Abstract
Background
Failed ACL reconstruction frequently is accompanied by irreparable medial meniscal tear and/or visible osteoarthritis (OA) in the medial tibiofemoral joint. Thus, assessment for the presence of varus malalignment is important in caring for patients in whom revision ACL reconstruction is considered.
Questions/purposes
We determined whether patients undergoing revision ACL reconstruction (1) have more frequent varus malalignment coupled with more severe degrees of medial meniscal injury and/or medial tibiofemoral OA, and (2) would meet potential indications for high tibial osteotomy more frequently than patients undergoing primary ACL reconstruction.
Methods
We compared 58 patients undergoing revision ACL reconstruction and 116 patients undergoing primary ACL reconstruction. The mechanical tibiofemoral angle and the weight loading line (%) of the knee were measured. Additionally, radiographic degrees of OA in the tibiofemoral joints, and meniscal conditions were assessed. Then, proportions of potential candidates for high tibial osteotomy between the two groups were compared based on the following indications: (1) weight loading line less than 5%, (2) weight loading line less than 25% and medial tibiofemoral OA Kellgren-Lawrence Grade 3 or greater, or (3) weight loading line less than 25% and Kellgren-Lawrence Grade 2 medial tibiofemoral OA plus subtotal or total medial meniscectomy status.
Results
The revision ACL reconstruction group had more frequent varus malalignment in terms of proportion of knees with more varus mechanical tibiofemoral angle than varus 5° (19% versus 8%, p = 0.029) and knees with weight loading line less than 25% (22% versus 9%, p = 0.011). This group also had more frequent high-grade injury of the medial meniscus (34% versus 16%, p = 0.007) and tended to have more frequent higher-grade radiographic OA at the medial tibiofemoral joint (19% versus 9%, p = 0.076). The percentage of patients meeting potential indications for high tibial osteotomy was greater in this group (14% versus 2%, p = 0.003).
Conclusions
We found that many patients undergoing revision ACL surgery may be reasonable candidates for concurrent high tibial osteotomy to address concomitant alignment and OA issues in the medial compartment. However, whether that additional intervention is offset by added risk and morbidity should be the focus of a future study, as it cannot be answered by a study of this design.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Revision ACL reconstruction is challenging, and its outcomes are known to be inferior to those of primary ACL reconstruction [12, 17, 25]. The presence of concomitant knee lesions such as meniscus injuries and osteoarthritis (OA) may be associated with inferior outcomes [1]. Multiple authors have reported that patients undergoing revision ACL reconstruction have concomitant advanced meniscal and/or articular damage, particularly at the medial tibiofemoral joint, such as irreparable tears of the medial meniscus and/or established medial tibiofemoral OA [1, 4, 8, 23]. Additionally, it has been our anecdotal observation that patients undergoing revision ACL reconstruction have varus malalignment more frequently than patients undergoing primary ACL reconstruction. If this is the case, preexisting medial tibiofemoral joint problems in the patients with failed ACL reconstruction can lead to more adverse consequences; varus malalignment is known to be one of the most important factors for progression of preexisting medial tibiofemoral OA and aggravation of symptoms [5, 6, 18–20, 22]. Moreover, in patients with large, irreparable medial meniscal tears, combined varus malalignment can further aggravate mechanical stress on the medial tibiofemoral joint and may result in early degeneration of the joint [3, 7, 13].
Consequently, we speculated that patients undergoing revision ACL reconstruction might be more likely to meet standard criteria for high tibial osteotomy than those undergoing primary ACL reconstruction. However, little information is available regarding the coronal alignment conditions and potential indications for high tibial osteotomy in these patient groups.
We therefore determined whether patients undergoing revision ACL reconstruction (1) have more frequent varus malalignment coupled with more severe degrees of medial meniscal injury and/or medial tibiofemoral OA, and (2) would meet potential indications for high tibial osteotomy more frequently than patients undergoing primary ACL reconstruction. We hypothesized that patients undergoing revision ACL reconstruction would have more frequent varus malalignment coupled with more severe degrees of medial meniscus injury and/or medial tibiofemoral OA, and therefore might become potential candidates for high tibial osteotomy more frequently than patients undergoing primary ACL reconstruction.
