Abstract
The cranio-cervical junction area is a very special and complex region of the spine. Junctional traumatic injuries are common in clinical practice and are mostly due to blunt trauma. In adults it more frequently involves the lower cervical spine, whereas in children the atlanto-axial region is more prone to injuries. Vertebral trauma may cause temporary or permanent disability that may be seen immediately after the traumatic event or, at a distance, as a result of mechanical instability. Traumatic injuries may involve the bone, the ligamentous system, and the spinal cord. Plain film of the cervical spine could be the first imaging examination requested in patients with suspected cervical trauma; however, it has low diagnostic performance, especially in patients with C-spine collar. Multidetector computed tomography represents the imaging technique of choice in emergency settings to evaluate the bone injuries. Magnetic resonance is indicated for the identification of the ligamentous and spinal cord injuries and for the preoperative assessment of the unstable cervical spine. Diagnostic pitfalls are related with technical and anatomical factors; the knowledge of these factors is important to avoid misdiagnosis. In this chapter, the relevant literature concerning all of these topics is finally summarized.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cranio-cervical junction
- Cranio-vertebral junction
- Spine injury
- Vertebral fracture
- Cervical injury
- Ligamentous injury
- Spinal cord injury
1 Introduction
The cranio-cervical (or craniovertebral) junction (CCJ or CVJ) area is a very special, intricate, and complex region of the spine.
This functional unit is constituted by bony segments connected via a complex ligamentous system whose vulnerability to injury may compromise the structural integrity of the cranio-cervical junction.
A comprehensive and detailed knowledge of this anatomical region is the key not only for an adequate surgical management of the disorders affecting this area but also to avoid complications.
The CCJ is the transition from the head to the spine; and it carries unique anatomical, biomechanical, and functional properties (Brotis et al. 2015).
It is composed of three bone elements: the first and second cervical vertebrae (also known as atlas and axis, respectively), and the occiput, in conjunction with a ligamentous complex, structured to perform its unique role of providing stability and mobility of the cervical spine.
The end-result is a magnificent interplay between motion and stability. The occipital condyles form the cranial end of the CCJ and articulate with the atlas or C1 vertebra at the atlanto-occipital joint. The latter is mainly responsible for flexion and extension movements. Similarly, atlas meets the axis vertebra (C2) at the atlanto-axial joint. This joint is responsible for most of the CCJ rotation (Brotis et al. 2015).
Junctional traumatic injuries are common in clinical practice. In fact, about half of all cervical fractures occur in this area (Fine et al. 1979).
Blunt trauma represents the most frequent mechanism of injury in modern countries.
Blunt trauma resulting injuries essentially depends on changes in pressure and shear forces produced by three main mechanisms: (1) direct-impact, (2) compression, and (3) rapid acceleration/deceleration injuries. Combined compression and deceleration (airbag/seat belt injuries) cause spinal trauma most frequently (Romano et al. 2017).
Approximately 10–30% of all spinal trauma results in spinal cord injury (Fine et al. 1979), which is considered a major source of morbidity and mortality, particularly in young people (Hu et al. 1996).
Clinical examination of upper cervical spine trauma can be considered a diagnostic challenge, since many neurological scenarios are possible, and the patient may often have an associated head trauma that may alter the level of consciousness and complicate examination.
The diagnosis of CCJ lesions in traumatized patients is a complex task and often involves multiple steps where radiologic imaging plays a central role.
In the setting of blunt trauma to the cranio-cervical junction, imaging plays a major role in the management and prognosis of these injuries. The acute imaging evaluation of what are usually high-energy mechanisms of injury typically involves an initial computed tomography (CT) assessment and, frequently, subsequent emergency magnetic resonance imaging (MR) assessment.
Injuries involving the upper cervical spine may be distinguished in: injuries affecting mainly bone structures (Menezes and Traynelis 2008) and predominantly ligamentous injury (Hadley 2002). Thus basing on the principle that bone injuries may heal with conservative treatment, whereas ligamentous injury would not heal properly, leading to an unstable spine.
The current imaging recommendations in the trauma scenario include an initial CT evaluation followed by MR, in case of significant bony injury or when a ligamentous injury is suspected (Sundgren et al. 2007).
In this chapter, the relevant literature concerning this issue, particularly focusing on “rare” CCJ traumatic events, is summarized.
2 Imaging Approach
CCJ injuries are observed, predominantly, as a result of motor-vehicle accidents, falls from heights, and sports; and thus, young men are more affected. Another age peak is seen in the elderly who have preexisting degenerative vertebral disease.
Even though plain films of the cervical spine are often the first imaging examination requested in patients with suspected cervical trauma, its low diagnostic performances, especially in patients with C-spine collar, and the wider availability of multidetector computed tomography (MDCT) have changed this algorithm (Tins and Cessar-Pullicino 2004; Frankel et al. 1994; Stiell et al. 2001).
Vertebral trauma is responsible for temporary or permanent disability that may be seen immediately after the traumatic event or, at a distance, as a result of mechanical instability.
MDCT imaging best depicts the biomechanical parameters that have caused specific injuries and thus helps to provide rapid and stable therapy decisions (Schueller et al. 2015a).
