Abstract
There is a long history of attempts to alleviate the pain of childbirth, particularly in Asian and Middle Eastern civilisations. In the UK, it was the administration of chloroform to Queen Victoria by John Snow in 1853 that is widely credited with popularizing the idea that labour pain should and could be treated. Medical analgesia is now well established around the globe with a wealth of research evidence describing methods, efficacy and complications.
In this article, we define ‘primary breakthrough pain’ as the moment when a woman first requests analgesia during labour. The management of this can include simple emotional support, inhaled analgesics, parenteral opioids and epidural analgesia.
‘Secondary breakthrough pain’ can be defined as the moment when previously used analgesia becomes ineffective. We concentrate our discussion of this phenomenon on the situation when epidural analgesia begins to fail. Only epidural analgesia offers the potential for complete analgesia, so when this effect is lost the recipient can experience significant distress and dissatisfaction. The best strategy to avert this problem is prevention by using the best techniques for epidural catheterisation and the most effective drug combinations. Even then, epidurals can lose their efficacy for a variety of reasons, and management is hampered by the fact that each rescue manoeuvre takes about 30 minutes to be effective. If the rescue protocol is too cautious, analgesia may not be successfully restored before delivery, leading to patient dissatisfaction. We therefore propose an aggressive response to epidural breakthrough pain using appropriate drug supplementation and, if necessary, the placement of a new epidural catheter. Combined spinal epidural techniques offer several advantages in this situation. The goal is to re-establish analgesia within 11 hour.
The primary aim of pain management during labour and delivery is to provide the level of comfort determined as acceptable to each individual woman. Some require little or no analgesia, while others demand complete abolition of pain. Whatever the individual’s personal point of breakthrough pain is, supporting clinicians should respond logically and rapidly to re-establish analgesia using locally agreed protocols. This approach will maximize patient satisfaction and hopefully increase the pleasure and satisfaction of childbirth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a long history of attempts to alleviate the pain of childbirth, particularly in Asian and Middle Eastern civilisations.[1,2] Some of these techniques might be considered primitive by today’s standards, for example, chanting rituals, religious incantations and even the infliction of physical pain as a form of distraction.[1,2] Intoxicating substances such as opium, cannabis and alcohol have also been used. Although the use of alcohol and cannabis during childbirth would provoke outrage now, opioids are considered completely acceptable, and are widely used.[1–3]
It is a widely held view that it was the administration of chloroform by John Snow to Queen Victoria in 1853 popularized the idea that maternal pain during childbirth should be eased.[2,3] However, despite continued advances in obstetric analgesia and anaesthesia, there is still a vogue for ‘natural’ childbirth, using alternative therapies. There is scant scientific evidence for these techniques, but enthusiasm and satisfaction levels are high amongst their advocates and users. One suspects much of this is about patient autonomy.
This article attempts to summarize and guide clinicians in the management of pain during labour.
1. What Are the Analgesic Goals in Labour?
If you ask this question of pregnant women, obstetricians and midwives, you are likely to get a different answer from each. Anaesthetists are somewhat naïve in thinking that people requesting analgesia in labour always desire complete resolution of pain. Evidence that this is not true comes from our own 10-year audit programme for epidural analgesia, which shows that 50% of epidural recipients experience pain at some time, usually during the second stage. Despite this, 97% judge their pain relief to be ‘excellent’ or ‘satisfactory’. This is presumably because women realize that pain is a natural feature of childbirth and are prepared to accept some discomfort during the delivery of their child. It is also accepted wisdom in the UK that, particularly during the second stage of labour when pushing is performed, feeling the pressure of contractions and the sensations of bearing down assists the delivery process. With this in mind, midwives sometimes deliberately allow epidural analgesia to recede towards the end of labour, or at least encourage women to accept breakthrough pain at this time. It is therefore true to say that the management of breakthrough pain sometimes consists of support and encouragement rather than the use of medical intervention.
2. What is Breakthrough Pain in Labour?
The commissioned title of this article suggests that pain can be prevented during labour, and that there are specific procedures to follow when pain returns. This is misleading. Labour is always painful, although a minority of women find the discomfort easily manageable. The majority of UK parturients request some analgesia at some stage,[4] but only epidural analgesia and its variants can offer the potential for complete pain relief. All other analgesic modalities merely obtund pain, never abolish it. Strictly speaking, it is only at the onset of labour or during epidural analgesia that pain can be said to ‘break through’. We shall describe these as ‘primary’ and ‘secondary’ breakthrough pain, respectively.
