Abstract
The percutaneous invasion of microorganisms through damaged skin layers can lead to the onset of infections with potentially life-threatening complications, especially in vulnerable populations like newborns, elderly, and diabetic patients. With the emergence of superbugs that are resistant to almost all the available antibiotics and the unfruitful discovery of new antimicrobial compounds in the last few decades, there is a demand for novel engineering strategies to approach skin and soft tissue infections associated with the used of biomaterials. Naturally occurring anti-biofouling and antimicrobial interfaces based on spatial structure offer an unprecedented opportunity for biomaterial design, as they do not contribute to bacterial resistance, do not pollute the environment, and can be easily implemented in a variety of biomaterial interfaces. In this article, we review the complications caused by biomaterials in contact with the skin, especially those that compromise medical adhesives, sutures, and wound dressing materials. Then, we introduced bioinspired designs that can be implemented in those materials based on nano- and microscale topographies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Skin microbiome
- Skin and soft tissue infections
- Bioinspired
- Biofilms
- Bactericidal nanostructures
- Microtopography
- Nanotopography
- Nanofabrication
- Medical adhesives
- Bandages
- Tapes
- Sutures
- Wound dressing
Introduction
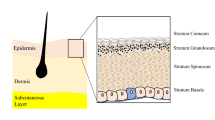
The skin is the largest organ in the human body and serves several functions including thermoregulation, sensation, maintenance of internal homeostasis, and protection against harsh environmental aggressors, such as harmful substances or pathogens [1]. The skin hosts numerous species of fungus, viruses, and about 1000 different species of bacteria, that constitute together the skin microbiome. The distribution and composition of these microbial flora is driven by many factors, including the skin topography (e.g., thickness and density of glands and hair follicles), the host physiology (e.g., age and sex), the environment (e.g., climate), and the immune system [1, 2]. Those factors together affect the type of microorganisms that can colonize the epithelial surface, which can further act competitively to exclude one another or synergistically for mutual benefit [3]. For example, commensal strains such as Staphylococcus epidermidis have been shown to cooperate with the host’s immune system to prevent the colonization of invasive microorganisms, ultimately reinforcing the epithelial barrier function [4]. It is now widely accepted that a broad community of protective bacteria normally habits the healthy skin and provides a host defense against pathogens. Indeed, alterations in the microbiome composition have been associated with the delay in the healing process of cutaneous injuries and the onset of some disease states [5].
The skin barrier can be disrupted because of cutaneous puncturing during routine medical procedures (e.g., the insertion of invasive devices like intravenous catheters), in chronic wounds like burns and other cutaneous lesions. It can also be broken as a consequence of an imbalance between commensal and invasive microbes in diseases such as atopic dermatitis. Similarly, continuous skin stripping associated with the removal of dressing materials and adhesives can also affect the epithelial layers beneath the biomaterial, particularly in chronically ill patients and vulnerable groups like newborns and elderly, where the skin is immature and susceptible to trauma [6]. The percutaneous invasion of microorganisms through damaged skin layers especially in diabetic, immunocompromised, and vulnerable populations, can lead to the onset of infections with potentially life-threatening complications, including bacterial dissemination to other body sites and bacteremia [7]. A retrospective study performed in California between 2005 and 2011 for patients with a primary diagnosis of skin and soft tissue infections (SSTIs) found that in both ambulatory and health care settings the incidence of SSTIs were almost twice that of urinary tract infections and tenfold of that of pneumonia [8]. SSTIs are commonly associated with exudates, ulcerations, fluid collection, or abscesses; whereas the bacterial strains often isolated from complicated SSTIs include Staphylococcus aureus, Pseudomonas aeruginosa, Enterococcus spp., Escherichia coli, and other Enterobacteriaceae [9, 10]. In chronic wounds, for example, the nutritional composition of the wound exudate is ideal for the growth of bacteria (e.g., S. aureus), yeast (e.g., Candida albicans), and fungus (e.g., Tinea species) [7, 11]. Moreover, foreign materials brought into contact with broken epithelial layers can further exacerbate the foci of infection, because the material’s surface can serve as a substrate and shelter for bacterial colonization and growth [7]. The likelihood of skin erosion and inflammation can also be increased by occlusive adhesive materials, which can trap moisture and contribute to fungal and bacterial proliferation [12].
A key issue in the treatment of skin infections and restoration of skin integrity is the presence of bacterial biofilms [10]. Biofilms are microbial communities encased by an extracellular polymeric substance that provide microbes with increased resistance to harsh environments such as a high concentration of antibiotics and desiccation. Biofilms challenge the treatment of wound infections either by conventional administration of antibiotics or by topic application of antimicrobial ointments and are one of the significant causes of the emergence and dissemination of antibiotic-resistant strains. Indeed, the spread of multidrug-resistant organisms have increased over the past 50 years, and there is little evidence that bacterial resistance to antibiotics will go away [13, 14]. Multidrug-resistant pathogens not only threaten our ability to control infections with antibiotics, but also lead to clinical and economic adverse outcomes, encompassing treatment failure with potential patient death, and increased health care costs linked to disease management, respectively [13]. In the context of skin infections associated with the use of biomaterials, conventional treatments rely on platforms that elude antibiotics, nanoparticles (NPs), or biocides agents at the infected site. Clinical treatments usually lack specificity against the infection-causing microorganisms, and thus, eradicating commensal bacteria that is necessary for the fitness of the skin, and contributing to the selection of increasingly resistant strains. Among the antimicrobial agents, NPs have gained attention due to their easy fabrication and broad-spectrum activity; however, the long-term effects associated with the use of NPs in human health and the environment remain to be seen. Preliminary reports have indicated that NPs can travel and gain access to organ systems and affect the biological function at the tissue, cellular, subcellular, and proteins levels [15].
In the last few decades, due to the emergence of superbugs that are resistant to almost all of the available antibiotics and the unfruitful discovery of new antimicrobial compounds [14], have led to the search of novel engineering strategies to treat skin and soft tissue infections. From the material science perspective, naturally occurring anti-biofouling and antimicrobial interfaces as well as the dynamic interactions between microbial communities and their niches, offer inspiration for the design of material interfaces that can target pathogenic bacteria while protecting the beneficial microbiome of the skin. Bioinspired anti-biofouling interfaces compromise physical and chemical barriers, and the symbiotic interactions between microbe–host and microbe–microbe (Fig. 1). Physical barriers consist of the natural components of the immune system capable of disrupting biofilm formation, killing bacteria by contact, or preventing the adhesion of microbes to the underlying surface by physical means. On the contrary, chemical barriers endure antimicrobial agents including Q-sensing quenchers, peptides, and enzymes, which are secreted by the host. A better understanding of the ecological interactions between microorganisms and their niches (e.g., abiotic surfaces, host, and interactions between microbes) can also lead to the discovery of new routes to treat lesions on the skin caused by pathogenic microorganisms.