In addition to the diagnosis of bony lesions, MDCT scan allows an accurate assessment of the stability/instability of the injury, which leads to the timing of surgical treatment, although the issue is still controversial in the literature (Parizel et al. 2010).
The radiologist must be able to recognize vertebral fractures, to classify according to the different patterns of fracture (compression, distraction, rotation), to drive the continuation of the diagnostic plan, and to indicate the use of MRI to rule out or characterize spinal cord injury (Schueller et al. 2015b).
The concept of stability is extremely important for the choice of therapy and is based on the “three-column model” by Denis: the anterior column consists in the anterior longitudinal ligament and the anterior two-thirds of the vertebral body, the middle column is the posterior one-third of the vertebral body including the anulus fibrosus and posterior longitudinal ligament, and the posterior column, which includes all structures posterior to the posterior longitudinal ligament (Schueller et al. 2015a).
The availability of fast, cost-effective imaging methods with high sensitivity and specificity in the detection of any potentially unstable injury that may cause or exacerbate neurologic deficits makes MDCT the imaging modality of choice for the evaluation of patients with acute traumatic injury of the CCJ and of the cervical spine (Diaz Jr. et al. 2005). An appropriately thin-section axial source data-set of 0.75 mm is recommended to obtain adequate MPR (ideally, 2 mm or less).
For the diagnosis of spinal lesions, axial images and sagittal reconstructions are necessary. Because of the curvatures of the vertebral column in the sagittal plane, the coronal images are not optimal and rarely provide additional information. However, sagittal and coronal reconstructions are recommended for a complete examination.
To obtain good quality sagittal and coronal MPR, a slice thickness of 1.0/1.5 mm and a reconstruction interval of 1.5 mm are suggested, both in the unenhanced and enhanced MDCT scans.
MDCT is fast, reduces motion artifacts, reduces partial volume effects, reduces image noise, and provides better i.v. contrast material opacification of blood vessels, enhancement of parenchymal organs, and high-quality MPR and isotropic visualization, which increase the diagnostic power of this imaging modality, to the benefit of traumatized emergency patients.
Since sagittal and coronal references are considered standard in the CT of the spine, they must therefore be included in the study protocol. In some cases of spine fracture, 3D surface renderings can provide additional information in diagnostic interpretation and surgical planning (Bensch et al. 2012).
If axial images and sagittal reformulations of sufficient quality are available, in most cases it is possible to confirm or rule out unstable lesions by distinguishing the direct and indirect signs of pathology.
The bone lesion presents as cortical defects with sharp non-sclerotic edges and fracture lines that extend into the bone. The degree of destruction of the vertebra varies from mild-to-severe comminution.
The evident malposition of the joints or vertebrae is a precise sign of injury and should be considered as such until proven otherwise, even in the absence of bone defects. Three-dimensional surface renderings can help to clarify whether a joint is in a physiological or pathological position.
If only soft tissue structures such as the intervertebral discs and the ligamentous complex are involved, the dislocation of the vertebral bodies indicates instability. Furthermore, the widening of the facet joint spaces is a sign of soft tissue injury and may involve instability. There are normal variations, but they are rarely limited to a single disk or joint.
Enlargement and/or angulation of 1 or more isolated intervertebral spaces also suggests lesions. A fracture or rupture of soft tissue structures is usually accompanied by an adjacent hemorrhage, which looks like a soft tissue vertebral column. Most lesion patterns show a preference for the segments of the spine that are biomechanically more susceptible to each specific type of injury (Bensch et al. 2004).
MR is indicated for the identification the ligamentous injuries and the treatment planning of the unstable cervical spine, for the direct evaluation of the spinal cord if its traumatic involvement is suspected, and in patients who cannot be clinically evaluated for more than 48 h due to altered level of consciousness (Como et al. 2009).
3 Bone Injuries
3.1 Occipital Condyle Fractures
Occipital condyle fractures (OCFs) are relatively unusual, occurring nearly universally in the setting of high-energy blunt trauma (Anderson and Montesano 1988; Aulino et al. 2005).
Often difficult to identify based on plain radiographs alone, OCFs are now diagnosed more frequently due to the widespread use of MDCT in the standard trauma evaluation (Bloom et al. 1997; Wasserberg and Bartlett 1995).
Occipital condyle fractures have typically been associated with lower cranial nerve palsies, particularly hypoglossal nerve injury.
Anderson and Montesano first classified OCFs based on the vector of force precipitating the injury according to this classification system:
-
Type I injuries result from axial loading, and the fractured condyle is comminuted with minimal or no displacement; generally stable lesions.
-
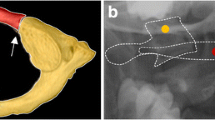
Type II fractures result from direct trauma to the skull and occur in conjunction with basilar skull fractures: these injuries are usually stable, with some potential degree of instability if the condyle is separated from the cranium (Fig. 1).
-
Type III injuries are avulsion fractures that occur from lateral flexion or rotatory forces with resultant pulling by the alar ligament; these injuries can be potentially unstable, especially if a bilateral lesion is present, leading to atlanto-occipital dissociation, implying ligamentous injury.