2.1 Primary Breakthrough Pain
We define primary breakthrough pain as the point at which women find the contractions of labour severe enough to request analgesia, and this can be anytime from the first uterine tightening to the onset of pushing. Natural childbirth advocates feel delaying or avoiding analgesics is desirable, and this seems a sensible approach, minimising the adverse effects and complications that analgesia can introduce. As an absolute ideology, the authors would reject this. It may be true that antenatal education, followed by support during labour from an educated and empathic birth partner can delay the onset of primary breakthrough pain, and this should be seen as beneficial prophylaxis for all women.
There are, however, several uncontrollable factors that will make labour more painful at an early stage, and it may be futile and cruel to delay the early administration of analgesia in such circumstances. Examples include large babies, occipito-posterior orientation of the foetal head, induction of labour and the personality and resilience of the woman. The key is a flexible approach, considering the requirements and circumstances of each individual patient rather than attempting to satisfy a rigid algorithm or, even worse, pursuing an anti-analgesic ideology.
2.2 Secondary Breakthrough Pain
Most women who receive epidural analgesia have done so after reaching their perceived pain limit, and express enormous relief and gratitude at the resolution of their pain. Others receive epidural analgesia before this point, perhaps because of prior experience of painful labour, or because of anticipation of considerable pain through the need to augment labour with oxytocic drugs. Either way, the return of pain, or the failure to satisfy the promise of complete analgesia with an epidural, can lead to dissatisfaction, disappointment, fear and even despair. This is compounded by the fact that drugs administered by the epidural route do not have a rapid onset of action, and each rescue manoeuvre can be expected to take 30 minutes. If the first is not successful, the patient may be in pain for at least an hour before analgesic control is restored, and she may even deliver before it is achieved. Satisfaction is often low in these circumstances, so we promote an aggressive approach to both the prevention and treatment of secondary breakthrough pain.
3. Management of Primary Breakthrough Pain
In UK practice, there are three basic pharmacological approaches to primary breakthrough pain in labour.[5] These are: (i) inhalational agents such as nitrous oxide and oxygen (Entonox); (ii) parenteral (intramuscular or intravenous) opioids such as pethidine (meperidine) or diamorphine; and (iii) epidural analgesia, using local anaesthetic and opioid combinations.
The first two options are popular with UK midwives, because they can prescribe and administer these agents without needing input from medical staff.
3.1 Inhalational Analgesia
3.1.1 Nitrous Oxide-Oxygen (Entonox)
Entonox, a 50 : 50 mixture of nitrous oxide and oxygen,[6–8] is used ubiquitously in the UK[5] as the drug of first choice to control labour pain because of its safety and near-ideal pharmacokinetic profile. The rapid onset of action and offset give the potential for useful effect during contractions, with minimal background adverse effects between them.
Nitrous oxide is analgesic, but is a weak anaesthetic.[7–9] A concentration of 50% is most unlikely to result in unconsciousness, and full anaesthesia is impossible in the absence of other hypnotic agents.[7–9] Proposed mechanisms of action include a combination of NMDA receptor antagonism, stimulation of endogenous opioid release in the brain and activation of descending noradrenergic inhibitory pain pathways.[9] It has a low blood gas solubility coefficient (0.47), which means it achieves high alveolar, blood and brain partial pressures very quickly during inhalation.[7–9] It thus produces therapeutic analgesic levels within 30 seconds of starting inhalation and offsets as quickly when inhalation is discontinued.[7,8] To achieve the ideal combination of rapid analgesia with a drug-free period between contractions, slow, deep inhalation should begin at the first twinge of contraction pain, with a return to breathing room air at the peak of the contraction.
The evidence for the therapeutic benefits of Entonox are equivocal, with some papers describing an analgesic benefit, and others little.[10,11] Entonox is an analgesic of modest potency at a concentration of 50%.[6–8] Many women will find it effective in early labour, but inadequate as contractions intensify, particularly if labour is augmented with oxytocin. Others simply do not enjoy the feeling of intoxication that is inevitable during Entonox inhalation. It remains one of the first drugs to use in early labour, and many women will continue to preach its virtues.