Patients and Methods
For this study, we developed two comparative groups: (1) a revision ACL reconstruction group and (2) a primary ACL reconstruction group as a control. For the revision ACL reconstruction group, we included only patients whose major symptom was sustained instability originating from failed previous ACL reconstruction. We did not include patients who had ACL damage or failure of a reconstructed ACL but had undergone high tibial osteotomy alone because their major symptom stemmed not from instability but from medial tibiofemoral OA. For this, we reviewed collected data for 65 knees in 63 patients undergoing revision ACL reconstruction between September 2005 and April 2012. We excluded seven knees (seven patients) with the following conditions: (1) five knees in five patients who underwent combined surgeries with other knee ligament reconstructions and (2) two knees of two patients who underwent rerevision ACL reconstruction owing to acute reinjury. This left 58 knees in 58 patients in the revision ACL reconstruction group. In developing the primary ACL reconstruction group for a control, because age and sex were potential demographic factors influencing variation in the degree of OA and of coronal alignment, we matched these two factors by individual matching methods. For this study, we sought to enroll two controls per case, ie, 116 control subjects. For this, we reviewed a database of 280 patients (247 male and 33 female patients) who underwent primary ACL reconstruction between January 2009 and April 2012 in a retrograde order and selected 116 patients as the age- and sex-matched control group. There were no differences in demographic features between groups (Table 1). All patients involved in this study were ethnically Korean and had undergone surgeries by one surgeon (CBC) at our institute.
To estimate sample size, we used the probability of a patient meeting a standardized set of potential indications for high tibial osteotomy as our target outcome variable. Since 2011, we have performed high tibial osteotomy combined with primary or revision ACL reconstruction for patients who had symptomatic ACL laxity and also met our indications of high tibial osteotomy for patients undergoing ACL reconstruction. The indications for concurrent high tibial osteotomy in patients undergoing ACL reconstruction are determined based on three objective findings (coronal limb alignment, degree of radiographic knee OA, and meniscal condition) and patients’ symptoms and functions, such as presence of varus thrust gait. In this study, we applied only the indications defined based on the aforementioned three objective factors to detect potential candidates for high tibial osteotomy. Those indications were (1) weight loading line less than 5% from the medial edge of the tibial plateau regardless of any other condition; (2) weight loading line less than 25% plus radiographic OA of Kellgren-Lawrence Grade 3 or higher at the medial tibiofemoral joint regardless of meniscal condition; and (3) weight loading line less than 25% plus Kellgren-Lawrence Grade 2 at the medial tibiofemoral joint plus subtotal or total medial meniscectomy status. Furthermore, even if a knee met one of these criteria, if its Kellgren-Lawrence grade was 3 or higher at the lateral compartment and/or subtotal or total lateral meniscectomy had been done, it would not be considered for high tibial osteotomy because of a potential concern of progression of lateral tibiofemoral OA after realignment. Our prior data indicated that the probability of a patient meeting these indications among controls was approximately 1.5%. We expected that the probability of potential indication for high tibial osteotomy in the revision ACL reconstruction group would be approximately 10 times higher than that of the primary ACL reconstruction group, ie, 15%. In that case, we would need to study 53 patients in the revision ACL reconstruction group and 106 patients in the primary ACL reconstruction if we set Type I error at 0.05 and power at 0.8 using either a chi-square test or Fisher’s exact test. This result verified the adequacy of the sample size for this study. This study was approved by the institutional review board of our hospital.