A 17-year-old male was admitted to the Emergency Department after a head blunt trauma. Axial (a), coronal (b) MIP and 3D reconstruction (c, d) images show a fracture of the occipital bone extending to the left condyle (type II fracture sec. Anderson and Montesano, type I sec. Tuli). There is also a bilateral haemosinus (arrow). This fracture can be associated with lower cranial nerve palsies, particularly hypoglossal nerve injury
Tuli et al. (Tuli et al. 1997) proposed a classification oriented to the treatment and based on the presence of fragment displacement, stability of the atlanto-occipital and atlantoaxial joints, and MR imaging evidence of ligamentous injury. The classification divides OCFs into 2 major categories:
-
Type 1: without displacement of fragments.
-
Type 2: with displacement of fragments.
Displaced OCFs were further subdivided into those fractures without radiographic evidence of instability of the occipitoatlantoaxial joint complex (Type 2a) and those demonstrating radiographic evidence of instability (Type 2b).
In the Tuli classification, OCFs types I and II of Anderson and Montesano classification are grouped together as Tuli type 1, as they have the same treatment. Tuli type 2A fractures may require a rigid collar, whereas type 2B lesions require surgical intervention (Tuli et al. 1997; Caroli et al. 2005).
3.2 Atlas Fractures
Atlas fractures may be difficult to diagnose. Classically, patients with C1 fractures present with pain in the upper neck and a history of trauma to the top of the head such as in shallow diving or in automobile collision (Garrett et al. 2010).
Once identified, atlas fractures can be classified by the fracture pattern.
Jefferson in 1920 described 4 types of atlas fractures:
-
Type 1: fractures involving the posterior arch only.
-
Type 2: anterior arch only.
-
Type 3: both arches involved.
-
Type 4: lateral mass fracture.
Similarly, Gehweiler in 1976 proposed a five-tired classification of the C1 vertebra:
-
Type I: fracture of the anterior arch.
-
Type II: fracture of the posterior arch.
-
Type III: combination fractures of anterior and posterior arches.
-
Type IV: lateral mass fractures.
-
Type V: fracture of the transverse process.
Landels and Van Peteghem in 1988 reduced the injury patterns in three:
-
Type I: fractures involving a single arch (Figs. 2, 3, and 4).
-
Type II: fractures involving both anterior and posterior arches (Fig. 5).
-
Type III: representing lateral mass fractures.
A 54-year-old man admitted to the Emergency Department with a history of car accident. Axial (a–c) and coronal (d) CT images show a fracture of the anterior arch of the atlas (type I sec. Landels, and type III sec. Levin and Edwards), and partial avulsion of the right tubercle for the insertion of the transverse ligament on the C1 lateral mass (c, arrow) (type II sec. Dickman and Sonntag) (b, c not visible on 3D reconstruction). 3D reconstruction images give an overall assessment of atlas injuries (e, f). Coexistence of a simultaneous transverse atlantal ligament rupture (TAL) requires cranio-cervical fixation
Levin and Edwards (Bellabarba et al. 2006) in 1991 classified C1 fractures in the following five groups:
-
Type I: posterior arch fracture (Fig. 2).
-
Type II: burst fracture.
-
Type III: anterior arch fracture (Fig. 3).
-
Type IV: transverse process fracture.
-
Type V: lateral mass fracture.
No classification scheme from the above has been tested for validity and reliability, and none guides treatment or prognosis.
C1 fractures are a complex group of upper cervical injuries, and diagnosis and treatment thereof require a holistic approach. The context of any concurrent spinal trauma in addition to patients’ overall health (e.g., obesity, myelopathy, ability to comply with treatment, osteoporosis) will dictate treatment methods. According to the latest recommendations, the treatment of isolated C1 fracture is independent from the specific injury pattern. The majority of these injuries can be treated with nonoperative immobilization and a hard cervical collar or a halo-vest; certain fracture characteristics will require surgical fixation or fusion. The coexistence of a simultaneous transverse atlantal ligament rupture (TAL) or a long-term local instability requires cranio-cervical fixation (Ryken et al. 2013).
The surgeon must be aware of the fracture patterns that require more extensive stabilization and follow patients closely for signs of instability and deformity after nonoperative management (Mead et al. 2016).
3.3 Axis Fractures
Andersons and D’Alonzo classified it into three categories:
-
Type I: apical dens fracture.
-
Type II: fracture through the base of the dens.
-
Type III: with the fracture line into the C2 body (Figs. 6 and 7).
A 23-year-old male was admitted to the Emergency Department after a motor vehicle crash. CT in axial plane (a, b), 3D reconstruction (c), and CT in sagittal plane (d) showing a fracture of the posterior arc of the atlas (a) (type I both sec. Landels and sec. Levin and Edwards), detachment of bilateral pars interarticularis of C2 (b), and anterior translation of the C2 body (d) “Hangman fracture type II sec. Levine and Edwards”. It is the most common type of Hangman’s fracture and results from hyper-extension followed by hyperflexion. It is unstable and may produce a small posterior fracture fragment that can narrow the canal and cause spinal cord injury (c)
Type II Anderson’s and D’Alonzo’s odontoid fractures have been further subclassified by Roy-Camille according to the inclination of the fracture line into subtype 1 (forward), subtype 2 (backwards), subtype 3 (horizontal), and subtype 4 (fracture with rotation or English policeman’s hat) (Brotis et al. 2015).