Bioinspired anti-biofouling interfaces can be divided into three main subcategories: physical and chemical barriers and symbiotic interactions. (i) Physical barriers are commonly found in the skin of animals, insects, and plants in the form of micro and nanoscale structures, as well as viscous mucus layers covering the epithelium. (ii) Chemical barriers compromise antimicrobial compounds excreted by the host. (iii) Symbiotic interactions favor the retention of favorable bacteria in the niche while limiting the resources available for pathogenic microbes
The advantage of physical barriers over chemical ones is that the former does not contribute to bacterial resistance, do not pollute the environment, and can be easily implemented in a variety of materials of clinical importance. In many ecological niches, physical and chemical barriers and symbiotic associations exist together as the first aid of defense against invasive pathogens. One example of this is the structure and composition of the mucus layer that covers mucosal tissues like the gastrointestinal, respiratory, reproductive, and urinary tracts. Mucin glycoproteins, the major constituent of the mucus layer, are responsible for the viscous and gel-like appearance of the mucus layer, which serves as a reservoir for a variety of antimicrobial molecules produced by the host [16]. The viscosity of the mucus glycoproteins has been implicated in preventing the adhesion of the bacteria to the underlying epithelium by promoting the motility in their planktonic state and inhibiting their aggregation into biofilms [17]. Similarly, the array of microbial agents embedded in the mucus layer favor the retention of commensal bacteria, while limiting the niche available for invasive microorganisms [16].
In this chapter, the state of the art on skin infections associated with the use of medical adhesives, sutures and wound dressing materials are briefly introduced. Bioinspired strategies based on antimicrobial and anti-biofouling topographies that can be implemented on those materials is critically reviewed here. Whenever possible, we place emphasis on anti-biofouling and antimicrobial properties of physical barriers found in the innate immune system of animals, insects, or plants.
Skin Lesions Associated with Biomaterials in Contact with the Skin
Medical Adhesives and Surgical Sutures
In recent years, tremendous advances have been taking place in the design of health monitoring and wearable medical devices that incorporate flexible and lightweight polymeric substrates. Those can conform to the surface of the skin while providing a noise-free, sensitive, and accurate monitoring of body signals such as temperature, heart rate, respiration rate, and blood pressure [18]. Medical adhesives are one integral part of such diagnostic devices and exist in the form of patches, bandages, or tapes that are used to fix to the skin electrodes and sensors for noninvasive monitoring of vital signals. Medical adhesives are also used to fix intravenous catheters and other dwelling devices. While a variety of fabrication techniques and materials have been investigated to provide a strong adhesion and noise-free signal at the interface between skin/material [19], there is a lack of studies focusing on strategies that mitigate medical adhesive-related skin injuries. Those lesions include the removal of superficial epithelial layers and undesirable growth of microorganisms underneath medical adhesives (e.g., fungus and bacteria), which are common complications that negatively affect vulnerable populations such as newborns, elderly, and critically ill patients, and that are often referred to as “forgotten wounds” [6, 20]. For example, conventional tapes applied to secure intravenous access have been reported to traumatize the skin and favor the colonization of Aspergillus Fumigatus conidia in immunocompromised infants, causing acute fungal infections [21]. Similarly, the application of skin protectants (such as Stomadhesive®) was implicated in a 5-year outbreak of S. aureus in a neonatal unit in the UK. In this study, in vitro Staphylococcal desiccation experiments indicated that the hydrated niche provided by Stomadhesive® on the skin plus the high content of sweat and other secretions absorbed by the material prevented bacterial desiccation and allowed the survival of S. aureus for up to 71 days [22]. In another study performed in patients aged 65 or older for 8 weeks, results indicated that the application of medical adhesive tapes resulted in contact dermatitis in 70.6 % of the cases, while trauma and infection had an incidence of the 20.6% and 8.8%, respectively. Because skin injuries in elderly groups take longer to heal, secondary infections have the potential to develop as a complication [23].
In neonate health care settings, skin lesions promoted by medical adhesives and other materials are well documented and include contact dermatitis, disruption of the epithelial layers as result of adhesive removal and skin infections (Fig. 2) [24, 25]. Moreover, it has been reported that neonates are at a higher risk of percutaneous invasion of microbes through broken skin layers, especially when they are kept inside incubators, which offer a moist and warm habitat for microbial growth and survival. The consequences of infection in neonates include secondary infections, additional days of hospitalization, increased risk of mortality, and a higher prevalence of a poor neurodevelopmental outcome [25, 26].
Contact dermatitis caused by medical adhesives in two infants. (A) Contact dermatitis reaction caused by transparent adhesive dressing, (B) hydrogel in EKG electrodes. (Image source: [27])
Besides the fixation of biomedical devices to the skin, medical adhesives can also be used for wound closure; however, in some scenarios, the medical adhesive does not support the required strength to facilitate wound closure. In this case, the surgical incision may require the use of sutures (for internal skin layers) or the combination with medical adhesives to ensure proper wound healing. Sutures are stranded materials used to join tissue edges and help in the closure and healing process of broad and deep wound incisions, as well as subcuticular openings [28, 29]. The use of linen as a suture material date more than 4000 years ago [30], along with a variety of other types of materials including silver, gold, iron, silk, cotton, steel wires, and even animal gut and hair [31]. It is estimated that about 234 million surgical operations are performed worldwide every year including surgical incisions, which requires the use of sutures. However, sutures are commonly associated with surgical site infections (SSI). The prevalence of SSI is around 5% and are responsible for increased patient morbidity, secondary infections, and more extended days in the hospital [32, 33]. According to the American Medical Association, between 2006 and 2009, 1.9% of surgical procedures were complicated by SSI in the USA alone [34]. In 2005 and 2002, the estimated cost of SSI was calculated in $10,443 to $25,546 US dollars each year, respectively. Indeed, this cost was superior when resistant microorganisms to antibiotics were present at the incision site, or if prosthetic joint implants were involved [35].
