Abstract
Purpose
The cranio-cervical junction (CCJ) is an anatomically, functionally and biomechanically complex region. It is commonly involved in trauma of varying severity that can be managed with a multitude of treatment options and carry diverse prognosis. Our objective is to evaluate the quality of currently used CCJ injury classifications in an evidence-based approach.
Methods
We performed two consecutive literature reviews. In the first, we tried to find which classifications are currently used in CCJ injuries. In the second, we scrutinized the gathered classifications in terms of validity, reliability, severity grading, treatment guidance and prognosis assessment.
Results
Twenty classifications are currently used to describe the CCJ injuries and 72 individual injury patterns have been recognized. Almost a third of them can grade severity, guide treatment and assess prognosis. Only two classifications have been tested for validity and reliability.
Conclusions
CCJ injuries are poorly described by the current classifications according to evidence-based criteria. There is an obvious need for a simple and reliable classification tool to guide patient management in the evidence-based medicine era.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cranio-cervical junction (CCJ) is the transition from the head to the spine and it carries unique anatomical, biomechanical and functional properties. It is formed by three bony elements, the intervening joint capsules and numerous ligaments. The end-result is a magnificent interplay between motion and stability. The occipital condyles form the cranial end of the CCJ, and articulate with the atlas or C1 vertebra at the atlanto-occipital joint. The latter is mainly responsible for flexion and extension movements. Similarly, atlas meets the axis vertebra (C2) at the atlanto-axial joint. This joint is responsible for most of the CCJ rotation. In addition to the joint capsules, two sets of ligaments—the intrinsic and extrinsic—limit the range of motion, adding to the CCJ stability. The alar and transverse atlantal ligaments (TAL) are the main representatives of the former group [1–3] (Fig. 1).
Artistic illustration of the CCJ anatomy (from Debenardi et al. [3])
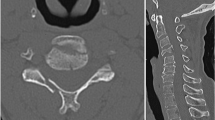
The CCJ integrity is severed when external forces are applied, as in trauma. The injury pattern depends on the size and vector of the applied moment, the site of force insertion, and the position of CCJ at the time of injury [4]. Theoretically, the number of potential injury patterns is unlimited. However, the injury patterns have been classified under common headings for simpler communication and patient management. The CCJ injury patterns and classification schemes should have specific properties. They should be valid and reliable, grade severity, help in patient management and predict outcome, as similar classifications used in other spine regions [5–7] (Fig. 2).
Injuries in the CCJ area involve a number of disciplines (neurosurgeons, orthopedics, radiologists, physiotherapists). Specialists are overflowed with guidelines and recommendations based on a diversity of classifications. To the best of our knowledge, there is no original article, meta-analysis or review to evaluate the quality of the classifications used in the injuries of the CCJ. The aim of the current paper is to find which CCJ injury classifications and injury patterns are most commonly used and to review their quality in terms of validity and reliability, severity assessment, treatment guidance and prognosis estimation.
Methodology
In the current study, we performed two consecutive literature reviews on CCJ injury classifications. In the first review, we sought in the Medical Literature for classifications and injury patterns that describe injuries in the CCJ. In the second literature review, we evaluated the quality of the gathered classification schemes and injury patterns in terms of terms of validity and reliability, severity assessment, treatment guidance and prognosis estimation.
Initially, AB and TP searched the databases of Medline, PubMed and Scopus for common classifications. The key terms of our search and the number of relevant results are depicted on Table 1. The main region of interest was the CCJ (occiput, C1, C2) injuries, either purely osseous or ligamentous. The articles were limited in human studies, more specifically in adults and written in English. There were no temporal limitations (1966–September 2014). The reviewers were blinded to the authors of the articles and evaluated them in terms of relevance. Additional relevant articles were extracted from the references of the initial full texts. Duplicate studies were eliminated. Then, the full text of the remaining articles was studied to gather all classifications and injury schemes that described the CCJ injuries.
The gathered classifications and injury patterns formed the substrate for the second literature review by AB and PT (Tables 2, 3, 4, 5, 6, 7). Less common classifications (in <5 studies) were eliminated from the literature review, as they are not practically in common use. In the same search engines as above, Medline, PubMed and Scopus, the reviewers used as key terms the name of the classification and each of the words “validity and reliability”, “severity grading”, “treatment” or “surgery”, “prognosis” or “outcome”. The data were registered on tables for each CCJ subregion (occipital condyles, occipito-atlantal junction, atlas, TAL, atlanto-axial junction, axis). The gathered classifications were presented on the rows of the tables and the quality properties on the columns. The collected data were recorder as “Yes” if the classification under investigation was characterized by the quality parameter, and “No” if it was not. Again, the search was limited in studies written in English, and performed in adult humans. Tables 2, 3, 4, 5, 6, 7 highlight the gathered classifications and their quality properties. No statistical tests of any kind were performed in the current study.
