Abstract
The objectives of our study were to describe a new CT sign of diaphragmatic injury, the “dangling diaphragm” sign, and assess its comparative utility relative to other signs in the diagnosis of diaphragmatic injury resulting from blunt trauma. CT scans of 16 blunt trauma patients (12 men and four women, mean age 36.6 years old) with surgically proven diaphragmatic injury and 32 blunt trauma patients (24 men and eight women; mean age 37.4 years old) without evidence of diaphragmatic injury at surgery were blindly reviewed by three board certified radiologists specializing in body imaging. Studies were evaluated for the presence of established signs of diaphragmatic injury, as well as the dangling diaphragm sign, in which the free edge of the torn hemidiaphragm curls inward from its normal course parallel to the body wall. The sensitivity and specificity of each sign were determined, as were the correlation between the signs and the interobserver agreement in evaluation of these findings. The radiologists’ overall impression as to whether rupture was present was also recorded. In select cases, coronal and/or sagittal reformatted images were available, and they were reviewed following evaluation of the original axial images. Any change in interpretation due to these images was noted. The sensitivity of the radiologists’ overall impression for detection of diaphragmatic injury was 77%, with 98% specificity. Individual signs of diaphragmatic injury had sensitivities ranging from 44% to 69%, with specificities of 98% to 100%. The dangling diaphragm sign had a sensitivity of 54% and a specificity of 98%, similar to the other signs. Multiple signs were present in most cases of diaphragmatic injury, and coronal and sagittal reformatted images had little impact. Diaphragmatic injury remains a challenging radiographic diagnosis. The dangling diaphragm is a conspicuous sign of diaphragmatic injury, and awareness of it may increase detection of diaphragmatic injury on CT studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic rupture of the diaphragm occurs in approximately 5% of cases of blunt trauma [1]. Rapid diagnosis is essential, as progressive herniation of visceral organs into the thoracic cavity can result in significant morbidity and mortality. In addition, preoperative identification allows for repair during any initial exploratory laparotomy. Unfortunately, identification is often obscured by co-occurring traumatic injuries, and delayed diagnosis occurs in up to two thirds of all cases [2]. Patients can present years later with complications related to delayed diagnosis [3, 4]. Multiple imaging modalities have been proposed for evaluation of the diaphragm in the setting of trauma, including radionuclide liver–spleen imaging, ultrasonography, radiography, computed tomography, and magnetic resonance imaging [5–8].
Standard radiography has a relatively poor reported sensitivity of 24–50% for diagnosis of traumatic diaphragm rupture, based on unilateral elevation of the hemidiaphragm or evidence of visceral organ herniation into the thorax [9, 10]. Standard axial CT has a reported sensitivity of 42–82% [10, 11]. Helical CT has reportedly improved detection rates of 73–92%, possibly in part secondary to the operator’s ability to review high-quality coronal and sagittal reformations in real time [8, 12, 13]. In addition, identification of and knowledge regarding imaging signs of diaphragmatic rupture both in the axial and reformatted series likely accounts for much of the improvement in sensitivity [8, 14].
Beginning first with helical CT and now with the current clinical standard multidetector CT (MDCT), the sensitivity of imaging in this diagnosis has improved, although several authors have noted relatively lower sensitivity for detecting right- than left-sided rupture [15–17].
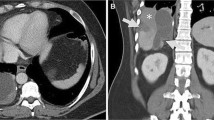
A number of signs of traumatic diaphragmatic rupture have been described, including diaphragmatic discontinuity, visceral herniation through the diaphragm, the collar sign, the dependent viscera sign, and the band and hump signs (of right-sided rupture; Figs. 1, 2, 3, and 4). We have recently observed an additional feature we have named the “dangling diaphragm” sign, in which the free edge of the torn diaphragm is visible as it curls inward toward the center of the abdomen away from and at near right angles to the chest wall (Figs. 5 and 6). As we define it, the sign differs from diaphragmatic discontinuity in that it is present when a comma-shaped fragment of diaphragm can be identified, whether or not a gap in the diaphragm is appreciated. We noted that this sign was quite conspicuous on a few of our recent cases, and we therefore sought to examine how well the sign performs relative to other known CT signs of blunt diaphragmatic rupture. The objectives of our study, therefore, were to assess in a blinded fashion the accuracy, sensitivity, specificity, and interoperator variability of previously described signs of blunt diaphragmatic rupture, as well as the new dangling diaphragm sign, along with the overall sensitivity and specificity of MDCT at our institution in a retrospective study of surgically proven cases.
