Abstract
Background
A few studies have examined the association between different types of dietary fiber as well as their sources and the risk of breast cancer (BC) and the present study aimed to investigate these associations in a case-control study among Iranian women.
Methods
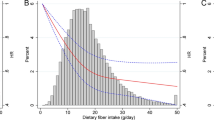
A total of 464 women with pathologically confirmed breast cancer within the past year and 498 age-matched healthy controls were included. Dietary intakes were assessed using a 168-item food frequency questionnaire. The association between dietary soluble, insoluble, total dietary fiber, as well as, fiber from fruits, vegetables, legumes, cereals, and nuts intake with odds of breast cancer was assessed using multivariate logistic regression analysis.
Results
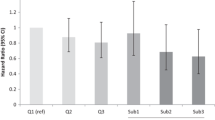
Mean total dietary fiber intake of patients with and without cancer were 33.1 ± 15.3 g per day (g/d) and 34.2 ± 16.5 (g/d), respectively. Dietary total fiber (OR = 0.65; 95%CI: 0.47–0.90, Ptrend = 0.01), insoluble fiber (OR = 0.68; 95%CI: 0.49–0.93, Ptrend = 0.01), fruits’ fiber (OR = 0.68; 95%CI: 0.49–0.94, Ptrend = 0.02), and vegetables’ fiber (OR = 0.66; 95%CI: 0.48–0.91, Ptrend = 0.01) were significantly associated with reduced likelihood of developing breast cancer in all participants. Furthermore, dietary total and insoluble fiber, as well as, fiber from fruits were significantly associated with lower odds of breast cancer in premenopausal women (P < 0.05). In contrast, cereals’ fiber significantly increased the risk of breast cancer by 84% in premenopausal women (OR = 1.84; 95%CI: 1.18–2.86, Ptrend = 0.009). In postmenopausal women, cereals’ fiber had a significant inverse association with odds of breast cancer (OR = 0.56; 95%CI: 0.31–1.03, Ptrend = 0.04). Also, fiber from vegetables was significantly associated with a lower risk of breast cancer in postmenopausal women (OR = 0.53; 95%CI: 0.30–0.94, Ptrend = 0.03).
Conclusion
Dietary fiber intake and more specifically insoluble, fruits’, and vegetables’ fiber intake might be associated with a reduced breast cancer risk, particularly in premenopausal women. Future prospective investigations are needed to confirm these findings.
Similar content being viewed by others
Introduction
Breast cancer (BC) with the age-standardized incidence of 47.8 per 100 000 globally was the second leading cause of cancer after lung cancer in 2020 and the first one in females which imposes a high economic burden on the health care system [1, 2]. Similar to western countries, BC is a major public health problem among women in the Middle East, as one-third of total cancer cases and 24% of total cancer deaths were due to breast cancer [3]. In Iran, 16 967 cases of breast cancer were diagnosed in 2020 and the disease was responsible for the highest number of cancer deaths among women [4].
Non-modifiable risk factors include aging, genetic predisposition, early menarche (< 12 years), late menopause (> 55 years), experiencing the first pregnancy over 30 years of age, and infertility, as well as, modifiable lifestyle related factors like use of contraceptives, hormonal treatment after menopause, no breastfeeding, physical activity, and being overweight or obese have been associated with BC incidence and recurrence [4,5,6,7,8,9]. Previous studies support the hypothesis that dietary intake is also associated with the risk of breast cancer [10,11,12,13]. It has been proposed that foods like dairy products [14], soy food [15], unrefined cereals [1] and olive oil [16] have a protective effect on the risk of breast cancer. In contrast, alcohol use, saturated fatty acids, red and processed meat intake increase the risk of BC [1, 17, 18]. Dietary fiber as a part of plant materials is known as a substance with beneficial effects on human health [19, 20]. Systematic reviews and meta-analyses of prospective studies showed that total dietary fiber is associated with a reduced risk of BC [21, 22]. In addition, several animal studies have examined the effect of different types of dietary fiber (soluble and insoluble fiber) on breast cancer risk [23]. Moreover, a meta-analysis of prospective studies showed a significant inverse association between soluble fiber intake and BC risk while no such association was observed for insoluble fiber [21].
Recently, studying the relationship between dietary fiber from several food groups like fruits, vegetables, cereals, legumes and nuts, which provide a large percentage of dietary fiber, with breast cancer risk has attracted researchers’ attention [24]. A meta-analysis of prospective studies illustrated that fruit originated fiber significantly decreases the risk of breast cancer [21]. However, San Francisco case-control study found no association between either fiber intake from vegetables and fruits or total fiber intake with breast cancer risk while higher intake of fiber from grains and beans reduced the risk by about 20% [25]. In contrast, Zhang et al. reported an inverse association between vegetable and fruit fiber intake but a null association was observed between cereal fiber intake and the risk of BC [26]. A meta-analysis including 6 cohort studies also showed no significant association between nut consumption and breast cancer [27]. However, recent investigations have proposed a protective effect for nuts intake [28, 29].