SSI has been classified into three different categories: superficial incisional, deep incisional, and intracavitary. Depending on the type of SSI, various procedures may be used to solve or reduce the infection such as reopening, draining, adjuvant antibiotic treatment, or even a new surgical intervention [36]. It has been suggested that an ideal suture should accomplish multiple requirements: suitable bending strength and mechanical properties, easy sterilization and manipulation, good tissue biocompatibility (lack of allergies, nontoxic leakages, noncarcinogenic), and proper biodegradability. Moreover, suture materials should avoid the adhesion of bacteria to reduce the risk of infections and skin complications [29]. To prevent bacterial infections, two main strategies have been performed on suture materials: (1) the use of cationic polymers that modify the surface chemistry, called passive coatings, and (2) the functionalization with drugs and molecules, which are released from the suture. However, surface modification by introducing micro- or nanotopography features has received increased attention because several studies have reported that nano- and microscale topographies can impair bacterial attachment [37].
Wound Dressing Materials
In the USA alone, chronic wounds are estimated to affect 1–2% of the whole population, estimated at about 25 billion dollars per year [38, 39]. The physical barrier and sensory system of the skin’s functional control includes a limiting capability to prevent microbial infections and cellular regeneration. An abrasion to the skin due to physical or chemical means, rupturing the epidermis, is defined as a wound. For the structure and sensory functions to be regained, a novel wound dressing, “artificial skin,” should provide a barrier to the external environment ultimately leading to accelerated tissue regeneration that in parallel limits bacterial infections. Initially, the first stage of infection is dominated by Gram-positive organisms (S. aureus, Streptococcus pyogenes); however, as the wound progresses, Gram-negative bacteria (E. coli, P. aeruginosa ) are found when the wound becomes chronic [40]. The skin’s physical barrier protects from the external stimuli by activating the natural immunity system. After an abrasion to the skin, the migration of microbial organisms compromises the body’s natural self-defense system, limiting the function of the fibroblasts and collagen production. The tissue scaffold from the previous wound area begins to form about 3 days after the initial wound due to fibroblasts and production of collagen and ground substance [41]. Despite the advancements and progress in wound dressing applications, current dressing technologies are limited by their susceptibility to bacterial infections while promoting healthy cellular regeneration.
Different research has highlighted the possibility of wounds developing from different materials, natural or synthetic, with various physical forms (films, foams, hydrogels, hydrocolloids). For example, cotton gauze is used primarily to treat shallow wounds and are favorable due to the low cost, availability, and easy use. However, gauze only provides the wound with limited antimicrobial and poor wetting properties. The inflammatory response and reepithelization are poorly affected by dry gauze due to the oxygen environment under the gauze [42]. Limited by bacterial growth and contamination, cotton gauze was coated with chitosan-Ag-ZnO to increase the antimicrobial properties [43]. The coated gauze was able to retain water, showed an increase in drying time and antibacterial efficiency. Foam or sponges provide an alternative to gauze characterized by their absorbance of massive wound exudate suitable for deep wounds and minor burns [44]. Hydrogels are characterized by their three-dimensional networks, maintain moisture levels in the wound environment, high absorbance, and tailorable mechanical properties. The macromolecular networks produced by chemical or physical crosslinking of suitable polymers give rise to biocompatible dressings sensitive to the physiological environments, wettability, and flexibility. However, hydrogels have been reported to display weak mechanical properties requiring a secondary dressing or a surface modification necessary to make it a suitable wound dressing [45].
Nanotechnology-based wound dressings offer an approach to target the rising complexity of the cellular regeneration process as well as provide solutions to microbial infections. Several nanotechnology approaches for the formation of wound dressings have been tested including electrospinning, self-assembly, and phase separation techniques that allows for polymeric scaffolds to mimic properties of the extracellular matrix (ECM), including their fibrous nature and unique nanoscale features [46]. Current research has highlighted electrospinning as a suitable technique for nanofiber fabrication due to the ability to produce well-defined porous networks analogous to those of the ECM. Electrospinning, a voltage driven process, uses an applied electrical force where droplets or fibers are extruded from the soluble polymer that can produce mechanically strong pours networks with high aspect ratios. Electrospun PLGA/silk fibroin to create scaffolds with improved biocompatibility that showed improved attachment and proliferation of fibroblasts for a fast and healthy regeneration process of the skin [47]. Electrospinning thus provides the required nanotopography for a suitable cellular regeneration process through the production of porous networks.
Bioinspired Physical Barriers
High Aspect Ratio Bactericidal Nanostructures
Nature has been making high aspect ratio (HAR) nanostructures with bactericidal properties for millions of years. Those topographies can be found in the cuticles of certain insects like the dragonfly and cicada wings, and the skin of animals such as a gecko (Fig. 4a). The topography of the naturally occurring bactericidal surfaces has been replicated into a variety of materials such as silicon [48], poly(methyl methacrylate) (PMMA) [49, 50], and diamond [51], and all of them have shown a bactericidal activity similar to that of their native natural counterparts. Thus, and although the data are still incomplete, various lines of evidence are consistent with the hypothesis that bactericidal properties of HAR nanostructures are due to a contact killing mechanism that involves the physical disruption of the bacterial cell envelope, and that is independent of the surface composition. However, how envelope damage occurs, and how the membrane layer (s) are affected remains unclear. In Gram-negative bacteria, the cell envelope is formed by a thin peptidoglycan wall sandwiched between the plasma and outer membrane, whereas in Gram-positive bacteria, the cell envelope is made of a thick peptidoglycan layer and a plasma membrane only. It has been long believed that the peptidoglycan wall is the major responsible for the mechanical properties of the bacterial cell envelope; however, this concept has recently challenged by showing that the outer membrane in Gram-negative bacteria can be stiffer than the peptidoglycan wall [52].
At least three mechanisms have been proposed to explain the bactericidal activity of HAR nanostructures based on experimental observations (Fig. 3b, c). Using yeast cells (i.e., Saccharomyces cerevisiae) seeded on the wings of cicada and dragonfly species, Nowlin et al. [53] showed that the strength of the cell–substrate interaction and the nanostructure geometry were critical for the reduction of cell viability, and that stronger adhesion forces induced greater physical damage of the wall membrane in S. cerevisiae. Micrographs, showing the interface between yeast cells and the dragonfly wing surface, clearly depicted the extension of the yeast wall membrane into the underlying topography, as indicated by the presence of the vacuoles on the space separating the nanopillars (Fig. 3b). Thus, cell lysis was believed to occur as a result of the mechanical stretching induced by the cell/substrate adhesion strength at the top of the nanostructures. In another set of experiments, Ivanova et al. [54] prepared hydrophilic nanocones of variable height on silicon by increasing the exposure time of the material to plasma etching. This etched silicon was shown to be hydrophilic. Thus, a set of nanostructured silicon was further modified with a thin layer of silane to yield hydrophobic substrates. Both hydrophilic and hydrophobic nanostructured silicon were then tested against S. aureus and P. aeruginosa . Their results indicated that the adhesion affinity of bacterial cells to the nanostructured surface did not play a pivotal role in the mechanistic killing of these bacterial cells (Fig. 3b). They proposed a mechanism also based on the mechanical stretching of the microbial wall membrane; however, in this case, cell adhesion to the underlying topography was neglected. The rupture of the cell wall was proposed to occur at the area suspending between attachment points, as mechanical stress overcomes the elasticity of the wall [48]. Moreover, based on the same mechanism, these authors have proposed that Gram-negative bacteria are more susceptible to cell lysis compared to Gram-positive species due to differences in the cell wall thickness, the latter being thicker.