Dangling diaphragm sign: a 53-year-old woman who sustained blunt abdominal trauma in a motor vehicle collision. Delayed image from axial contrast-enhanced CT shows a curvilinear flap of torn left hemidiaphragm in the left upper quadrant (arrow), the dangling diaphragm sign. Note large area of active extravasation of contrast material along the anterior diaphragmatic contour (asterisk)
Materials and methods
Following approval by the Institutional Review Board, a search of the Stanford Trauma Registry was performed for all cases of surgically proven diaphragmatic rupture resulting from blunt trauma, in which the subject had a preoperative CT scan through the diaphragm, from January 1, 2000 to May 31, 2006. A total of 16 cases were found, with 12 men and four women. Mean age in the positive cases was 36.6 years old, with a range of 16 to 73. Injury severity score (ISS) was also determined for each case, with an average value of 32.1 (range 10 to 66).
Thirty-two control cases (24 men and eight women) were also included in the study for a total study population of 48 cases. The mean age of the control group was 37.4 years old. These were cases of blunt trauma with no findings of diaphragmatic injury at surgery and also with a preoperative CT scan. These cases were also selected using a search of the Stanford Trauma Registry, for the same time period. The control cases were matched to the positive cases for sex, age, and ISS. A ratio of negative to positive cases of 2:1 was chosen to provide additional information than what would have been obtained with a 1:1 ratio, while still representing a reasonable number of cases for retrospective review. A higher ratio of 3:1 would have introduced the potential for statistical separation or overfitting artifacts, and a ratio of 19:1, approaching the true prevalence of the injury, would have required re-review of over 300 cases, which was not practical.
CT scans were performed over a time period spanning March, 2001–May 2007. Because of the wide date range, a variety of MDCT technologies and scan protocols were in use at that institution during that time period. One scan was performed on four-slice scanner (GE Lightspeed QXi), 32 scans on an eight-detector scanner (31 on GE Lightspeed Ultra and 1 on GE Lightspeed Plus) and 12 scans on a 16-detector scanner (Lightspeed 16). Detector configuration for the MDCT scans was either 4, 8, or 16 × 1.25, depending on the scanner. Three cases from 2001 (two negative cases and one positive case) were performed on a single slide scanner (GE High Speed CTi). In all cases, the abdomen was scanned following administration of iodinated contrast at a 300 or 350 mg I/ml concentration and abdominal images reconstructed at 5 mm section thickness for primary viewing. In 30 of the cases (16 negative and 14 positive cases), the abdominal portion of the scan was preceded by an angiogram of the chest in which contrast was injected at a rate of 4 or 5 ml/s and images were reconstructed at 1.25-mm (n = 25; 13 negative and 12 positive cases), 2.5-mm (n = 3, all in 2001; two negative and one positive case), or 3-mm sections (two 2001 cases; one negative and one positive). In abdomen-only studies, contrast was injected at a rate of 2 ml/s. Images of the abdomen and pelvis were acquired following a delay of 70 s from the beginning of contrast injection at 120 kVp and 320–400 mA.
