Abstract
Diaphragmatic injury is an uncommon traumatic condition. It can be easily missed due to a lack of awareness by both clinicians and radiologists. A high index of suspicion is required for the establishment of an early diagnosis and prevention of life-threatening complications. Multidetector computed tomography (MDCT) is the modality of choice for the detection of diaphragmatic injury. In this review article, we illustrate the MDCT appearance of blunt and penetrating diaphragmatic injuries and emphasize the role of the emergency radiologist in detecting these entities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diaphragmatic injury (DI) was first reported by Sennertus in 1591. He described autopsy findings of gastric herniation through a diaphragmatic defect caused by a self-inflicted stab wound [1]. Today, diaphragmatic injury remains an uncommon traumatic condition. In Europe and Canada, the vast majority of the cases of DI are due to blunt trauma [2, 3]. Blunt diaphragmatic injury (BDI) is estimated to occur in up to 5 % of trauma patients admitted to hospital [3]. In contrast, penetrating injuries, most commonly due to gunshot wounds (GSW), account for the majority of the traumatic diaphragmatic injuries in the United States [4]. The incidence of diaphragmatic injury in penetrating trauma is estimated at 10–15 % [5].
Unfortunately, diaphragmatic injury is an easily missed diagnosis. Currently, the lion’s share of patients with blunt trauma are managed using a conservative approach. There is also a growing trend toward conservative management of patients with penetrating injuries who have normal vital signs and no clinical indication for surgery. However, when a conservative approach is chosen, it is estimated that blunt diaphragmatic injury remains undiagnosed at initial presentation in 7–66 % of cases [6]. For penetrating DI, one study estimated that 7 % of cases can be occult [7].
There are multiple explanations for the suboptimal detection rate of diaphragmatic injury. There is an overall lack of awareness by clinicians and radiologists regarding this uncommon condition. No specific clinical signs of DI are known. In addition, diaphragmatic injury usually occurs in polytrauma patients and its presentation can be overshadowed by associated injuries, which have been reported in 52–100 % of patients in different series [8, 9].
From an imaging standpoint, the diagnosis of diaphragmatic injury can be challenging. Multiple signs have been described in the imaging literature. However, in a significant proportion of cases, the diaphragmatic defect cannot be directly visualized and the radiologist has to rely on a combination of indirect signs. Furthermore, the defects in penetrating diaphragmatic injury are notoriously difficult to detect due to their small size (1–2 cm).
Unfortunately, diaphragmatic injury does not heal spontaneously. A negative pleuroperitoneal gradient and continuous diaphragmatic motion prevent healing of the lesion. Positive-pressure ventilation eradicates this gradient while the patient is intubated but with extubation after improvement of the patient’s clinical status, herniation of abdominal organs into the thoracic cavity can develop. Eventually, small untreated diaphragmatic tears may increase in size and present symptomatically, sometimes years later [10]. Untreated patients can develop complications related to herniation. The stomach, colon, omentum and spleen are the most common herniated structures when the patient has a left-sided DI while the liver can herniate in cases of right-sided injury [6]. Herniated organs are at risk of incarceration and ischemia with the potential for subsequent perforation.
Chest radiographs have poor accuracy for the detection of diaphragmatic injury. Correct preoperative diagnosis of DI was made on preoperative chest radiographs in only 39–65 % of patients [3, 9, 11]. The results are worse in cases of injury to the right hemidiaphragm. Presently, multidetector computed tomography (MDCT) is the mainstay in the assessment of trauma patients. 64-section or higher MDCT scanners are able to acquire near-isotropic data sets. Multiplanar reformations (MPR) can be easily and quickly created on workstations. The advantages of MDCT make it ideally suited for the evaluation of the diaphragm and provide hope for a solution to the diagnostic conundrum of diaphragmatic injury.
