Abstract
This article reviews current and evolving concepts in the diagnosis of penetrating diaphragmatic injury with multidetector CT (MDCT). As criteria for nonoperative management in the setting of penetrating trauma become more inclusive, confident exclusion of penetrating diaphragmatic injury (PDI) has become imperative. Diagnostic performance of MDCT for PDI has improved substantially with the use of thin sections and multiplanar reformats. Evaluation of injury trajectory in nonstandard planes using 3D post-processing software can aid in the diagnosis. Contiguous injury and transdiaphragmatic trajectory are the best predictors of PDI. Careful appraisal of the diaphragm for defects should be undertaken in all patients with thoracoabdominal penetrating trauma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multidetector CT (MDCT) remains the first-line imaging modality for screening hemodynamically stable victims of penetrating torso trauma. Injuries to the thoracoabdominal region, defined as the area below the nipple line and above the inferior costal margins, make up a significant proportion of these penetrating torso trauma cases, and diaphragmatic injuries are often encountered in this cohort. The clinical relevance of penetrating diaphragmatic injury (PDI) has increased with the growing emphasis on selective nonoperative management (NOM) in penetrating trauma. Powell et al. retrospectively examined a group of patients selected for NOM based on benign abdominal exam and hemodynamic stability who went on to diagnostic laparoscopy. Of these patients, 20 % were found to have a diaphragmatic injury [1]. Another retrospective study examining 97 patients with thoracoabdominal stab wounds with no urgent need for laparotomy found an occult diaphragmatic injury rate of 7 % overall, with a rate of 17 % in the subgroup of patients with left-sided injury, possibly reflecting the protective effect of the liver on the diaphragm [2].
PDI is a distinct entity from blunt diaphragmatic rupture (BDR). Defects are often small, and in the early post-injury period when patients are likely to undergo CT, there is usually simple breach of the diaphragm without herniation [3, 4]. This is in contrast to the large rents typically seen in BDR [3, 5–10]. Findings of PDI can be quite subtle at CT, and diagnosis remains a challenge.
PDIs and NOM of penetrating torso trauma
Carte blanche laparotomy for patients with penetrating injury in the thoracoabdominal region leads to a large number of nontherapeutic laparotomies, with rates of complications ranging from 8.7 to 20.4 % [11]. As such, trauma surgeons increasingly favor selective NOM in a significant proportion of patients with knife wounds who lack peritoneal signs [11–14] and in a subset of patients with transabdominal wounds from gunshot trauma [15, 16]. PDIs are often clinically occult, but because of the pressure gradient between abdominal and thoracic cavities, can increase in size over widely variable periods of time. Delayed presentations can occur months to years after injury. Devastating outcomes can result from incarceration and strangulation of abdominal viscera, with a reported mortality of 20–25 % [17, 18]. Therefore, patients with penetrating thoracoabdominal trauma should be assumed to harbor a diaphragmatic injury until proven otherwise.
Conservative management requires confident exclusion of these and other surgically important injuries. Prospective studies evaluating patients with penetrating thoracoabdominal injuries found CT to have a sensitivity of 90.5–98 % and specificity of 90–96 % for identifying clinically significant organ injury or need for laparotomy [14, 19, 20]. But, the accuracy and reliability of CT for diagnosis of PDIs have been less favorable, with a wide range of sensitivities between 14 and 94 % [9, 21, 22]. The diaphragm is a thin sloping structure that is not well appreciated on conventional thick section axial images, and significant improvements in diagnostic performance have been described employing thinner sections and multiplanar reformats in conventional and nonstandard planes [9, 21, 23]. In more recent studies, sensitivities of 73–100 % and overall accuracies of 70–89 % have been reported [9, 23]. Highly sensitive predictors are needed to exclude PDI, and herniation-related signs are typically absent. Because of this, recent studies have also focused on the ability of CT to detect direct and indirect signs of simple diaphragmatic breach [9, 23, 24].
