Abstract
Diaphragmatic injuries are uncommon injuries in the chest, thus they can easily be missed by the radiologist and surgeon. Therefore, a high index of suspicion is important for an early diagnosis and to avoid any complications. Multidetector computed tomography is the modality of choice for the diaphragmatic injuries. On MDCT, there are direct and indirect signs of diaphragmatic injuries. In this chapter we discuss the findings associated with blunt as well as penetrating diaphragmatic injuries with an emphasis on the role of the radiologist in making the diagnosis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Traumatic injuries to the diaphragm are caused by blunt or penetrating trauma, either to the chest or abdominal wall. Regardless of the etiology, these injuries require treatment to avoid the serious complications of obstruction or strangulation of herniated viscera. As nonoperative management increases and fewer initially occult cases of diaphragmatic injury are diagnosed intraoperatively, the imaging diagnosis of these injuries has become increasingly more important (Fair et al. 2015). Despite the importance of recognizing these injuries, detecting diaphragmatic injuries is still a diagnostic challenge for many radiologists and trauma surgeons (Reber et al. 1998; Hanna et al. 2008).
Penetrating diaphragmatic injuries are commonly caused by gunshot or stab wounds. There is no definite predilection for the side of diaphragmatic injury among victims of gunshot wounds (Patlas et al. 2015). Serious injuries from stab wounds are more common on the left than on the right, which is probably due to protective effect from the liver on the right hemidiaphragm, a greater proportion of right-handed assailants, and a relative underdiagnosis of subtle right diaphragmatic injuries (Patlas et al. 2015).
Surgery has long played a significant role in the management of patients presenting with penetrating thoracoabdominal injuries; however, selective nonoperative management is increasingly recommended for these patients, with good outcomes in the setting of both blunt and penetrating traumas (Croce et al. 1995; Iochum et al. 2002; Como et al. 2010; Dreizin et al. 2015). There is a growing trend for conservative management of blunt traumatic patients. As nonoperative management of traumatic patients increases, it is possible that some diaphragmatic injuries which were once only identified intraoperatively will only be detected radiologically or after complications of diaphragmatic injury arise. This trend in the shift of the management strategy will require a need for greater vigilance by radiologists for subtle signs of diaphragmatic injury.
The radiologic detection of diaphragmatic injuries is difficult because many physicians are unfamiliar with the scope of diaphragmatic injuries and their imaging findings (Hanna et al. 2008; Desir and Ghaye 2012). Many imaging signs have been described for the detection of these injuries; however, some patients present with only one or a few of the many known signs. As such, being familiar with the radiologic signs of diaphragmatic injury is essential for the practicing radiologist, especially in the emergency setting.
Frequently, significant or life-threatening thoracic and abdominal injuries can distract the radiologist from the more subtle findings of diaphragmatic injuries. The key to a successful radiologic diagnosis of diaphragmatic injury is to have a high degree of suspicion based on clinical setting and to develop a familiarity with the classic imaging findings of traumatic diaphragmatic injury (Guth et al. 1995).
Although some animal models suggest spontaneous healing of small diaphragmatic defects, there are no published reports of a human diaphragmatic injury healing without surgery (Shatney et al. 2003; Desir and Ghaye 2012). Physiologic negative intrathoracic pressures during unassisted ventilation and the constant motion of the diaphragm likely impede healing of diaphragmatic injuries and can result in delayed herniation of intra-abdominal contents (Desir and Ghaye 2012). In cases of missed diaphragmatic injury, reports indicate potential for delayed complications of visceral herniation with potential for obstruction or strangulation, with mortality of approximately 30–60 % in cases of visceral strangulation (Murray et al. 1996; Desir and Ghaye 2012; Panda et al. 2014; Dreizin et al. 2015). Therefore, it is essential that these injuries be detected as early as possible.
2 Anatomic and Developmental Considerations
The diaphragm is a thin musculotendinous sheet with a concave undersurface and apertures allowing passage of transdiaphragmatic structures. The largest of these are the hiatuses of the inferior vena cava, esophagus, and aorta. The caval hiatus is located at the T8–T9 intervertebral disk level to the right of the central tendon. The inferior vena cava is adherent to its margin (Standring 2016). The esophageal hiatus is at the level of the tenth vertebral body. The esophagus is not directly continuous with the muscle of the esophageal hiatus (Standring 2016). The aortic hiatus is an osseo-aponeurotic aperture at the lower level of the twelfth vertebral body, passing outside of the diaphragmatic muscle fibers adjacent to the vertebral column, and is not affected by their contraction (Standring 2016).
Congenital areas of weakness may be present between diaphragmatic muscle fibers that insert on the sternum and the ribs (sternocostal triangles) and between the fibers that insert on the ribs and the lumbar vertebrae (lumbocostal triangles). These areas of weakness are likely responsible for nontraumatic Morgagni and Bochdalek hernias (Thomas Sadler et al. 2003). In addition, the interface between the embryologic septum transversum (originating anteriorly) and the pleuroperitoneal folds corresponds to potential areas of inherent weakness in the posterolateral diaphragm, which may be predisposed to rupture in the setting of high-energy abdominal trauma (Desir and Ghaye 2012).
3 Mechanism of Injury
In the USA, penetrating diaphragmatic injuries are twice as common as blunt diaphragmatic injuries (Fair et al. 2015). Penetrating injuries are due to knife and gunshot wounds and tend to result in smaller diaphragmatic injuries, typically on the order of 1 or 2 cm in length (Iochum et al. 2002; Desir and Ghaye 2012). The small size of the corresponding diaphragmatic defect may also lead to difficulty directly appreciating these injuries on imaging studies (Desir and Ghaye 2012). Because of the small size of defects generally seen in penetrating diaphragmatic injuries, herniation of abdominal contents is uncommon after penetrating diaphragmatic injury (Dreizin et al. 2015). Penetrating injuries may injure any organs or structures in line with the trajectory of the wound and as such may vary widely in distribution (Iochum et al. 2002) but commonly involve liver and hollow viscus (Fair et al. 2015).