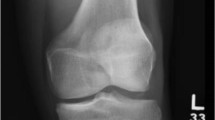
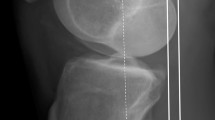
We performed radiographic evaluation to assess parameters for coronal limb alignment including the weight loading line and mechanical tibiofemoral angle, and degrees of OA in the tibiofemoral joint of the knee. For all study subjects, radiographic evaluation was done using preoperative radiographs taken within 1 month before index surgery in our institution. We used a preoperative standing 45° flexion posteroanterior radiograph (Rosenberg view) and a standing AP knee radiograph taken on a 14- × 17-inch (36- × 43-cm) grid cassette for evaluation of OA in the tibiofemoral joint and a standing whole-limb AP radiograph taken on a 14- × 51-inch (36- × 130-cm) grid cassette for evaluation of coronal limb alignment. To control the rotational position of the AP radiograph, an identical foot rotation angle was obtained using a reference foot template on the platform incorporated for our plane radiographic system. In addition, appropriateness of a knee position (patellar facing forward) of the whole-limb AP radiograph was confirmed using a preview monitor before final acquisition of the radiograph. All radiographic images were digitally acquired using a picture archiving and communication system (PACS). Assessment was performed on a 24-inch (61-cm) monitor (U2412 M; Dell, Round Rock, TX, USA) in portrait mode using PACS software (Infinite, Seoul, Korea). This software package allows the investigator to detect the bisecting point of any area on the femur or tibia and to measure the angle between any two lines drawn on the digital image. The minimum detectable changes by the software were 0.1° in angle and 0.1 mm in length.
The mechanical tibiofemoral angle was defined as the angle formed by the intersection between the mechanical axes of the femur (the line from the femoral head center to the femoral intercondylar notch center) and the tibia (the line from ankle talus center to the center of the tibial spine tips). A negative value was given to knees in varus alignment. The weight loading line of the knee (%) was defined as the portion of the mechanical axis of the limb (the line from the femoral head center to the ankle talus center) passing through the knee from the edge of the medial tibial plateau to the edge of the lateral tibial plateau.
Radiographic degrees of OA in the medial tibiofemoral joint and the lateral tibiofemoral joint were assessed separately based on the Kellgren-Lawrence grading system [10]. We then classified the radiographic degree of OA in each compartment into two groups: Type 1 (none to mild OA) involving Kellgren-Lawrence Grades 0, 1, and 2 and Type 2 (moderate to severe OA) involving Kellgren-Lawrence Grades 3 and 4.
To determine intraobserver and interobserver reliabilities of radiographic assessment, two orthopaedic surgeons (HHW and MSJ) performed all radiographic assessments in 20 randomly selected knees twice, with a 3-week interval between evaluations. The intraobserver and interobserver reliabilities of measurements for the mechanical tibiofemoral angle and the weight loading line were evaluated using intraclass correlation coefficients (ICCs), while those for judgment of types of radiographic OA were evaluated using kappa statistics. All ICCs of intraobserver and interobserver reliabilities of alignment measurements were greater than 0.96 (range, 0.96–0.98), and all kappa coefficients were greater than 0.85 (range, 0.86–1.00), representing satisfactory agreement. Thus, measurements taken by one investigator (HHW) were used in the analyses.
The conditions of the medial and lateral meniscus were assessed separately based on operative findings during ACL reconstruction. Meniscal conditions were categorized into five grades: (1) no tear; (2) presence of tear but repaired; (3) irreparable tear undergoing partial meniscectomy or loss of meniscus equivalent to partial meniscectomy; (4) irreparable tear undergoing subtotal meniscectomy or loss of meniscus equivalent to subtotal meniscectomy; and (5) irreparable tear undergoing total meniscectomy or loss of meniscus equivalent to total meniscectomy. The meniscal conditions then were classified into two types: Type 1 (no to low-grade injury) involving no tear, repair, or partial meniscectomy and Type 2 (high-grade injury) involving subtotal or total meniscectomy.
All statistical calculations were performed with SPSS® for Windows® (Version 17.0; SPSS Inc, Chicago, IL, USA), and p values less than 0.05 were considered significant throughout. To examine differences in coronal limb alignments between groups, the mechanical tibiofemoral angle and the weight loading line percentage were compared using Student’s t-test. Additionally, to examine the proportion of patients with varus malalignment, we dichotomized the alignment results with cut-off values of 5° varus for the mechanical tibiofemoral angle and 25% for the weight loading line and then compared their proportions between groups using the chi-square test. Comparisons of meniscal and radiographic OA conditions then were performed using the chi-square or Fisher’s exact test. Based on the results of the coronal alignment and meniscal and radiographic OA conditions, the proportions of potential candidates for high tibial osteotomy were computed and then compared between two groups using Fisher’s exact test.
