriented graft), and CT scan with 3D reconstructions (which can identify locations and orientation of the tunnels, measure tunnel widening, and assess availability of bone stock for revision reconstruction).
Option 1: Graft Revision
If the structurally intact yet lax ACL graft is believed to be due to tunnel malposition, the most obvious solution is a revision ACL reconstruction with proper tunnel placement. For tunnels that are grossly malpositioned but not significantly widened, there may be enough “real estate” to place entirely new tunnels or sockets in proper anatomic locations. In other cases, convergence between new and old tunnels may be unavoidable – techniques to address this problem are discussed in detail in subsequent chapters.
Option 2: Graft Augmentation
Some vertically oriented grafts provide adequate anterior-posterior stability, but lack rotational stability, resulting in patient complaints of the knee giving out – particularly with pivoting and cutting movements. A careful examination demonstrates negative or grade 1A Lachman and anterior drawer tests, with a positive pivot shift. Imaging and arthroscopic exam confirm a graft that is well-positioned in the sagittal plane, but is too vertical in the coronal plane, thereby adequately replicating the anteromedial (AM) bundle of the ACL, but not the posterolateral (PL) bundle. In this scenario, especially if the graft appears well-vascularized and incorporated, it is reasonable to consider augmentation with a small-size graft to replicate the PL bundle, serving to add rotational stability to an already anteriorly stable knee [21].
To add a PL bundle to an existing vertical graft, a similar technique as used to perform selective bundle reconstruction for partial ACL tears with an intact AM bundle should be used. A 5–7-mm diameter graft is sufficient, as larger grafts may cause impingement; a doubled semitendinosus graft readily serves this purpose.
To ensure adequate rotational stability is restored, it is essential to respect anatomic footprints of the PL bundle on the femur and tibia. On the femoral side, the PL bundle inserts distal to the AM bundle, typically just inferior to the bifurcate ridge [22]. Outside-in or AM portal drilling can both be used to place a femoral socket in this location, avoiding convergence with the existing femoral tunnel; fluoroscopy can be used intraoperatively to verify guide-wire position prior to reaming.
On the tibial side, the insertion of the PL bundle is located about 10 mm posterolateral to the center of the AM bundle [22], just medial to the lateral tibial spine. Compared to the typical angle of the tibial tunnel seen in cases with vertical grafts (which is usually about 20–30 degrees in the coronal plate), the angle of the guide-wire when adding the PL bundle reconstruction should be about 20–30 degrees more oblique (i.e., about 40–60 degrees in the coronal plane). The graft should be secured with the knee in 60–70 degrees of flexion and slight external rotation, with a posterior drawer force applied.
An additional consideration for intact grafts with lack of rotational stability (with adequate anterior stability) is the integrity of the anterolateral ligament (ALL) [23]. For patients with this complaint, if the graft appears to be appropriately oriented, secured, and taught to arthroscopic palpation, consideration can be given to adding ALL reconstruction, which will be discussed separately in Chap. 18.
Scenario 3: Unrecognized or Unaddressed Additional Injuries/Conditions
ACL tears occur frequently in conjunction with other pathologies, including meniscal tears, injuries to other ligaments, lower extremity coronal malalignment, and/or abnormal tibial slope. Failure to recognize and address these issues can result in excessive stress on the ACL graft, leading to graft stretching and laxity, clinical instability, and even graft failure. When encountering a knee with an intact ACL graft and persistent laxity, it is important for the surgeon to perform a thorough workup to identify the aforementioned potential contributing factors and plan accordingly when considering surgical intervention.
Coronal Plane Malalignment
Significant deviations from a normal mechanical axis impart abnormal forces to the knee joint and can contribute to failure of an ACL reconstruction. Varus malalignment, in particular, has been noted in greater proportion of ACL revision cases compared to successful index reconstructions [24,25,26] and is typically managed with a valgus-producing high tibial osteotomy (HTO), which can be done with a medial opening or lateral closing wedge technique [27, 28]. By correcting alignment, HTO can help normalize knee kinematics, allowing the ACL to function appropriately without excessive stress [29]. Both single-stage and two-stage approaches have been proposed for treating a knee with a failed ACL reconstruction and deformity. In the setting of an intact graft with clinical instability, we feel it best to choose a two-stage approach, as correction of varus deformity (especially if combined with tibial slope decrease) may provide enough stability improvement to obviate the need for graft revision. Details of managing coronal plane deformity are discussed in Chap. 15.