Results
The first literature review (Fig. 1) resulted in 449 abstracts. Four articles were excluded, as they were common in more than one keyword list. From the remaining 445 abstracts that were pooled for review, 23 abstracts addressed other disease entities. Finally, only 20 articles from the remaining 422 articles that were selected for our study, presented a novel classification scale. More than half of the articles (239) were reporting on C2 isolated injuries. The least articles involved the TAL (Table 1).
There were 20 widely used classifications and 72 injury patterns for the description of injuries of the CCJ (Table 1). No classification scheme has been excluded from the study as all of them have been used in more than five studies. Again, most of the classifications and injury patterns describe C2 injuries, 9 and 33, respectively. Two classifications were used for occipital condyle fracture (OCF) description; two for occipito-atlantal dissociations (OAD); four for atlas fractures; one for TAL rupture; two for atlanto-axial dislocation (AAD); four for odontoid fractures; three for axis pars fractures; and two for C2 vertebral body fractures.
In the second literature review (Tables 1, 2, 3, 4, 5, 6, 7), only 2/20 classifications were tested for validity and reliability, and were focused on odontoid fractures. 6/20 classifications permitted injury severity grading. Less than half of them (9/20) could guide patient management and only a third (6/20) assisted in prognosis estimation. The only classifications that fulfilled all the quality characteristics set at our study were describing the odontoid fractures. Thus, the Medical Literature poorly describes the CCJ injuries, as 0/18 classifications (except for the odontoid fractures) do not match the preset criteria.
Discussion
Occipital condyle fractures
OCFs have initially been described by Bell in 1817 and are rare entities [8, 9]. Nowadays, their severity is graded in an ordinal fashion by the two most commonly employed classifications. Anderson and Montesano [10] reported that OCFs could be classified according to the fracture morphology in three types. Type I fractures include comminuted OCFs, Type II represent linear skull base fractures that extend to the occipital condyle, and Type III are OCFs with an avulsed fragment. The latter are potentially unstable. This classification does not guide treatment according to the current recommendations, nor predict prognosis [9] (Table 2). Tuli et al. [11] described another OCF classification based on the instability of the entire CCJ. According to the latter classification, Type 1 fractures include un-displaced OCFs that are stable. Type 2A fractures are displaced OCF with proven radiological stability at the CCJ. Finally, Type 2B fractures are displaced OCF with unstable CCJ. Tuli’s classification [9] is more compatible with the current treatment recommendations. The latter suggest external cervical immobilization for all isolated unilateral OCFs and halo-vest stabilization for bilateral ones. In addition, halo-vest immobilization or CCJ fusion is recommended for OCFs associated with other unstable CCJ injuries. Mueller et al. [12] revealed that isolated OCFs carry a good prognosis in contrast to others with simultaneous AOD present a worse prognosis. Neither classification has been tested for validity or reliability, yet (Table 1).
Occipito-atlantal dissociations
OADs represent a spectrum of often fatal injuries between the head and the atlas [13]. The most common classification used to describe the OADs is the one presented by Traynelis et al. [14] in 1986 according to the injury morphology. Type I OADs include anterior dislocations of the occiput in comparison to the atlas vertebra. Similarly, Type II and Type III OADs represent longitudinal and posterior dislocations, respectively. The injury patterns in this classification are nominal categories and do not grade severity. Alternatively, the Harborview atlanto-occipital dislocation classification by Chapman et al. [15] grade OADs in 3 stages: stage 1 (incomplete OAD), stage 2 (occult OAD, partially reduced injury due to “rebound phenomenon”), and stage 3 (obvious OAD with >2 mm diastasis). Irrespective of the classification and the grading system used, the recommended treatment is CCJ fusion. In addition, no OAD classification scale has ever been validated or tested for reliability and neither classification guides treatment nor predict patient outcome (Table 3).