Countries with low and medium income have a greater burden of premenopausal breast cancer for both new cases and deaths compared with higher income countries [30]. As premenopausal and postmenopausal breast cancer has increased worldwide, early prevention is essential to control the burden of breast cancer in all parts of the world. To address these important gaps, this study aims to examine the association between types and sources of fiber with the overall odds of breast cancer and according to menopausal status among Iranian women in a large case–control study. To the best of our knowledge, this is the first study to assess the relationship between soluble and insoluble fiber intake and also dietary fiber from different sources with the chance of developing breast cancer in the Middle-East.
Methods
Participants
This was a hospital-based, case–control study among Iranian women aged 19–80 years which was conducted between 2014 and 2016 at the Cancer Institute, located at Imam Khomeini Hospital Complex, Tehran, Iran. Cases were patients with histopathologically confirmed breast cancer in the preceding year, without history of any other cancers and long-term dietary restrictions. Apparently healthy subjects including visitors, relatives, and friends of non-cancer patients who were hospitalized for other chronic diseases in the same hospital and had no long-term dietary restrictions were recruited as controls. To assure that the distribution of cases and controls regarding age (± 10 years) and the geographic place of living were the same, they were frequency-matched (controls were selected based on the frequency of age and also the living place of controls). We excluded individuals with total energy intake of > 4500 or < 800 kcal/d (n = 116) and who did not respond to more than 70 items of the food frequency questionnaire (FFQ, 1.85% cases, 3.05% controls, n = 25) from this study. Finally, 464 cases and 498 controls remained for the final analysis. The study was approved by the Bioethics Committee of Iran Cancer Institute, Tehran University of Medical Sciences, Tehran, Iran, and all participants signed informed consent (ethics code: 93-03-51-27113).
Assessment of dietary intake
A food frequency questionnaire (FFQ) filled by interview was used to assess participants’ usual diet over the preceding year [31, 32]. The validity and reliability of the FFQ were also confirmed by comparing two FFQs completed 1 year apart and the average of 12 dietary 24-hour recalls in a previous study [31, 33]. The FFQ was a block-format questionnaire containing 168 food items with standard serving size. Participants were requested to report their consumption on a daily, weekly, or monthly basis. When the participants could not report their frequency of consumption with the given portion sizes, they were requested to report their own portion sizes for food items. Then dietitians calculated daily intake of reported food items and converted them to grams per day using household measures. We used the USDA food composition database that was modified for Iranian foods to compute nutrient composition of the consumed foods. To cover seasonal changes in food intake, all participants were asked to report the frequency of food intake regardless of the current time of their availability during the past year. In addition, previous investigations were used to extract the dietary fiber of each food, and then the amount of fiber of each food was multiplied by the gram of the same food intake [34,35,36,37].
Assessment of other variables
Weight was measured using a digital scale to the nearest 100 g while participants wore minimum clothing. Height was measured to the nearest 0.5 cm by a tape measure while the participants stood in a normal position without shoes. Body Mass Index (BMI) was calculated using the following formula: BMI = weight (kg) / heigh (m) squared. Physical activity (PA) was gathered by validated Global Physical Activity Questionnaire (GPAQ) which included sixteen questions in four physical activity domains: job-related activities; transportation activities; recreation and sports activities and sedentary behaviors. This questionnaire was translated to Persian and the measured data were analyzed according to the GPAQ analysis Guide [38] to calculate MET-hours per week values. Additional information on age, education status, family history of breast cancer, alcohol and tobacco use, age at menarche, marital status, pregnancy history, parity, infertility treatment, age at menopause, postmenopausal hormone therapy, and contraceptive use were collected through face-to-face interview.
Statistical methods
Energy-adjusted dietary fibers intake was calculated using residual method [39]. Then, participants were categorized based on tertiles of dietary total fiber, soluble and insoluble fiber, as well as fruits, vegetables, and nuts fiber intake of healthy participants. We used one-way ANOVA or t-test and χ2 test to compare continuous and categorical variables, across tertiles of dietary intakes, respectively. To examine the association between dietary intakes and odds of breast cancer, logistic regression analysis was used in crude and multivariable adjusted models. Participants’ age (continuous) and energy intake were adjusted in the first model. Additional adjustments were done for educational level (un university/university), parity (nulliparous, 1, 2–3, ≥ 4), oral contraceptive use (yes vs. no), cigarette smoking (yes vs. no), alcohol use (yes vs. no), marital status (married, unmarried), physical activity (continuous, Met-h/w), family history of breast cancer (yes vs. no), menopausal status (yes vs. no) and BMI (continuous) in the second model. The analyzes were performed for whole study participants as well as stratified by menopausal status. P values < 0·05 were considered statistically significant. All analyses were performed by STATA version 14 (State Corp., College Station, TX).
Results
In total, 464 cases (aged 45.9 ± 10.3 years) and 498 controls (aged 44.0 ± 11.2 years) were entered into the current analysis. The characteristics of study participants are shown according to tertiles of total dietary fiber intake in participants with and without cancer in Table 1. Participants in the third tertile of dietary total fiber were older (cases: 47.4 νs. 44.4 years, P = 0.03; controls: 45.6 νs. 41.6 years, P < 0.01) and more physically active (cases: 33.4 νs. 15.0 MET h/wk, P = 0.0002; controls: 41.1 νs. 22.4, P < 0.001) than those in the bottom tertile in both case and control groups. Consumption of total dietary fiber intake was significantly different among premenopause and postmenopause women with breast cancer (P = 0.01). Healthy women in the highest tertile of total dietary fiber intake used more oral contraceptives than those in the lowest tertile (P = 0.02). Higher intakes of soluble, insoluble fiber and fiber from fruits, vegetables, and legumes and lower intakes of cereal fiber were found among patients and healthy women in the third tertile of total fiber intake.