Sagittal Plane Malalignment
Excessively high posterior tibial slope (PTS) increases anterior translation of the tibia in weight-bearing and has been established as an independent predictor of ACL reconstruction failure [30, 31]. It’s been reported that a PTS of greater than 12 degrees significantly increases the risk of ACL graft failure [32, 33], whereas biomechanical studies have confirmed that slope-reducing osteotomies decrease ACL graft forces and anterior tibial translation under axial load [34]. A number of clinical studies have shown successful outcomes with ACL revision reconstruction combined with tibial osteotomies that corrected excessive PTS [35, 36]. Sagittal plane deformity is further discussed in Chap. 16.
Additional Ligamentous Injury and Meniscal Deficiency
The most common additional ligamentous insufficiency that contributes to failure of ACL reconstruction is that of the posterolateral corner (PLC) [37]. Careful clinical examination is paramount in identifying this when preparing for ACL revision, as PLC structures may appear intact on imaging, but nevertheless exhibit laxity, especially when the original trauma is chronologically remote. Both isolated PLC reconstruction and those combined with ACL graft revision may be used to address persistent instability in cases of an intact ACL graft with residual instability. Management of the posterolateral corner as part of ACL revision reconstruction is discussed in detail in Chap. 14.
Finally, meniscal deficiency and certain meniscocapsular lesions have been shown to contribute to increased laxity both in ACL-deficient and ACL-reconstructed knees, leading to increased anterior translation and rotation [38,39,40,41]. Management of these lesions is discussed in Chaps. 19 and 20.
Summary
Not uncommonly, a patient may present with a clinically failed (i.e., unstable) ACL reconstruction, despite imaging findings of an intact graft. It is the surgeon’s job to perform a meticulous evaluation, using detailed history, thorough physical examination, advanced imaging, and sometimes examination under anesthesia, including arthroscopy, to determine the cause for this instability. Dividing the potential causes into three main groups, as described in this chapter, can be helpful to determine the best surgical approach. Grafts that are well positioned may be lax due to failure of fixation, insufficient initial tension, or graft stretching; this scenario requires a revision with a stiffer graft, more rigid fixation, and appropriate intraoperative graft tensioning. Malpositioned grafts usually need to be revised with creation of tunnels in anatomic locations, although in some cases, an isolated posterolateral bundle reconstruction can add rotational stability to an existing graft that demonstrates adequate anterior stability. Finally, other issues that contribute to knee laxity must be sought out and addressed, including varus malalignment, high posterior tibial slope, additional ligamentous injuries, and meniscal deficiency.
Additionally, a surgeon must remember that, from a psychological standpoint, when imaging shows an intact graft, it can be difficult to convince a patient that revision surgery is necessary and that they will need to go through an extensive period of convalescence and rehabilitation all over again. It is, therefore, crucial to engage the patient as an active participant in decision-making, to recognize and acknowledge their goals and expectations, to explain in detail the issues that are contributing to their instability, and to ensure appropriate rehabilitation prior to any repeat surgical intervention.
Case 1
Patient is an 18-year-old collegiate volleyball player who presented 1 year after BTB autograft ACL reconstruction with a medial meniscus repair, complaining of knee pain, mechanical symptoms, and intermittent buckling. She completed a full course of rehabilitation, including a return-to-play protocol with her athletic trainer, and resumed training, but was unable to wean from the brace for athletic participation and did not feel ready to return to competition. Clinical examination demonstrated a normal gait, neutral lower extremity alignment, full range of motion with pain and clicking, tenderness over the medial joint line, and normal strength. Stability examination showed 1B Lachman and anterior drawer tests, while a pivot shift could not be properly assessed due to guarding. The PCL, collateral ligaments, and corners were stable. Imaging showed neutral alignment, good tunnel positions on X-rays (Fig. 6.1), and intact graft in a proper orientation, but with significant anterior tibial translation on MRI (Fig. 6.1b), indicating laxity. Considering these findings, ACL laxity and symptoms of instability were thought to be due to either insufficient initial graft tension (at the time of index surgery) or subsequent graft stretching.
Due to failure of conservative management and significant limitations on her athletic participation, patient was indicated for and elected to proceed with a revision ACL reconstruction. Exam under anesthesia confirmed isolated ACL laxity, with positive Lachman, anterior drawer, and pivot shift tests. Arthroscopy examination showed an intact graft that exhibited significant laxity to probing and anterior tibial translation (Fig. 6.2). Graft orientation and tunnel positions were confirmed to be acceptable. Revision to a quadrupled hamstring autograft was then performed. After the semitendinosus and gracilis tendons were harvested and whipstitched, they were pretensioned at 80–90N for 20–30 minutes. For graft placement, we were able to utilize the same tunnel positions, as the tunnels were well healed from previous BTB graft plugs (Fig. 6.2). The graft was secured to the femur with an adjustable button-loop device. The knee was cycled 20 times and placed into full extension, reverse Lachman force was applied to ensure reduction of the tibia posteriorly, and, while applying maximal manual force to the graft, an interference screw was placed into the tibial tunnel. The knee was cycled again, and the graft was re-tensioned from the femoral side. Excellent graft tension was observed on direct probing (Fig. 6.2) and on stability testing. To decrease the risk slippage, we also secured the distal graft sutures over a post and tied the tensioning sutures on the femoral side.