The cases were put in random order (including both positive and negative cases) and independently reviewed by three board certified radiologists specializing in body imaging with 30, 20, and 2 years of posttraining experience, respectively. The radiologists were blinded to the surgical findings and original CT interpretation. A standard form was completed by each radiologist for each case, on which they were to indicate the presence or absence of diaphragmatic discontinuity, visceral herniation through the diaphragm, collar sign, dependent viscera sign, and dangling diaphragm sign (“direct” signs of diaphragmatic injury). The definitions of each sign as used by the radiologists are given in Table 1. We did not evaluate the band or hump signs, as these are specific for right-sided injury only. The radiologists also indicated the presence or absence of fractures of the lower ribs, splenic injury, hepatic injury, pancreatic injury, pleural effusion, free fluid in the abdomen, active extravasation of contrast adjacent to the diaphragm, and elevation of the diaphragm on the scout image (signs of injury/“indirect signs” of diaphragmatic rupture). Originally, for each finding, the confidence in the result was indicated on a four-point scale, with 0 = definitely not present, 1 = probably not present, 2 = probably present, and 3 = definitely present. However, to strengthen the power of the statistical analysis, the “0” and “1” ratings were later combined, and the “2” and “3” ratings were combined to create a binary “yes” or “no” rating scale. Also, the overall impression of the radiologist as to whether or not there was diaphragmatic injury was indicated, using the same four-point scale, and subsequently condensed into a binary yes–no assessment.
During the time period encompassed by this study, it was not our department’s routine practice to obtain additional reformatted images in coronal or sagittal planes; these would have to have been requested by the radiologist present at the time of the study. In a total of 13 cases, coronal and/or sagittal reconstructions were obtained, primarily for evaluation of the spine, in slice thicknesses ranging from 0.6 to 3 mm. Seven of the 13 cases were in the control patients without diaphragmatic injury, and six were the test cases. Of these, four patients had been scanned on 16-slice scanners; however, the protocols did not specify isotropic voxels. Any additional images such as multiplanar reformatted images or axial images with thinner collimation were reviewed only after completion of review of the 5-mm axial images. Any change in interpretation based on these additional images was also recorded, using the same scoring system.
After the study was completed and all the retrospective reviews were recorded, the original CT reports were reviewed by one investigator and compared with the three blinded radiologists’ readings.
Statistical analysis
Correlations among the imaging predictors of rupture were calculated using Kendall’s tau-b coefficient (Table 2). Statistical significance was assessed using Sidak-adjusted p values. A value of p < 0.01 was used to indicate significance.
Binary versions of each predictor were then created by combining the “Probably” and “Definitely” categories to create either Yes or No responses. Ratings of “definitely not present” or “probably not present” (0 or 1) were combined as a no response, and “probably present” or “definitely present” were combined as a yes response. Using these binary scores, sensitivity, specificity, and area under the ROC curve were calculated for each sign of rupture. Interobserver agreement among the three readers for the binary scores of each predictor was assessed by the kappa statistic. Confidence intervals for kappa were estimated by 1,000 bootstrap replications.
Two types of composite score were then created from the five direct signs (dangling, discontinuity, herniation, collar, dependent) and three indirect signs (Elevation on Scout, Pleural Effusion, and Rib Fracture) rupture. The first composite score was the sum of each of the component binary (0 or 1) scores; the direct composite score thus ranged from 0 to 5; the indirect composite score ranged from 0 to 3 (Table 4). Of the eight original indirect signs, these three were selected because only they had significantly elevated odds ratios. The second composite score was a binary one representing the logical disjunction of the component scores; it thus corresponded to either none of the signs being present or at least one of the components being present (Table 5).
Results
Fourteen patients had left-sided rupture, and two had right-sided rupture. Because of the small number of right-sided cases, no side-dependent analysis of the signs was performed.
Three positive cases, all left-sided ruptures, were not detected by any of the radiologists. A fourth positive case was called probable rupture by one radiologist and negative by the other two. In all four cases, there were left pleural effusions, and in two, there were associated splenic ruptures and left upper quadrant hematomas, and we speculated that the blood adjacent to the diaphragm decreased its visualization as a distinct structure. The other 12 positive cases, including both right-sided ruptures, were correctly categorized by all three radiologists, giving sensitivity of the overall assessment of 77%. The overall impression of the radiologists was highly specific, with only two false-positive interpretations (specificity 98%).