Approach to the patient with suspected diaphragmatic injury
The detection of diaphragmatic injury requires a high index of suspicion. Clinical information regarding the mechanism of injury is of paramount importance. Injury of the diaphragm should be considered when there has been a trauma with significant force. Car accidents are the most common cause of blunt diaphragmatic injury (90 %) [3, 6, 12]. Occasionally, a fall from height or crushing blow can result in DI. The forces from impact lead to increased intraabdominal pressure with subsequent rupture of the diaphragm. Avulsion of the attachments of the diaphragm after a lateral blow to the chest wall and direct injury of the diaphragm by fractured ribs have also been proposed as mechanisms of injury [9]. Blunt diaphragmatic injury occurs more often on the left side due to congenital weakness of the posterolateral area of the left hemidiaphragm and the protective effect of the liver on the right side. In addition, the steering wheel is located on the left side in the majority of countries, resulting in more left-sided injuries related to impact from the steering wheel. However, it is possible that right-sided injuries are underreported due to more subtle imaging findings and higher initial mortality related to associated injuries. Left-sided tears have been reported in 56–86 % of cases [8, 9], in comparison with right-sided injuries which are estimated to occur in 11–39 % of cases. Bilateral tears are uncommon and appear in 2.4–13 % of cases [9]. Large tears (more than 10 cm) are usually observed in BDI. Immediate herniation of abdominal organs into the thoracic cavity occurs in many cases of blunt diaphragmatic injury due to the typically large size of the defect. The presence of herniation helps identify the location of the diaphragmatic rent.
On the contrary to cases of blunt diaphragmatic injury, penetrating trauma causes DI by direct laceration. The resulting diaphragmatic rents are typically small. Therefore, the majority of patients with penetrating diaphragmatic injury do not develop immediate complications related to herniation of abdominal organs [14, 15]. The herniation usually develops later if the diaphragmatic injury is missed during the initial assessment. Penetrating DI often occurs (42 %) in patients with wounds in the thoracoabdominal area defined by the nipple line superiorly and the costal margin inferiorly [4]. There is no predilection for a particular side in GSWs. Stab wounds usually penetrate the left hemidiaphragm due to the predominance of right-handed attackers.
Despite its low sensitivity, chest radiographs can have a useful role in the initial imaging evaluation of patients with suspected diaphragmatic injury. Chest radiographs are routinely obtained on trauma patients during their initial triage. There is a proportion of patients who are too hemodynamically unstable to undergo CT and are immediately taken for life-saving surgery. However, these patients usually still have radiographs before surgery. Careful inspection of the radiographs can demonstrate signs highly suspicious for DI. They include the presence of gas-containing hollow viscera within the thoracic cavity and an abnormal course of the nasogastric tube with its distal end projecting above the diaphragm [16]. Moreover, a high position of a hemidiaphragm in comparison to the contralateral side (more than 6 cm) should alert imagers to the possibility of diaphragmatic injury. Nonetheless, most patients with DI show nonspecific signs on chest radiographs including obliteration of the diaphragmatic contour, mild elevation of the injured diaphragm, shift of the mediastinum to the contralateral side, or evidence of additional traumatic thoracic injury (pneumothorax, pleural effusion, or rib fractures) [6]. Patients with diaphragmatic injury are quite often victims of severe polytrauma. Therefore, these nonspecific findings are frequently attributed to associated thoracic injuries. However, when these findings are present, the emergency radiologist should raise suspicion for diaphragmatic injury and advise the clinicians to carefully inspect the diaphragm during surgery. The interpretation of chest radiographs in trauma patients requires significant expertise and emphasizes the essential role of the emergency radiologist embedded in the trauma bay.
Conventional CT had a low sensitivity for detection of diaphragmatic injury (ranging 14–61 %) and moderate specificity (76–99 %) [12, 17]. The invention of MDCT revolutionized trauma imaging and improved imaging detection of DI. A recent study demonstrated a sensitivity of 77 % and specificity of 98 % for MDCT in the detection of blunt diaphragmatic injury [18]. Dreizin et al. [19] reported a range of sensitivities from 73 to 100 % and a range of specificities from 50 to 92 % for the diagnosis of penetrating diaphragmatic injury using 64-section MDCT. The improved accuracy of MDCT in comparison to conventional CT can be explained by the acquisition of near-isotropic data sets and widespread use of multiplanar reformations. Unfortunately, the results of the clinical trials can be difficult to reproduce in a busy clinical trauma practice. Nchimi et al. showed that only 50 % of blunt diaphragmatic ruptures had been diagnosed prospectively on the admission CT [20]. When the same cases were assessed retrospectively, the sensitivity of reviewers ranged from 56.2 to 87.5 % Diaphragmatic injury remains a challenging radiological diagnosis requiring the expertise of a dedicated emergency radiologist. The visualization of the entire diaphragm can be an onerous task. The diaphragm may be imperceptible in areas of eventration [18]. The radiologist should carefully assess axial images in addition to coronal and sagittal MPRs. Many trauma centres perform multiphase studies, scanning the chest in arterial phase and the abdomen and pelvis in portal venous and delayed phases. This approach provides the radiologist with the opportunity to assess the diaphragm for direct and indirect signs of diaphragmatic injury in different phases. Multiphasic imaging helps to ascertain the trajectory of injury due to better visualization of associated bleeding. Some indirect signs like the band sign, described below, are better appreciated on coronal multiplanar reformations of images obtained in portal venous phase.