CT protocol
Victims of penetrating torso trauma who are hemodynamically unstable or have overt signs of peritonitis are not candidates for NOM and are taken directly for exploration. Hemodynamically stable patients with penetrating thoracoabdominal trauma are usually scanned at our institution using a triple contrast protocol, with oral, rectal, and intravenous contrast. A total of 600 ml of 2 % sodium diatrizoate (Hypaque sodium; Nycomed, Princeton NJ) is administered 30 min prior to and then immediately before CT. A typical 64-section MDCT triple contrast protocol for penetrating injury involves acquisition of a single sweep arterial phase scan from the thoracic inlet through the symphysis pubis (Fig. 1) following administration of 100 ml of IV contrast at 4 ml/s through an 18–20 gauge cannula in an antecubital vein. This is performed to screen for vascular and hollow visceral injuries and is followed by a portal venous phase scan of the upper abdomen, for better appreciation of parenchymal injury to the solid organs. Arterial and portal venous phase scans can be acquired using fixed delays of 30 and 70 s, respectively [23]. Images are acquired using 0.625-mm collimation and reconstructed with 50 % overlap at 3 mm for interpretation and 2 mm for 3D post-processing. Coronal and sagittal multiplanar reformats are routinely generated by the technologist, and additional post-processing is performed by the radiologist using thin client software (TeraRecon, Inc., Foster City, CA) which is available at all workstations.
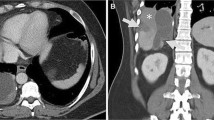
Coronal reformatted arterial phase image from penetrating torso trauma protocol MDCT in an 18-year-old gunshot trauma victim. The patient was deemed hemodynamically stable at admission and had not developed peritoneal signs by the time CT was performed. Extravasated oral and rectal contrast is seen resulting from the multiple GI tract injuries to the cecum, sigmoid, and transverse colon, jejunum, stomach, and left hemidiaphragm. b A discrete diaphragmatic defect was not seen in this patient. However, the presence of contrast and blood on both sides of the left hemidiaphragm was highly suggestive of diaphragmatic injury (arrow). In the presence of multiple injuries, this sign is sensitive but not specific. In this case, because contrast was found on the thoracic surface of the diaphragm, PDI was suspected at CT and subsequently confirmed and repaired during exploratory laparotomy. Diaphragmatic injuries are sometimes missed during exploration in patients with multiple injuries
Multiplanar reconstructions
With high-quality coronal and sagittal images, the diagnostic value of MDCT for evaluating PDI has increased dramatically [9, 21]. Because of the high incidence of PDI in thoracoabdominal penetrating trauma, any penetrating injury occurring below the nipple line or above the costal margin warrants a careful evaluation of the diaphragm in multiple planes. An appropriate index of suspicion and careful evaluation in multiple planes is likely responsible for the learning curve seen in the diagnosis of these injuries, which is more often made by experienced trauma radiologists [23, 25]. The combination of decreased respiratory motion and near isotropic resolution made possible by 64-section and higher CT scanners has further improved our ability to resolve these injuries with conventional multiplanar reconstructions (MPRs) and allows additional problem solving in nonstandard planes by evaluating thin section images using post-processing software as needed.
Signs of PDI
Signs of PDI can be grouped into two main categories—those that are herniation-related and those seen in simple breach. Published ranges of sensitivities and specificities for both types of signs in penetrating trauma are shown in Table 1.
Herniation-related signs
Herniation-related signs are also referred to as “BDR-related” by some authors because they are more commonly seen in blunt trauma [26], but all of these signs are also seen in PDIs with sufficiently large defects, and the term “herniation-related” is more inclusive [25]. Herniation-related signs include collar sign, dependent viscera, hump sign, and dangling diaphragm. These signs are highly specific but notably insensitive in the setting of penetrating trauma, as herniation is often not apparent given the typically small defect size.
Collar sign
Collar sign is defined as an area of constriction at the level of the diaphragm around the herniated contents, which usually contain hollow viscera (Fig. 2a) or outpouchings of fat [10, 22, 27].
a Collar sign. Coronal thick slab image in a 21-year-old stabbing victim. The injured left hemidiaphragm (arrows) is constricted around herniated stomach and colon. The diaphragmatic injury had propagated to 10 cm in length at exploratory laparotomy. The stomach and transverse colon were reduced, and the diaphragmatic injury was repaired. b Dependent viscera sign. Axial thick slab image in the same patient shows the stomach (star) abutting the posterior ribs
Dependent viscera sign
In the supine position, the posterior diaphragm supports the abdominal viscera. If a diaphragmatic injury is present, the abdominal viscera (usually the stomach or bowel) are no longer supported and fall dependently against the posterior ribs [28] (Fig. 2b).