Results
The revision ACL reconstruction group had more frequent varus coronal limb malalignment (Table 2) coupled with more severe degrees of medial meniscus injury and/or medial tibiofemoral OA (Table 3) than the primary ACL reconstruction group. In terms of the average mechanical tibiofemoral angle and weight loading line percentage the patients in the revision ACL reconstruction groups had significantly more varus alignment than those in the primary ACL reconstruction group (p = 0.006 and 0.010, respectively), but average differences of the values were relatively small, 1.1° and 5%, respectively. Based on our cut-off values, however, varus malalignment was found in 19% of the revision ACL reconstruction group versus 8% of the primary ACL reconstruction group in terms of the mechanical tibiofemoral angle (p = 0.029), and 22% of the revision ACL reconstruction group versus 9% of the primary ACL reconstruction group in terms of the weight loading line % (p = 0.011) (Table 2). In the comparison of meniscal condition, high-grade medial meniscal injury (subtotal or total meniscectomy) was significantly more prevalent in the revision ACL reconstruction group than in the primary ACL reconstruction group (34% versus 16%, p = 0.007) (Table 3). Additionally, there was a tendency toward more frequent higher-grade radiographic OA at the medial tibiofemoral compartment in the revision ACL reconstruction group than in the primary ACL reconstruction group (19% versus 9%, p = 0.076) (Table 3).
Consequently, when our indications for high tibial osteotomy were applied, the revision ACL reconstruction group included significantly more potential candidates for high tibial osteotomy than the primary ACL reconstruction group (eight of 58 patients [14%] versus two of 116 patients [2%], p = 0.003) (Table 4).
Discussion
Clinical results after revision ACL reconstruction have been reported to be less satisfactory than those after primary ACL reconstruction [12, 17, 25]. One of the most important causes of the inferior outcomes could be an established medial tibiofemoral joint problem, such as an irreparable medial meniscal tear and/or progressed medial tibiofemoral joint OA, conditions that frequently are combined in patients undergoing revision ACL reconstruction [1, 4, 8, 23]. Given that medial tibiofemoral joint problems can result in more serious clinical consequences when coupled with varus malalignment, information regarding coronal limb alignment in patients undergoing revision ACL reconstruction is crucial to establishing management plans with better outcomes. We sought to address this issue by determining whether (1) patients undergoing revision ACL reconstruction have more frequent varus malalignment coupled with more severe degrees of medial meniscal injury and/or medial tibiofemoral OA, and (2) have conditions that might benefit from high tibial osteotomy more frequently than those undergoing primary ACL reconstruction.
This study has several limitations that should be considered. First, our definition of varus malalignment and criteria for potential indication of high tibial osteotomy were set arbitrarily. However, our cut-off value for varus malalignment, ie, varus 5° of the mechanical tibiofemoral angle or 25% of the weight loading line, was biomechanically meaningful, as more varus alignments than these are known to adversely affect tibiofemoral mechanics and pressure distribution on the knee [24]. Moreover, several clinical studies have used similar cut-off values for varus malalignment and indication for high tibial osteotomy [2, 9, 11, 16, 21]. Thus, we believe that our definitions of varus malalignment and criteria for high tibial osteotomy are clinically reasonable. Second, we have performed high tibial osteotomy combined with primary or revision ACL reconstruction for patients who met our indications only since 2011, when we started considering the need of high tibial osteotomy in patients undergoing ACL reconstruction. Thus, we performed concurrent high tibial osteotomy not for all 10 patients involved in this study who met our indications, but only for study patients who underwent surgery between 2011 and 2012 (four patients in the revision group and one patient in the primary group. Nevertheless, we intended to include our whole series of patients undergoing revision ACL reconstruction to establish adequate sample size for more reliable results. As we used indications for high tibial osteotomy based on objective factors, we believe that we were able to define the potential candidates in all study patients without bias. In addition, this study did not provide the clinical outcomes of the patients undergoing concurrent high tibial osteotomy. Thus, we cannot draw a definite conclusion whether concurrent high tibial osteotomy based on our indications would be beneficial. Nevertheless, considering the aforementioned adverse effects of varus malalignment coupled with medial tibiofemoral joint problems, if indicated, concurrent high tibial osteotomy may be a clinically sound option for mostly young and active patients undergoing ACL surgeries. However, this should be confirmed by further studies. Third, we used indications for high tibial osteotomy defined using three objective findings