Atlas fractures
Acute isolated atlas (C1) fractures with intact transverse ligament are rare, representing 1–2 % of the spinal column fractures [16]. Jefferson [17] in 1920 described 4 types of atlas fractures: Type 1 (fractures involve the posterior arch only), Type 2 (anterior arch only), Type 3 (both arches are involved) and Type 4 (lateral mass fracture). Similarly, Gehweiler [18] in 1976 proposed a five-tired classification of the C1 vertebra: Type I (fracture of the anterior arch), Type II (fracture of the posterior arch), Type III (combination fractures of anterior and posterior aches), Type IV (lateral mass fractures, and Type V (fracture of the transverse process). Landels and Van Peteghem [19] in 1988 reduced the injury patterns in three: Type I fractures (involving a single arch), Type II (fractures involving both anterior and posterior arches) and Type III (representing lateral mass fractures). Levin and Edwards [20] in 1991 classified C1 fractures in the following five groups: posterior arch fracture, burst fracture, anterior arch fracture, transverse process fracture and lateral mass fracture. No classification scheme from the above has been tested for validity and reliability and none guides treatment or prognosis (Table 4). According to the latest recommendations, the treatment of isolated C1 vertebra is independent from the specific injury pattern [16]. A cervical spine immobilization mode alone, either with a hard cervical collar or a halo-vest, is sufficient. The co-existence of a simultaneous TAL rupture or a long-term local instability requires cranio-cervical fixation [16].
Transverse atlantal ligament injury
TAL injury can either be suspected from a lateral mass displacement >7 mm on antero-posterior cervical spine radiographs or directly visible on a high-resolution MRI [20, 21]. Dickman et al. in 1996 classified the TAL injuries into two injury patterns [21]. The first one included disruptions of the ligament per se and was named as Type I injuries. The authors reported that these injuries could not heal well without early internal fixation. The second pattern, Type II TAL injury, was characterized by avulsion or fracture of the TAL tubercle from C1. The surgeons recommended expectant treatment with cervical orthosis for the latter injury, and only if instability persisted beyond 3–4 months, then they suggested delayed operative intervention. They are further subclassified into Subtype IIa (with simultaneous lateral mass fracture) and Subtype IIb (tubercle avulsion) [21]. Dickman’s classification, despite the fact that it is not validated or tested for validity, governs treatment of atlas injuries, as stated above [16]. It has no prognostic value (Table 5).
Injury of the atlanto-axial joint
Atlanto-axial rotatory fixation (AARF) is nosological entity that occurs most commonly in children but it is not limited to this age group. In addition, its etiology is not always traumatic. However, the authors decided to include it for completeness sake. The most common classification of atlanto-axial rotatory fixation (AARF) is that proposed by Fielding and Hawkins [23] in 1977. It has never been tested for validity or reliability. The authors described four ordinal groups: Type I (pivotal rotation around dens and no C1-to-C2 displacement), Type II (rotation around the lateral process, with anterior C1-to-C2 displacement 3–5 mm), Type III (rotation with anterior C1-to-C2 displacement >5 mm), and Type IV (rotator fixation with posterior displacement). However, there are increasing reports that doubt if the Fielding and Hawkins classification is sufficient in the computerized tomography (CT) and magnetic resonance imaging (MRI) era [24]. Recently, Pang and Li proposed a Fielding Type I subclassification based on dynamic CT imaging and the concept of “pathological stickiness”. In subtype I, there is no rotation between C1 and C2 in dynamic CTs. In subtype II, the C1–C2 rotation will decay but never reach normality. Last but not least, in subgroup III, the C1–C2 angle will reduce to zero, only if the head is rotated more than 20° to the contralateral side [25]. However, the treatment is irrelevant of Fielding and Pang and Li classifications. Traction with adjuvant muscle relaxants and analgesics are necessary in an effort to reduce C1–C2 fixation as soon as diagnosis is set. If reduction is achieved, the patient is changed to a rigid cervical orthosis. If not, then open surgical reduction and stabilization are mandatory [26, 27]. Time is an independent prognostic factor of outcome and recurrence that no AARF classification takes into account [26, 27]. Furthermore, neither scale has been validated.