Naturally occurring bactericidal surfaces are characterized by high aspect ratio nanostructures. (A) High aspect ratio (HAR) bactericidal nanostructures can be found in the cuticles and skin of some insects and animals. Based on experimental observations, at least three mechanisms are proposed for the observed bactericidal activity of HAR nanostructures: (B) mechanical stretching of the membrane with or without cell adhesion [48, 53], and (C) shear forces that tear apart the outer membrane [55]. (D) Proposed biophysical models of microbial membrane damage depicting the cell envelope in Gram-negative bacteria
Besides mechanical stretching of the microbial wall, other authors have suggested that shear forces are a key factor involved in the bactericidal mechanisms of HAR nanostructures. Bandara et al. [55] by studying the interaction between E. coli and dragonfly wing nanopillars, indicated that wall damage in E. coli occurred without direct contact with the topography (Fig. 3c). The nanopillars were proposed to tear the outer membrane as the bacteria attempted to move away from the unfavorable surface. The authors also suggested that under this condition, E. coli could secrete higher amounts of extracellular polymeric substance (EPS), which in turn increased the adhesion strength to the underlying topography [55]. However, bacterial lysis can occur only when the cell wall is compromised; therefore, cell integrity should be preserved even after outer membrane tearing. The production of EPS can indeed be an emergent behavior upon mechanical stress and has also been reported for S. aureus growing on nanopillared-Si surfaces [56]. Diu et al. [57] have also proposed that shear forces may be associated with the stronger bactericidal effects on nanowire titania surfaces observed against motile bacteria [57]. All of these experimental observations indicate that more than one mechanism involved in the disruption of the bacterial cell envelope on HAR nanostructures may exist. For example, simple differences in wall thickness do not explain the biocidal activity observed in a variety of microorganisms with marked differences in envelope composition, like those of eukaryotic microorganisms (e.g., yeast) and Gram-negative and Gram-positive bacterial cells when subject to the topographies such as those of dragonfly wings. A complete list of biocidal nanotopographies found in nature and obtained via synthetic means has been recently summarized in excellent reviews by other authors (see [58, 59]).
Like the mechanisms based on experimental observations, biophysical models have been proposed aiming to shed light on the bactericidal mechanism observed experimentally on HAR nanostructures. Li and Chen [50] have proposed a thermodynamic model based on the balance between the adhesion energy and deformation energy of the cell membrane. According to this model, nanopillars with a large radius and small spacing induce more substantial stretching degree on the cell envelope compared to those with a radius smaller than a critical value (Fig. 3c). It is proposed that thick nanopillars generate a drastic increase in the contact adhesion per unit of horizontal area, which is accompanied by an increase in the stretching strain of the wall [50]. However, experimental observations made on cicada wing surfaces have shown that sharper and higher number of nanopillars have enhanced killing activity against Pseudomonas fluorescens [60]. An alternative mathematical model using a classical elasticity theory framework has been proposed by Xue et al. [61]. In this model, only gravity force and geometrical parameters of the surface topography are considered and predicts that the maximum stretching of the bacterial envelope happens at the top of the nanopillars, thus smaller and sharper nanopillars generate greater stretching responses to bacteria resting on them [61]. Moreover, authors indicate that the physical interactions at the interface between the bacterial cell and the nanostructure, cannot provide enough energy to permit full cell adhesion. Instead, gravity and nonspecific forces such as van der Waals interactions play a crucial role in cell damage. However, this model does not account for the deformation of the membrane in S. cerevisiae observed by Nowlin et al. [53] in dragonfly wing surfaces.
Finally, another thermodynamic model based on the experimental observations made on P. aeruginosa in contact with cicada wing topographies has been proposed [62]. This model also suggests mechanical disruption of the microbial envelope, being the wall rigidity a key determinant in the bacterial sensitivity to the bactericidal nature of the cicada wing topographies. As a result, less rigid bacterial walls will be more affected by nanopillars as in the case of Gram-negative species, in which a single peptidoglycan layer composes the cell envelope compared to the much thicker wall in Gram-positive bacteria. It is suggested that when the bacterium absorbs onto the nanopillar structures, the cell wall breaks in the regions suspended between the pillars (Fig. 3d). In this model, the bending of the membrane between adhesion points is neglected (i.e., the stretching degree of the cell wall at the vertices of the nanopillars and suspending between the them is assumed to be the same), and no specific biological interactions play a significant role in cell lysis [62]. Despite the lack of clarity on the exact killing contact mechanism, all the biophysical models proposed till now agree upon the idea that bactericidal nanopillars do not pierce the microbial envelope, but instead, it involves some mechanical stretching. Indeed, both superhydrophobic and hydrophilic HAR nanostructures have been observed to induce bacterial lysis by mechanical rupture of the cell wall, pointing out that the surface morphology rather than an alteration in the interfacial energy is the major responsible for the observed bactericidal activity [54]. However, a common observation is that both superhydrophobic and hydrophilic HAR nanostructures yield lower bacterial adhesion compared to smooth substrates of similar chemical composition, probably due to a reduction in surface area available for bacterial attachment [63].