Of the three fracture patterns described, Type 1, the least common, involves an obliquely oriented fracture through the distal third of the odontoid, typically distal to the level of the transverse cruciate ligament. These fractures are often secondary to an avulsion injury involving the apical ligament and in, the absence of other ligamentous disruption, are stable injuries. Type 2, the most common of the three, involves a horizontal fracture through the neck (or base) of the odontoid at its intersection with the C2 body. Of the three types, these are noted to have the highest non-union rate with non-operative treatment. Type 3 fractures are, in fact, C2 vertebral body fractures wherein the fracture line extends into one or both of the superior articulating processes, toward the C1–2 joint. These fractures demonstrate a high rate of union with non-operative treatment (Jefferson and Harrop 2017).
Pars interarticularis fractures are best seen on transverse and parasagittal CT images. They are often asymmetric and are considered atypical when the fracture extends into the posterior vertebral body. Atypical fracture patterns are actually quite common and may involve the transverse foramen, placing the vertebral artery at risk for injury (Al-Mahfoudh et al. 2016).
3.3.1 Hangman’s Fractures
Also named as traumatic spondylolisthesis of C2, Hangman’s fracture refers to bilateral pars interarticularis fractures, which bear similarities to findings seen in persons who have undergone judicial hanging. Most of these fractures result from falls and motor vehicle crashes and reflect a variety of injury mechanisms.
The most widely used classification for traumatic spondylolisthesis is the system devised by Effendi and modified by Levine and Edwards, as outlined in the following subsections:
-
Type 1 fractures – Type 1 fractures are bilateral pars fractures without angulation or significant translation. These result from hyperextension and axial loading and are considered mechanically and neurologically stable.
-
Type 2 fractures – Type 2 fractures include disruption of the C2–3 disk with anterior translation of the C2 body. These are the most common hangman’s fracture type and result from hyper-extension with axial loading followed by hyperflexion. They are unstable and may produce a small posterior fracture fragment that can narrow the canal and cause spinal cord injury (Figs. 4 and 7).
-
Type 2A fractures – Type 2A fractures are unstable flexion-distraction injuries with C2 angulation but without translation (Fig. 8).
-
Type 3 fractures – Type 3 fractures are combined anterior translation and angulation with facet subluxation or frank dislocation. These are highly unstable injuries that result from hyperflexion and compression (Bernstein and Baxter 2012).
A 35-year-old male was admitted to the Emergency Department after a motor vehicle crash. Axial (a) and coronal (b) and sagittal (c) CT images and 3D reconstructions (d–f) showing detachment of bilateral pars interarticularis of C2, with a slight translation of the C2 body and an oblique line of fracture and angulation of the fragments (c). “Hangman fracture type IIa sec. Levine and Edwards.” This is an unstable fracture
4 Ligamentous Injuries
The cranio-cervical junction is composed of two major joints: the atlanto-occipital joint and the atlanto-axial joint. These two joints are responsible for the majority of the movement available in the entire cervical spine and the anatomical structure of each is based on different biomechanical principles. The mechanical properties of the atlanto-occipital joint are primarily determined by bony structures, whereas those of the atlanto-axial joint are primarily determined by ligamentous structures.
4.1 Occipitocervical Dislocation
Traumatic occipitocervical dissociation (OCD) represents a spectrum of often fatal injuries between the head and the atlas.
It results from ligamentous injury to the cranio-cervical junction and is associated with high mortality and significant neurologic morbidity.
The widespread availability of MDCT and the development of better diagnostic criteria allow a timely diagnosis and a good clinical outcome for this quite rare injuries, once considered fatal (Blackwood III 1908).
Up to 20% of patients with OCD may have only neck pain as symptom, with normal neurological examination at presentation (Horn et al. 2007; Mendenhall et al. 2015; Sweet et al. 2010). So, any patient involved in high-energy trauma should be suspected for OCD, irrespective of clinical findings, and appropriate precautionary measures should be taken until the diagnosis is ruled out.
Traynelis et al. (Traynelis et al. 1987) classified OCD patterns into three types according to the direction of dislocation of the occiput relative to the cervical spine:
-
Type I OCD consists in anterior displacement of the occiput with respect to C1.
-
Type II is primarily a longitudinal distraction with separation of the occiput from the atlas.
-
Type III OCD exists when the occiput is posteriorly dislocated from C1.
Bellabarba et al. (Bellabarba et al. 2006) recently published a three-stage classification, also known as Harborview classification system more “clinically oriented.” It considers the injury severity and quantifies the stability of the occipitocervical junction with the therapeutic implications. Stage I injury is defined as a stable minimally or nondisplaced cranio-cervical injury in which there is sufficient preservation of ligamentous integrity, thus allowing nonoperative treatment. Stage 2 injury includes partially or completely spontaneously reduced bilateral OCD involving minimal displacement (Harris lines within ≤2 mm beyond the upper limit of normal) in which a positive traction test confirms a complete loss of cranio-cervical ligamentous integrity, requiring internal fixation. Stage 3 injury refers to a highly unstable injury defined by gross cranio-cervical malalignment (Harris lines >2 mm beyond acceptable limits), requiring internal fixation (Bellabarba et al. 2006).