Hump sign/band sign
Hump and band signs are variations of collar sign and are seen in the setting of herniation of the liver through the right hemidiaphragm. The hump sign refers to a focal abnormality of the normal contour of the right hemidiaphragm related to bulging of the liver parenchyma through the site of diaphragmatic injury. The band sign describes a linear ring of low attenuation involving the liver parenchyma at the site of diaphragmatic breech, thought to be due to decreased perfusion from constriction at the narrow region of herniation [10, 27]. Herniation of viscera is less likely through right-sided diaphragmatic defects because of the protective effect of the liver; however, ventilation can be impaired when herniated liver causes significant decreases in lung volume. For this reason, right-sided defects are repaired selectively.
Dangling diaphragm sign
Dangling diaphragm is usually seen with large diaphragmatic defects. The free edges of the diaphragm near the defect are retracted and take on a curled appearance, as if they were freely dangling. Dangling diaphragm, hump sign, and band sign have not been independently evaluated in penetrating trauma but are known to occur in this setting [29] (Fig. 3).
Signs of simple breach
Because herniation-related signs are specific but usually absent in PDI, a number of authors have attempted to elucidate findings that are sensitive in this setting. Thickening of the diaphragm is neither sensitive nor specific [9], and active arterial extravasation along the diaphragm is an insensitive indirect sign [22], both of which lack clinical utility. CT trajectograms showing a missile or knife track traversing the diaphragm were first evaluated as a sign of simple breach by Larici et al. using single-slice helical CT [22]. The thick section images and correspondingly poor quality of reconstructions by today’s standards led to suboptimal results (sensitivity 36 %).
A sign described initially by Shanmuganathan et al. in 2004 [30] called “contiguous injury on both sides of the diaphragm”—now simply referred to as contiguous injury—serves as an indirect but more sensitive surrogate of transdiaphragmatic injury [23], a sort of “poor man’s trajectogram.” The sign is positive when there is organ laceration, blood, gas, shrapnel, or other evidence of injury immediately adjacent to both sides of the diaphragm (Figs. 1b and 4). This may be along an injury trajectory or may be more diffuse, such as hemothorax and hemoperitoneum spanning the length of the diaphragm [23]. Contiguous injury was evaluated by Bodanapally et al. but only for patients with single penetrating wounds [9]. Multiple injuries above and below the diaphragm can result in the sign appearing positive even though the diaphragm itself remains intact. A more recent study concluded that while contiguous injury is sensitive regardless of whether there are single or multiple wounds, it is no longer specific in the setting of multiple entry wounds [23]. While only a high sensitivity is needed to confidently exclude these injuries, specificity is also valuable because it allows the radiologist to pinpoint the diaphragmatic injury for the trauma surgeon prior to repair [23]. In the chaotic trauma setting, these are sometimes missed at laparotomy. Diaphragmatic injuries can also be missed laparoscopically, particularly in posterior locations [1, 31–38].
Contiguous injury. Axial CT image in a 29-year-old patient with PDI from a right thoracoabdominal stab wound. Hemothorax and hemoperitoeneum abut both sides of the right hemidiaphragm (arrows). Lacerated posterior right lobe of the liver and foci of free air are also demonstrated. The patient underwent repair of the PDI. No other surgically important injury during exploration
With 64-section and higher MDCT, the sensitivity of CT trajectograms has increased substantially. Near isotropic resolution allows improved visualization and characterization of both gunshot and knife wound tracks, particularly when viewed along their lengths using double oblique planes (Figs. 5 and 6), which can be rapidly generated using 3D post-processing software [23]. This technique, which we refer to as CT trajectography (CTT), as well as associated pitfalls have recently been described by independent groups in both civilian and wartime penetrating torso trauma [23, 39–42]. The high sensitivity of contiguous injury has been confirmed in several studies [9, 23, 24], and its absence may be a reliable indicator for excluding diaphragmatic injury in patients who may otherwise be candidates for NOM.