3.1.2 Other Inhalational Drugs
The use of inhalational anaesthetics like chloroform, and then trichloroethylene and methoxyflurane lie in the history of obstetric analgesia,[3] but agents such as isoflurane, desflurane and, most significantly, sevoflurane are now being investigated.[5] Isoflurane has been added to Entonox in sub-anaesthetic doses to provide superior patient satisfaction scores.[5]
The newest area of research is with sevoflurane. Studies have shown that an inhalational dose of 0.8% provides an excellent balance of pain relief and reduced risk of sedation compared with higher concentrations.[12,13] Compared with Entonox, sevoflurane 0.8% gave greater pain relief, and although it did produce more sedation, this was felt to be a favourable characteristic by the mothers.[14] As with all inhalational anaesthetics, there is a theoretical risk of uterine relaxation, and an effect on contractions.[8] There are few data on labouring women, but on isolated uterine muscle sevoflurane produces a dose-dependent inhibition of contractility.[15,16] Further investigation of maternal and foetal effects is required before this technique can be recommended without reservation.
3.2 Opioids
Opioids (administered intramuscularly or intravenously) have many theoretical disadvantages for labour pain management, the principal ones being the inability to achieve adequate analgesia without causing maternal sedation between contractions, and respiratory depression of the neonate. Doses are limited because of these reasons, making opioid analgesia no more effective than Entonox.[17,18] We use opioids mainly in the early stages of labour, assisting rest and sleep. UK anaesthetists see opioids as a very poor option, being particularly concerned about their delaying action on gastric emptying and the consequent increased risk of regurgitation of stomach contents should general anaesthesia be required.[5–7] Midwives do, however, appreciate having these drugs available, especially in settings without the availability of epidural analgesia, such as midwifery-led maternity units and for home deliveries.
3.2.1 Pethidine (Meperidine)
Pethidine is a synthetic opioid drug derived from phenylpiperidine,[5–8] and is the most commonly used opioid for labour analgesia in the UK.[19] It does have a poor side effect profile, being one of the weaker analgesics in the opioid family.[6–8] It frequently causes nausea and vomiting, and may accumulate in the foetus for up to 4 hours after administration, potentially causing foetal respiratory depression.[5,7] This is due to its lipid solubility, allowing it to pass across the placenta more freely and become trapped in the foetal circulation in the ionized form.[5–7] The other issue with pethidine relates to one of its metabolites, norpethidine. Norpethidine has half the analgesic potency, six times the half-life and twice the stimulant effect of the parent compound, occasionally resulting in tachycardias and pyrexias, and rarely convulsions and coma.[5–8]
3.2.2 Diamorphine
A recent survey of opioid prescribing in consultant-led maternity units showed that diamorphine is increasingly used, being available in one-third of labour wards.[20] The advantages of diamorphine are that it is a potent opioid with high lipid solubility, and so has a fast onset of action.[6–8] It also has a longer duration of action than pethidine.[6–8] Studies show that it does provide some benefits over pethidine. It may provide better analgesia,[5,21] less nausea and vomiting,[22] and higher foetal Apgar scores.[22] In our unit, diamorphine is often used when an intra-uterine death has occurred, to provide analgesia, but to also aid sleeping.
3.2.3 Other Opioids
There are a number of other drugs that are either used throughout the world in maternity units or are being studied. One example is meptazinol, a partial agonist at the μ-opioid receptor.[6–8] It provides more cardiovascular stability, less respiratory depression and fewer foetal effects than pethidine at equi-analgesic doses.[23,24] It does, however, produce a higher incidence of nausea and vomiting.[7,23,24]
3.2.4 Patient-Controlled Opioid Analgesia
Fast-acting, short-duration and non-accumulating opioids used in an on-demand device should in theory provide good analgesia for patients in labour.