Multivariable logistic regression models and 95% CIs were used to assess the association between dietary total fiber, soluble fiber, insoluble fiber, as well as fiber from fruits, vegetables, legumes, and cereals with odds of having BC. There was a significant negative association between dietary total fiber intake and odds of breast cancer among the whole population (Highest vs. lowest tertile: odds ratio (OR) = 0.72; 95% confidence interval (95%CI): 0.53–0.99, Ptrend = 0.04). Although no trend toward significant association was observed between breast cancer risk and insoluble fiber in the whole study population in the crude model, after adjusting for confounder variables, individuals in the third tertile had a lower odd of breast cancer than those in the bottom tertile (Model 2: OR = 0.68; 95% confidence interval (95%CI): 0.48–0.96, Ptrend = 0.03). Also, the chance for developing breast cancer in the highest tertile of dietary fiber intake from fruits was 33% lower compared to the lowest tertile (Model 2: OR = 0.67; 95%CI: 0.47–0.95, Ptrend = 0.02). Women in the third tertile of fiber intake from vegetables had a significantly lower odds of breast cancer compared with those in the bottom tertile in crude and first models; however, we did not find such a significant association in model 2. Furthermore, significant relationship was observed between dietary soluble fiber, as well as, fiber from legumes and cereals, and breast cancer (Table 2).
The stratified analysis revealed that premenopausal women in the third tertile of dietary total fiber intake had lower odds of breast cancer, compared with those in the bottom tertile in the crude model (Table 3). Also, this association remained significant when we adjusted for further confounders in other models. Premenopausal women in highest tertile of insoluble fiber and fiber from fruits intake had also a lower risk of breast cancer compared with those in the first tertile, in model 1 (OR = 0.65; 95%CI:0.43–0.96, Ptrend = 0.03 and OR = 0.63; 95%CI:0.42–0.94, Ptrend = 0.02, respectively). However, after adjustment for further confounders this relationship was disappeared. However, in this population, higher intakes of dietary fiber from cereals were significantly associated with a higher risk of breast cancer, either before or after adjustment for confounders. Women in the third tertile of fiber intake from cereals had an 84% higher odds of developing breast cancer than those in the lower tertile, in model 2 (OR = 1.84; 95%CI: 1.18–2.86, Ptrend < 0.01, Table 3).
In postmenopausal women, there was a significant inverse association between fiber from cereals and odds of breast cancer, either before (Model 1: OR = 0.49; CI = 0.28–0.85, Ptrend = 0.009) and after adjustment for potential confounders (Model 2: OR = 0.56; 95%CI: 0.31–1.03, Ptrend = 0.04). Also, the chance for developing breast cancer in the highest tertile of dietary fiber intake from vegetables was 45% lower compared to the lowest tertile with a significant trend in the first model (Model 1: OR = 0.53; 95%CI: 0.30–0.94, Ptrend = 0.03). But, after adjustment for further confounders this association disappeared. (Table 4).
We also checked and reported multivariable-adjusted odds ratios and 95% CIs for breast cancer across tertiles of fruits, vegetables, nuts, peanuts, almond, walnut, and pistachio intake among the whole population (Table 5) premenopausal (Table 6) and postmenopausal women (Table 7). No significant association was observed in this regard.
Discussion
Overall, the effect of different types and sources of dietary fiber and breast cancer etiology remains uncertain. Also, data on the relationship between fiber consumption and breast cancer are limited in Middle-Eastern countries and most data are from Western nations. The present case-control study showed that dietary total fiber intake and more specifically insoluble, fruits’ and vegetable’ fiber intakes were associated with reduced BC risk. Among premenopausal women, a significant inverse association between dietary total fiber, insoluble fiber, and fiber from fruits and breast cancer was noted. In contrast, fiber from cereals was associated with an increased odds of breast cancer in premenopausal women. However, t in postmenopausal women, vegetables’ and cereals’ fiber were associated with lowered risk of breast cancer.
We found that fiber intake was significantly associated with reduced odds of breast cancer in the whole study population. Two previous case-control studies have reported inverse association between fiber intake and risk of breast cancer [40, 41]. In a study of Uruguayan women, dietary fiber was associated with a strong reduction in the risk of breast cancer with a significant dose-response pattern [40]. Some biological mechanisms have been explained for the beneficial effects of dietary fiber on breast cancer risk. Indirectly, fiber may decrease the risk of breast cancer by controlling blood sugar and lowering levels of insulin resistance [42]. In addition, dietary fiber inhibits the colonic β-D-glucuronidase activity by changing the composition of intestinal microbiota [43] and also may increase serum concentrations of sex hormone–binding globulin (SHBG) [44]; therefore, deconjugation and reabsorption of estrogen are reduced [45]. Thereby, dietary fiber may reduce circulating levels of estrogen and incidence of breast cancer. As a result, dietary fiber promotes cell apoptosis, thereby prevents the development of cancer [46]. The total fiber intake was not associated with breast cancer risk in the Nurses’ Health Study [47]. Deschasaux, M et al. also confirmed the lack of an overall association between the intake of dietary fiber and breast cancer risk in a cohort study [48]. This study also mentioned that the reason for not observing any relationship between total dietary fiber and breast cancer risk might be the lack of statistical power, and insufficient contrast between compared quartiles of dietary fiber intake [48]. The differences between the results of these studies and the current study may be explained by the importance of specific fiber fractions rather than total fiber intake, the genetic variations of study populations, and the differences in the intake of dietary components, such as spices and herbs that contain anticancer agents [49, 50].