Penetrating diaphragmatic injuries from stabbings occur more frequently on the left than the right (Patlas et al. 2015). This is theorized to result from the higher number of right-handed assailants who face their victim at the time of injury (Panda et al. 2014). Another factor that may contribute to the relative frequency of left-sided penetrating diaphragmatic injuries is the protection which the liver provides and whose absence on the left results in areas of weakness in the left hemidiaphragm (Panda et al. 2014).
Blunt diaphragmatic injuries are most commonly the result of motor vehicle accidents, but other causes include falls and severe blows to the body. It has been proposed that multiple mechanisms of injury may be involved in a blunt diaphragmatic injury, which may be differentiated by the direction of greatest impact at the time of injury. A frontal impact on the abdomen is proposed to increase intra-abdominal pressure, resulting in subsequent upward force from intra-abdominal contents moving toward the relatively low-pressure thorax (Iochum et al. 2002; Desir and Ghaye 2012). Lateral impacts have been proposed to injure the diaphragm through shear forces (Iochum et al. 2002; Desir and Ghaye 2012). Other factors such as fractured ribs or the phase of the respiratory cycle may also play a role in the mechanism of blunt diaphragmatic injury (Rees et al. 2005; Desir and Ghaye 2012). In contrast to the small size of penetrating diaphragmatic injuries, blunt diaphragmatic injuries tend to be large (>10 cm) (Iochum et al. 2002). Perhaps not surprisingly, left hemidiaphragmatic injuries are associated with splenic injuries, and right hemidiaphragmatic injuries are associated with hepatic injuries.
Diaphragmatic injury will essentially never occur in isolation. Penetrating diaphragmatic injuries are associated with liver injury (53.6 %), splenic injury (29.1 %), pulmonary injury (28.1 %), stomach injury (26.6 %), hemothorax (26.2 %), and pneumothorax (20.4 %) (Fair et al. 2015). Blunt diaphragmatic injuries are associated with pulmonary injury (48.7 %), splenic injury (44.8 %), liver injury (39.7 %), pneumothorax (30 %), and hemothorax (21.5 %) (Fair et al. 2015). Other injuries commonly associated with blunt diaphragmatic injury include renal, aortic, cardiac, and osseous injuries, such as spinal, pelvic, and rib fractures (Iochum et al. 2002; Desir and Ghaye 2012; Fair et al. 2015). The coincident injuries seen in association with blunt diaphragmatic injury, for instance, result in mortality of approximately 12–42 % (Iochum et al. 2002; Desir and Ghaye 2012).
The proportion of left-sided to right-sided diaphragmatic injuries is higher after blunt trauma with frontal impact; however, relative numbers of right and left diaphragmatic injury are similar after posterior impacts (Desir and Ghaye 2012). Side impacts typically result in injury on the side of impact (Desir and Ghaye 2012). The increased frequency of left-sided blunt diaphragmatic injuries is attributed to the protective effect of the liver on the right hemidiaphragm and the vulnerability of an unprotected area of congenital weakness of the left diaphragm (Desir and Ghaye 2012). Some of the difference in frequency of left and right injuries may also be due to underdiagnosis of subtle right-sided injuries (Killeen et al. 1999; Patlas et al. 2015). The left hemidiaphragm runs next to abdominal fat that makes its contour more visible, while the right hemidiaphragm may be difficult to distinguish from the higher-attenuation hepatic parenchyma (Killeen et al. 1999; Iochum et al. 2002; Desir and Ghaye 2012).
4 Epidemiology
The relative frequency of penetrating and blunt diaphragmatic injuries varies, with significantly higher numbers of penetrating injuries seen in several large studies (Hammer et al. 2014; Fair et al. 2015; Gao et al. 2015). Some smaller studies have included a greater number of blunt diaphragmatic injuries than penetrating diaphragmatic injuries, which may be due to their small sample size or possibly because the frequency of gunshot wounds and stabbings is proportionally lower in their study populations (Panda et al. 2014; Leung et al. 2015).
Penetrating diaphragmatic injuries are more common among young men, with males making up 91.4 % of cases in the USA (Fair et al. 2015). The average age of US patients diagnosed with penetrating diaphragmatic injuries is 31 years (standard deviation of 13 years) (Fair et al. 2015). The relatively high proportion of men presenting with penetrating diaphragmatic injury is probably due to the fact that men are more likely than women to be involved in stabbings and shootings (Hanna et al. 2008). Penetrating diaphragmatic injuries are reported in 10–42 % of penetrating thoracoabdominal traumas (Spann et al. 1995; Bodanapally et al. 2009; Yucel et al. 2015).
Blunt diaphragmatic injuries are also more common among men (Fair et al. 2015). Men comprised 67.9 % of blunt diaphragmatic injuries in a recent study of over 3700 diaphragmatic injuries in the USA, with an average age of 44 years (standard deviation of 19 years). Blunt thoracoabdominal trauma results in diaphragmatic injury in 0.8–8.0 % of cases (Iochum et al. 2002; Desir and Ghaye 2012). When compared to patients with penetrating diaphragmatic injuries, patients with blunt diaphragmatic injuries have longer stays in intensive care, longer ventilator requirements, and higher mortality (19.8 % vs. 8.8 %) (Fair et al. 2015).