MDCT signs of diaphragmatic injury
There are numerous CT signs of diaphragmatic injury. A recent review by Desir et al. listed nineteen signs of BDI [6]. The plethora of signs underscores the difficulties faced by the radiologist in trying to detect DI. The authors of the present review paper practice in leading European and North American level-1 trauma centers. We would like to focus on the signs that we find useful in our combined experience of more than 50 years of interpretation of trauma imaging.
A segmental diaphragmatic defect or discontinuous diaphragm is a highly specific but non-sensitive sign of diaphragmatic injury. The sign represents an abrupt loss of diaphragmatic continuity (Fig. 1). As expected, higher sensitivity (up to 90 %) was shown in cases of blunt diaphragmatic injury due to the typically larger size of the defects [15]. The sensitivity in penetrating injuries ranged 8–60 % [15, 19]. Not surprisingly, the sensitivity of MDCT for detection of segmental diaphragmatic defects was higher in cases when the left hemidiaphragm was injured. Defects in the right hemidiaphragm are more challenging to directly visualize due to an inherent lack of contrast between the diaphragm and liver [9]. A tear of the left hemidiaphragm is usually better appreciated due to the presence of intra-abdominal and retroperitoneal fat adjacent to the undersurface of the left hemidiaphragm (Fig. 2). Both hemidiaphragms should be meticulously scrutinized on coronal and sagittal multiplanar reformations (Figs. 1b, 3) and compared with the contralateral side due to the rarity of bilateral injuries. Chen et al. noted a significantly lower incidence of diaphragmatic discontinuity in patients with hemothorax and suggested that diaphragmatic defects can be masked by blood [21]. However, their study was performed using 4-section MDCT. Therefore, their ability to assess diaphragmatic discontinuity on reformatted images was limited by the presence of stepladder artifacts. The shortened acquisition time of 64-section MDCT scanners eliminates these artifacts and improves the quality of MPRs.
a Axial contrast-enhanced 64-MDCT in a patient with traumatic right diaphragmatic injury. There are multiple herniated small bowel (white arrowheads) and colonic loops (white arrows). Note the “dependent viscera” sign with small bowel loops abutting the posterior ribs. b Coronal reformation in the same patient shows discontinuity of the diaphragm (white arrows) and herniated colonic loops (white arrowheads). c Sagittal reformation in the same patient clearly demonstrates a diaphragmatic defect (white arrows) and herniated bowel loops (white arrowheads)
The specificity of the presence of a segmental defect ranges from 90 to 100 % in blunt and penetrating injuries [6, 17, 19]. Nevertheless, the presence of a segmental diaphragmatic defect alone can be seen in patients with congenital hernias and acquired nontraumatic defects (Fig. 4). Discontinuity of the posterior diaphragm is an anatomic variant described in 11 % of normal patients [22, 23]. Nontraumatic defects are typically located between the diaphragmatic crura and lateral arcuate ligaments and are encountered in elderly patients. Posterior diaphragmatic or Bochdalek defects are observed more often on the left side at the posterolateral location [6]. Usually, nontraumatic defects and congenital hernias have small openings and contain peritoneal fat. However, some congenital hernias can contain abdominal organs. Painstaking search for additional signs of diaphragmatic injury facilitates differentiation between traumatic injuries and nontraumatic defects. Traumatic diaphragmatic injury will be seen in patients with severe polytrauma and multiple associated thoracic and abdominal injuries.