Diamorphine has been used in a patient-controlled device to try and mimic the advantages of Entonox, but research shows it to be no more beneficial than via the intramuscular route.[25]
Fentanyl and alfentanil have been used, as 50 μg or 500 μg boluses, respectively. Fentanyl was shown to provide more effective analgesia, with similar neonatal outcomes.[26]
The emergence of remifentanil, with its advantageous pharmacokinetic profile,[7] heightened interest in the use of parenteral opioids in a patient-controlled device. Remifentanil is a synthetic, pure μ-receptor agonist, which is rapidly broken down by nonspecific plasma and tissue esterases.[5–8] Its duration of action is determined by metabolism and not distribution (like fentanyl and alfentanil), and as a result of the abundance of these esterases the elimination half-life of remifentanil is 3–10 minutes.[6–8] In light of these properties, there is little risk of drug accumulation, and so remifentanil is associated with a reduced risk of adverse effects when used in prolonged labour. In addition, because the metabolism of remifentanil is not affected by plasma cholinesterase, there is little consequence in patients with cholinesterase deficiency.[7] Several studies have looked at its use, with or without a background infusion, using a bolus dose of 25–50 μg up to every 5 minutes.[27–29] Although some mothers were sleepy, they were always rousable.[27] Not surprisingly, the more remifentanil used, either via increased background infusion doses or bolus dose, the greater the likelihood of cardio-respiratory depression.[27,28] This makes appropriate monitoring essential during usage. Foetal Apgar scores at 1 and 5 minutes had a median of 9.[27]
Fentanyl and remifentanil do offer genuine alternatives to regional analgesia in the parturient, providing on-demand pain relief and good foetal outcomes.
3.3 Epidural Analgesia
Approximately 25% of women in the UK and 66% in the US receive epidural analgesia during labour,[30] with a wide variation between units. This variation may depend on the availability of anaesthetists, who are required for catheter insertion and ongoing management. However, in the authors’ city, two similar tertiary referral maternity units have epidural rates of 29% and 55%, for no obvious reason except perhaps differences in midwifery culture. What is more consistent is the efficacy of epidural analgesia, which produces satisfaction scores impossible with other analgesic methods.[31]
Of course, the term ‘epidural analgesia’ only describes a route of drug administration. It is the details of the technique employed to access the epidural space and the drug regimen subsequently administered that determines efficacy, adverse effects and complications. Comments such as “epidurals cause leg weakness” are therefore very misleading, because this particular adverse effect is drug and dose dependent, and can be largely avoided.
Having said this, there are some basic principles of achieving successful epidural analgesia that are widely accepted. These will be discussed in some detail, because the successful initiation and maintenance of epidural analgesia is the key to preventing secondary breakthrough pain. These basic principles cover:
-
epidural catheterization techniques;
-
the use of the intrathecal route;
-
choice of drugs for the epidural and intrathecal routes;
-
methods of maintaining analgesia.
3.3.1 Epidural Catheterization
Epidural drugs need to be delivered into the appropriate part of the epidural space if the target nerve roots are to be adequately bathed in the delivered drugs. In the context of labour pain, which is transmitted via nerve roots from the tenth thoracic to the sacral segments,[8] it is most appropriate to site an epidural catheter between mid-to-high lumbar vertebral spaces, being the mid-point of the nerve roots needing to be covered. Even then, the method of locating the epidural space has some influence. Loss of resistance to injection is the basic technique employed by anaesthetists, but if air is used for this purpose, air bubbles can form when therapeutic solutions are subsequently injected. These can prevent adequate contact between the solution and the nerve route, leading to missed segments of analgesic blockade and the delay of adequate analgesia.[32] This technique is commonly used in the US and Asian subcontinent, whereas loss of resistance to saline is preferred in the UK in the belief that more reliable initial analgesia is achieved.
The length of epidural catheter threaded into the epidural space is also important. An excessive amount can result in the catheter tip leaving the epidural space through an intervertebral foramen, leading to inadequate drug distribution, or increased risk of epidural vein cannulation.[33] On the other hand, too short a length can predispose to catheter displacement. Around 5 cm is a sensible compromise, perhaps increasing this slightly for the obese patient.[34] There is also an argument for predicted longer labours, up to 6 cm should be inserted to reduce the risk of displacement and failure.[33] This uses the idea that you can always withdraw the catheter slightly if required, but you cannot put more in.
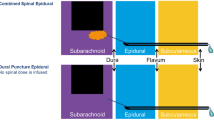
3.3.2 Intrathecal Drug Administration
A loading dose given into the epidural space will achieve maximum effect within 15–30 minutes, depending on the drug concentration and volume, and the intensity of contraction pain. This onset time can be reduced to 5–10 minutes by injecting drugs directly into the CSF. Missed segments due to poor drug distribution, which can be caused by fibrous septa within the epidural space, are less likely with the intrathecal technique. However, dural puncture introduces the potential complications of post-dural puncture headache and, albeit very rarely, meningitis.[35,36] It is therefore a matter of controversy whether the saving of a few minutes of pain over the course of a whole labour is justified. Some units never use the intrathecal route, others always use it and others employ the technique when faced with an extremely distraught patient. This latter approach is employed in our unit, resulting in a 14% use of the intrathecal route for initial analgesia.