As planned by our study design, there were no significant differences between the control group and the diaphragm rupture group with respect to patient age (37.4 ± 17.8 vs. 36.6 ± 18.3) or injury severity score (27 ± 12.7 vs. 32.1 ± 16.9).
Coronal and sagittal reformatted images were available in six of the positive cases and four of the negative cases. Thin axial images were available in ten of the positive cases and 17 of the negative cases. No overall interpretations were changed after review of the additional images. In one (positive) case, the confidence in diagnosing diaphragmatic rupture was increased from probably present to definitely present based on the reformatted images. In six interpretations, a sign (most commonly the collar sign) was appreciated on the reformatted images but not the axial images; however, in all of these cases, the diagnosis was confidently made on the original axial images, and there was no change in the overall interpretation.
The sensitivity, specificity, and AUC of the direct CT signs of diaphragmatic rupture (diaphragmatic discontinuity, dangling diaphragm, visceral herniation, collar sign, and dependent viscera sign) are shown in Table 1. Within the estimated confidence intervals, the direct signs had similar sensitivity, specificity, and accuracy, although the collar sign was somewhat less sensitive and accurate than the others. The direct signs were also highly correlated with one another (Table 2), with the highest associations between visceral herniation and diaphragmatic discontinuity. In particular, the dangling diaphragm sign was closely correlated with discontinuity and visceral herniation. There was a single interpretation (one of 48) with only one of the five signs present (visceral herniation), while in 29% of interpretations in the positive cases (14 out of 48), all five signs were present.
Elevation of the hemidiaphragm on the scout image had similar sensitivity to the cross-sectional direct CT signs (54%), but lower specificity (89%). Other signs of injury not directly related to the diaphragm were either insensitive, nonspecific, or both (Table 3). Pancreatic injury was the least predictive of associated diaphragmatic injury (4%, CI 1–14%), followed by active extravasation (12%, CI 5–25%).
The overall assessment of the radiologist was more sensitive than any single sign (77%, Table 1) and showed excellent specificity (98%). For readers 1, 2, and 3, the sensitivities were 75%, 75%, and 81%, respectively. Specificities were 94%, 100%, and 100%, respectively, with reader one having two false positives.
The composite scores of 0 or 1 for each sign were combined across the three readers and analyzed (Tables 4 and 5). Scores of 3, 4, or 5 were seen in a total of 30 assessments, almost all of which were rupture cases. Likewise, low composite scores of 0, 1, or 2 in the direct signs were seen almost exclusively in cases without rupture. When these data are collapsed such that the presence of any of the five signs is considered indicative of rupture (Table 5), 45 of the maximal 48 assessments (by three readers in 16 positive cases) were correct, yielding a sensitivity of 94%. As expected, however, calling a diaphragm rupture present in the setting of only one direct sign positive yielded a low specificity of only 38%.
Interobserver agreement is shown in Table 6. The highest agreement was seen with the diaphragmatic discontinuity sign, followed by visceral herniation, and then the dangling diaphragm and dependent viscera signs.
As might be expected in a retrospective study, these results differed slightly from the prospective original CT interpretations of these cases. At the time of interpretation, none of the negative cases were called positive (no false positives), but six of the positive cases were missed. The four false negative cases from the retrospective review were among the six missed at the time of the original interpretation. Two additional cases were missed prospectively. One of those was a right-sided diaphragmatic rupture that was detected on the retrospective review. The other was a case of left-sided rupture in which, on retrospective review, the dangling diaphragm sign is clearly visible.
Discussion
Diaphragmatic rupture secondary to blunt trauma may be overlooked on imaging because of its association with multiple other serious internal injuries, as well as the often subtle appearance on imaging. Penetrating traumatic injuries to the diaphragm tend to produce smaller defects than those in blunt trauma, but are often suspected due to the trajectory of injury visible as blood or gas on CT or implicit from entry and exit wounds. Because of these marked differences in clinical presentation and imaging appearance, we did not include penetrating trauma in our analysis.