including coronal limb alignment, degree of radiographic knee OA, and meniscal condition. However, indications for high tibial osteotomy should be determined not only based on these objective findings but also based on patients’ symptoms and function, such as medial knee pain or presence of varus thrust gait. Thus, the proportion of potential candidates for high tibial osteotomy may change when including the indications based on patients’ symptoms and function. For example, a patient undergoing ACL reconstruction with 10% of the weight loading line of the knee but no medial tibiofemoral OA and medial meniscal injury would not be a candidate for high tibial osteotomy in our definition. However, if the patient had significant varus thrust gait or sustained medial knee pain, a high tibial osteotomy might be indicated. Nevertheless, such symptoms and function for high tibial osteotomy can be more frequent in patients undergoing revision ACL reconstruction [1, 4, 14–16]. Therefore, our findings for more potential candidates in the revision ACL reconstruction group might not change even if we added patients’ symptoms and function to the indications for high tibial osteotomy. Moreover, we believe that our indications for high tibial osteotomy based on the objective findings provide more generalizable results. Fourth, although the average values of the mechanical tibiofemoral angle and weight loading line were statistically different between the two groups, their differences were relatively small, 1.1° and 5% on average, so the differences might not be clinically meaningful. This result may stem from the nature of our study subjects; as we intended to focus on the patients undergoing ACL reconstruction, we included only patients with sustained instability originating from ACL laxity, not patients who had ACL damage but had undergone high tibial osteotomy alone because their major symptom stemmed from medial tibiofemoral OA. Nevertheless, the proportion of patients with varus malalignment in the revision ACL reconstruction group was more than double that in the primary ACL reconstruction group. This finding would be more clinically meaningful when considering the higher proportion of medial tibiofemoral problems in the revision ACL reconstruction group. Finally, the characteristics of our study subjects, such as the male predominance (93%) and Asian population, might limit direct application of our findings in populations with different characteristics. Although more frequent medial meniscus injury and/or cartilage damage at the medial tibiofemoral joint has been reported consistently in several studies with various populations [1, 4, 8, 23], further study would be required to draw a conclusion for this issue.
Our findings support the hypothesis that patients undergoing revision ACL reconstruction have more frequent varus malalignment than those undergoing primary ACL reconstruction. Similar to previous reports [4, 8], more frequent high-grade medial meniscal tears were found in our revision ACL reconstruction group than in the primary ACL reconstruction group. Similarly, the incidence of moderate to severe radiographic medial tibiofemoral joint OA tended to be higher in the revision ACL reconstruction group. It is unclear why the revision ACL reconstruction group had more frequent varus malalignment than the primary ACL reconstruction group. The varus malalignment might be preexisting and a cause of failure in the reconstructed ACL [15, 16], or this finding may be a consequence of failed ACL reconstruction owing to medial tibiofemoral joint space narrowing by progression of medial tibiofemoral OA. Its causal relationship would be important to determine for management of patients undergoing primary ACL reconstruction and revision ACL reconstruction. However, as all but one initial ACL reconstruction in our revision group were performed in other hospitals and therefore information regarding initial alignment for these patients was extremely limited, we were unable to draw a conclusion regarding causal relationships in this study. Nevertheless, our findings highlight the fact that knee surgeons need to pay more attention to coronal limb alignment in the management of patients receiving revision ACL reconstruction. Additionally, owing to a possibility of a cause for failure of ACL reconstruction, varus malalignment in the patients undergoing primary ACL reconstruction, although relatively uncommon, may need to be considered and studied.
Our findings also support the hypothesis that the revision ACL reconstruction group would have more potential candidates for high tibial osteotomy than the primary ACL reconstruction group. Coupled with more frequent varus malalignment, the higher incidence of medial tibiofemoral joint problems in the patients of the revision ACL reconstruction group led to much more frequent potential candidates for high tibial osteotomy by our criteria (14% versus 2%, p = 0.003). Based on this notable finding, we reasonably suggest that a combined high tibial osteotomy and revision ACL reconstruction in potential candidates could improve longer-term clinical outcomes, particularly for younger and more active patients. Nevertheless, this speculation must be tested in further studies.