5 Radiographic Evaluation
Even with the increasing use of MDCT imaging, first-line trauma imaging is usually a portable chest radiograph. There are numerous limitations of chest radiographs such as lack of patient cooperation, the use of portable equipment, and suboptimal patient positioning (Iochum et al. 2002). Despite these factors, initial radiographic evaluation may successfully render a diagnosis of diaphragmatic injury. The sensitivity of initial radiographs has a wide range of reported values, from 17 to 65 % (Iochum et al. 2002; Patlas et al. 2015). The reported sensitivity of chest radiograph for right-sided diaphragmatic injuries (approximately 17 %) is lower than for left-sided injuries (approximately 27–60 %) (Iochum et al. 2002).
The most valuable signs of diaphragmatic rupture seen on chest radiography are definite visualization of abdominal viscera above the diaphragm (with or without a focal constriction of herniated viscera as they pass through the violated diaphragm, the collar sign) and visualization of the tip of a nasogastric tube above the diaphragm (Gelman et al. 1991; Desir and Ghaye 2012). The sensitivity for an NG tube crossing the left diaphragm on chest radiograph has a sensitivity of approximately 44–64 % (Gelman et al. 1991; Guth et al. 1995).
Another finding that is highly suggestive of diaphragmatic injury is the unexplained elevation of a hemidiaphragm. In the setting of blunt abdominal trauma, a 4 cm elevation of either hemidiaphragm is correlated with injury to that hemidiaphragm; however, some authors suggest a higher cutoff of 6 cm from the contralateral diaphragm (Gelman et al. 1991; Guth et al. 1995; Desir and Ghaye 2012).
Unfortunately, most patients with a traumatic diaphragmatic injury present with nonspecific findings on chest radiography, such as obscured outline of the injured hemidiaphragm, mild elevation of the affected hemidiaphragm, mediastinal shift to the contralateral side, and sequela of trauma such as effusions, pneumothorax, or rib fractures (Gelman et al. 1991; Guth et al. 1995; Desir and Ghaye 2012, Patlas, Leung et al. 2015).
If a patient cannot be imaged by CT (either because their condition is too unstable to allow transport to the scanner or due to a lack of availability of CT scanning), serial chest radiographs may be useful, especially after extubation (Gao et al. 2015). Because of the artificially increased intrathoracic pressures while undergoing positive pressure ventilation, herniation of intra-abdominal contents into the thorax may be delayed or prevented until after extubation. For this reason, comparison between radiographs should be made from before and after cessation of positive pressure ventilation when possible in patients unable to be imaged by CT (Gao et al. 2015).
Although chest radiographs may be diagnostic for diaphragmatic injuries, they are generally inferior to CT images in their evaluation, with sensitivity not greater than 65 % (Gelman et al. 1991; Patlas et al. 2015). One potential pitfall in the diagnosis of diaphragmatic injuries by chest radiography is a normal-appearing (false-negative) radiograph in the setting of acute diaphragmatic injury, which may be present in 15 % of patients presenting with diaphragmatic rupture (Guth et al. 1995).
Differential considerations must be kept in mind when nonspecific findings are present in the setting of acute thoracoabdominal trauma. Congenital hernias can also mimic traumatic herniation. Eventration of abdominal contents into the thoracic cavity can be mistaken for an acute finding if not recognized as nontraumatic. Other differential considerations for subtle abnormalities on chest radiographs may include atelectasis, pleural effusion, hemothorax, pulmonary contusion, pulmonary laceration, or phrenic nerve palsy (Gelman et al. 1991; Guth et al. 1995; Iochum et al. 2002).
6 CT Evaluation
Evaluation with MDCT is increasingly common, as are powerful workstations which allow review of reformatted images in a timelier manner. The maturation of CT technology, including MDCT, has improved CT scan sensitivity for blunt diaphragmatic injury from approximately 60 % with conventional CT scans to 77–100 % with MDCT, with MDCT specificity of approximately 93–98 % (Desser et al. 2010; Magu et al. 2012). The sensitivity of MDCT for penetrating diaphragmatic injuries is approximately 73–100 %, with specificity of approximately 50–92 % (Bodanapally et al. 2009; Dreizin et al. 2015).
7 CT Signs of Blunt Diaphragmatic Injury
Regarding blunt diaphragmatic rupture, Desir and Ghaye have classified signs into three groups: direct, indirect, and signs of uncertain or controversial origin (Desir and Ghaye 2012). Signs of blunt diaphragmatic injuries are described below using this classification.
Direct signs of blunt diaphragmatic rupture include the following:
-
Visualized diaphragmatic defect – A visualized defect of the diaphragm may demonstrate muscular retraction and thickening of diaphragmatic muscular fibers near the defect. A diaphragmatic injury is most easily visualized directly when air or fat abuts the diaphragm. This sign’s reported sensitivity and specificity range from approximately 17 to 90 % and 90 to 100 %, respectively, in the setting of blunt trauma (Desir and Ghaye 2012; Hammer et al. 2014):
-
Pitfalls: Eventration of the diaphragm may make the diaphragm imperceptible in some individuals (Desser et al. 2010). Fluid or soft tissue attenuation material (hemothorax, pleural effusion, ascites, lung consolidation, etc.) in contact with the diaphragm may obscure a true diaphragmatic injury; however, this may be less common when scanned by MDCT with a greater number of detectors (Chen et al. 2010; Patlas et al. 2015). Additionally, approximately 6 % of asymptomatic adults will have evidence of nontraumatic diaphragmatic defects, which mimic a focal injury in the setting of acute trauma (Iochum et al. 2002).