It is mentioned that the effect of dietary fiber on breast cancer could differ based on the type of dietary fiber [51]. Dietary fibers generally are grouped in two main components (soluble and insoluble fiber) based on chemical composition [52]. Most plants contain both soluble and insoluble fiber, but in different amounts [53]. Soluble fiber dissolves in water like plant pectin and gums; while insoluble fiber doesn’t dissolve in water like plant cellulose and hemicellulose [52]. In the present study, the intake of insoluble fiber was associated with lower odds of breast cancer after adjustment for several confounders in the whole study population but this association was not significant for dietary soluble fiber. A systematic review and meta-analysis of prospective studies demonstrated that high consumption of total fiber, soluble and insoluble fiber were associated with a reduced risk of breast cancer. Also, similar association was found for dietary total fiber in pre and postmenopausal women [21]. While this finding was not consistent with our findings for soluble fiber as well as for women with postmenopausal breast cancer. The gelatinous environment obtained from soluble fiber, especially with high viscosity, reduces the time of gastrointestinal emptying, digestion and thus absorption after consumption [54]. Estrogens are conjugated in the liver and estrogen metabolites are excreted in the bile [55]. Approximately 80% of the estrogen present in the intestinal tract is decongested by microbiome enzymes and reabsorbed [44]. Therefore, the mechanism by which the soluble fiber modulates blood estrogen concentrations is likely the reduction of estrogen reabsorption and its hepatic intestinal circulation. Also these components of dietary fiber combine with harmful and carcinogenic substances in the gut and promote their discharge and decomposition [56]. Insoluble fiber can promote the production of short-chain fatty acids (SCFAs) by bacterial fermentation in the colon [57]. Studies have found that SCFAs are associated with reduced tumor development [57]. Furthermore, insoluble fibers can promote the growth of probiotics and inhibit the growth of pathogenic bacteria, thereby inhibiting production of carcinogens and promoting their decomposition in the intestine [56].
In this study, we also checked the association between food groups containing fiber including fruits, vegetables, nuts, peanuts, almond, walnut and pistachio and BC. In this study, no significant relationship was observed between these food groups and breast cancer in the whole population as well as pre- and post- menopausal women. Kazemi A et al., conducted a systematic review and meta-analysis of prospective studies for the association of various food groups and risk of breast cancer. This study showed that high intakes of vegetables and fruits were associated with lower risks of breast cancer while no significant association was observed for nuts intake [18]. However, a case-control study found that the high consumption of peanuts, walnuts, or almonds significantly reduced the risk for breast cancer by 2–3 times [58]. Also in another study, it was shown that the pistachio kernel extract beneficially affects the proliferation of breast cancer cells [59]. A large number of recent studies stated that nuts alter lipid metabolism by reducing the ingestion of low-density lipoprotein (LDL) and elementary fatty acids, thereby lowering cholesteryl ethers in cancer cells [28]. The antioxidant components (bioactive molecules) present in nuts [60] can induce apoptosis [61], reduce oxidative DNA damage [28] and proliferation of MCF-7 cells [29]. But in general, studies on the relationship between nuts and occurrence of breast cancer are low and more studies are needed.
When we reanalyzed the results based on menopausal status, a significant association was observed between dietary total fiber, insoluble fiber, fiber from fruits and fiber from cereals and risk of breast cancer among premenopausal women. Unlike insoluble fiber and fiber from fruits, cereal fiber increased the odds of breast cancer in premenopausal women. In contrast, UK Women’s Cohort Study found that fiber from cereals has a protective effect against breast cancer in pre-menopausal women [62]. Contamination of cereals with the mycotoxin Zearalenone may explain our findings. Zearalenone (ZEA) is a mycotoxin with high estrogenic activity which commonly contaminates cereals worldwide [63, 64]. This toxin promotes breast cancer cell growth, DNA synthesis, cell cycle progression and also altered expression of several genes related with breast cancer [65]. Claeys et al. suggested the possible link of ZEA and its metabolites with breast cancer from epidemiological studies [66]. A case-control study also reported the association between urinary ZEA concentrations and breast cancer risk (adjusted OR = 1.54, 95% CI = 1.10–2.77) [67]. There is some evidence that cereals consumed in Iran are also exposed to ZEA contamination. A study in Tehran with 72 samples of rice, bread, puffed corn snack and wheat flour, detected ZEA contamination in cereals [68]. Furthermore, another study confirmed the occurrence of ZEA in Iranian maize [69]. Although the amount of ZEA contamination was lower than the maximum permissible level in Iran, it was higher than similar studies from other regions [70]. Since the cereals are ranked as the first group of foods consumed in Iran and many countries [71], ZEA intake may exceed the standard amount and as a xenoestrogen would increase the estrogenic burden and risk of breast cancer. It should be noted that the toxin is resistant to heating and not disappear during the cooking process [72]. On the other hand, cereals are high GL foods because they contain 50–80% carbohydrates by weight. Several studies have explored the connection between high carbohydrate intake, especially simple carbohydrates, and breast cancer, due to a synergistic effect of insulin resistance and high GL [73]. This could explain why premenopausal women who consume more cereal fiber have a higher risk of breast cancer.