3.3.3 Drug Choices
The principal class of drug used to achieve epidural and intrathecal analgesia is local anaesthetic agents. By far the most commonly used is bupivacaine, with some units preferring the more expensive ropivacaine. These drugs effectively block conduction in pain fibres, but inevitably also block touch, motor and autonomic fibres.[7,8] This results in the main adverse effects of neuraxial-administered local anaesthetics: numbness, immobility and hypotension.[8]
The use of bupivacaine in a concentration of 0.25% was widely used in the 1980s and early 1990s in the UK, and the adverse effects described were common. Nowadays, most UK units employ a combination of 0.1% bupivacaine mixed with 2 μg/mL of the opioid fentanyl (Dresner M, UK National Survey, unpublished data). Given via the epidural route, fentanyl may have its effect through systemic absorption into the blood stream, but it also attaches to μ-receptors in the substantia gelatinosa of the dorsal horns of the spinal cord.[7,8] Analgesia is achieved without the usual opioid adverse effects of sedation and nausea, because central receptors are not significantly occupied. This is also true of the intrathecal route, although pruritis is then a common minor adverse effect.[6–8] Fentanyl, thereby, has a sparing effect on local anaesthetics, the concentration of which can be reduced to the point where the adverse effects are minimized. This approach has been shown to increase patient satisfaction, and even reduce the number of operative deliveries experienced by epidural recipients.[37]
3.3.4 Maintaining Epidural and Intrathecal Analgesia
Whichever route is employed to initiate analgesia, it is the administration of epidural drugs that allows its continuation. There are three choices of technique, which can be combined as necessary: (i) intermittent bolus injection; (ii) continuous infusion; and (iii) patient-controlled boluses.
Intermittent Bolus Injection
Intermittent bolus administration has the advantages of not requiring expensive delivery equipment and possibly reducing the total drug dosage. This may reduce the adverse effects quoted above, but is relatively labour intensive in requiring the midwife or anaesthetist to draw up, check and administer the bolus. Given the relatively slow onset time of each bolus, some anticipation and education is required if breakthrough pain is to be avoided. Compared to the other techniques, it produces similar satisfaction scores for analgesia by patients.[38]
Continuous Infusion
Continuous infusions are known to increase the total drug dose given throughout labour, and there is no doubt that a cumulative effect can lead to more intense motor blockade than the other two maintenance techniques.[39] It was for this reason that we attempted to reduce and subsequently remove continuous infusions from our regimen. However, this led to small but noticeable downward trends in patient and midwife satisfaction scores that were reversed when the original regimen was restored.[40] In reality, good education and understanding by the midwives may have avoided this. However, it became apparent that after many years of reliance on the relatively labour-sparing infusion technique, the midwives did not have the experience to respond to breakthrough pain promptly. Whilst this predominance of local culture over theory and evidence was disappointing, the proposed benefits of reducing total dosage have probably been overstated. The research that demonstrated improved satisfaction and normal deliveries by using low concentration solutions[37] led to the assumption that further benefits could be gained by preserving motor function throughout labour. It has since been shown that mobility per se has no advantage in terms of obstetric outcomes as long as low concentration solutions are used.[41,42] We have also shown through a patient questionnaire study in our unit that most women are not prepared to sacrifice any analgesia for more mobility.[43] We are, therefore, comfortable with our use of continuous infusions, despite the theoretical advantages of the other maintenance techniques.
Patient-Controlled Boluses
Patient-controlled epidural top-ups, with or without a background infusion, have been shown to be very effective, and have the attractive feature of handing some autonomy to the patient.[38,39,44] Again, because of the lag time for the onset of action of each bolus, patients need a level of education and intelligence to get the best from this technique. If local culture and the cost of the necessary equipment were not issues, the authors would have adopted this technique.
Continuous infusions and patient-controlled top-ups should employ dosage regimens that are effective but not excessive, but there is obviously some inter-patient variation in dose requirements. It is therefore inevitable that some patients will experience excessive blockade, requiring their infusions to be temporarily discontinued. Conversely and more commonly, periods of breakthrough pain can occur, particularly as contractions intensify with advancing labour. In this circumstance, these techniques need to be augmented with a midwife- or anaesthetist-administered top-up bolus. These are usually effective, but on occasions analgesic control is lost. This situation requires careful analysis and prompt action if patient confidence and satisfaction is not to be lost.