-
-
Dangling diaphragm sign (Desser et al. 2010) – The appearance of this sign overlaps with visualization of a diaphragmatic defect, as described above. This less commonly described sign refers to visualization of the free edge of the torn diaphragm curling inwards on itself, which appears as a comma-shaped soft tissue structure. Thickening of this free flap of the diaphragm has also been reported. Sensitivity and specificity of the dangling diaphragm sign are reported as 54 and 98 %, respectively (Desser et al. 2010):
-
Pitfalls: This sign’s pitfalls are similar to those of the visualized diaphragmatic defect.
-
-
Absent diaphragm – The diaphragm may be absent in the area of a diaphragmatic injury. When the diaphragm or a portion of the diaphragm is not visualized after acute injury, abdominal contents are commonly herniated. Absence of the visualized diaphragm has a reported sensitivity and specificity of 18–43 % and 91 %, respectively (Desir and Ghaye 2012):
-
Pitfalls: This sign’s pitfalls are similar to those of the visualized diaphragmatic defect.
Indirect signs of blunt diaphragmatic rupture may be the only evidence to suggest a blunt diaphragmatic injury:
-
-
Herniation through a defect – Herniation of abdominal contents into the abdomen may occur in the setting of trauma or as the result of either congenital or acquired diaphragmatic hernias. Abdominal contents may herniate into either the pleural or, less likely, the pericardial space. Reported sensitivity of herniated abdominal contents after blunt trauma is higher on the left than on the right (42–91 % on the left, 8–50 % on the right), while specificity is reportedly at 98–100 % (Desir and Ghaye 2012):
-
Pitfalls: Diaphragmatic hernias (e.g., Bochdalek or Morgagni hernias) are potential mimics of this sign, especially if prior imaging is not available to demonstrate the stable nature of the hernia.
-
-
Collar sign – This sign refers to a waist-like band constricting herniated abdominal contents as they pass from the abdomen to the thoracic cavity through the sometimes-not-visualized diaphragmatic defect. This sign may be best appreciated on reformatted sagittal or coronal images. Overall sensitivity and specificity for blunt diaphragmatic injury are reported as 44–63 % and 98–100 %, respectively, with sensitivity lower on the right (50 %) than on the left (78 %) (Killeen et al. 1999):
-
Pitfalls: Prior trauma or diaphragmatic slips may result in atypical contours of abdominal organs and may be mistaken for a collar sign (Desir and Ghaye 2012). The collar sign may also be present in congenital or acquired hernias. Motion artifact has caused an artifactually narrowed appearance of upper abdominal organs and the diaphragm, though this motion artifact is less likely with faster scan times.
-
-
Hump and band signs – These signs are a subset of the collar sign, primarily used in evaluating the right diaphragm. The “hump” being referenced is a focal outpouching of the liver which has herniated above the injured right diaphragm. The “band” refers to an area of hypoattenuation within the liver at the level of the diaphragmatic defect on contrast-enhanced studies (Rees et al. 2005). It is hypothesized that compression from the rim of the damaged diaphragm results in a rim of relative hypoperfusion of the liver at the site of herniation (Rees et al. 2005). Both the hump and band signs are best appreciated on coronal and sagittal reformatted images. While specificity for these signs has not been determined, sensitivity of the hump sign is reported to be 50–83 %, and sensitivity of the band sign is reported to be 33–42 % (Rees et al. 2005; Chen et al. 2010):
-
Pitfalls: Similar to the collar sign, prior hepatic laceration or fracture or diaphragmatic slips may be mistaken for a positive hump sign (Desir and Ghaye 2012). Also, because of their subtle nature when compared to the collar sign, these signs may be missed if only axial views are reviewed. They are more apparent on sagittal and coronal reformatted images. A congenitally high right hemidiaphragm may also mimic a hump sign.
-
-
Dependent viscera sign – When supine, the left hemidiaphragm normally suspends the stomach, spleen, and bowel above the posterior chest wall, while the right hemidiaphragm normally suspends the liver away from the posterior chest wall, each separated by posteroinferior portions of the lungs. When abdominal viscera are herniated into the pleural space, this support is no longer present, and the herniated abdominal contents can fall against the posterior chest wall (Cantwell 2006). In the setting of blunt trauma, sensitivity for this sign is reported as 54–90 %, with a reported specificity of practically 100 % (Bergin et al. 2001; Desser et al. 2010; Desir and Ghaye 2012):
-
Pitfalls: Patients with congenital or hiatal hernias may demonstrate this sign without acute injury. This sign has been reported to have a low sensitivity for small ruptures, atypically configured or anteriorly located ruptures or when pleural effusion is present (Bergin et al. 2001; Cantwell 2006; Desir and Ghaye 2012).
-
-
Abdominal contents peripheral to the diaphragm or lung – When the normal contour of the diaphragm is well visualized, abdominal contents may be seen outside this contour. If abdominal contents are seen outside the normal contour of the diaphragm, they will have herniated into the thoracic cavity. Sensitivity and specificity are not reported for this sign (Desir and Ghaye 2012):
-
Pitfalls: In the unlikely situation that the diaphragm was inverted (such as from a large effusion), this relationship may be abnormal (Desir and Ghaye 2012).
-
-
Elevated abdominal organs – Because many processes may result in discrepancies of the apparent heights of the right and left hemidiaphragm, unilateral elevation of abdominal organs into the thoracic cavity is insufficient to diagnose diaphragmatic rupture. When seen in conjunction with other features suggesting diaphragmatic rupture, elevation of abdominal organs into the thoracic cavity may help reassure the correct diagnosis. Although other values have also been suggested, a significant correlation has been shown between a 4 cm elevation of the right relative to the left hemidiaphragm and right-sided rupture. Overall sensitivity and specificity for a 4 cm diaphragmatic asymmetry are reported to be 50–83 % and 89–99 %, respectively (Desir and Ghaye 2012):
-
Pitfalls: Mimics of this sign may include phrenic nerve injury, atelectasis, or subpulmonic effusion.