From our data, it is clear that even in the MDCT era blunt diaphragmatic injury remains a challenging radiographic diagnosis, and direct visualization and evaluation of the entire diaphragm is difficult. In areas of eventration, the diaphragm may be imperceptible even on multiplanar reformatted images. Therefore, other evidence of diaphragmatic injury, such as visceral herniation into the thorax, is helpful.
In this study, we have introduced the dangling diaphragm sign, in which the injured diaphragm curls inward from its normal course parallel to the abdominal wall. In our study, this sign had similar sensitivity and specificity to other CT signs of diaphragmatic injury, such as the dependent viscera sign, collar sign, and visceral herniation into the thorax. These signs were all highly correlated with one another, and in most cases, several were present. In particular, a diaphragmatic defect was usually present when either visceral herniation or the dangling diaphragm sign were seen. Indeed, the correlation between the dangling diaphragm sign and the diaphragmatic defect is to be expected, given that the dangling diaphragm sign refers specifically to the configuration of the discontinuous diaphragm fragment.
Nevertheless, one important attribute of CT signs of diaphragmatic injury is their conspicuity. While several signs may be present in a particular case when a focused search is performed in a clinical trial setting, in a busy clinical trauma practice, it is helpful to have one particular sign “catch the eye”, drawing the radiologist’s attention to the possibility of diaphragmatic injury. With suspicion then raised, the images can then be scrutinized for additional corroborating evidence.
The sensitivities we found for the individual direct signs of diaphragmatic rupture, as well as the 77% sensitivity we found based on the radiologists’ overall assessment, are similar to that found in other studies in the literature. Kileen et al. studied 41 blunt trauma patients with helical CT and found a sensitivity of 78% for detecting left-sided rupture and 50% for right-sided rupture [16]. Bergin et al. found an overall sensitivity for helical CT of 90%, with 100% sensitivity for left-sided rupture and 75% for right-sided rupture [15]. More recently, Larici et al. reviewed the utility of sagittal and coronal reconstructions in helical CT scans of 47 patients (25 with diaphragmatic rupture and 22 without) and found a sensitivity of 84% [13]. In another study of 179 blunt trauma patients in which 16 had diaphragmatic ruptures, 100% sensitivity was achieved by the two staff radiologists searching for any of 11 CT signs of rupture [8]. Of their 11 signs, intrathoracic herniation was the most sensitive, and diaphragmatic discontinuity had a sensitivity of only 46%, which is somewhat different from our results.
The CT signs of diaphragmatic injury evaluated in our study all had excellent specificity. However, other signs of injury not directly related to the diaphragm, such as pleural effusion, or rib fractures were not particularly useful. In addition, we found that multiplanar reformatted images had little impact on the diagnosis of rupture, similar to the findings of Larici et al. in a prior study of helical CT [13]
Contrary to our expectations, the dangling diaphragm sign did not prove to be better than other previously described signs of diaphragmatic rupture, as both discontinuity and visceral herniation had higher sensitivities (Table 1). And although this sign is often quite conspicuous, in practice, our study found lower interobserver agreement for the presence of this sign than for any of the other direct signs apart from the dependent viscera sign or the collar sign, although the ratings were similar within the confidence intervals generated.
One limitation of our study is that only patients who underwent surgical exploration were included. Therefore, clinically occult injuries may have been missed. Because of the rarity of diaphragmatic rupture, it was necessary to include cases dated back to 2001 in order to obtain the largest possible sample. As a result, the MDCT protocols used in this study are not the current clinical standard of isotropic voxels. Therefore, the value of our coronal and sagittal reformations may under-represent what would have been obtained if 64-slice scanner or higher had been used for these cases. Also, our sample size is relatively small due to the uncommon nature of the injury and the requirement that subjects have a preoperative CT scan. Finally, our case mix of one of three rupture cases and two of three without rupture does not reflect the true prevalence of this injury among blunt trauma patients, which is much lower.