a, b Orthogonal double oblique CT trajectographic images in a 19-year-old patient with gunshot wound show transdiaphragmatic trajectory at two points of the right hemidiaphragm, one anteriorly and one posteriorly (arrows). The patient was managed conservatively without complication. A HIDA scan was performed that showed no bile leak or biliary pleural fistula
MDCT pitfalls
Evaluation of wound tracks can be misleading on axial images as these may appear to traverse the diaphragm even though on conventional MPRs or CTT; the path can be shown to cross just above or below it. The distinction is also important for appropriate operative sequencing (i.e., initial laparotomy or thoracotomy).
The diaphragm consists of a central aponeurosis and peripheral muscular portion which inserts anteriorly at the xiphoid process, laterally at the costal margins, and posteriorly on the upper lumbar vertebrae. The diaphragm blends with the abdominal wall musculature at its insertion. Wound tracks crossing through this portion result in “corner injuries” that may or may not involve the free diaphragm; the need for surgical repair of these injuries can be difficult to establish with CT [25] (Fig. 7).
Double oblique CT trajectogram in a 24-year-old patient with thoracoabdominal gunshot wound. On the right, it is unclear whether the bullet track crosses the free diaphragm or whether the injury is inferior to its muscular attachment to the body wall. Both left and right hemidiaphragmatic injuries were confirmed at surgery. A gastric wound was also present which was repaired, and argon beam coagulation was used to repair the through-and-through liver injury
Knife wound tracks can be very difficult to appreciate on thick sections due to volume averaging. Even on thin sections, knife wounds can appear discontinuous, and the trajectory may have to be extrapolated when possible [25]. The tracks may appear to terminate close to the diaphragm, without obviously traversing it (Fig. 8). A careful appraisal of the diaphragm may reveal a small defect in positive cases [25]. No study to date has specifically evaluated diagnostic accuracy for PDI in the subset of patients with stab wounds.
Double oblique CT trajectogram along a knife wound track in a 31-year-old patient with left PDI from thoracoabdominal stab wound. The track extended to but not beyond the hemidiaphragm (a). A diaphragmatic defect seen near the end of the track is shown to better advantage on the coned down axial image (b). A small diaphragmatic rent was found intra-operatively and repaired
Trajectories may appear not to follow a straight course when the phase of respiration at the time of the injury is different than during the scan or as a result of arm elevation (Fig. 9). This may lead to apparent track discontinuity or false curvature. Ricochet off of bone can also dramatically alter the wound path. Curving trajectories may result from bullet yaw or tumbling (Fig. 10). Conceivably, shockwave and cavitation around the path of a gunshot wound can transmit to the opposite side of the diaphragm, resulting in contiguous injury even though the diaphragm itself may remain intact [9]. Transdiaphragmatic trajectory can also be obscured or displaced by neighboring more diffuse manifestations of penetrating injury such as hemoperitoneum, hemothorax, pneumothorax, injury related to chest tube insertion, or extravasated luminal contrast from perforated bowel [23, 25].
Preexisting diaphragmatic defects can be mistaken for PDIs. Small regions of discontinuity in the diaphragm have been described as incidental findings in postmortem subjects and appear to occur with increased incidence in patients with emphysema [43].
Conclusion
As criteria for NOM becomes more inclusive, confident exclusion of PDI has become imperative. Older studies describing low diagnostic accuracy of CT for PDI are not applicable to the current state of thin section MDCT. Contiguous injury and transdiaphragmatic trajectory are the best predictors of PDI. Careful appraisal of the diaphragm for defects should be undertaken in all patients with thoracoabdominal penetrating trauma.