-
-
Concomitant pneumothorax with pneumoperitoneum or hemothorax with hemoperitoneum – With the presence of either air or blood in both the thoracic and abdominal cavities, one should strongly consider diaphragmatic injury in the setting of trauma. Effusion or ascites may also pass between the thoracic and abdominal cavities in the setting of a damaged diaphragm (Desir and Ghaye 2012):
-
Pitfalls: It may be difficult to prove that the combination of pneumothorax with pneumoperitoneum or hemothorax with hemoperitoneum does not represent synchronous injuries within both cavities (Desir and Ghaye 2012).
Signs of uncertain or controversial origin:
-
-
Thickening of the diaphragm – Muscular fibers of the diaphragm may retract and thicken after diaphragmatic injury. The thickening of the diaphragm can vary in appearance, and no standard measurements for diaphragmatic thickness are established. In the setting of blunt diaphragmatic injury, overall sensitivity has been reported as 56–75 %, and specificity is reported to be approximately 95 % (Desir and Ghaye 2012):
-
Pitfalls: The diaphragm may be congenitally thickened due to unequal distribution of muscular fibers during embryologic migration. Additionally, blood or fluid accumulated near the diaphragm such as a retroperitoneal hematoma may mimic thickening of the diaphragm and incorrectly suggest a diaphragmatic injury (Nchimi et al. 2005; Desir and Ghaye 2012).
-
-
Diaphragmatic and peridiaphragmatic extravasation of contrast – Arterial contrast extravasation from the diaphragm is highly specific for diaphragmatic injury. Although sensitivity is low (reported between 0 and 12 %), specificity is reported between 93 and 98 % (Nchimi et al. 2005; Desser et al. 2010):
-
Pitfalls: This sign is nonspecific because extravasation of contrast can be difficult to localize to the diaphragm (and to exclude bleeding of adjacent organs) (Desir and Ghaye 2012).
-
-
Fractured rib or ribs – Rib fractures can suggest injury to the diaphragm by their size, position, and location. The relative location of a rib fragment may indicate it has crossed the surface of the adjacent diaphragm. Sensitivity and specificity of rib fractures in diagnosing diaphragmatic injury are unknown (Desir and Ghaye 2012).
8 CT Signs of Penetrating Diaphragmatic Injury
In the setting of penetrating trauma, contiguous injury to organs above and below the diaphragm is the most useful and accurate sign, with sensitivity and specificity of 82–100 % and 82–83 %, respectively (Bodanapally et al. 2009; Panda et al. 2014; Dreizin et al. 2015).
Direct visualization of a diaphragmatic defect in the setting of penetrating trauma has a broad range of reported sensitivities (7–100 %) (Panda et al. 2014; Dreizin et al. 2015); however, specificity is consistently high, reported in the range of 90–100 % (Bodanapally et al. 2009; Dreizin et al. 2015).
Thickening of the diaphragm near the area of penetrating injury, presumably due to retraction of muscle fibers from the site of injury, has a reported sensitivity of approximately 48–83 %, with specificity reported near 70 % (Bodanapally et al. 2009; Panda et al. 2014).
Although penetrating diaphragmatic injuries typically result in small diaphragmatic defects, a penetrating injury may result in a large diaphragmatic defect based on its trajectory. Any of the signs related to the larger blunt diaphragmatic injuries can be seen in the setting of a large defect. Because of this, signs related to herniation (collar sign, dependent viscera sign, herniation of abdominal contents into the thoracic cavity) tend to have low sensitivities and high specificities in the setting of penetrating trauma, as discussed below.
The collar sign also has low sensitivity in the range of 0–24 %, with specificity reported near 100 % (Bodanapally et al. 2009; Panda et al. 2014; Dreizin et al. 2015).
The dependent viscera sign may theoretically be seen in large defects associated with penetrating trauma, but was not reported in two recent studies (Bodanapally et al. 2009; Dreizin et al. 2015).
Sensitivity of herniation of abdominal fat or viscera into the thoracic cavity in the setting of penetrating trauma is approximately 7–17 %, and specificity approaches 100 % (Bodanapally et al. 2009; Patlas et al. 2015).
Concurrent hemothorax and hemoperitoneum have a sensitivity of 50 % and a specificity of 95 % for penetrating abdominal injuries (Nchimi et al. 2005).
The reported sensitivity for the dangling diaphragm sign is 0–17 %, without reported specificity (Panda et al. 2014; Dreizin et al. 2015). In describing the dangling diaphragm sign, Desser et al. acknowledged that it would be less likely in penetrating trauma (Desser et al. 2010).
Active extravasation of contrast in or along the diaphragm has a sensitivity of 8 % and a specificity of 100 % (Dreizin et al. 2015).
9 Additional Pitfalls in CT Imaging
Although herniation of intra-abdominal contents is not needed to diagnose diaphragmatic injury, it does represent a potential complication of both blunt and penetrating diaphragmatic injuries. As was previously mentioned, herniation of abdominal viscera into the thoracic cavity can be prevented or delayed due to positive pressure ventilation. Positive pressure ventilator assistance is commonly needed as part of the supportive measures implemented after major trauma.