We found a protective association between dietary fibers intake and breast cancer in postmenopausal women. Consistent with this analyzes, another study was conducted by Lubin et al. found higher intake of total fiber decreased the risk of breast cancer in the younger age group, while in the 50-or-over age category the trend was inconsistent [41]. In contrast, a random-effects meta-analysis of prospective observational studies conducted by Farvid et al. demonstrated that high total fiber consumption was associated with a reduced risk of both premenopausal and postmenopausal breast cancer separately while this association was stronger in premenopausal women [21]. The high levels of estradiol can induce the expression of estrogen receptor (ER) in the mammary tissues which affects the cancer cell behavior [74]. Estrogen motivates mammary cell proliferation by regulating the expression of BRCA1 gene [75]. Because circulating estrogen levels play a role in breast cancer, differences in the source of estrogen secretion before and after menopause may explain different findings in pre- and postmenopausal women in this study. In premenopausal women, the main sources of estradiol are ovaries while in postmenopausal women estrogen production by the ovaries is stopped and instead, it is produced as a paracrine factor in a number of extragonadal sites including mesenchymal cells of adipose tissue, osteoblasts and chondrocytes of bone, the vascular endothelium and aortic smooth muscle cells, and numerous sites in the brain [76]. Therefore, circulating estrogen levels in postmenopausal women, unlike premenopausal women, do not stimulate estrogen action, because in these cases circulating estrogen originates from areas outside the gonads and act locally [76]. On the other hand, dietary interventions aimed to reduce serum estradiol levels, have been suggested as a method of preventing breast cancer [77]. Dietary fibers reduce deconjugation and reabsorption of estrogen [45]. However, this beneficial effect of dietary fiber can especially reduce endocrine secretion of estrogen in premenopausal women by lowering the circulating estrogen and then reduce the risk of breast cancer. Since the total level of circulating estrogen drops significantly after menopause, the effect of dietary fiber on estrogen may be more pronounced in premenopausal women than in postmenopausal women.
The current study assessed the link between breast cancer with all fiber sources as well as fiber types by a comprehensive analysis. We also performed subgroup analysis based on the menopausal status and considered a wide range of potential confounders. This case-control study has a large sample size compared to similar studies conducted in the Middle East. However, after subgroup analyses, there was a lack of statistical power for the magnitude of the observed association. Our study has the potential for inherent recall and selection bias due its case-control design, which can restrict us inferring causality. In addition, due to the use of FFQ for dietary assessment, there is a possibility of misclassification of participants in terms of dietary fiber intake. Also, in such designs, it is not possible to check the causal relationship. Another limitation of the study is the possibility of the effect of the outcome of interest on the usual diet of the participants in the case group. The presence of residual confounding variables is also possible.
Conclusion
Our findings demonstrated an inverse association between total dietary fiber, fiber from fruits and fiber from vegetables with odds of breast cancer in the whole population. In addition, we found a significant association between dietary insoluble fiber and lower odds of breast cancer in the total and premenopausal women. However, this relationship was not significant for the soluble fiber intake. Based on our results, the intake fiber from fruits reduced the occurrence and fiber from cereals increased the risk of BC among premenopausal women. In postmenopausal women, fiber intake from vegetables and cereals had a protective association with odds of breast cancer. Further prospective studies are needed to examine the association between the sources of dietary fiber and fiber types with the risk of breast cancer based on menopausal status.
Data availability
The data of the present study will be available for the corresponding author(Kazem Zendehdel) .
References
De Cicco P, Catani MV, Gasperi V, Sibilano M, Quaglietta M, Savini I. Nutrition and Breast Cancer: A Literature Review on Prevention, Treatment and Recurrence. Nutrients. 2019;11(7).
De Vrieze T, Nevelsteen I, Thomis S, De Groef A, Tjalma WAA, Gebruers N, et al. What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Supportive care cancer: Official J Multinational Association Supportive Care Cancer. 2020;28(2):439–49.
Naja F, Nasreddine L, Awada S, El Sayed Ahmad R, Hwalla N. Nutrition in the Prevention of breast Cancer: a Middle Eastern Perspective. Front Public Health. 2019;7:316.
Kamińska M, Ciszewski T, Łopacka-Szatan K, Miotła P, Starosławska E. Breast cancer risk factors. Przeglad Menopauzalny = Menopause Rev. 2015;14(3):196–202.
Sun YS, Zhao Z, Yang ZN, Xu F, Lu HJ, Zhu ZY, et al. Risk factors and preventions of breast Cancer. Int J Biol Sci. 2017;13(11):1387–97.
Ban KA, Godellas CV. Epidemiology of breast cancer. Surg Oncol Clin N Am. 2014;23(3):409–22.
Rosato V, Bosetti C, Negri E, Talamini R, Dal Maso L, Malvezzi M, et al. Reproductive and hormonal factors, family history, and breast cancer according to the hormonal receptor status. Eur J cancer Prevention: Official J Eur Cancer Prev Organisation (ECP). 2014;23(5):412–7.