C2 fractures
Odontoid fractures have traditionally been classified according to Anderson’s and D’Alonzo’s anatomical classification into three categories: Type I, apical dens fracture; Type II, fracture through the base of the dens; and Type III, with the fracture line into the C2 body [28]. Type II Anderson’s and D’Alonzo’s odontoid fractures have been further subclassified by Roy–Camille according to the inclination of the fracture line into subtype 1 (forward), subtype 2 (backwards), subtype 3 (horizontal) and subtype 4 (fracture with rotation or English policeman’s hat) [29]. In 1988, Hadley et al. [30] added in Anderson’s and D’Alonzo classification a highly unstable fracture pattern with comminution of the odontoid base, Type IIA. In 1979, Althoff [31] presented another anatomic classification in which four fracture types could be recognized. In Type A and Type B fractures, the fracture line passes through the neck of the odontoid and the rostral part of the axis, respectively. In Type C fractures, the fracture line crosses the axis body and one articular facet. Type D fractures involve both superior articular facets. Finally, Grauer et al. [32] proposed a “treatment-oriented classification” of odontoid fractures, in 2005. This classification is morphological and distinguishes the following types: Type I fractures (fracture line above the C1 arch), Type II (caudal to the C1 arch), Type III (like Type II with extension to the facets). The authors further subclassified Type II fractures according to the direction of the fracture line, displacement and comminution in Type IIA (non-displaced, non-comminuted fractures), Type IIB (displaced and transverse fractures), and Type IIC (fracture line from antero-inferior to supero-posterior or with significant comminution) [32].
Francis et al. [33] in 1981 classified Hangman’s in five injury patterns of escalated severity: the displacement of C2 over C3, the angulation of the C2 over C3, and the status of the C2–C3 intervertebral disc. In about the same period, Effendi et al. [34] classified axis pars fractures according to the mechanism of injury into three categories. Axial loading and hyperextension are usually associated with isolated hairline fractures and no displacement of the C2 body (Effendi Type I fractures). Hyperextension and rebound flexion usually result in the displacement of the anterior segment and C2–C3 disc disruption (Effendi Type II fractures). A primary flexion and rebound hyperextension end-up in pars fractures with angulated anterior segment and C2–C3 facet dislocation (Effendi Type III fractures) [34]. Four years later, Levine and Edwards [35] refined the definitions of Effendi’s each group and added two mechanisms of stress loading. Hyperextension and lateral bending are usually causing non-parallel bilateral pars fractures without significant displacement or angulation (Levin and Edwards Type IA or “atypical” pars fractures). Finally, a flexion–distraction injury mechanism usually results in severe angulation of the anterior fragment without displacement (Levine and Edwards Type IIA fracture) [35]. The updated treatment recommendations for pars fractures advocate surgery for (a) displaced fractures, (b) angulated fractures, (c) fractures with C2–C3 disc disruption and (d) fractures where normal alignment cannot be achieved with external immobilization. Traction is strictly prohibited for Type IIA fractures. For all other cases, external reduction and immobilization is considered as the initial treatment mode [36]. All above-mentioned classifications can be used to accurately select the surgical candidates and are useful for prognosis assessment. No scale regarding the atlas pars fractures up to date has been tested for validity and reliability regarding the atlas pars fractures (Table 7).
The term “miscellaneous C2 fractures” was initially used by Hadley et al. [37] to describe all non-odontoid, non-Hangman’s fractures. Fractures of the C2 body, lateral mass, laminae, pedicles, spinous processes are all covered under this “umbrella” term. According to Benzel et al. [38], C2 body fractures are classified as Type I (coronal), Type II (sagittal), and Type III (transverse) based on the fracture line plane. In 1996 Fujimura et al. [39] described a four-scale classification of the axis bony injuries: Type I, avulsion fractures at the antero-inferior vertebral body margin; Type II, transverse fractures; Type III, burst fractures; and Type IV, sagittal plane fractures. No classification provides with a severity scale or a prognostic basis (Table 7). Immobilization is a broadly accepted treatment mode for these clinical entities, irrespective of the classification used and the assigned grouping [36].
Limitations of the study
The authors recognize the existence of important limitations in the current study. Three of them are related to methodological issues. The literature review was limited to the English language. There could exist CCJ injury classifications in other languages as well, that could be potentially very useful. Moreover, there could exist CCJ injury classifications that are not popular (in less than five studies), but still be potentially very useful in our daily hospital practice. Unfortunately, we could not find any evidence-based medicine compatible remedy to this issue. Probably, a qualitative study would dig for all potential classifications, which is far beyond our scope. Another methodological limitation of the current study is that CCJ injury classification preference is indirectly deduced from the published literature rather from direct questioning those related to the management of these injuries. In other words, there might be difference between the classification a spine surgeon uses to treat his patients and the classification that he reports his results in the literature.