Although these represent a spectrum of cranio-cervical injury severity, we reserve the term “cranio-cervical dissociation” for Stage 2 and 3 injuries, where ligamentous instability is complete.
4.2 Transverse Atlantal Ligament Injury
The TAL has the role to retain the odontoid process against the anterior arch of atlas, preventing its backward dislocation that may compress or transect the rostral cervical spinal cord causing instantaneous death or severe neurological deficit (Riascos et al. 2015).
Dickman and Sonntag classified the TAL injury in two types:
-
Type I, disruptions of the substance of the ligament, without an osseous component.
-
Type II, fractures and avulsions involving the tubercle for the insertion of the transverse ligament on the C1 lateral mass (Type II injuries) (Fig. 3).
These two kinds of injuries have specific clinical characteristics leading to different treatment.
TAL lesions in avulsion (type II) present high rate of healing with conservative treatment (external immobilization), different from lesions of the substance of TAL (type I), in which the conservative treatment rarely lead to heal, being the early surgical internal fixation the best treatment in these cases.
5 Craniovertebral Junction Injuries in Children
Atlanto-axial region in children is more prone to injuries than in adults where lower cervical spine is involved more frequently.
The high cervical region in children has several well-described characteristics which predisposes it to injuries:
-
Increased ligamentous laxity which allows excessive motion of the spine.
-
More horizontally oriented facets that allow excess translational rotation in an antero-posterior.
-
Less mature bone maturation (ossification).
-
Higher fulcrum of cervical movement (C2-C3) (in adults at C5-C6).
-
Higher inertia and torque forces associated with a large head/body mass ratio, which shifts fulcrum hip to up (Oppenlander et al. 2014; Joaquim and Alpesh 2011).
Fractures of the odontoid process of the axis account for 10–20% of all cervical spine fractures. Clinical evidence of acute cord injury for at least 1 day and evidence of acute cord injury, spinal cord or column injuries by imaging or electrophysiological studies.
In newborns, all upper cervical injuries usually are associated with cephalic presentation and the use of forceps for rotational maneuvers.
Combination fractures of C1-C2, as already mentioned, are relatively common (Calvy et al. 1987).
Vehicular trauma is the most common cause of upper cervical injuries (56%), followed by falls (17%), twice as frequent in young children. Athletic- and sports-related injuries (wrestling, football, diving, gymnastics, etc.) constitute 13% (more common in old children), whereas, penetrating injuries account for 4% of all spinal injuries. Odontoid epiphysiolysis is typically seen in children <7 years. The neurocentral synchondrosis, which may not fuse completely until the age of 7 years, represents a vulnerable site of injury in young children. Birth injuries are a known cause for SCI (spinal cord injury) in neonates (6%).
The craniovertebral junction which comprises the basi-occiput, atlas, axis, and their supporting ligaments constitutes the most complex and dynamic region of the cervical spine. The wide range of movements possible at this region makes it vulnerable to injury and instability.
Scott et al. (Scott et al. 1990) in a study on the treatment of atlanto-occipital instability in pediatric patients categorized the CVJ injuries in 4 broad categories:
-
Atlantoaxial rotatory subluxation.
-
Atlantoaxial ligamentous instability.
-
Traumatic atlantoaxial fracture.
-
Atlanto-occipital dislocation.
After receiving a child or adult with trauma, physical examination is important in aiding diagnosis; and in a patient with suspected spinal trauma, primary goal should be to achieve immobilization of the spine along with ensuring adequate airway, ventilation, and perfusion. Spinal immobilization prevents vertebral column and spinal cord from further injury during imaging or transportation to a specialized center. In children <8 years, head is relatively larger as compared to torso which forces the neck into a position of flexion when the head and torso are supine on a flat surface.
As children can suffer multiple-level injury, evaluation of entire spinal axis is essential The initial evaluation of C1-C2 injury begins with obtaining plain X-ray films (Shin et al. 2010).
Fracture or nondiagnostic findings on plain radiographs are further delineated by either thin section CT. All patients with neurological deficit undergo MR scans to exclude an acute surgical lesion like extradural hemorrhage (EDH) or herniated disc although the latter is extremely uncommon in children.
Management of spinal cord injuries is usually conservative in children as in adults. Halo vest provides superior immobilization in upper cervical and CCJ injuries and can be used in a child as young as 1 year of age with minimal difficulty (Kim et al. 2011). Custom molding brace has been used especially for lower cervical injuries.
Indications for early surgical intervention, i.e., within 2 weeks of injury, include:
-
1.
Injuries that cannot be reduced and stabilized by external means.
-
2.
Partial spinal cord injury with progressive neurological deficit.
-
3.
EDH.
-
4.
Herniated discs.
6 Pitfalls
Pitfalls in imaging refer to imaging findings which could be misinterpreted as pathology, when they may be a normal appearance or of a less significant etiology than originally thought. These may be related with uncorrected technique or to normal developmental anatomy and normal developmental variance.
6.1 Technical Factors
High-quality radiographs require careful patient positioning relative to the X-ray tube and appropriate exposure factors (kV and mAs). Underexposure can diminish bone detail, and overexposure can obscure soft tissue signs which could facilitate diagnosis and injury detection.