4. The Management of Secondary Breakthrough Pain During Epidural Analgesia
In the authors’ unit, only 3% of recipients score their labour epidurals as poor or useless. This demonstrates that from the patients’ perspective, which after all is the most important, epidural analgesia using the principles described in section 3.3 is extremely effective. However, we believe this level of failure would be higher if breakthrough pain was not promptly and aggressively managed. Thoughtful analysis of symptoms and consideration of the differential diagnosis are the keys to rapid resolution of the problem.
4.1 General Strategy
Every manoeuvre to remedy epidural breakthrough pain takes about 30 minutes given the time to prepare solutions and administer them, and the relatively slow onset time. It is therefore easy to understand how an overly cautious approach can lead to 2 hours of unresolved pain, during which delivery might occur. Dissatisfaction is the likely result. We therefore advocate the following general strategy.
-
Aim to restore analgesia in a maximum of 60 minutes.
-
Offer immediate analgesic ‘first aid’ in the form of Entonox.
-
Assess the pattern of breakthrough pain, consider the differential diagnosis (especially catheter dislodgment) and proceed to rescue dose or epidural catheter replacement as appropriate.
-
If the rescue dose is ineffective at 30 minutes, resite the epidural catheter with a combined intrathecal and epidural technique (this gives more rapid onset of analgesia, and also bypasses obstacles such as epidural fibrous septa).
There are three common patterns of breakthrough pain during epidural analgesia, each with its own list of causes and appropriate solutions.
4.2 Global or Upper Abdominal Pain
Global or upper abdominal pain usually occurs because the volume of drug administered is insufficient to bathe all the necessary nerve roots, and is simply remedied by increasing infusion rates or the volume of top-up boluses. In our experience, 0.1% bupivacaine with 2 μg/mL of fentanyl is almost always effective, with boluses of up to 20 mL sufficient to remedy this kind of breakthrough pain. On rare occasions, a solution containing either stronger local anaesthetic, fentanyl or both might be required for intense pain during augmented labour.
If global or upper abdominal breakthrough pain is not abolished by such a top-up, or even intensifies despite the top-up, it is most likely that the epidural catheter has become dislodged and needs replacing. It is therefore important to check the epidural puncture site for evidence of catheter displacement early in the process of managing breakthrough pain.
4.3 Unilateral Block
Unilateral block has become relatively rare since the introduction of epidural opioids. It is caused by uneven spread of drug solutions within the epidural space. This can occur because of poor catheter position, most commonly caused by passing too much catheter into the epidural space. The manoeuvre of withdrawing the epidural catheter and giving a drug top-up is completely avoidable by not putting in too much catheter in the first place.
A simple cause of unilateral breakthrough pain is prolonged lateral positioning of the patient. The flow of drug solutions within the epidural space is affected to some extent by gravity, and so women resting on one side can develop intense blockade in the dependent side and breakthrough pain in the uppermost side. For this reason, and for pressure area care, midwives should be careful not to allow women with epidurals to remain motionless for prolonged periods of time. The solution is simply to ask the women to lie with the painful side down and to give an epidural drug top-up.
Unilateral blockade is occasionally resistant to such treatment manoeuvres, and in these circumstances it is possible that fibrous septa within the epidural space are preventing adequate drug distribution. In this situation, the epidural should be resited at a different interspace, and it makes sense to initiate this analgesia with an intrathecal injection so as to bypass the epidural space. This way, 90 minutes of analgesia will be delivered even if the resited epidural catheter is affected by the same problem. This may be enough for delivery to be achieved.
4.4 Persistent Perineal Pain or Pressure
Persistent perineal pain or pressure usually occur in situations of extreme stimulation, such as with a large baby, occipito-posterior presentation, augmentation of labour with oxytocin or a combination of these. It can be extremely difficult to achieve complete analgesia in this situation without causing profound motor block in the legs, so it is wise to warn patients of this fact at an early stage. A top-up of 20 mL of the aforementioned solution should be given in the sitting position. If this fails, a further 10 mL of 0.25% bupivacaine with 50–100 μg fentanyl is justified if the patient accepts the likely consequence of increased motor block.