References
Powell BS, Magnotti LJ, Schroeppel TJ et al (2008) Diagnostic laparoscopy for the evaluation of occult diaphragmatic injury following penetrating thoracoabdominal trauma. Injury 39:530–534
Leppäniemi A, Haapiainen R (2003) Occult diaphragmatic injuries caused by stab wounds. J Trauma Acute Care Surg 55:646–650
Aboutanos M, Duane T, Malhotra A, Ivatury R (2007) Diaphragm. In: Britt LDTD, Feliciano DV (eds) Acute care surgery: principles and practice. Springer, New York
Shatney CH, Sensaki K, Morgan L (2003) The natural history of stab wounds of the diaphragm: implications for a new management scheme for patients with penetrating thoracoabdominal trauma. Am Surg 69:508–513
Dreizin D, Munera F (2012) Blunt polytrauma: evaluation with 64-section whole-body CT angiography. RadioGraphics 32:609–631
Desir A, Ghaye B (2012) CT of blunt diaphragmatic rupture. RadioGraphics 32:477–498
Iochum S, Ludig T, Walter F, Sebbag H, Grosdidier G, Blum AG (2002) Imaging of diaphragmatic injury: a diagnostic challenge? RadioGraphics 22:S103–S116
Shackleton KL, Stewart ET, Taylor AJ (1998) Traumatic diaphragmatic injuries: spectrum of radiographic findings. RadioGraphics 18:49–59
Bodanapally U, Shanmuganathan K, Mirvis S et al (2009) MDCT diagnosis of penetrating diaphragm injury. Eur Radiol 19:1875–1881
Sliker CW (2006) Imaging of diaphragm injuries. Radiol Clin N Am 44:199–211
Como JJ, Bokhari F, Chiu WC et al (2010) Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 68:721–733
Demetriades D, Hadjizacharia P, Constantinou C et al (2006) Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg 244:620–628
Inaba K, Demetriades D (2007) The nonoperative management of penetrating abdominal trauma. Adv Surg 41:51–62
Velmahos GC, Constantinou C, Tillou A, Brown CV, Salim A, Demetriades D (2005) Abdominal computed tomographic scan for patients with gunshot wounds to the abdomen selected for nonoperative management. J Trauma 59:1155–1160, discussion 1160–1151
Ginzburg E, Carrillo EH, Kopelman T et al (1998) The role of computed tomography in selective management of gunshot wounds to the abdomen and flank. J Trauma 45:1005–1009
Melo EL, de Menezes MR, Cerri GG (2012) Abdominal gunshot wounds: multi-detector-row CT findings compared with laparotomy: a prospective study. Emerg Radiol 19:35–41
Hegarty M, Bryer J, Angorn I, Baker L (1978) Delayed presentation of traumatic diaphragmatic hernia. Ann Surg 188:229–233
Degiannis E, Levy R, Sofianos C, Potokar T, Florizoone MG, Saadia R (1996) Diaphragmatic herniation after penetrating trauma. Br J Surg 83(1):88–91
Múnera F, Morales C, Soto JA et al (2004) Gunshot wounds of abdomen: evaluation of stable patients with triple-contrast helical CT. Radiology 231:399–405
Ramirez RM, Cureton EL, Ereso AQ et al (2009) Single-contrast computed tomography for the triage of patients with penetrating torso trauma. J Trauma Acute Care Surg 67:583–588. doi:10.1097/TA.1090b1013e3181a39330
Stein DM, York GB, Boswell S, Shanmuganathan K, Haan JM, Scalea TM (2007) Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. J Trauma Acute Care Surg 63:538–543. doi:10.1097/TA.1090b1013e318068b318053c
Larici A, Gotway M, Litt H et al (2002) Helical CT with sagittal and coronal reconstructions: accuracy for detection of diaphragmatic injury. AJR 179:451–457
Dreizin D, Borja M, Danton G et al (2013) Penetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology 268:729–737
Hammer MM, Flagg E, Mellnick VM, Cummings KW, Bhalla S, Raptis CA (2014) Computed tomography of blunt and penetrating diaphragmatic injury: sensitivity and inter-observer agreement of CT Signs. Emerg Radiol 21(2):143–149
Dreizin D, Borja M, Danton G et al (2013) “Appendix E1: pearls and pitfalls in the multidetector CT diagnosis of PDI: a tutorial” in Penetrating enetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology 268:729–737