The dangling diaphragm sign was described by Desser et al. [18]. This sign is documented when the free edge of the torn hemidiaphragm curls inward toward the center of the body forming a curvilinear soft tissue density. The sign is better appreciated on coronal MPRs. Its sensitivity for the detection of DI is 54 % and specificity is 98 % [18].
Visualization of abdominal visceral or fat herniation into the pleural cavity is an important sign of diaphragmatic injury. The most common herniated organ on the right side is the liver (Fig. 5). Herniation of the rigid liver requires a diaphragmatic defect of sufficient size in addition to rupture of the ligaments that keep the liver in place [9]. On the other hand, the hollow viscera and fat found within the left upper quadrant (Figs. 6, 7) are more mobile and deformable [15]. Therefore, the sensitivity of abdominal herniation on MDCT for right-sided blunt DI is 8–50 % versus 42–91 % for left-sided injury [6]. As stated above, herniation is not a sensitive sign of penetrating diaphragmatic injury. A recent study using 64-section MDCT reported sensitivities ranging only 7–13 % [19].
a Coronal reformation of axial contrast-enhanced 64-MDCT depicts a large left segmental diaphragmatic defect (white arrows) with herniation of small bowel loops (black arrows) and a colonic loop (white arrowheads). b Sagittal reformation in the same patient shows thickening of herniated small bowel loops (white arrowheads) and colon (white arrows) suggesting bowel ischemia
A waistlike constriction of herniated viscera at the site of the diaphragmatic rent is called the CT collar sign (Figs. 5b, 6b, 8). The constriction can be suspected on axial images but is better assessed on coronal and sagittal reformations. The sign has a sensitivity of 63 % and specificity of 100 % for the diagnosis of the blunt diaphragmatic injury. The sign is more sensitive for detection of left-sided DI (78 %) than right-sided DI (50 %) [24]. The collar sign has high specificity (100 %) but very low sensitivity (0–7 %) in penetrating injuries [4, 19]. The radiologist has to consider that a collar sign can be seen in congenital and acquired nontraumatic diaphragmatic hernias and strive to corroborate this sign with additional evidence of diaphragmatic injury.
Sagittal reformation of axial contrast-enhanced 64-MDCT shows a left hemidiaphragmatic injury with herniation of the stomach. There is marked constriction of the stomach at the site of the diaphragmatic rent (white arrows) illustrating the collar sign. The gastric herniation causes left basal atelectasis (black arrows)
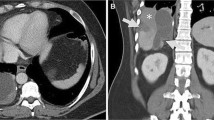
The ongoing challenge to detect right-sided injuries coupled with advancements in imaging technology, including the routine use of multiplanar reformations, led to the description of two additional signs of right-sided injury - the hump and band signs [9]. It is much easier to assess these signs on sagittal and coronal reformations. The hump sign is a rounded herniation of hepatic tissue into the thoracic cavity (Fig. 5a). The sign can be misinterpreted as a high dome of the right hemidiaphragm on axial images. Therefore, the evaluation of a trauma CT cannot be considered complete without a review of the reformations. The band sign is a linear area of hypodensity through the liver at the level of the torn diaphragm. It has been suggested that the band of low density is created as a result of compression of the liver by the injured diaphragm with subsequent hepatic hypoperfusion. The band is almost imperceptible on the axial images due to its in-plane orientation. When image acquisition is obtained during multiple phases of enhancement, the band is more conspicuous on the portal venous phase. The radiologist should be cautious not to misinterpret the band sign as a linear hepatic laceration [21].
In healthy subjects, intraabdominal organs are always separated from the posterior chest wall by the costophrenic sulcus. In patients with DI, the abdominal organs are no longer supported posteriorly by the diaphragm. As a result, they fall to a dependent position, obliterate the sulcus, and abut the posterior ribs. This is referred to as the dependent viscera sign [25]. The sign was originally described when the liver abutted the right posterior chest wall (Fig. 9) and the stomach and bowel abutted the left posterior ribs (Figs. 1a, 10). However, the sign can be documented when any intraabdominal organs lie in contact with the posterior ribs. The dependent viscera can be appreciated on axial images and sagittal reformations. It has a sensitivity of 90 % and specificity of 100 % in cases of blunt DI [25], but is not helpful in cases of penetrating diaphragmatic injury due to the small size of the rents. Two recent studies of the MDCT performance for the diagnosis of penetrating injuries were not able to detect any cases using this sign [4, 19].