5. Conclusion
Most of the patients in the authors’ unit are very satisfied with the analgesia we provide for them, and it is our aim to make every patient this happy. Our methods and regimens have been changed and adapted over many years, taking into account information from our continuous ongoing audit of mother and midwife satisfaction scores, but also new developments in obstetric anaesthesia.
It is important to treat all breakthrough pain aggressively to get the best results, with the aim of getting the patient comfortable within 60 minutes, if not sooner.
References
Natural childbirth techniques [online]. Available from URL: http://www.manbit.com/obstetspain/obnatindx.htm [Accessed 2007 Oct 24]
Wikipedia. Anesthesia [online]. Available from URL: http://en.wikipedia.org/wiki/Anesthesiology [Accessed 2007 Oct 24].
Yentis SM, Hirsch NP, Smith GB. Anaesthesia and intensive care A-Z: an encyclopaedia of principles and practice. 3rd ed. London: Elsevier Butterworth-Heinemann, 2005
Lally JE, Murtagh MJ, Macphall S, et al. More in hope than expectation: a systematic review of women’s expectations and experience of pain relief in labour. BMC Med 2008; 6: 7
Wee M. Analgesia in labour: inhalational and parenteral. Anaesth Intensive Care Med 2004; 5: 233–4
Sasada M, Smith S. Drugs in anaesthesia and intensive care. 2nd ed. Oxford: Oxford University Press, 2002
Peck TE, Hill SA, Williams M. Pharmacology for anaesthesia and intensive care. 2nd ed. Cambridge: Cambridge University Press, 2003
Aitkinhead AR, Rowbotham DJ, Smith G. Textbook of anaesthesia. 4th ed. London: Churchhill Livingstone, 2001
Bricker S. The anaesthesia science viva book. Cambridge: Cambridge University Press, 2004
Carstoniu J, Levytam S, Norman P. Nitrous oxide in early labour: safety and analgesic efficacy assessed by a double blind, placebo-controlled study. Anesthesiology 1994; 80: 30–5
Su F, Wei X, Chen X, et al. Clinical study on the efficacy and safety of labour analgesia with inhalation of nitrous oxide in oxygen. Zhonghua Fu Chan Ke Za Zhi 2002; 37: 584–7
Toscano A, Pancaro C, Giovannoni S, et al. Sevoflurane analgesia: a pilot study. Int J Obstet Anesth 2003; 12: 79–82
Yeo ST, Holdcroft A, Yentis SM, et al. Analgesia with sevoflurane during labour: I. Determination of the optimum concentration. Br J Anaesth 2007; 98: 105–9
Yeo ST, Holdcroft A, Yentis SM, et al. Analgesia with sevoflurane during labour: II. Sevoflurane compared with Entonox for labour analgesia. Br J Anaesth 2007; 98: 110–5
Yoo KY, Lee JC, Yoon MH. The effects of volatile anaesthetics on spontaneous contractility of isolated human pregnant uterine muscle: a comparison among sevoflurane, desflurane, isoflurane and halothane. Anesth Analg 2006; 103: 443–7
Yildiz K, Dogru K, Dalgic H, et al. Inhibitory effects of desflurane and sevoflurane on oxytocin induced contractions of isolated pregnant human myometrium. Acta Anaesthesiol Scand 2005; 49: 1355–9
Olofsson C, Irestedt L. Traditional analgesic agents: are parenteral narcotics passe and do inhalational agents still have a place in labour? Baillieres Clin Obstet Gynaecol 1998; 12: 409–21
Yentis SM. Proposer: the use of Entonox for labour pain should be abandoned. Int J Obstet Anesth 2001; 10: 27–9
Elbourne D, Wiseman RA. Types of intra-muscular opioids for maternal pain relief in labour. Cochrane Database Syst Rev 2000; (2): CD001237
Tuckey JP, Prout RE, Wee MY. Prescribing intramuscular opioids for labour analgesia in consultant-led maternity units: a survey of UK practice. Int J Obst Anesth 2008: 17; 3–8
Saravanakumar K, Garstang JS, Hasan K. Intravenous patient-controlled analgesia for labour: a survey of UK practice. Int J Obst Anesth 2007; 16: 221–5
Fairlie FM, Marshall L, Walker JJ, et al. Intramuscular opioids for maternal pain relief in labour: a randomised control trial comparing pethidine with diamorphine. Br J Obstet Gynaecol 1999; 106: 1181–7