Kelsey JL, Gammon MD, John EM. Reproductive factors and breast cancer. Epidemiol Rev. 1993;15(1):36–47.
Picon-Ruiz M, Morata-Tarifa C, Valle-Goffin JJ, Friedman ER, Slingerland JM. Obesity and adverse breast cancer risk and outcome: mechanistic insights and strategies for intervention. Cancer J Clin. 2017;67(5):378–97.
Xiao Y, Xia J, Li L, Ke Y, Cheng J, Xie Y, et al. Associations between dietary patterns and the risk of breast cancer: a systematic review and meta-analysis of observational studies. Breast Cancer Res. 2019;21(1):NA–NA.
Kotepui M. Diet and risk of breast cancer. Contemp Oncology/Wspolczesna Onkologia. 2016;20(1).
Hou R, Wei J, Hu Y, Zhang X, Sun X, Chandrasekar EK, et al. Healthy dietary patterns and risk and survival of breast cancer: a meta-analysis of cohort studies. Cancer Causes Control. 2019;30(8):835–46.
Harris H, Bergkvist L, Wolk A. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations and breast cancer risk. Int J Cancer. 2016;138(11):2657–64.
Vidal García E, Sala Serra M, Continente Garcia X, Serral Cano G, Puigpinós i Riera R. The association between breast cancer and consumption of dairy products: a systematic review. Nutrición hospitalaria, 2020, vol 37, núm 3, p 589–598. 2020.
Okekunle AP, Gao J, Wu X, Feng R, Sun C. Higher dietary soy intake appears inversely related to breast cancer risk independent of estrogen receptor breast cancer phenotypes. Heliyon. 2020;6(7):e04228.
Sealy N, Hankinson SE, Houghton SC. Olive oil and risk of breast cancer: a systematic review and dose-response meta-analysis of observational studies. Br J Nutr. 2021;125(10):1148–56.
Mourouti N, Kontogianni MD, Papavagelis C, Panagiotakos DB. Diet and breast cancer: a systematic review. Int J Food Sci Nutr. 2015;66(1):1–42.
Kazemi A, Barati-Boldaji R, Soltani S, Mohammadipoor N, Esmaeilinezhad Z, Clark CCT, et al. Intake of various food groups and risk of breast Cancer: a systematic review and dose-response Meta-analysis of prospective studies. Advances in nutrition (Bethesda. Md). 2021;12(3):809–49.
Dhingra D, Michael M, Rajput H, Patil RT. Dietary fibre in foods: a review. J Food Sci Technol. 2012;49(3):255–66.
Jafari A, Ghanbari M, Shahinfar H, Bellissimo N, Azadbakht L. The association between dietary acid load with cardiometabolic risk factors and inflammatory markers amongst elderly men: a cross-sectional study. Int J Clin Pract. 2021;75(6):e14109.
Farvid MS, Spence ND, Holmes MD, Barnett JB. Fiber consumption and breast cancer incidence: a systematic review and meta-analysis of prospective studies. Cancer. 2020;126(13):3061–75.
Dong J-Y, He K, Wang P, Qin L-Q. Dietary fiber intake and risk of breast cancer: a meta-analysis of prospective cohort studies–. Am J Clin Nutr. 2011;94(3):900–5.
Cohen LA, Zhao Z, Zang EA, Wynn TT, Simi B, Rivenson A. Wheat Bran and Psylium diets: effects on N-Methylnitrosourea-Induced Mammary Tumorigenesis in F344 rats. JNCI: J Natl Cancer Inst. 1996;88(13):899–907.
Su X, Tamimi RM, Collins LC, Baer HJ, Cho E, Sampson L, et al. Intake of fiber and nuts during adolescence and incidence of proliferative benign breast disease. Cancer Causes Control: CCC. 2010;21(7):1033–46.
Sangaramoorthy M, Koo J, John EM. Intake of bean fiber, beans, and grains and reduced risk of hormone receptor-negative breast cancer: the San Francisco Bay Area breast Cancer Study. Cancer Med. 2018;7(5):2131–44.
Zhang CX, Ho SC, Cheng SZ, Chen YM, Fu JH, Lin FY. Effect of dietary fiber intake on breast cancer risk according to estrogen and progesterone receptor status. Eur J Clin Nutr. 2011;65(8):929–36.
Zhang D, Dai C, Zhou L, Li Y, Liu K, Deng YJ, et al. Meta-analysis of the association between nut consumption and the risks of cancer incidence and cancer-specific mortality. Aging. 2020;12(11):10772–94.
Falasca M, Casari I, Maffucci T. Cancer chemoprevention with nuts. J Natl Cancer Inst. 2014;106(9).
Vanden Heuvel JP, Belda BJ, Hannon DB, Kris-Etherton PM, Grieger JA, Zhang J, et al. Mechanistic examination of walnuts in prevention of breast cancer. Nutr Cancer. 2012;64(7):1078–86.
Heer E, Harper A, Escandor N, Sung H, McCormack V, Fidler-Benaoudia MM. Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Global Health. 2020;8(8):e1027–37.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran lipid and glucose study. Br J Nutr. 2012;108(6):1109–17.
Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran lipid and glucose study. J Epidemiol. 2010;20(2):150–8.
Englyst HN, Bingham S, Runswick S, Collinson E, Cummings J. Dietary fibre (non-starch polysaccharides) in cereal products. J Hum Nutr Dietetics. 1989;2(4):253–71.
Englyst H, Bingham S, Runswick S, Collinson E, Cummings J. Dietary fibre (non-starch polysaccharides) in fruit, vegetables and nuts. J Hum Nutr Dietetics. 1988;1(4):247–86.
Li BW, Andrews KW, Pehrsson PR. Individual sugars, soluble, and insoluble dietary fiber contents of 70 high consumption foods. J Food Compos Anal. 2002;15(6):715–23.
Kumar V, Sinha AK, Makkar HP, De Boeck G, Becker K. Dietary roles of non-starch polysachharides in human nutrition: a review. Crit Rev Food Sci Nutr. 2012;52(10):899–935.
Organization WH. Global physical activity questionnaire (GPAQ) analysis guide. Geneva: World Health Organization. 2012:1–22.
Rhee JJ, Cho E, Willett WC. Energy adjustment of nutrient intakes is preferable to adjustment using body weight and physical activity in epidemiological analyses. Public Health Nutr. 2014;17(5):1054–60.
De Stefani E, Correa P, Ronco A, Mendilaharsu M, Guidobono M, Deneo-Pellegrini H. Dietary fiber and risk of breast cancer: a case-control study in Uruguay. Nutr Cancer. 1997;28(1):14–9.
Lubin F, Wax Y, Modan B. Role of fat, animal protein, and dietary fiber in breast cancer etiology: a case-control study. J Natl Cancer Inst. 1986;77(3):605–12.
Breneman CB, Tucker L. Dietary fibre consumption and insulin resistance - the role of body fat and physical activity. Br J Nutr. 2013;110(2):375–83.
Gerber M. Fiber and breast cancer: another piece of the puzzle–but still an incomplete picture. J Natl Cancer Inst. 1996;88(13):857–8.
Adlercreutz H, Höckerstedt K, Bannwart C, Bloigu S, Hämäläinen E, Fotsis T, et al. Effect of dietary components, including lignans and phytoestrogens, on enterohepatic circulation and liver metabolism of estrogens and on sex hormone binding globulin (SHBG). J Steroid Biochem. 1987;27(4–6):1135–44.
Rose DP, Goldman M, Connolly JM, Strong LE. High-fiber diet reduces serum estrogen concentrations in premenopausal women. Am J Clin Nutr. 1991;54(3):520–5.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Holmes MD, Liu S, Hankinson SE, Colditz GA, Hunter DJ, Willett WC. Dietary carbohydrates, fiber, and breast cancer risk. Am J Epidemiol. 2004;159(8):732–9.
Deschasaux M, Zelek L, Pouchieu C, His M, Hercberg S, Galan P, et al. Prospective association between dietary fiber intake and breast cancer risk. PLoS ONE. 2013;8(11):e79718.
Cao S, Zhu Z, Zhou J, Li W, Dong Y, Qian Y, et al. Associations of one-carbon metabolism-related gene polymorphisms with breast cancer risk are modulated by diet, being higher when adherence to the Mediterranean dietary pattern is low. Breast Cancer Res Treat. 2021;187(3):793–804.
Hazra S, Ray AS, Rahaman CH. Natural phytocompounds from common Indian spices for identification of three potential inhibitors of breast Cancer: a Molecular Modelling Approach. Molecules. 2022;27(19):6590.
Shultz TD, Howie BJ. In vitro binding of steroid hormones by natural and purified fibers. Nutr Cancer. 1986;8(2):141–7.
McRorie JW Jr., McKeown NM. Understanding the physics of functional fibers in the gastrointestinal tract: an evidence-based Approach to resolving Enduring misconceptions about Insoluble and Soluble Fiber. J Acad Nutr Dietetics. 2017;117(2):251–64.
DeVries JW. On defining dietary fibre. Proc Nutr Soc. 2003;62(1):37–43.
Jenkins DJ, Axelsen M, Kendall CW, Augustin LS, Vuksan V, Smith U. Dietary fibre, lente carbohydrates and the insulin-resistant diseases. Br J Nutr. 2000;83(Suppl 1):S157–63.
Adlercreutz H, Martin F. Biliary excretion and intestinal metabolism of progesterone and estrogens in man. J Steroid Biochem. 1980;13(2):231–44.
Levy JI, Fabian MP, Peters JL. Meta-Analytic approaches for Multistressor dose-response function development: strengths, limitations, and Case studies. Risk Analysis: Official Publication Soc Risk Anal. 2015;35(6):1040–9.
Chen S, Chen Y, Ma S, Zheng R, Zhao P, Zhang L, et al. Dietary fibre intake and risk of breast cancer: a systematic review and meta-analysis of epidemiological studies. Oncotarget. 2016;7(49):80980–9.
Soriano-Hernandez AD, Madrigal-Perez DG, Galvan-Salazar HR, Arreola-Cruz A, Briseño-Gomez L, Guzmán-Esquivel J, et al. The protective effect of peanut, walnut, and almond consumption on the development of breast cancer. Gynecol Obstet Invest. 2015;80(2):89–92.