Patient recovered well, returning to full competition 1 year postoperatively. Her last clinical examination showed no more than 1A Lachman and anterior drawer and a negative pivot shift. She did not complain of any instability sensation or buckling.
Case 2
Patient is a 55-year-old active male who initially injured his knee playing softball and underwent an ACL reconstruction with allograft at an outside institution. He began having recurrent symptoms of instability shortly after weaning from the postoperative brace, and despite extensive rehabilitation, this did not improve. On exam, his gait was normal, and range of motion and strength were full; however, stability examination demonstrated a 2A Lachman, 1A anterior drawer, and a positive pivot shift with a glide. Imaging with plain radiographs (Fig. 6.3) and an MRI (Fig. 6.3b) demonstrated an intact graft in a vertical orientation, largely due to an excessively posterior tibial tunnel position. Due to the patient’s persistent symptoms, evidence of instability on exam, and imaging findings of a vertically oriented graft, a decision was made to proceed with revision surgery. Given the patient’s age and activity level, an allograft was selected. Intraoperatively, the previous graft was resected, and completely separate tunnels were drilled (Fig. 6.4), allowing appropriate orientation of the new graft. Secure fixation was obtained on the femoral side with an adjustable button-loop construct, and on the tibial side with an interference screw in the tunnel, backed up by a staple over the distal tail of the graft. At his 1-year follow-up, the patient reported no instability and had a negative Lachman, anterior drawer, and pivot shift tests on exam, and imaging showed appropriate graft orientation and tunnel position (Fig. 6.5).
References
Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87(6):737–50.
Pilia M, Murray M, Guda T, Heckman M, Appleford M. Pretensioning of soft tissue grafts in anterior cruciate ligament reconstruction. Orthopedics. 2015;38(7):e582–7.
Lockwood WC, Marchetti DC, Dahl KD, Mikula JD, Williams BT, Kheir MM, Turnbull TL, LaPrade RF. High-load preconditioning of human soft tissue hamstring grafts: an in vitro biomechanical analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):138–43.
Gertel TH, Lew WD, Lewis JL, Stewart NJ, Hunter RE. Effect of anterior cruciate ligament graft tensioning direction, magnitude, and flexion angle on knee biomechanics. Am J Sports Med. 1993;21(4):572–81.
Van Kampen A. The effect of different graft tensioning in anterior cruciate ligament reconstruction: a prospective randomized study. Arthroscopy. 1998;14(8):845–50.
Brown CH Jr, Wilson DR, Hecker AT, Ferragamo M. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy. 2004;20(9):922–35.
Kamelger FS, Onder U, Schmoelz W, Tecklenburg K, Arora R, Fink C. Suspensory fixation of grafts in anterior cruciate ligament reconstruction: a biomechanical comparison of 3 implants. Arthroscopy. 2009;25(7):767–76.
Steiner ME, Hecker AT, Brown CH Jr, Hayes WC. Anterior cruciate ligament graft fixation: comparison of hamstring and patellar tendon grafts. Am J Sports Med. 1994;22(2):240–7.
Maletis GB, Inacio MC, Desmond JL, Funahashi TT. Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Joint J. 2013;95(5):623–8.
Mars Group. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med. 2014;42(10):2301–10.
Magnussen RA, Taylor DC, Toth AP, Garrett WE. ACL graft failure location differs between allografts and autografts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):1–6.
Cristiani R, Sarakatsianos V, Engström B, Samuelsson K, Forssblad M, Stålman A. Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):381–8.
Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, Renström P. Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts: a prospective, randomized study. JBJS. 2002;84(9):1503–13.
Freedman KB, D'Amato MJ, Nedeff DD, Kaz A, Bach BR. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11.
Burnham JM, Malempati CS, Carpiaux A, Ireland ML, Johnson DL. Anatomic femoral and tibial tunnel placement during anterior cruciate ligament reconstruction: anteromedial portal all-inside and outside-in techniques. Arthrosc Tech. 2017;6(2):e275–82.
Rupp S, Müller B, Seil R. Knee laxity after ACL reconstruction with a BPTB graft. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):72–6.