As mentioned above, the topographies of the dragonfly and cicada wings have been replicated in polymers such as PMMA or acrylic. However, high aspect ratio bactericidal nanostructures have not been yet achieved in softer polymers and hydrogels of clinical relevance, because HAR nanostructures tend to ground collapse in aqueous environments due to adhesion and capillary forces acting on them [64]. For example, HAR nanopillars fabricated on polydimethylsiloxane (PDMS) obtained by replica molding, collapse when the dimension of the nanopillars exceed an aspect ratio higher than six [64]. Even though HAR nanostructures have been fabricated in polyurethane (PU), there have yet been any reports regarding their mechano-bactericidal activity. Topographies inspired by the shark’s skin has been reproduced in PDMS [65], but its effect on the bacterial viability and physiology is different from that evoked by HAR nanostructures (see section “Biofilm Control via Surface Micro and Nanotexture”). Like polymers with a low Young’s modulus (few KPa), the fabrication HAR topographies in hydrogels at the nanoscale with precise control of the size and shape distribution capable of resisting capillary forces have remained challenging [64, 66]. Hydrogels possess mechanical characteristics like those of soft tissues, which make them a desirable interface with the skin. Plasma modification can address the needs for unique nanotopography in hydrogels and clinically relevant polymers by altering the surface morphology and chemical composition. Unlike chemical modifications, plasma treatment eliminates the high cost of chemicals and toxic by-products. For a successful wound dressing, for instance, there is a need for plasma surface modification to alter the properties of the material to improve the biocompatibility and increase the antimicrobial properties, leaving the bulk material unaffected. The bulk properties of the material can be a composite of materials that are known to have antimicrobial properties or other desirable properties. By manipulating the surface properties, the surface can be used to control the attachment and colonization of bacteria, maintain the wettability and tissue-like structure to improve compatibility and offer the shortest healing time.
In recent studies, we have employed plasma modification for nanostructure growth in a variety of natural polymers including bacterial cellulose, chitosan, and silk (Fig. 4a). Bacterial cellulose (BC) is a hydrogel produced at the interface liquid/air by Acetobacter xylinum and is commonly used as a wound dressing material for the treatment of burns and other skin lesions. BC has also been employed as a substitute for small blood vessels and as a platform for the design of magnetic hydrogels for endovascular reconstruction [67,68,69]. By treating bacterial cellulose with low-energy argon ions, we have observed the growth of nanocones at the surface of the material, which can resist heat and aqueous immersion. Preliminary results using E. coli and Klebsiella pneumoniae cultured on these nanostructured BC have been shown to kill these bacterial strains effectively via a contact killing mechanism similar to that of natural bactericidal nanostructures. We have observed maximum envelope stretching at the top of the nanocones, which may be linked to cell lysis and the observed bacterial death.
Argon plasma irradiation induces nanopillar growth in bacterial cellulose and chitosan. (A) Pristine or unmodified bacterial cellulose (BC) is composed of interlaced fibers. After treatment with argon plasma, nanocones evolved in the surface of the material. (B) Chitosan is characterized by a relatively smooth surface. Similar to BC, it develops high aspect nanostructures whose orientation and height depend on the irradiation parameters. (C) Pristine silk reveals a heterogeneous surface at the microscale. When silk is irradiated with argon plasma, it develops oriented nanopillars capable of impairing bacteria adhesion. All the panels correspond to scanning electron micrographs
Similar to BC, chitosan has shown a remarkable response to plasma irradiation (Fig. 4b). Chitosan is a deacetylated derivative of chitin and one of the most abundant natural polymers. Chitosan is known for its biocompatibility, biodegradability, non-toxicity, antimicrobial properties, and biofunctionality. Its applications include coatings for bone implant materials [70, 71], wound dressings [72] and carrier for drug delivery [73]. We have observed the formation of nanofeatures on chitosan upon plasma irradiation. The type and dimensions of these features have been shown to be dependent on the irradiation parameters. The activity of cultured bacteria on these structures was studied. Surfaces with high aspect ratio nanopillars, triggered by high fluence (i.e., number of ions impacting the surface per unit area) irradiations, showed prominent bactericidal behavior. Such antibacterial activity was observed against both Gram-negative (E. coli) and Gram-positive (S. aureus) bacteria. Observations on these results showed a reduced presence of bacteria and increased death on the surface with increasing HAR nanopillars (unpublished data by the authors).
The formation of HAR nanostructures is not unique to polysaccharides such as BC and chitosan, but instead can also be fabricated on natural proteins such as silk (Fig. 4c). Silk fibroin, which is produced by silkworms (e.g., Bombyx mori) and spiders (e.g., Nephila clavipes), is a biocompatible and biodegradable protein, with tailorable mechanical properties. Thanks to these properties, silk has been used in sutures, scaffolds for tissue engineering, and the regeneration of bone, tendon, skin, and in peripheral nerve restoration [74, 75]. Because surface properties modulate the immune response of biomaterials and can control microbial infections, we have been introducing nanopillars into silk by plasma modification to enhance the cellular response and the bactericidal capabilities of this material.
Biofilm Control via Surface Micro- and Nanotexture
The manifestation of microbial association into biofilms either as a free-floating or surface-bound community is abundant in nature, as we see the formation of biofilms in almost every habitat on earth ranging from the plaque that grows on the surface of our teeth to the biofilms that form in the bottom of the ocean. The key benefits of microbial aggregation compared to a planktonic lifestyle lie in that biofilms provide to microbial communities increased ecological stability, cooperative and collective social behaviors, and protection against environmental challenges [76]. Bacterial attachment to surfaces is believed to occur in two main stages. During the first stage, bacterial cells are loosely attached or close to the surface. Bacteria can easily spin, vibrate, and return to the planktonic state. The primary forces dominating this reversible attachment are van der Waals forces, electrostatic forces, and hydrophobic interactions. The second stage is characterized by an irreversible attachment of the bacteria to the substratum, which is assisted by exopolysaccharides, and by adhesins such as pili and flagella [77].
One of the most outstanding puzzles in studies of microbial/surface interactions has been to understand how surface properties affect microbial life. This has been difficult given the complexity and variations in the composition of the outer membrane among microbial species, the impact of external factors such as the medium composition and pH in the microbial and surface properties, and the difficulty in isolating the surface parameters in material interfaces. Many studies, for example, have investigated the low adhesion and anti-biofouling capabilities of a variety of leaves, including those of the rice, taro, and lotus plants based on their low-adhesion and hydrophobic nature, but these features seem to be more critical on water immersed environments than on aerial habitats [59]. The consensus is that microorganisms can colonize any surface sooner or later and that even hydrophobic surfaces experienced microbial growth.
However, the investigation on microbial communities in a variety of ecological niches has indicated that the spatial structure of the microenvironment has essential implications on bacterial growth and biofilm structure. For example, the spatial variation and heterogeneity of the leaf surface in plants such as composition, thickness, permeability, and topography drives the nonrandom microscale spatial distribution of microorganisms and its interaction with other microbial colonizers [78]. This compartmentalized microbial distribution is not unique to the leaves in plants, but instead is a common feature in a variety of ecological niches. Regional differences in skin anatomy, for example, contribute to the selection of a unique set of microorganisms adapted to inhabit specific body sites [1].