Reboredo-Rodríguez P, González-Barreiro C, Cancho-Grande B, Simal-Gándara J, Giampieri F, Forbes-Hernández TY, et al. Effect of pistachio kernel extracts in MCF-7 breast cancer cells: inhibition of cell proliferation, induction of ROS production, modulation of glycolysis and of mitochondrial respiration. J Funct Foods. 2018;45:155–64.
Carlsen MH, Halvorsen BL, Holte K, Bøhn SK, Dragland S, Sampson L, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr J. 2010;9:3.
Chen HS, Bai MH, Zhang T, Li GD, Liu M. Ellagic acid induces cell cycle arrest and apoptosis through TGF-β/Smad3 signaling pathway in human breast cancer MCF-7 cells. Int J Oncol. 2015;46(4):1730–8.
Cade JE, Burley VJ, Greenwood DC. Dietary fibre and risk of breast cancer in the UK women’s Cohort Study. Int J Epidemiol. 2007;36(2):431–8.
Mally A, Solfrizzo M, Degen GH. Biomonitoring of the mycotoxin zearalenone: current state-of-the art and application to human exposure assessment. Arch Toxicol. 2016;90(6):1281–92.
Kuiper-Goodman T, Scott PM, Watanabe H. Risk assessment of the mycotoxin zearalenone. Regul Toxicol Pharmacology: RTP. 1987;7(3):253–306.
Yip KY, Wan MLY, Wong AST, Korach KS, El-Nezami H. Combined low-dose zearalenone and aflatoxin B1 on cell growth and cell-cycle progression in breast cancer MCF-7 cells. Toxicol Lett. 2017;281:139–51.
Claeys L, Romano C, De Ruyck K, Wilson H, Fervers B, Korenjak M, et al. Mycotoxin exposure and human cancer risk: a systematic review of epidemiological studies. Compr Rev Food Sci Food Saf. 2020;19(4):1449–64.
Belhassen H, Jiménez-Díaz I, Arrebola JP, Ghali R, Ghorbel H, Olea N, et al. Zearalenone and its metabolites in urine and breast cancer risk: a case-control study in Tunisia. Chemosphere. 2015;128:1–6.
Yazdanpanah H, Zarghi A, Shafaati AR, Foroutan SM, Aboul-Fathi F, Khoddam A, et al. Exposure assessment of the tehran population (Iran) to zearalenone mycotoxin. Iran J Pharm Research: IJPR. 2012;11(1):251–6.
Hadiani MR, Yazdanpanah H, Ghazi-Khansari M, Cheraghali AM, Goodarzi M. Survey of the natural occurrence of zearalenone in maize from northern Iran by thin-layer chromatography densitometry. Food Addit Contam. 2003;20(4):380–5.
Zinedine A, Soriano JM, Moltó JC, Mañes J. Review on the toxicity, occurrence, metabolism, detoxification, regulations and intake of zearalenone: an oestrogenic mycotoxin. Food Chem Toxicology: Int J Published Br Industrial Biol Res Association. 2007;45(1):1–18.
Esmaillzadeh A, Azadbakht L. Major dietary patterns in relation to general obesity and central adiposity among Iranian women. J Nutr. 2008;138(2):358–63.
Lauren DR, Smith WA. Stability of the fusarium mycotoxins nivalenol, deoxynivalenol and zearalenone in ground maize under typical cooking environments. Food Addit Contam. 2001;18(11):1011–6.
Li N, Guo X, Sun C, Lowe S, Su W, Song Q, et al. Dietary carbohydrate intake is associated with a lower risk of breast cancer: a meta-analysis of cohort studies. Nutr Res. 2022;100:70–92.
Dunneram Y, Greenwood DC, Cade JE. Diet, menopause and the risk of ovarian, endometrial and breast cancer. Proc Nutr Soc. 2019;78(3):438–48.
Kachhap SK, Dange P, Nath Ghosh S. Effect of omega-6 polyunsaturated fatty acid (linoleic acid) on BRCA1 gene expression in MCF-7 cell line. Cancer Lett. 2000;154(2):115–20.
Simpson ER. Sources of estrogen and their importance. J Steroid Biochem Mol Biol. 2003;86(3–5):225–30.
Wu AH, Pike MC, Stram DO. Meta-analysis: dietary fat intake, serum estrogen levels, and the risk of breast cancer. J Natl Cancer Inst. 1999;91(6):529–34.
Acknowledgements
We would like to express our special thanks to the participants, without whom the study would not have been possible.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
FZ, MMN and BS participated in drafted the initial version. FT and BS designed the study and helped in the data analysis. FZ implemented comments and suggestions of the co-authors. KZ and ASA contributed in conception, design and data analysis. All authors reviewed the final version of the manuscript. KZ and AS supervised the study.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The methodology of the present study was approved by the ethics committee of Tehran University of Medical Sciences, Tehran, Iran and written informed consents for entering the study and publication of study results were taken from all participants.
Consent for publication
No individual detail is presented in this manuscript; therefore, it is not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zademohammadi, F., Sasanfar, B., Toorang, F. et al. Dietary soluble, insoluble, and total fiber intake and their dietary sources in association with breast cancer. BMC Public Health 24, 2560 (2024). https://doi.org/10.1186/s12889-024-19861-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19861-4