A rotated spine can result in loss of alignment of endplate margins and poor visibility of facet joints. In the cervical region, this can simulate facet joint subluxation. Rotation can lead to asymmetry in the odontoid lateral mass interval which could be misinterpreted as a sign of fracture of the atlas ring.
In the odontoid projection, if the mouth is not adequately opened, the incisor teeth may overlie the peg, mimicking a rare vertical fracture of the peg.
If there is too much or too little tilt of the X-ray tube through the open mouth, there is superimposition of the occiput or of the anterior arch of the atlas, respectively, on the base of the odontoid peg which can simulate a fracture, unless the arch of C1 is followed across and beyond the peg (Keller et al. 2015).
Movement artifacts may affect images especially in the traumatized spinal injury patient who may also have associated brain injury.
At CT, the presence of metalwork in the spine, e.g., previous surgery, can result in significant artifacts especially if instrumentation is made in stainless steel, whereas titanium results in rather less artifact. Imaging technique, such as slight angulation of the gantry and altered exposure factors, or the availability of new reconstruction software, may help to reduce the degree of artifact and improve interpretation. The use of ultrafine slice thickness, slice overlap, and appropriate windowing will facilitate high-resolution sagittal and coronal reconstructions, which will help to increase fracture detection and minimize the risk of missed fracture (Sugimoto et al. 2012).
6.2 Anatomical Factors
In the developing skeleton, the recognition of normal appearances at different stages of growth together with knowledge of normal variants is crucial to avoid pitfalls of interpretation in spinal injury.
In the immature skeleton, areas of lucency may be representative of cartilaginous development due to the expected sites of secondary ossification centers. Each vertebra typically ossifies from three primary ossification centers, one in each half of the vertebral neural arch and one in the body, termed the centrum. Ossification starts at different times in the vertebral arches and in the body. Generally, the vertebral arches unite between 1 and 3 years of age, while the centrum unites with the arches at the neurocentral synchondroses between 3 and 6 years of age. In the upper cervical spine, the centrum unites with the posterior neural arch at approximately the third year.
Exceptions to the above ossification process occur in the first and second cervical vertebrae.
The C1 vertebra ossifies from three centers. Initially, there is an ossification center for each lateral mass which gradually extends into the posterior arch, where the two usually fuse later than in other vertebrae at about the age of 3 or 4 years. Toward the end of the first year, a third center of ossification appears within the anterior arch and unites with the lateral masses between the ages of 6 and 8 years. Failure of fusion or congenital absence of any of these ossification centers may simulate a fracture, but awareness of the normal developmental process, the typical location, and the smooth margins at the defect site will help to avoid misinterpretation (Fesmire and Luten 1989).
The central pillar of the axis (C2) also develops from three segments, namely, the tip of the dens, the base of the dens, and the centrum. The basilar odontoid synchondrosis usually fuses between 3 and 6 years but may be delayed. This should not be mistaken for a fracture. The vestigial form may persist, being represented by a fine sclerotic line, and not to be misinterpreted as a fracture line, which would appear clearly lucent with an irregular margin (Fig. 9). Synchondroses tend to be symmetrical in location, occur at typical sites, and have smooth well-corticated margins.
A 34-year-old man was admitted at the Emergency Department after a head blunt trauma. Coronal (a), axial (b), and sagittal (c) images show a discontinuity through the odontoid, which may mimic a fracture (arrows). Smooth corticated margin, opposed to the irregular margin of a fresh fracture, helps differentiate this normal finding from an injury
Secondary centers of ossification (apophyses) occur at typical locations, as do accessory ossicles, and should not be confused with fracture fragments.
Typically, ossicles are corticated and usually have a smooth margin although occasionally they may have a very subtle marginal irregularity. The Bergman ossicle at the proximal tip of the odontoid peg is a developmental ossicle (the primordial proatlas) and forms the tip of the dental axis. It is frequently located in a V-shaped vertical cleft at the apex of the dens and fuses between the ages of 2 and 12 years, but may remain as a separate ossicle and may not be confused with an avulsion injury (Macalister 1893).
The os odontoideum is not a true accessory ossicle but the result of multiple minor avulsion injuries in childhood. It should not be misdiagnosed as fracture and is correctly identified by the smooth corticated margins opposed to the irregular margins of a fresh facture with cortical break/disruption. The os odontoideum can be stable or unstable. The unstable os odontoideum is associated with abnormal movement which can be readily detected on flexion and extension radiographs, MR may identify secondary effects on the cord as focal atrophy and intrinsic cord signal change or fluid signal between the ossicle and its bone origin. These features are the results of chronic instability and are not related with acute event (Platzer et al. 2007).
Other potential pitfalls in the normally developed spine include prominent lucency of the posterior border of the vertebral body, at the site of the basivertebral venous plexus, and also venous channels within the vertebral body as seen on axial CT images which may simulate a fracture (Fig. 9). The typical Y configuration extending to the basivertebral venous plexus almost confirms the venous nature and excludes a fracture (Kohler and Zimmer 1993).
7 Conclusions
CCJ injuries may cause acute catastrophic neurologic deficits as well as chronic disability.