Future perspectives
From the above, it becomes obvious that there is a strong need for the adoption of a universally acceptable working classification instrument regarding the CCJ injuries. Such tools exist in classifying injuries of the subaxial cervical spine and of the thoracic and lumbar region. In these cases, some widely respected bodies, such as the Arbeitsgemeinschaft für Osteosynthesefragen (AO) Study Group or the Spine Trauma Study Group, developed and validated their classifications, AO, SLICS and TLICS, respectively [40–42]. Nowadays, the penetrance and acceptance of these classifications is very high within those involved in spine trauma care, despite the fact that they are still evolving. Similarly, a Central Body respected by the international community should either test for reliability and validity an already existing classification instrument or develop and establish a new one from the beginning. In the optimal case, a single spine trauma classification would describe all spinal injuries from the occipital condyles to the sacrum, but a few CCJ injury classifications would be just as good for the moment. Towards this aim a centralized registry would be of help because out-of-date regional patterns of CCJ classification would vanish. Moreover, with a centralized spine trauma registry, rare injury patterns would not be anymore so rare to the scientific community. Furthermore, the gathered knowledge on natural history, treatment and prognosis would assist future trauma patient management. It is worth noting that neither the AO Study Group nor the Spine Trauma Study Group have dealt with the classifications of the CCJ injuries. Finally, the authors understand that a single review article, such as ours, is not enough to change an old-fashioned, long-held scientific community attitude. However, we dare to reveal a feeling of heterogeneity and complexity in CCJ injuries classifications with EBM terms. It is also worth including the neurological status of the patient within the CCJ injury classification to add some prognosis to the information gained from the scale [41, 42]. Furthermore, there is lack of a uniform approach to the CCJ injuries and limited number of validated studies. And let’s be frank; 72 injury patterns for the CCJ challenge both our ability to learn them and reproduce them in the daily hospital praxis.
Conclusion
The CCJ injuries are poorly described by the current classification and injury patterns. There is vital need for restructuring the scientific basis over these injuries so as to gain the maximum information out of a minimal number of injury patterns.
Abbreviations
- CCJ:
-
Cranio-cervical junction
- TAL:
-
Transverse atlantal ligament
- OCF:
-
Occipital condyle fracture
- OAD:
-
Occipito-atlantal dissociation
- AAD:
-
Atlanto-axial dislocation
- AARF:
-
Atlanto-axial rotatory fixation
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- EBM:
-
Evidence-based medicine
- STSG:
-
Spine Trauma Study Group
- SLICS:
-
Subaxial cervical spine injury classification system
- TLICS:
-
Thoracolumbar injury classification scale
References
Tubbs RS, Hallock JD, Radcliff V, Naftel RP, Mortazavi M, Shoja MM, Loukas M, Cohen-Gadol AA (2011) Ligaments of the craniocervical junction. J Neurosurg Spine 6:697–709
Menezes AH, Traynelis VC (2008) Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Childs Nerv Syst 24:1091–1100
Debernardi A, D’Aliberti G, Talamonti G, Villa F, Piparo M, Collice M (2011) The craniovertebral junction area and the role of the ligaments and membranes. Neurosurgery 68:291–301
Smorgick Y, Fischgrund JS (2013) Occipitocervical injuries. Semin Spine Surg 25:14–22
Mirza SK, Mirza AJ, Chapman JR, Anderson PA (2002) Classifications of thoracic and lumbar fractures: rationale and supporting data. J Am Acad Orthop Surg 10:364–377
Sethi MK, Schoenfeld AJ, Bono CM, Harris MB (2009) The evolution of thoracolumbar injury classification systems. Spine J 9:780–788
van Middendorp JJ, Audigé L, Hanson B, Chapman JR, Hosman AJ (2010) What should an ideal spinal injury classification system consist of? A methodological review and conceptual proposal for future classifications. Eur Spine J 19:1238–1249
Bell C (1817) Surgical observations. Middx Hosp J 4:469–470
Theodore N, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Ryken TC, Walters BC, Hadley MN (2013) Occipital condyle fractures. Neurosurgery 72(Suppl 2):106–113
Anderson PA, Montesano PX (1988) Morphology and treatment of occipital condyle fractures. Spine 13:731–736
Tuli S, Tator CH, Fehlings MG, Mackay M (1997) Occipital condyle fractures. Neurosurgery 41:368–377