Nchimi A, Szapiro D, Ghaye B et al (2005) Helical CT of blunt diaphragmatic rupture. Am J Roentgenol 184:24–30
Mirvis S, Shanmuganagthan K (2007) Imaging hemidiaphragmatic injury. Eur Radiol 17:1411–1421
Bergin D, Ennis R, Keogh C, Fenlon HM, Murray JG (2001) The “dependent viscera” sign in CT diagnosis of blunt traumatic diaphragmatic rupture. Am J Roentgenol 177:1137–1140
Desser T, Edwards B, Hunt S, Rosenberg J, Purtill M, Jeffrey RB (2010) The dangling diaphragm sign: sensitivity and comparison with existing CT signs of blunt traumatic diaphragmatic rupture. Emerg Radiol 17:37–44
Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Hogan GJF, Scalea TM (2004) Penetrating torso trauma: triple-contrast helical CT in peritoneal violation and organ injury—a prospective study in 200 patients. Radiology 231:775–784
Spann JC, Nwariaku FE, Wait M (1995) Evaluation of video-assisted thoracoscopic surgery in the diagnosis of diaphragmatic injuries. Am J Surg 170:628–630, discussion 630–621
Rossi P, Mullins D, Thal E (1993) Role of laparoscopy in the evaluation of abdominal trauma. Am J Surg 166:707–710, discussion 710–701
Paci M, Ferrari G, Annessi V, de Franco S, Guasti G, Sgarbi G (2006) The role of diagnostic VATS in penetrating thoracic injuries. World J Emerg Surg : WJES 1:30
Miles EJ, Dunn E, Howard D, Mangram A (2004) The role of laparoscopy in penetrating abdominal trauma. JSLS: J Soc Laparoendosc Surg / Soc Laparoendosc Surg 8:304–309
Friese RS, Coln CE, Gentilello LM (2005) Laparoscopy is sufficient to exclude occult diaphragm injury after penetrating abdominal trauma. J Trauma 58:789–792
Chiu WC, Shanmuganathan K, Mirvis SE, Scalea TM (2001) Determining the need for laparotomy in penetrating torso trauma: a prospective study using triple-contrast enhanced abdominopelvic computed tomography. J Trauma 51:860–868, discussion 868–869
Bautz PC, Knottenbelt JC (1994) Diaphragmatic injury—a source of hazard in laparoscopy. Injury 25:401–402
Ahmed N, Whelan J, Brownlee J, Chari V, Chung R (2005) The contribution of laparoscopy in evaluation of penetrating abdominal wounds. J Am Coll Surg 201:213–216
Brook O, Eran A, Engel A (2012) CT multiplanar reconstructions (MPR) for shrapnel injury trajectory. Emerg Radiol 19:43–51
Fischer T, Folio L, Backus C, Bunger R (2012) Case report highlighting how wound path identification on CT can help identify organ damage in abdominal blast injuries. Mil Med 177:101–107
Folio LR, Fischer T, Shogan P, Frew M, Dwyer A, Provenzale JM (2011) Blast and ballistic trajectories in combat casualties: a preliminary analysis using a Cartesian positioning system with MDCT. Am J Roentgenol 197:W233–W240
Folio L, Fischer T, Shogan P et al (2011) CT-based ballistic wound path identification and trajectory analysis in anatomic ballistic phantoms. Radiology 258:923–929
Caskey C, Zerhouni E, Fishman E, Rahmouni A (1989) Aging of the diaphragm: a CT study. Radiology 171:385–389
Rees O, Mirvis SE, Shanmuganathan K (2005) Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clin Radiol 60:1280–1289
Chen HW, Wong YC, Wang LJ, Fu CJ, Fang JF, Lin BC (2010) Computed tomography in left-sided and right-sided blunt diaphragmatic rupture: experience with 43 patients. Clin Radiol 65:206–212
Murray JG, Caoili E, Gruden JF, Evans SJ, Halvorsen RA, Mackersie RC (1996) Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. Am J Roentgenol 166:1035–1039
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dreizin, D., Bergquist, P.J., Taner, A.T. et al. Evolving concepts in MDCT diagnosis of penetrating diaphragmatic injury. Emerg Radiol 22, 149–156 (2015). https://doi.org/10.1007/s10140-014-1257-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-014-1257-6