In micropatterned arrays, bacteria have been observed to organize spontaneously and follow the symmetry of the underlying topography independently of the surface composition, especially when the characteristic dimensions of the topographical features become comparable to those of the bacterial cells. A variety of geometries have been considered, and all of them support the idea that bacteria tend to maximize the adhesion area when presented with features at the micro- and nanoscale. Bacterial arrangement in some of those geometries is exemplified in Fig. 5. For example, by using a periodic array with variable dimensional parameters such as post diameter, height, pitch, and array symmetry, Hochbaum and Aizenberg [79] showed that P. aeruginosa oriented normal to the substrate and along the nanoposts when the spacing between adjacent features approached that of the characteristic size of the cell. In contrast, when the nearest neighbor post spacing was more significant than the length of the cell, the adhesion of P. aeruginosa to the substrate was random, as depicted in Fig. 5. Inspired by the nonfouling properties of the skin of echinoderms and other marine organisms, the same authors employed static and dynamic microscale wrinkle topographies on polydimethylsiloxane (PDMS) to reduce and control bacterial biofilm attachment. In the static configuration, bacteria patterned spontaneously on the PDMS wrinkles following the spacing and orientation of the trough [80]. By applying a dynamic uniaxial mechanical strain to the PDMS, those authors showed up to 80% of P. aeruginosa biofilm reduction for a specific set of strain parameters. In our laboratory, we also have fabricated wrinkles in PDMS by using argon plasma irradiation for bacteria/surface interaction studies, but at dimensions much smaller than those used by Epstein et al. [80]. We have observed that besides the preferential settlement of E. coli on the valley of the wrinkles, bacterial deformation also occurs as a result of the tortuosity imposed by the topography.
Bacteria self-organization in nano- and microscale topographies. Bacteria attached perpendicular to a substrate with nanopillar arrays when the spacing between posts is comparable to the bacterium size. The same effect is observed in microscale wrinkles, channels, and ridges with similar dimensions. Bacteria adopt those configurations to maximize the contact area with the substratum
Microtopograhies inspired by the sharkskin have also been demonstrated to limit bacterial communication and alter biofilm formation. For example, Chung et al. [65] used a topography inspired on the sharkskin (Sharklet AF™), which was fabricated in PDMS with 2 μm width and spacing and 3 μm height and cultured with S. aureus for 14 days. At the end of the incubation period, the Sharklet AF™ topography did not show evidence of biofilm development, whereas, on flat PDMS, biofilm formation was evident at day 7 [65]. The authors suggested that the height of the features contributed to colony isolation. In a similar study, Sakamoto et al. [81], using the sharkskin micropatterned surface, determined whether the height of the patterns in the Sharklet AF™ topography was a determinant for biofilm disruption. Those authors found that the depth of the groove was not crucial for the antibacterial effect, but instead, the tortuosity due to the variety of surface topography was vital for the decrease in biofilm formation and swarming motility [81].
Future Perspectives
A key issue in the treatment of skin infections is the presence of bacterial biofilms, which are particularly difficult to manage when they are associated with the surface of biomaterials. Interfaces implementing nano- and microscale topographies offers an unprecedented opportunity to prevent the microbial colonization and biofilm formation in common biomaterial products used in contact with the skin, such as medical adhesives, sutures, and wound dressing materials, which usually serve as the origin of infection. One of the major advantages that anti-biofouling and antimicrobial physical barriers provide compared to other methods is that they do not contribute to bacterial resistance, do not pollute the environment, and are easy to implement. Moreover, the potential application of those nano- and microscale interfaces are not limited to the design of materials for the treatment of infections but also provide a tool for studying how variations in the structural space of natural environments modulate the interactions between microbial communities and the host.
References
Grice EA, Segre JA (2011) The skin microbiome. Nat Rev Microbiol 9(4):244
Byrd AL, Belkaid Y, Segre JA (2018) The human skin microbiome. Nat Rev Microbiol 16(3):143
Williams MR, Gallo RL (2015) The role of the skin microbiome in atopic dermatitis. Curr Allergy Asthma Rep 15(11):65
Naik S, Bouladoux N, Linehan JL et al (2015) Commensal–dendritic-cell interaction specifies a unique protective skin immune signature. Nature 520(7545):104
Nakatsuji T, Chen TH, Narala S et al (2017) Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci Transl Med 9(378):eaah4680
McNichol L, Lund C, Rosen T, Gray M (2013) Medical adhesives and patient safety: state of the science consensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Dermatol Nurses Assoc 5(6):323–338
Qin Y (2019) Antimicrobial textile dressings to manage wound infection. In: Rajendran S (ed) Advanced textiles for wound care. Woodhead Publishing, Cambridge
Miller LG, Eisenberg DF, Liu H et al (2015) Incidence of skin and soft tissue infections in ambulatory and inpatient settings, 2005–2010. BMC Infect Dis 15(1):362
Fung HB, Chang JY, Kuczynskf S (2003) A practical guide to the treatment of complicated skin and soft tissue infections. Drugs 63(14):1459–1480
Serra R, Grande R, Butrico L et al (2015) Chronic wound infections: the role of Pseudomonas aeruginosa and Staphylococcus aureus. Expert Rev Anti Infect Ther 13(5):605–613
Lawton S, Langøen A (2009) Assessing and managing vulnerable periwound skin. World Wide Wounds. http://www.worldwidewounds.com/2009/October/Lawton-Langoen/vulnerable-skin-2.html. Accessed 30 January 2019