Mueller FJ, Fuechtmeier B, Kinner B, Rosskopf M, Neumann C, Nerlich M, Englert C (2012) Occipital condyle fractures. Prospective follow-up of 31 cases within 5 years at a level-1 trauma centre. Eur Spine J 21:289–294
Theodore N, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Ryken TC, Walters BC, Hadley MN (2013) The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery 72(Suppl 2):114–126
Traynelis VC, Marano GD, Dunker RO, Kaufman HH (1986) Traumatic atlanto-occipital dislocation. Case report. J Neurosurg 65:863–870
Chapman JR, Bellabarba C, Newell DW (2001) Craniocervical injuries: atlanto-occipital dissociation and occipital condyle fractures. Semin Spine Surg 13:90–105
Ryken TC, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, Theodore N, Walters BC, Hadley MN (2013) Management of isolated fractures of the atlas in adults. Neurosurgery 72(Suppl 2):127–131
Jefferson G (1920) Fracture of the atlas vertebra: report of four cases, and a review of those previously recorded. Br J Surg 7:407–422
Gehweiler JA, Denise E, Duff DE, Martinez SS, Miller MD, William M, Clark WM (1976) Fractures of the atlas vertebra. Skelet Radiol 1:97–102
Landells CD, Van Peteghem PK (1988) Fractures of the atlas: classification, treatment and morbidity. Spine 13:450–452
Levine AM, Edwards CC (1991) Fractures of the atlas. J Bone Joint Surg (Am) 73:680–691
Spence KF Jr, Decker S, Sell KW (1970) Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg (Am) 52:543–549
Dickman CA, Mamourian A, Sonntag VKH, Drayer BP (1991) Magnetic resonance imaging of the transverse atlantal ligament for the evaluation of atlantoaxial instability. J Neurosurg 75:221–227
Fielding WJ, Hawkins RJ (1977) Atlanto-axial rotatory fixation (fixed rotatory subluxation of the atlantoaxial joint). J Bone Joint Surg (Am) 59:37–44
Tahsin E, Yurdal G (2013) Is the fielding classification system enough for managing atlantoaxial rotatory dislocation? Neurosurg Quart 23:145–147
Pang D, Li V (2005) Atlantoaxial rotatory fixation: part 2. New diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurgery 57:941–953
Pang D, Li V (2005) Atlantoaxial rotatory fixation: part 3. A prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation. Neurosurgery 57:954–972
Pang D (2010) Atlantoaxial rotatory fixation. Neurosurgery 66:161–183
Anderson LD, D’Alonzo RT (1988) Fractures of the odontoid process of the axis. J Bone Joint Surg (Am) 56:1663–1674
Roy-Camille R, Saillant G, Judet T, De Botton G, Michel G (1980) Factors of severity in the fractures of the odontoid process. Rev Chir Orthop Reparatrice Appar Mot 66:183–186
Hadley MN, Browner CM, Liu SS, Sonntag VK (1988) New subtype of acute odontoid fractures (Type IIA). Neurosurgery 22:67–71
Althoff B (1979) Fracture of the odontoid process. An experimental and clinical study. Acta Orthop Scand Suppl 177:1–95
Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, Albert TJ, Fehlings MG, Vaccaro AR (2005) Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J 5:123–129
Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R (1981) Traumatic spondylolisthesis of the axis. J Bone Joint Surg (Br) 63:313–318
Effendi B, RoyD Cornish B, Dussault RG, Laurin CA (1981) Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg (Br) 63:319–327
Levine AM, Edwards CC (1985) The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg (Am) 67:217–226
Pryputniewicz DM, Hadley MN (2010) Axis fractures. Neurosurgery 66:68–82
Hadley MN, Dickman CA, Browner CM, Sonntag VK (1989) Acute axis fractures: a review of 229 cases. J Neurosurg 71:642–647
Benzel EC, Hart BL, Ball PA, Baldwin NG, Orrison WW, Espinosa M (1994) Fractures of the C2 vertebral body. J Neurosurg 81:206–212
Fujimura Y, Nishi Y, Kobayashi K (1996) Classification and treatment of axis body fractures. J Orthop Trauma 10:536–540
Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai LY, Oner FC (2013) AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J 22:2184–2201
Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Oner FC, Aarabi B, Vaccaro AR (2007) The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine 32:2620–2629
Lee JY, Vaccaro AR, Lim MR, Oner FC, Hulbert RJ, Hedlund R, Fehlings MG, Arnold P, Harrop J, Bono CM, Anderson PA, Anderson DG, Harris MB, Brown AK, Stock GH, Baron EM (2005) Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci 10:671–675
Conflict of interest
No funds of any kind have been taken.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brotis, A.G., Paraskevi, T.M., Tsitsopoulos, P. et al. An evidence-based approach towards the cranio-cervical junction injury classifications. Eur Spine J 24, 931–939 (2015). https://doi.org/10.1007/s00586-015-3877-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3877-2