In conclusion, we have presented the dangling diaphragm sign, a new CT sign of diaphragmatic injury. In our series, this sign was not seen in isolation and was correlated with the presence of other signs of rupture, especially visceral herniation and diaphragmatic discontinuity. Awareness of this and other relatively conspicuous signs of diaphragmatic injury will increase the likelihood of radiologists detecting this rare but critically important injury on CT studies, thereby minimizing delays in diagnosis.
References
Meyers BF, McCabe CJ (1993) Traumatic diaphragmatic hernia. Occult marker of serious injury. Ann Surg 218:783–790. doi:10.1097/00000658-199312000-00013
Sangster G, Ventura VP, Carbo A, Gates T, Garayburu J, D’Agostino H (2007) Diaphragmatic rupture: a frequently missed injury in blunt thoracoabdominal trauma patients. Emerg Radiol 13:225–230. doi:10.1007/s10140-006-0548-y
van de Ven K, Vanclooster P, de Gheldere C, Meersman A, Verhelst F (1995) Strangulation: a late presentation of right-sided diaphragmatic rupture. Acta Chir Belg 95:226–228
Wright BE, Reinke T, Aye RW (2005) Chronic traumatic diaphragmatic hernia with pericardial rupture and associated gastroesophageal reflux. Hernia 9:392–396. doi:10.1007/s10029-005-0339-5
Barbiera F, Nicastro N, Finazzo M et al (2003) The role of MRI in traumatic rupture of the diaphragm. Our experience in three cases and review of the literature. Radiol Med (Torino) 105:188–194
Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K (2004) Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma. Am J Emerg Med 22:601–604. doi:10.1016/j.ajem.2004.08.015
Kim EE, McConnell BJ, McConnell RW, Duke JH, Dillon M (1983) Radionuclide diagnosis of diaphragmatic rupture with hepatic herniation. Surgery 94:36–40
Nchimi A, Szapiro D, Ghaye B et al (2005) Helical CT of blunt diaphragmatic rupture. AJR 184:24–30
Gelman R, Mirvis SE, Gens D (1991) Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. AJR 156:51–57
Shapiro MJ, Heiberg E, Durham RM, Luchtefeld W, Mazuski JE (1996) The unreliability of CT scans and initial chest radiographs in evaluating blunt trauma induced diaphragmatic rupture. Clin Radiol 51:27–30. doi:10.1016/S0009-9260(96) 80214-5
Murray JG, Caoili E, Gruden JF, Evans SJ, Halvorsen RA Jr, Mackersie RC (1996) Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. AJR 166:1035–1039
Israel RS, McDaniel PA, Primack SL, Salmon CJ, Fountain RL, Koslin DB (1996) Diagnosis of diaphragmatic trauma with helical CT in a swine model. AJR 167:637–641
Larici AR, Gotway MB, Litt HI et al (2002) Helical CT with sagittal and coronal reconstructions: accuracy for detection of diaphragmatic injury. AJR 179:451–457
Kaya SO, Karabulut N, Yuncu G, Sevinc S, Kiroglu Y (2006) Sinus cut-off sign: a helpful sign in the CT diagnosis of diaphragmatic rupture associated with pleural effusion. Eur J Radiol 59:253–256. doi:10.1016/j.ejrad.2006.04.015
Bergin D, Ennis R, Keogh C, Fenlon HM, Murray JG (2001) The “dependent viscera” sign in CT diagnosis of blunt traumatic diaphragmatic rupture. AJR 177:1137–1140
Killeen KL, Mirvis SE, Shanmuganathan K (1999) Helical CT of diaphragmatic rupture caused by blunt trauma. AJR 173:1611–1616
Rees O, Mirvis SE, Shanmuganathan K (2005) Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clin Radiol 60:1280–1289. doi:10.1016/j.crad.2005.06.013
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Desser, T.S., Edwards, B., Hunt, S. et al. The dangling diaphragm sign: sensitivity and comparison with existing CT signs of blunt traumatic diaphragmatic rupture. Emerg Radiol 17, 37–44 (2010). https://doi.org/10.1007/s10140-009-0819-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-009-0819-5