Gray M, Black JM, Baharestani MM et al (2011) Moisture-associated skin damage: overview and pathophysiology. J Wound Ostomy Continence Nurs 38(3):233–241
Friedman ND, Temkin E, Carmeli Y (2016) The negative impact of antibiotic resistance. Clin Microbiol Infect 22(5):416–422
Projan SJ (2003) Why is big pharma getting out of antibacterial drug discovery? Curr Opin Microbiol 6(5):427–430
Schrand AM, Rahman MF, Hussain SM, Schlager JJ, Smith DA, Syed AF (2010) Metal-based nanoparticles and their toxicity assessment. Wiley Interdiscip Rev Nanomed Nanobiotechnol 2(5):544–568
Linden SK, Sutton P, Karlsson NG, Korolik V, McGuckin MA (2008) Mucins in the mucosal barrier to infection. Mucosal Immunol 1(3):183
Caldara M, Friedlander RS, Kavanaugh NL, Aizenberg J, Foster KR, Ribbeck K (2012) Mucin biopolymers prevent bacterial aggregation by retaining cells in the free-swimming state. Curr Biol 22(24):2325–2330
Khan Y, Ostfeld AE, Lochner CM, Pierre A, Arias AC (2016) Monitoring of vital signs with flexible and wearable medical devices. Adv Mater 28(22):4373–4395
Kwak MK, Jeong HE, Suh KY (2011) Rational design and enhanced biocompatibility of a dry adhesive medical skin patch. Adv Mater 23(34):3949–3953
LeBlanc K, Baranoski S (2014) Skin tears: the forgotten wound. Nurs Manage 45(12):36–46
Anderson A, Foster RS, Brand R, Blyth CC, Kotecha RS (2014) Acute onset of pustules at the site of tape placement in an immunocompromised infant with acute myeloid leukemia. Pediatr Dermatol 31(5):609–610
Wilcox MH, Fitzgerald P, Freeman J et al (2000) A five year outbreak of methicillin-susceptible Staphylococcus aureus phage type 53, 85 in a regional neonatal unit. Epidemiol Infect 124(1):37–45
Konya C, Sanada H, Sugama J, Okuwa M, Kamatani Y, Nakagami G, Sakaki K (2010) Skin injuries caused by medical adhesive tape in older people and associated factors. J Clin Nurs 19(9-10):1236–1242
de Goffau MC, Bergman KA, de Vries HJ, Meessen NE, Degener JE, van Dijl JM, Harmsen HJ (2011) Cold spots in neonatal incubators are hot spots for microbial contamination. Appl Environ Microbiol 77(24):8568–8572
Ness MJ, Davis DM, Carey WA (2013) Neonatal skin care: a concise review. Int J Dermatol 52(1):14–22
Hornik CP, Fort P, Clark RH, Watt K, Benjamin DK Jr, Smith PB, Manzoni P, Jacqz-Aigrain E, Kaguelidou F, Cohen-Wolkowiez M (2012) Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev 88:S69–S74
Lund C (2014) Medical adhesives in the NICU. Newborn Infant Nurs Rev 14(4):160–165
Anjum S, Gupta A, Sharma D et al (2017) Antimicrobial nature and healing behavior of plasma functionalized polyester sutures. J Bioact Compat Pol 32(3):263–279
Kondrup JD, Qayyum AM (2018) Closing the gap: novel abdominal wound closure techniques. Surg Technol Int 32:25–31
Greenberg JA, Clark RM (2009) Advances in suture material for obstetric and gynecologic surgery. Rev Obstet Gynecol 2(3):146
Dennis C, Sethu S, Nayak S, Mohan L, Morsi Y, Manivasagam G (2016) Suture materials—current and emerging trends. J Biomed Mater Res A 104(6):1544–1559
Altman GH, Diaz F, Jakuba C, Calabro T et al (2003) Silk-based biomaterials. Biomaterials 24(3):401–416
Walter CJ, Dumville JC, Sharp CA, Page T (2012) Systematic review and meta-analysis of wound dressings in the prevention of surgical-site infections in surgical wounds healing by primary intention. Br J Surg 99(9):1185–1194
Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK (2011) Improving risk-adjusted measures of surgical site infection for the National Healthcare Safely Network. Infect Control Hosp Epidemiol 32(10):970–986
Berrios-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surg 152(8):784–791
Kathju S, Nistico L, Hall-Stoodley L, Post JC, Ehrlich GD, Stoodley P (2009) Chronic surgical site infection due to suture-associated polymicrobial biofilm. Surg Infect (Larchmt) 10(5):457–461
Serrano C, García-Fernández L, Fernández-Blázquez JP et al (2015) Nanostructured medical sutures with antibacterial properties. Biomaterials 52:291–300
Crovetti G, Martinelli G, Issi M, Barone M et al (2004) Platelet gel for healing cutaneous chronic wounds. Transfus Apher Sci 30(2):145–151
Gottrup F (2004) A specialized wound-healing center concept: importance of a multidisciplinary department structure and surgical treatment facilities in the treatment of chronic wounds. Am J Surg 187(5):S38–S43
Simões D, Miguel SP, Ribeiro MP, Coutinho P, Mendonça AG, Correia IJ (2018) Recent advances on antimicrobial wound dressing: a review. Eur J Pharm Biopharm 127:130–141
Cardona AF, Wilson SE (2015) Skin and soft-tissue infections: a critical review and the role of telavancin in their treatment. Clin Infect Dis 61(suppl_2):S69–S78
Han G, Ceilley R (2017) Chronic wound healing: a review of current management and treatments. Adv Ther 34(3):599–610
Abbasipour M, Mirjalili M, Khajavi R, Majidi MM (2014) Coated cotton gauze with Ag/ZnO/chitosan nanocomposite as a modern wound dressing. J Eng Fiber Fabr 9(1):155892501400900114
Brown MS, Ashley B, Koh A (2018) Wearable technology for chronic wound monitoring: current dressings, advancements, and future prospects. Front Bioeng Biotechnol 6:47
Kamoun EA, Kenawy ERS, Chen X (2017) A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J Adv Res 8(3):217–233
Hamdan S, Pastar I, Drakulich S, Dikici E, Tomic-Canic M, Deo S, Daunert S (2017) Nanotechnology-driven therapeutic interventions in wound healing: Potential uses and applications. ACS Cent Sci 3(3):163–175
Shahverdi S, Hajimiri M, Esfandiari MA, Larijani B, Atyabi F, Rajabiani A, Dehpour AR, Gharehaghaji AA, Dinarvand R (2014) Fabrication and structure analysis of poly(lactide-co-glycolic acid)/silk fibroin hybrid scaffold for wound dressing applications. Int J Pharm 473(1):345–355
Linklater DP, Juodkazis S, Rubanov S, Ivanova EP (2017) Comment on “Bactericidal Effects of Natural Nanotopography of Dragonfly Wing on Escherichia coli”. ACS Appl Mater Interfaces 9(35):29387–29393
Dickson MN, Liang EI, Rodriguez LA, Vollereaux N, Yee AF (2015) Nanopatterned polymer surfaces with bactericidal properties. Biointerphases 10(2):021010
Li X, Chen T (2016) Enhancement and suppression effects of a nanopatterned surface on bacterial adhesion. Phys Rev E 93(5):052419