Osler M. A double blind study comparing meptaziniol and pethidine for pain relief in labour. Eur J Obstet Gynecol Reprod Biol 1987; 26: 15–8
Morrison CE, Dutton D, Howie H, et al. Pethidine compared with meptazinol during labour: a prospective randomised double blind study in 1100 patients. Anaesthesia 1987; 42: 7–14
McInnes RJ, Hillan E, Clark D, et al. Diamorphine for pain relief in labour: a randomised controlled trial comparing intramuscular injection and patient-controlled analgesia. Br J Obstet Gynaecol 2004; 111: 648–55
Morley-Forster PK, Reid DW, Vandeberghe H. A comparison of patient-controlled analgesia fentanyl and alfentanil for labour analgesia. Can J Anaesth 2000; 47: 113–9
Voilikas I, Butwick A, Wilkinson C, et al. Maternal and neonatal side effects of remifentanil patient-controlled analgesia in labour. Br J Anaesth 2005; 95: 504–9
Roelants F, De Franceschi E, Veyckemans F, et al. Patient-controlled intravenous analgesia using remifentanil in the parturient. Can J Anaesth 2001; 48: 175–8
Balki M, Kasodekar S, Dhumne S, et al. Remifentanil patient-controlled analgesia for labour: optimizing drug delivery regimens. Can J Anaesth 2007; 54: 626–33
McGrady E, Litchfield K. Epidural analgesia in labour. CEACCP 2004: 4; 114–7.
Dickinson JE, Paech MJ, McDonald SJ, et al. Maternal satisfaction with childbirth and intrapartum analgesia in nulliparous labour. Aust N Z J Obstet Gynaecol 2003; 43: 463–8
Norman D, Winkelman C, Hanrahan E, et al. Labour epidural anaesthetics comparing loss of resistance to air versus saline; does the choice matter? AANA J 2006; 74: 301–8
D’ Angelo R, Berkebile BL, Gerancher JC. Prospective examination of epidural catheter insertion. Anesthesiology 1996; 84: 1524–5
Beilin Y, Bernstein HH, Zucker-Pinchoff B. The optimal distance that a multiorifice epidural catheter should be threaded into the epidural space. Anesth Analg 1995; 81: 301–4
Harding SA, Collis RE, Morgan BM. Meningitis after combined spinal-extradural anaesthesia in obstetrics. Br J Anaesth 1994; 73: 545–7
Cascio M, Heath G. Meningitis following a combined spinal epidural technique in a labouring term parturient. Can J Anaesth 1996; 43: 399–402
Collis RE, Davies DWL, Aveling W. Randomised comparison of combined spinal-epidural and standard epidural analgesia in labour. Lancet 1995; 345: 1413–6
Purdie J, Reid J, Thorburn J, et al. Continuous extradural analgesia: comparison of midwife top-ups, continuous infusions and patient controlled administration. Br J Anaesth 1992; 68: 580–4
Collis RE, Plaat FS, Morgan BM. Comparison of midwife top-ups, continuous infusion and patient-controlled epidural analgesia for maintaining mobility after a low-dose combined spinal-epidural. Br J Anaesth 1999; 82: 233–6
Jones M, Dresner M. Long term audit of satisfaction with epidural analgesia. Int J Obstet Anesth 2002; 11 Suppl.: 31
Collis RE, Harding SA, Morgan BM. Effect of maternal ambulation on labour with low-dose combined spinal-epidural analgesia. Anaesthesia 1999; 54: 535–9
Wilson MJ, Cooper G, MacArthur C, et al. Comparative Obstetric Mobile Epidural Trial (COMET) Study Group UK. Anesthesiology 2002; 67: 1567–75
Charlton JS, Dresner M, Freeman J. The role of motor block in patient satisfaction with epidural analgesia. Int J Obstet Anesth 2000; 9: 202
Van der Vyver M, Halpern S, Joseph G. Patient-controlled epidural analgesia versus continuous infusion for labour analgesia: a meta-analysis. Br J Anaesth 2002; 89: 459–65
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akerman, N., Dresner, M. The Management of Breakthrough Pain During Labour. CNS Drugs 23, 669–679 (2009). https://doi.org/10.2165/00023210-200923080-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200923080-00004