Diaphragmatic thickening can represent retraction of the ruptured diaphragm (Fig. 11) or muscular hematoma [26]. It can be seen in complete tears requiring surgery as well as partial thickness tears. Nchimi et al. reported that this sign was falsely positive in 8/163 patients due to the presence of associated retroperitoneal hematoma [20]. Hematoma tracking from splenic, liver or bowel injuries can also cause diaphragmatic thickening. Nevertheless, the presence of diaphragmatic thickening without associated retroperitoneal hematoma should be considered suggestive for DI [6, 20]. The diaphragmatic thickness can be compared with the contralateral side. Bodanapally et al. [4] found a sensitivity of 48 % and specificity of 70 % for detection of penetrating injury. Nchimi et al. reported a sensitivity of 36.3 % for detection of left-sided blunt injury and a sensitivity of 100 % for right-sided blunt injury [20].
The constant search for new sensitive and specific signs of penetrating diaphragmatic injury led to the description of a new sign by Bodanapally et al.—the contiguous injury sign [4]. When a weapon penetrates the diaphragm, it creates a contiguous injury on both sides of the diaphragm. Of note, the diaphragmatic defect itself can be missed in these cases due to its small size. Injuries to organs on either side of the diaphragm implies a full-thickness transdiaphragmatic injury. This is more applicable to low-energy knife wounds, as opposed to high-energy gunshot wounds, which can cause secondary cavitations without direct penetration [4]. The sensitivity of the contiguous injury sign is 82–100 % and the specificity is 82–83 % [4, 19]. A recent study of a large group of patients with diaphragmatic injury evaluated with MDCT demonstrated the ongoing challenge of prospective identification of DI [15]. The interpreting radiologists prospectively identified only 47 % of the penetrating injuries. However, a retrospective review of the same group of patients showed a sensitivity of 83 % for detection of diaphragmatic injury using the contiguous injury sign. It is possible that the radiologists looked for diaphragmatic defects only during their prospective evaluation and tended to overlook the additional signs of injury. As with multiple signs described above, the contiguous injury sign is better appreciated on MPRs.
A rent of the diaphragm disrupts the thoracoabdominal border and allows free passage of air and fluid from the thorax to the abdomen and vice versa. Therefore, the simultaneous presence of pneumothorax and pneumoperitoneum and/or hemothorax and hemoperitoneum are indirect CT signs of diaphragmatic injury [6, 17, 20]. The presence of both hemothorax and hemoperitoneum has a sensitivity of 50 % and specificity of 90 % for the detection of blunt diaphragmatic injury [20]. The simultaneous presence of blood on either side of the diaphragm should be regarded as a marker of severe injury and lead to a prompt assessment of the diaphragm as well as a search for the more sensitive signs of DI. It can be an onerous task because blood may mask segmental diaphragmatic defects [17, 18, 27].
Summary
Despite advances in imaging technology, diaphragmatic injury is still a challenging condition for prospective radiological interpretation. Particularly with penetrating diaphragmatic injuries, direct visualization of a diaphragmatic defect can be impossible. Therefore, the radiologist must remember to look for indirect signs, such as the presence of contiguous injuries on both sides of the diaphragm. The radiologist must also pay special attention to multiplanar reformations, since many described signs of DI are better appreciated on the reformations. 64-section or higher MDCT with its high resolution and better quality of multiplanar reformations is the modality of choice for the evaluation of trauma patients with this often life-threatening entity. In interpreting the imaging of a trauma patient, it is crucial for the radiologist to enquire about the mechanism of injury and use the various MDCT signs to keep this uncommon condition in consideration.