Additionally, herniation or eventration of abdominal organs such as the liver, spleen, or bowel through a thinned diaphragm may mimic a traumatic injury and should be correlated to prior imaging if available (Iochum et al. 2002). In cases of eventration, close examination of the margins of the diaphragm may demonstrate a faint line that corresponds to the thinned diaphragm overlying the eventrated organs.
10 MRI Evaluation
The use of MRI in an acute trauma setting is usually impractical because of patient hemodynamic instability and resuscitative medical equipment incompatibility. MRI can be successfully used in cases of equivocal initial imaging in hemodynamically stable patients, late presentation of a diaphragmatic injury, or suspicion of a chronic diaphragmatic injury (Killeen et al. 1999; Barbiera et al. 2003).
One benefit of using MRI to evaluate the diaphragm is the ability to image directly in coronal and sagittal planes without needing to rely on reconstructions, as is the case with CT (Killeen et al. 1999; Iochum et al. 2002). Directly imaged sagittal and coronal planes allow appreciation of the contrast between the mediastinal or the abdominal fat and the low-signal band of the diaphragm itself. Diaphragmatic injuries can be diagnosed by visualization of diaphragmatic defects directly or by visualizing herniation of fat across the diaphragm. It has been suggested that T1 imaging in sagittal and coronal planes may be enough to clearly contrast the fat of the mediastinum and abdominal cavity to the hypointense band of the diaphragm and may be sufficient to diagnose defects of the diaphragm (Shanmuganathan et al. 1996; Killeen et al. 1999).
As with CT, MR imaging signs of diaphragmatic injury include disruption of the diaphragmatic contour or intrathoracic herniation of abdominal contents, such as viscera or fat (Iochum et al. 2002; Barbiera et al. 2003). At least one small series has demonstrated the ability to diagnose diaphragmatic injuries as small as 1 cm (Barbiera et al. 2003).
Many of the same findings described in the above CT signs of diaphragmatic injury may apply equally well to MR imaging. Diaphragmatic discontinuity and herniation of fat or viscera have been commonly reported together in cases detected with MR imaging (Shanmuganathan et al. 1996; Barbiera et al. 2003). Any of the signs which rely on the physical relationships of the thoracic and abdominal organs (e.g., the collar sign, directly visualized defect of the diaphragm, herniation of abdominal viscera into the thoracic cavity, or diaphragmatic extravasation of contrast) may be equally applicable to MR and CT imaging; however, the sensitivity and specificity of these signs in MR imaging have not yet been clarified. In a small series of patients with equivocal imaging findings, the sensitivity and specificity of MRI in detecting diaphragmatic injuries were both 100 % (Shanmuganathan et al. 1996).
11 Ultrasound
Little has been published on the sonographic diagnosis of diaphragmatic rupture; however, there are case reports that suggest its potential during focused assessment with sonography in trauma (FAST) exams (Blaivas et al. 2004; Kirkpatrick et al. 2006; Gangahar and Doshi 2010). Findings during FAST or modified FAST exams which have been demonstrated in the setting of proven traumatic diaphragmatic injuries include elevation of the diaphragm, poor diaphragmatic excursion, replacement of the expected sliding of the lung by the liver in the lower chest (liver sliding sign), or organs being either obscured or apparently absent on FAST exam due to anatomic distortions in the setting of herniation (Rip’s absent organ sign) (Blaivas et al. 2004; Kirkpatrick et al. 2006; Gangahar and Doshi 2010). No significant statistical data on the sonographic diagnosis of diaphragmatic injury is available.
Potential pitfalls with sonographic evaluation of the diaphragm in the acute setting include non-acute causes of diaphragmatic dysfunction and eventration of the diaphragm (Blaivas et al. 2004; Kirkpatrick et al. 2006). The nonvisualization of organs is also a nonspecific finding in ultrasonography and can be attributable to other causes such as COPD, obesity, or dextrocardia (Gangahar and Doshi 2010).
Conclusion
Diaphragmatic injuries are caused by penetrating and blunt trauma, both of which are frequently associated with additional traumatic injuries. Both radiologists and surgeons, especially in the setting of life-threatening injuries, miss diaphragmatic injuries. A missed diaphragmatic injury puts a patient at risk of delayed injury and complications such as strangulation, with potentially disastrous consequences. Selective nonoperative management is becoming more common in management of both blunt and penetrating trauma. In order to ensure that diaphragmatic injuries are not missed, radiologists should be familiar with the signs or diaphragmatic injury and should have a high degree of suspicion in the setting of blunt or penetrating trauma. Comparison to prior imaging may help differentiate chronic or congenital mimics of diaphragmatic injury. The proliferation of MDCT and increasing use of multiplanar reconstructions have also made the evaluation for diaphragmatic injuries more accurate and reliable and should always be employed.