Although similar in the mechanism of injury, each lesion requires a specific treatment to optimize the patient outcome. Many injuries may be conservatively treated; others, however, require a more aggressive surgical approach.
Due to the rarity of some of the described injuries, general recommendations for the treatment are often difficult to establish.
As a general rule, ligamentous injuries should be considered unstable lesions requiring surgical treatment. Bony injuries in the majority of cases can be conservatively treated, reserving surgery for unstable patterns.
The instability and the presence of a neurological injury can guide surgical treatment, which often involves early stabilization and rehabilitation. However, in the literature many cases of unstable injuries associated with neurological deficit successfully non-operatively managed are described. Often the prolonged immobilization and the bed rest may be associated with side effects. In some of these cases, occult instability is noted with delayed dynamic imaging and requires late surgical intervention.
The speed and the accuracy of MDCT, both in acquiring data and in reformatting images, make it the most suitable diagnostic method in the total body evaluation of the polytrauma patient. Actually, it allows promptly managing the patient, establishing if conservative or operative approach is needed (interventional or surgical). MR is intended as second-level examination for the evaluation of soft tissues and cord injuries.
The imaging evaluation of the spine can be challenging and there are many pitfalls to be avoided. Familiarity with normal radiological anatomy, awareness of technical factors which can lead to misinterpretation, and knowledge of normal ossification and normal variants will minimize the risk of over- or under-reporting radiological findings.
Abbreviations
- CCJ:
-
Cranio-cervical junction
- CVJ:
-
Craniovertebral junction
- CT:
-
Computed tomography
- MR:
-
Magnetic resonance
- MDCT:
-
Multidetector computed tomography
- MPR:
-
Multiplanar reform
- OCFs:
-
Occipital condyles fractures
- TAL:
-
Transverse atlantal ligament
- OCD:
-
Occipitocervical dissociation
- SCI:
-
Spinal cord injury
- EDH:
-
Extradural hemorrhage
References
Al-Mahfoudh R, Beagrie C, Woolley E et al (2016) Management of typical and atypical Hangman’s fractures. Global Spine J 6(3):248–256. https://doi.org/10.1055/s-0035-1563404
Anderson PA, Montesano PX (1988) Morphology and treatment of occipital condyle fractures. Spine 13:731–736
Aulino JM, Tutt LK, Kaye JJ et al (2005) Occipital condyle fractures: clinical presentation and imaging findings in 76 patients. Emerg Radiol 11:342–347
Bellabarba C, Mirza SK, West GA et al (2006) Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine 4:429–440
Bensch FV, Kiuru MJ, Koivikko MP et al (2004) Spine fractures in falling accidents: analysis of multidetector CT findings. Eur Radiol 14(4):618–624. Epub 2003 Oct 7
Bensch FV, Koivikko MP, Koskinen SK (2012) Multidetector computed tomography of spinal fractures. Semin Roentgenol 47(4):330–341. https://doi.org/10.1053/j.ro.2012.05.003
Bernstein MP, Baxter A (2012) Cervical spine trauma: pearls and pitfalls. Pitfalls in clinical imaging
Blackwood NJ III (1908) Atlo-occipital dislocation: a case of fracture of the atlas and axis, and forward dislocation of the occiput on the spinal column, life being maintained for thirty-four hours and forty minutes by artificial respiration, during which a laminectomy was performed upon the third cervical vertebra. Ann Surg 47:654–658
Bloom AI, Neeman Z, Slasky BS et al (1997) Fracture of the occipital condyles and associated cranio-cervical ligament injury: incidence, CT imaging and implications. Clin Radiol 52:198–202
Brotis AG, Paraskevi TM, Tsitsopoulos P et al (2015) An evidence-based approach towards the cranio-cervical junction injury classifications. Eur Spine J 24(5):931–939
Calvy TM, Segall HD, Gilles FH (1987) CT anatomy of the craniovertebral junction in infants and children. AJNR Am J Neuroradiol 8(3):489–494
Caroli E, Rocchi G, Orlando ER et al (2005) Occipital condyle fractures: report of five cases and literature review. Eur Spine J 14(5):487–492
Como JJ, Diaz JJ, Dunham CM, Chiu WC, Duane TM, Capella JM et al (2009) Practice management guidelines for identification of cervical spine injuries following trauma: update from eastern association for the surgery of trauma practice management guidelines committee. J Trauma 67(3):651–659
Diaz JJ Jr, Aulino JM, Collier B et al (2005) The early work-up for isolated ligamentous injury of the cervical spine: does computed tomography scan have a role? J Trauma 59:897–904
Fesmire FM, Luten RC (1989) The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med 7:133–142
Fine PR, Kuhemeir KV, DeVivo MJ et al (1979) Spinal cord injury: an epidemiologic perspective. Paraplegia 17:237–250
Frankel HL, Rozycki GS, Ochsner MG et al (1994) Indications of obtaining surveillance thoracic and lumbar spine radiographs. J Trauma 37:673–676