References
Reid J (1840) Diaphragmatic hernia produced by a penetrating wound. Edin Med Surg J 53:104–107
Simpson J, Lobo DN, Shah AB, Rowlands BJ (2000) Traumatic diaphragmatic rupture: associated injuries and outcome. Ann R Coll Surg Engl 82:97–100
Chughtai T, Ali S, Sharkey P et al (2009) Update on managing diaphragmatic rupture in blunt trauma: a review of 208 consecutive cases. Can J Surg 52:177–181
Bodanapally UK, Shanmuganathan K, Mirvis SE et al (2009) MDCT diagnosis of penetrating diaphragm injury. Eur Radiol 19:1875–1881
Spann JC, Nwariaku FE, Wait M (1995) Evaluation of video-assisted thoracoscopic surgery in the diagnosis of diaphragmatic injuries. Am J Surg 170:628–630
Desir A, Ghaye B (2012) CT of blunt diaphragmatic rupture. Radiographics 32:477–498
Leppäniemi A, Haapiainen R (2003) Occult diaphragmatic injuries caused by stab wounds. J Trauma 55(4):646–650
Meyers BF, McCabe CJ (1993) Traumatic diaphragmatic hernia. Occult marker of serious injury. Ann Surg 218(6):783–790
Rees O, Mirvis SE, Shanmuganathan K (2005) Multidetector-row CT of right hemidiaphragmatic rupture caused by blunt trauma: a review of 12 cases. Clin Radiol 60:1280–1289
Sliker CW (2006) Imaging of diaphragm injuries. Radiol Clin North Am 44:199–211
Bergeron E, Clas D, Ratte S et al (2002) Impact of deferred treatment of blunt diaphragmatic rupture: a 15-year experience in six trauma centers in Quebec. J Trauma 52:633–640
Gelman R, Mirvis SE, Gens D (1991) Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. AJR Am J Roentgenol 156:51–57
Shanmuganathan K, Killeen K, Mirvis SE, White CS (2000) Imaging of diaphragmatic injuries. J Thorac Imaging 15:104–111
Clarke DL, Greatorex B, Oosthuizen GV, Muckart DJ (2009) The spectrum of diaphragmatic injury in a busy metropolitan surgical service. Injury 40:932–937
Hammer MM, Flagg E, Mellnick VM et al (2013) Computed tomography of blunt and penetrating diaphragmatic injury: sensitivity and inter-observer agreement of CT signs. Emerg Radiol 21:143–149
Perlman SJ, Rogers LF, Mintzer RA, Mueller CF (1984) Abnormal course of nasogastric tube in traumatic rupture of left hemidiaphragm. AJR Am J Roentgenol 142:85–88
Murray JG, Caoili E, Gruden JF et al (1996) Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. AJR Am J Roentgenol 166:1035–1039
Desser TS, Edwards B, Hunt S et al (2010) The dangling diaphragm sign: sensitivity and comparison with existing CT signs of blunt traumatic diaphragmatic rupture. Emerg Radiol 17:37–44
Dreizin D, Borja MJ, Danton GH et al (2013) Penetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology 268:729–737
Nchimi A, Szapiro D, Ghaye B et al (2005) Helical CT of blunt diaphragmatic rupture. AJR Am J Roentgenol 184:24–30
Chen HW, Wong YC, Wang LJ et al (2010) Computed tomography in left-sided and right-sided blunt diaphragmatic rupture: experience with 43 patients. Clin Radiol 65:206–212
Restrepo CS, Eraso A, Ocazionez D et al (2008) The diaphragmatic crura and retrocrural space: normal imaging appearance, variants, and pathologic conditions. Radiographics 28:1289–1305
Naidich DP, Megibow AJ, Ross CR et al (1983) Computed tomography of the diaphragm: normal anatomy and variants. J Comput Assist Tomogr 7:633–640
Killeen K, Mirvis SE, Shanmuganathan K (1999) Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol 173:1611–1616
Bergin D, Ennis R, Keogh C et al (2001) The “dependent viscera” sign in CT diagnosis of blunt traumatic diaphragmatic rupture. AJR Am J Roentgenol 177:1137–1140
Leung JC, Nance ML, Schwab CW, Miller WT Jr (1999) Thickening of the diaphragm: a new computed tomography sign of diaphragm injury. J Thorac Imaging 14:126–129
Larici AR, Gotway MB, Litt HI et al (2002) Helical CT with sagittal and coronal reconstructions: accuracy for detection of diaphragmatic injury. AJR Am J Roentgenol 179:451–457
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patlas, M.N., Leung, V.A., Romano, L. et al. Diaphragmatic injuries: why do we struggle to detect them?. Radiol med 120, 12–20 (2015). https://doi.org/10.1007/s11547-014-0453-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-014-0453-5