Fisher LE, Yang Y, Yuen MF, Zhang W, Nobbs AH, Su B (2016) Bactericidal activity of biomimetic diamond nanocone surfaces. Biointerphases 11(1):011014
Rojas ER, Billings G, Odermatt PD, Auer GK, Zhu L, Miguel A, Chang F, Weibel DB, Theriot JA, Huang KC (2018) The outer membrane is an essential load-bearing element in Gram-negative bacteria. Nature 559(7715):617
Nowlin K, Boseman A, Covell A, LaJeunesse D (2015) Adhesion-dependent rupturing of Saccharomyces cerevisiae on biological antimicrobial nanostructured surfaces. J R Soc Interface 12(102):20140999
Ivanova EP, Hasan J, Webb HK et al (2013) Bactericidal activity of black silicon. Nat Commun 4:2838
Bandara CD, Singh S, Afara IO, Wolff A, Tesfamichael T, Ostrikov K, Oloyede A (2017) Bactericidal effects of natural nanotopography of dragonfly wing on Escherichia coli. ACS Appl Mater Interfaces 9(8):6746–6760
Hizal F, Choi CH, Busscher HJ, van der Mei HC (2016) Staphylococcal adhesion, detachment and transmission on nanopillared Si surfaces. ACS Appl Mater Interfaces 8(44):30430–30439
Diu T, Faruqui N, Sjöström T, Lamarre B, Jenkinson HF, Su B, Ryadnov MG (2014) Cicada-inspired cell-instructive nanopatterned arrays. Sci Rep 4:7122
Lin N, Berton P, Moraes C, Rogers RD, Tufenkji N (2018) Nanodarts, nanoblades, and nanospikes: mechano-bactericidal nanostructures and where to find them. Adv Colloid Interface Sci 252:55–68
Tripathy A, Sen P, Su B, Briscoe WH (2017) Natural and bioinspired nanostructured bactericidal surfaces. Adv Colloid Interface Sci 248:85–104
Kelleher SM, Habimana O, Lawler J, O’reilly B, Daniels S, Casey E, Cowley A (2015) Cicada wing surface topography: an investigation into the bactericidal properties of nanostructural features. ACS Appl Mater Interfaces 8(24):14966–14974
Xue F, Liu J, Guo L, Zhang L, Li Q (2015) Theoretical study on the bactericidal nature of nanopatterned surfaces. J Theor Biol 385:1–7
Pogodin S, Hasan J, Baulin VA et al (2013) Biophysical model of bacterial cell interactions with nanopatterned cicada wing surfaces. Biophys J 104(4):835–840
Luan Y, Liu S, Pihl M, van der Mei HC, Liu J, Hizal F, Choi CH, Chen H, Ren Y, Busscher HJ (2018) Bacterial interactions with nanostructured surfaces. Curr Opin Colloid Interface Sci 38:170–189
Zhang Y, Lo CW, Taylor JA, Yang S (2006) Replica molding of high-aspect-ratio polymeric nanopillar arrays with high fidelity. Langmuir 22(20):8595–8601
Chung KK, Schumacher JF, Sampson EM, Burne RA, Antonelli PJ, Brennan AB (2007) Impact of engineered surface microtopography on biofilm formation of Staphylococcus aureus. Biointerphases 2(2):89–94
Ma S, Yu B, Pei X, Zhou F (2016) Structural hydrogels. Polymer 98:516–535
Arias SL, Shetty A, Devorkin J, Allain JP (2018) Magnetic targeting of smooth muscle cells in vitro using a magnetic bacterial cellulose to improve cell retention in tissue-engineering vascular grafts. Acta Biomater 77:172–181
Arias SL, Shetty AR, Senpan A, Echeverry-Rendón M, Reece LM, Allain JP (2016) Fabrication of a functionalized magnetic bacterial nanocellulose with iron oxide nanoparticles. J Vis Exp (JoVE):111
Echeverry-Rendon M, Reece LM, Pastrana F, Arias SL, Shetty AR, Pavón JJ, Allain JP (2017) Bacterial nanocellulose magnetically functionalized for neuro-endovascular treatment. Macromol Biosci 17(6):1600382
Civantos A, Martinez-Campos E, Ramos V, Elvira C, Gallardo A, Abarrategi A (2017) Titanium coatings and surface modifications: toward clinically useful bioactive implants. ACS Biomater Sci Eng 3(7):1245–1261
Douglas TE, Kumari S, Dziadek K et al (2017) Titanium surface functionalization with coatings of chitosan and polyphenol-rich plant extracts. Mater Lett 196:213–216
Ribeiro MP, Espiga A, Silva D, Baptista P, Henriques J, Ferreira C, Silva JC, Borges JP, Pires E, Chaves P, Correia IJ (2009) Development of a new chitosan hydrogel for wound dressing. Wound Repair Regen 17(6):817–824
Abarrategi A, Civantos A, Ramos V, Sanz Casado JV, López-Lacomba JL (2007) Chitosan film as rhBMP2 carrier: delivery properties for bone tissue application. Biomacromolecules 9(2):711–718
Lopez-Cebral R, Silva-Correia J, Reis RL, Silva TH, Oliveira JM (2017) Peripheral nerve injury: current challenges, conventional treatment approaches, and new trends in biomaterials-based regenerative strategies. ACS Biomater Sci Eng 3(12):3098–3122
Vepari C, Kaplan DL (2007) Silk as a biomaterial. Prog Polym Sci 32(8-9):991–1007
Nadell CD, Drescher K, Foster KR (2016) Spatial structure, cooperation and competition in biofilms. Nat Rev Microbiol 14(9):589
Petrova OE, Sauer K (2012) Sticky situations: key components that control bacterial surface attachment. J Bacteriol 194(10):2413–2425
Leveau JH (2015) Life of microbes on aerial plant parts. In: Lugtenberg B (ed) Principles of plant-microbe interactions. Springer, Cham
Hochbaum AI, Aizenberg J (2010) Bacteria pattern spontaneously on periodic nanostructure arrays. Nano Lett 10(9):3717–3721
Epstein AK, Hong D, Kim P, Aizenberg J (2013) Biofilm attachment reduction on bioinspired, dynamic, micro-wrinkling surfaces. New J Phys 15(9):095018
Sakamoto A, Terui Y, Horie C et al (2014) Antibacterial effects of protruding and recessed shark skin micropatterned surfaces of polyacrylate plate with a shallow groove. FEMS Microbiol Lett 361(1):10–16
Acknowledgments
Material characterization was partially carried out in the Materials Research Laboratory Central Facilities at the University of Illinois at Urbana-Champaign. Authors would like to thank Zachariah Koyn for his technical support on performing part of the material irradiations. Sandra L. Arias would like to thank Monika Makurath and Roshni Bano for their helpful discussions on microbial physiology.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Arias, S.L., Devorkin, J., Civantos, A., Jaramillo, C., Allain, J.P. (2020). Bioinspired Interfaces for the Management of Skin Infections. In: Li, B., Moriarty, T., Webster, T., Xing, M. (eds) Racing for the Surface. Springer, Cham. https://doi.org/10.1007/978-3-030-34475-7_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-34475-7_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34474-0
Online ISBN: 978-3-030-34475-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)