A 62-year-old man who was struck by a car: Computed tomography (CT) images demonstrate the absence of the interposition of lungs between the upper abdominal contents and the chest wall consistent with the dependent viscera sign (arrow). There is intrathoracic herniation of abdominal viscera as demonstrated by visualization of abdominal organs within the pleural space (circle). Additionally, coronal reconstructions demonstrate elevation of left-sided abdominal contents above the left diaphragmatic dome (line)

A 62-year-old man who was struck by a car: Computed tomography (CT) image demonstrates the tear in the diaphragm results in a waist-like constriction of the stomach (image C arrowheads). These findings are representative of the collar sign. The patient’s CT findings of a left diaphragmatic rupture were confirmed at surgery

A 25-year-old who suffered a motor vehicle collision: CT images demonstrate a linear band of hypoattenuation through the liver, the band sign (images A and B, dashed line). Once again, we see abdominal organs located within the left pleural space (image A, circle) and the dependent viscera sign (image A, arrow). Abdominal contents are located above the level of the diaphragm (image B, arrowheads). The patient’s CT findings of bilateral diaphragmatic rupture were confirmed at surgery. Bilateral diaphragmatic injury can occur in 5–8 % of cases of blunt trauma with diaphragmatic injury. Consequently, a careful inspection of the contralateral hemidiaphragm should be pursued once a diaphragmatic injury is found

A 33-year-old in motor vehicle collision: Axial CT images demonstrate the dangling diaphragm sign as evidenced by the inward curling of the diaphragm from its normal course (images A and B, arrows). Additionally, there is thickening of the injured diaphragm (images A and B, arrows). The collar sign is also present (images A and B, arrowheads)

A 33-year-old in motor vehicle collision: The topogram demonstrates apparent elevation of the left hemidiaphragm (image C, dashed line). The coronal CT reformations confirm elevated abdominal organs within the left thorax ≥4 cm above the level of the level of the right diaphragmatic dome (image D, dashed line). Diaphragmatic rupture was confirmed at surgery

A 47-year-old man stabbed in the left flank: Axial CT images demonstrate contiguous injuries above and below the diaphragm which raise the suspicion of diaphragmatic injury. There is a left hemothorax (image A, arrow), hemoretroperitoneum with blood tracking along the gastrosplenic ligament (image B, arrow), and a focus of free gas abutting the spleen (image A, arrowhead)

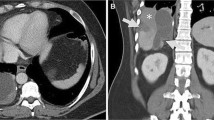
A 34-year-old man with gunshot wound to the right chest: Axial CT images demonstrate a pulmonary contusion (image B, circle), hemothorax (image A, arrow), and hepatic laceration (image A, arrowhead). Contiguous injury on both sides of the diaphragm suggests diaphragmatic injury

A 34-year-old man with gunshot wound to the right chest: Multiplanar reconstruction demonstrates the wound tract (image C, dashed line) traversing the right hemidiaphragm with injuries on both sides of the diaphragm. This case illustrates the value of coronal images to find the wound tract. The patient’s diaphragmatic injury was confirmed at surgery

A 21-year-old man with gunshot wound to the right chest: Axial CT image shows a liver laceration with active extravasation of contrast (image A, arrow) and an associated subcapsular hematoma. Axial lung windows demonstrate a pulmonary contusion (image A, arrowhead) and trace pneumothorax. Illustrative wound tracts of metallic shot pellets traverse the right hemidiaphragm. No diaphragmatic discontinuities are seen on CT, but these findings are consistent with diaphragm laceration

A 21-year-old man with gunshot wound to the right chest: Once again we see the benefit of multiplanar reformations. Coronal images show that the wound tract (dashed line) courses through the right hemidiaphragm. Contiguous injury above and below the right hemidiaphragm was also demonstrated as lung injury from the bullet tract can be seen above the diaphragm (arrow) and active extravasation within the liver is seen along the path of the shot (arrowhead). Right diaphragmatic injury was confirmed at surgery

A 28-year-old man with a gunshot wound to the left upper quadrant: Axial images demonstrate pulmonary contusion. The bullet tract (images A and B, dashed line) traverses the left hemithorax and left upper quadrant. The wound tract (image C, dashed line) also courses inferiorly through the abdomen, and there is evidence of hemoperitoneum (arrowhead). Contiguous injuries above and below the diaphragm are concerning for diaphragmatic injury. Sagittal reformations show the wound tract (image D, dashed line) coursing from above the diaphragm into the abdomen. Left diaphragmatic injury was confirmed at surgery

GSW with tract through the upper abdomen; image shows active extravasation from hepatic laceration (arrow) and below the left hemidiaphragm (arrowhead)

MVC with large right diaphragmatic defect, herniation of the liver into the left thorax, band, and collar signs
References
Barbiera F, Nicastro N, Finazzo M, Lo Casto A, Runza G, Bartolotta TV, Midiri M (2003) The role of MRI in traumatic rupture of the diaphragm. Our experience in three cases and review of the literature. Radiol Med 105(3):188–194
Bergin D, Ennis R, Keogh C, Fenlon HM, Murray JG (2001) The “dependent viscera” sign in CT diagnosis of blunt traumatic diaphragmatic rupture. AJR Am J Roentgenol 177(5):1137–1140
Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K (2004) Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma. Am J Emerg Med 22(7):601–604