Chhabra A, Diduch DR, Blessey PB, Miller MD. Recreating an acceptable angle of the tibial tunnel in the coronal plane in anterior cruciate ligament reconstruction using external landmarks. Arthroscopy. 2004;20(3):328–30.
Morgan JA, Dahm D, Levy B, Stuart MJ, MARS Study Group. Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25(5):361.
Zavras TD, Race A, Bull AM, Amis AA. A comparative study of’isometric’points for anterior cruciate ligament graft attachment. Knee Surg Sports Traumatol Arthrosc. 2001;9(1):28–33.
Inderhaug E, Strand T, Fischer-Bredenbeck C, Solheim E. Effect of a too posterior placement of the tibial tunnel on the outcome 10–12 years after anterior cruciate ligament reconstruction using the 70-degree tibial guide. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1182–9.
Chhabra A, Starman JS, Ferretti M, Vidal AF, Zantop T, Fu FH. Anatomic, radiographic, biomechanical, and kinematic evaluation of the anterior cruciate ligament and its two functional bundles. JBJS. 2006;88(suppl_4):2–10.
Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39(4):743–52.
Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pécora JR, Camanho GL, Demange MK. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3652–9.
Won HH, Chang CB, Je MS, Chang MJ, Kim TK. Coronal limb alignment and indications for high tibial osteotomy in patients undergoing revision ACL reconstruction. Clinical Orthopaedics and Related Research®. 2013;471(11):3504–11.
Jan van de Pol G, Arnold MP, Verdonschot N, van Kampen A. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37(3):481–7.
Hinckel BB, Demange MK, Gobbi RG, Ricardo J, Camanho GL. The effect of mechanical varus on anterior cruciate ligament and lateral collateral ligament stress: finite element analyses. Orthopedics. 2016;39(4):e729–36.
Zaffagnini S, Bonanzinga T, Grassi A, Muccioli GM, Musiani C, Raggi F, Iacono F, Vaccari V, Marcacci M. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):934–41.
Klek M, Dhawan A. The role of high Tibial osteotomy in ACL reconstruction in knees with coronal and sagittal plane deformity. Curr Rev Musculoskelet Med. 2019;12(4):466–71.
Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees: a two-to seven-year follow-up study. Am J Sports Med. 1993;21(1):2–12.
Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW, Brady AW, Nakama GY, LaPrade RF. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296–302.
Arun GR, Kumaraswamy V, Rajan D, Vinodh K, Singh AK, Kumar P, Chandrasekaran K, Santosh S, Kishore C. Long-term follow up of single-stage anterior cruciate ligament reconstruction and high tibial osteotomy and its relation with posterior tibial slope. Arch Orthop Trauma Surg. 2016;136(4):505–11.
Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41(12):2800–4.
Lee CC, Youm YS, Do Cho S, Jung SH, Bae MH, Park SJ, Kim HW. Does posterior tibial slope affect graft rupture following anterior cruciate ligament reconstruction? Arthroscopy. 2018;34(7):2152–5.
Imhoff FB, Mehl J, Comer BJ, Obopilwe E, Cote MP, Feucht MJ, Wylie JD, Imhoff AB, Arciero RA, Beitzel K. Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3381–9.
Schuster P, Geßlein M, Schlumberger M, Mayer P, Richter J. The influence of tibial slope on the graft in combined high tibial osteotomy and anterior cruciate ligament reconstruction. Knee. 2018;25(4):682–91.
Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–52.
Kim SJ, Choi DH, Hwang BY. The influence of posterolateral rotatory instability on ACL reconstruction: comparison between isolated ACL reconstruction and ACL reconstruction combined with posterolateral corner reconstruction. JBJS. 2012;94(3):253–9.
Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–8.
DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, Nakama GY, Engebretsen L, LaPrade RF. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46(10):2422–31.
Cristiani R, Rönnblad E, Engström B, Forssblad M, Stålman A. Medial meniscus resection increases and medial meniscus repair preserves anterior knee laxity: a cohort study of 4497 patients with primary anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(2):357–62.
Grassi A, Macchiarola L, Urrizola Barrientos F, Zicaro JP, Costa Paz M, Adravanti P, Dini F, Zaffagnini S. Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and meniscal deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case-control study. Am J Sports Med. 2019;47(2):285–95.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Golant, A., Geswell, M., Nicholas, S.J. (2022). Management of the Structurally Intact ACL with Residual Instability. In: Alaia, M.J., Jones, K.J. (eds) Revision Anterior Cruciate Ligament Reconstruction. Springer, Cham. https://doi.org/10.1007/978-3-030-96996-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-96996-7_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96995-0
Online ISBN: 978-3-030-96996-7
eBook Packages: MedicineMedicine (R0)