Garrett M, Consiglieri G, Kakarla UK et al (2010) Occipitoatlantal dislocation. Neurosurgery 66(3):48–55
Hadley MN (2002) Guidelines for management of acute cervical injuries, vol 50. Neurosurgery 50:S1–S6
Horn EM, Feiz-Erfan I, Lekovic GP et al (2007) Survivors of occipito-atlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine 6:113–120
Hu R, Mustard CA, Burns C (1996) Epidemiology of incident spinal fractures in a complete population. Spine 21:492–499
Jefferson RW, Harrop JS (2017) Update on upper cervical spine injury classifications. Semin Spine Surg 29(1):9–13
Joaquim AF, Alpesh A (2011) Cranio-cervical traumatic injuries: evaluation and surgical decision making. Global Spine J 1(1):37–42
Keller S, Bieck K, Karul M et al (2015) Lateralized odontoid in plain film radiography: sign of fractures? A comparison study with MDCT. Rofo 187(9):801–807
Kim SK, Shin JJ, Kim TH et al (2011) Clinical outcomes of halo-vest immobilization and surgical fusion of odontoid fractures. J Korean Neurosurg 50(1):17–22
Kohler A, Zimmer EA (1993) Shoulder girdle and thorax. In: Schmidt S, Freyschmidt J, Kohler A (eds) Borderlands of normal and early pathologic findings in skeletal radiology, 4th edn. Thieme Medial Publishers, New York, pp 234–245
Macalister A (1893) Notes on the development and variations of the atlas. J Anat Physiol. 27:519–542
Mead LB, Millhouse PW, Krystal J et al (2016) C1 fractures: a review of diagnoses, management options, and outcomes. Curr Rev Musculoskelet Med 9(3):255–262
Mendenhall SK, Sivaganesan A, Mistry A et al (2015) Traumatic atlanto-occipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a Level 1 trauma center over 15 years. Spine J 15:2385–2395
Menezes AH, Traynelis VC (2008) Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Childs Nerv Syst 24:1091–1100
Oppenlander ME, Clark JC, Sonntag VK et al (2014) Pediatric craniovertebral junction trauma. Adv Tech Stand Neurosurg 40:333–353
Parizel PM, van der Zijden T, Gaudino S et al (2010) Trauma of the spine and spinal cord: imaging strategies. Eur Spine J 19(1):8–17
Platzer P, Jaindl M, Thalhammer G et al (2007) Cervical spine injuries in pediatric patients. J Trauma 62:389–396
Riascos R, Bonfante E, Cotes C et al (2015) Imaging of atlanto-occipital and atlantoaxial traumatic injuries: what the radiologist needs to know. Radiographics 35(7):2121–2134
Romano F, Iacobellis F, Guida F et al (2017) Traumatic injuries: mechanisms of lesions. In: Diagnostic imaging in polytrauma patients. Springer, Cham, pp 35–50
Ryken TC, Aarabi B, Dhall SS et al (2013) Management of isolated fractures of the atlas in adults. Neurosurgery 72(2):127–131
Schueller G, Scaglione M, Linsenmaier U et al (2015a) The key role of the radiologist in the management of polytrauma patients: indications for MDCT imaging in emergency radiology. Radiol Med 120(7):641–654
Schueller G, Scaglione M, Linsenmaier U et al (2015b) The key role of the radiologist in the management of polytrauma patients: indications for MDCT imaging in emergency radiology. Radiol Med 120(7):641–654. https://doi.org/10.1007/s11547-015-0500-x
Scott EW, Haid RW Jr, Peace D (1990) Type I fractures of the odontoid process: implications for atlanto-occipital instability. Case report. J Neurosurg 72(3):488–492
Shin JJ, Kim SJ, Kim TH et al (2010) Optimal use of the halo-vest orthosis for upper cervical spine injuries. Yosei Med J 51(5):648–652
Stiell IG, Wells GA, Vandemheen KL et al (2001) The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 286:1841–1848
Sugimoto Y, Ito Y, Shiozaki Y, Shimokawa T, Mazaki T (2012) Motion induced artifact mimicking cervical dens fracture on the CT scan: a case report. Asian Spine J 6(3):216–218
Sundgren PC, Philipp M, Maly PV (2007) Spinal trauma. Neuroimaging Clin N Am 17:73–85
Sweet J, Ammerman J, Deshmukh V et al (2010) Cruciate paralysis secondary to traumatic atlanto-occipital dislocation. J Neurosurg Spine 12:19–21
Tins BJ, Cessar-Pullicino VN (2004) Imaging of acute cervical spine injuries: review and outlook. Clin Radiol 59:865–880
Traynelis VC, Marano GD, Dunker RO et al (1987) Traumatic atlanto-occipital dislocation. Case report. J Neurosurg 66(5):789
Tuli S, Tator CH, Fehlings MG (1997) Occipital condyle fractures. Neurosurgery 41:368–377
Wasserberg J, Bartlett RJ (1995) Occipital condyle fractures diagnosed by high-definition CT and coronal reconstructions. Neuroradiology 37:370–373
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sorbo, A. et al. (2022). Traumatic Emergent Injuries: Cranio-Cervical Junction. In: Scaglione, M., Çalli, C., Muto, M., Wirth, S. (eds) Emergency Radiology of the Head and Spine. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/978-3-030-91047-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-91047-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91046-4
Online ISBN: 978-3-030-91047-1
eBook Packages: MedicineMedicine (R0)