Bodanapally UK, Shanmuganathan K, Mirvis SE, Sliker CW, Fleiter TR, Sarada K, Miller LA, Stein DM, Alexander M (2009) MDCT diagnosis of penetrating diaphragm injury. Eur Radiol 19(8):1875–1881
Cantwell CP (2006) The dependent viscera sign. Radiology 238(2):752–753
Chen HW, Wong YC, Wang LJ, Fu CJ, Fang JF, Lin BC (2010) Computed tomography in left-sided and right-sided blunt diaphragmatic rupture: experience with 43 patients. Clin Radiol 65(3):206–212
Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, Ivatury RR, Scalea TM (2010) Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 68(3):721–733
Croce MA, Fabian TC, Menke PG, Waddle-Smith L, Minard G, Kudsk KA, Patton JH Jr, Schurr MJ, Pritchard FE (1995) Nonoperative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients. Results of a prospective trial. Ann Surg 221(6):744–753; discussion 753–745
Desir A, Ghaye B (2012) CT of blunt diaphragmatic rupture. RadioGraphics 32(2):477–498
Desser TS, Edwards B, Hunt S, Rosenberg J, Purtill MA, Jeffrey RB (2010) The dangling diaphragm sign: sensitivity and comparison with existing CT signs of blunt traumatic diaphragmatic rupture. Emerg Radiol 17(1):37–44
Dreizin D, Bergquist PJ, Taner AT, Bodanapally UK, Tirada N, Munera F (2015) Evolving concepts in MDCT diagnosis of penetrating diaphragmatic injury. Emerg Radiol 22(2):149–156
Fair KA, Gordon NT, Barbosa RR, Rowell SE, Watters JM, Schreiber MA (2015) Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: a new examination of a rare diagnosis. Am J Surg 209(5):864–868; discussion 868–869
Gangahar R, Doshi D (2010) FAST scan in the diagnosis of acute diaphragmatic rupture. Am J Emerg Med 28(3):387.e381–383
Gao JM, Du DY, Li H, Liu CP, Liang SY, Xiao Q, Zhao SH, Yang J, Lin X (2015) Traumatic diaphragmatic rupture with combined thoracoabdominal injuries: difference between penetrating and blunt injuries. Chin J Traumatol 18(1):21–26
Gelman R, Mirvis SE, Gens D (1991) Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. AJR Am J Roentgenol 156(1):51–57
Guth AA, Pachter HL, Kim U (1995) Pitfalls in the diagnosis of blunt diaphragmatic injury. Am J Surg 170(1):5–9
Hammer MM, Flagg E, Mellnick VM, Cummings KW, Bhalla S, Raptis CA (2014) Computed tomography of blunt and penetrating diaphragmatic injury: sensitivity and inter-observer agreement of CT Signs. Emerg Radiol 21(2):143–149
Hanna WC, Ferri LE, Fata P, Razek T, Mulder DS (2008) The current status of traumatic diaphragmatic injury: lessons learned from 105 patients over 13 years. Ann Thorac Surg 85(3):1044–1048
Iochum S, Ludig T, Walter F, Sebbag H, Grosdidier G, Blum AG (2002) Imaging of diaphragmatic injury: a diagnostic challenge? RadioGraphics 22(Suppl 1):S103–S116
Killeen KL, Mirvis SE, Shanmuganathan K (1999) Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol 173(6):1611–1616
Kirkpatrick AW, Ball CG, Nicolaou S, Ledgerwood A, Lucas CE (2006) Ultrasound detection of right-sided diaphragmatic injury; the “liver sliding” sign. Am J Emerg Med 24(2):251–252
Leung VA, Patlas MN, Reid S, Coates A, Nicolaou S (2015) Imaging of Traumatic Diaphragmatic Rupture: Evaluation of Diagnostic Accuracy at a Level 1 Trauma Centre. Can Assoc Radiol J 66(4):310–317
Magu S, Agarwal S, Singla S (2012) Computed tomography in the evaluation of diaphragmatic hernia following blunt trauma. Indian J Surg 74(4):288–293
Murray JG, Caoili E, Gruden JF, Evans SJ, Halvorsen RA Jr, Mackersie RC (1996) Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. AJR Am J Roentgenol 166(5):1035–1039
Nchimi A, Szapiro D, Ghaye B, Willems V, Khamis J, Haquet L, Noukoua C, Dondelinger RF (2005) Helical CT of blunt diaphragmatic rupture. AJR Am J Roentgenol 184(1):24–30
Panda A, Kumar A, Gamanagatti S, Patil A, Kumar S, Gupta A (2014) Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagn Interv Radiol 20(2):121–128
Patlas MN, Leung VA, Romano L, Gagliardi N, Ponticiello G, Scaglione M (2015) Diaphragmatic injuries: why do we struggle to detect them? Radiol Med 120(1):12–20
Reber PU, Schmied B, Seiler CA, Baer HU, Patel AG, Buchler MW (1998) Missed diaphragmatic injuries and their long-term sequelae. J Trauma Inj Infect Crit Care 44(1):183–188
Rees O, Mirvis SE, Shanmuganathan K (2005) Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clin Radiol 60(12):1280–1289
Shanmuganathan K, Mirvis SE, White CS, Pomerantz SM (1996) MR imaging evaluation of hemidiaphragms in acute blunt trauma: experience with 16 patients. AJR Am J Roentgenol 167(2):397–402
Shatney CH, Sensaki K, Morgan L (2003) The natural history of stab wounds of the diaphragm: implications for a new management scheme for patients with penetrating thoracoabdominal trauma. Am Surg 69(6):508–513
Spann JC, Nwariaku FE, Wait M (1995) Evaluation of video-assisted thoracoscopic surgery in the diagnosis of diaphragmatic injuries. Am J Surg 170(6):628–630; discussion 630–621
Standring S (2016) Diaphragm and phrenic nerves. Gray’s anatomy. S. Standring, Elsevier, UK, pp 970–975
Thomas Sadler JL, Langman J, Sadler-Redmond SL, Sulik KK (2003) Langman’s medical embryology. Lippincott Williams & Wilkins, Philadelphia, PA
Yucel M, Bas G, Kulali F, Unal E, Ozpek A, Basak F, Sisik A, Acar A, Alimoglu O (2015) Evaluation of diaphragm in penetrating left thoracoabdominal stab injuries: the role of multislice computed tomography. Injury 46(9):1734–1737
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Olsen, A., Nicola, R., Raptis, C., Patlas, M. (2016). Traumatic Diaphragmatic Injuries. In: Scaglione, M., Linsenmaier, U., Schueller, G., Berger, F., Wirth, S. (eds) Emergency Radiology of the Chest and Cardiovascular System. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/174_2016_42
Download citation
DOI: https://doi.org/10.1007/174_2016_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42582-5
Online ISBN: 978-3-319-42584-9
eBook Packages: MedicineMedicine (R0)