In this series, we found that patients undergoing revision ACL reconstruction had more frequent varus malalignment and medial TF joint problems than patients undergoing primary ACL reconstruction. Consequently, patients undergoing revision ACL reconstruction met a standard set of high tibial osteotomy indications more frequently. These findings suggest that knee surgeons should integrate considerations of medial TF joint condition and coronal limb alignment in the treatment of patients undergoing revision ACL reconstruction. Additionally, it would be worth researchers starting to consider coronal limb alignment as a possible predictor variable to follow in large prospective studies of primary ACL reconstruction to see whether varus malalignment causes failure or is the result of it.
References
Ahn JH, Lee YS, Chang MJ, Yim HS. Analysis of revision anterior cruciate ligament reconstruction according to the combined injury, degenerative change, and MRI findings. Knee. 2011;18:382–386.
Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002;10:38–43.
Binfield PM, Maffulli N, King JB. Patterns of meniscal tears associated with anterior cruciate ligament lesions in athletes. Injury. 1993;24:557–561.
Brophy RH, Wright RW, David TS, McCormack RG, Sekiya JK, Svoboda SJ, Huston LJ, Haas AK, Steger-May K; Multicenter ACL Revision Study (MARS) Group. Association between previous meniscal surgery and the incidence of chondral lesions at revision anterior cruciate ligament reconstruction. Am J Sports Med. 2012;40:808–814.
Bruyere O, Genant H, Kothari M, Zaim S, White D, Peterfy C, Burlet N, Richy F, Ethgen D, Montague T, Dabrowski C, Reginster JY. Longitudinal study of magnetic resonance imaging and standard X-rays to assess disease progression in osteoarthritis. Osteoarthritis Cartilage. 2007;15:98–103.
Chang CB, Koh IJ, Seo ES, Kang YG, Seong SC, Kim TK. The radiographic predictors of symptom severity in advanced knee osteoarthritis with varus deformity. Knee. 2011;18:456–460.
Hede A, Larsen E, Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16:122–125.
Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:199–217.
Kean CO, Birmingham TB, Garland JS, Jenkyn TR, Ivanova TD, Jones IC, Giffin RJ. Moments and muscle activity after high tibial osteotomy and anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2009;41:612–619.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Lattermann C, Jakob RP. High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc. 1996;4:32–38.
Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551–1557.
McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556.
Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees: a two- to seven-year follow-up study. Am J Sports Med. 1993;21:2–12.
Noyes FR, Barber-Westin SD. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131–1143.
Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28:282–296.
Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K. Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5- to 9-year follow-up. Am J Sports Med. 2006;34:1604–1614.
Sharma L, Chmiel JS, Almagor O, Felson D, Guermazi A, Roemer F, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M. The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis. 2013;72:235–240.
Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, Cahue S, Marshall M, Hudelmaier M, Dunlop D. Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58:1716–1726.
Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940–1945.
Stein BE, Williams RJ 3rd, Wickiewicz TL. Arthritis and osteotomies in anterior cruciate ligament reconstruction. Orthop Clin North Am. 2003;34:169–181.
Teichtahl AJ, Cicuttini FM, Janakiramanan N, Davis SR, Wluka AE. Static knee alignment and its association with radiographic knee osteoarthritis. Osteoarthritis Cartilage. 2006;14:958–962.
Thomas NP, Kankate R, Wandless F, Pandit H. Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med. 2005;33:1701–1709.
Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38:349–355.
Wright RW, Gill CS, Chen L, Brophy RH, Matava MJ, Smith MV, Mall NA. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94:531–536.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at the Joint Reconstruction Center, Seoul National University Bundang Hospital, Seongnam-si, Republic of Korea.
About this article
Cite this article
Won, H.H., Chang, C.B., Je, M.S. et al. Coronal Limb Alignment and Indications for High Tibial Osteotomy in Patients Undergoing Revision ACL Reconstruction. Clin Orthop Relat Res 471, 3504–3511 (2013). https://doi.org/10.1007/s11999-013-3185-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3185-2