Abstract
Objective
The primary objective of this study was to determine the relationship between transcutaneous bilirubin (TcB) levels and total serum bilirubin (TSB) levels in extremely preterm infants.
Study design
We conducted a prospective multicenter study of extremely preterm infants less than 30 weeks gestation in California. Difference between paired TcB and TSB values were compared based on gestational age, birth weight, maternal race/ethnicity, chronological age as well as during and after phototherapy.
Results
TSB values ranged from 0 to 12.6 mg/dl and the TcB values ranged from 0 to 14.2 mg/dl. TSB was predicted with a high degree of accuracy at TSB = 2.37 + 0.54 (TcB) with r = 0.786. There was good correlation across gestational age, birth weight, race/ethnic, chronological age subgroups as well as during and after phototherapy.
Conclusion
Our study supports the use of TcB as a screening tool for monitoring jaundice in extremely preterm infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Unconjugated hyperbilirubinemia is one the most commonly encountered conditions in the newborn period. About 60 percent of term and 80 percent of preterm infants will present with clinical jaundice with a serum level above 5 mg/dl [1]. In most cases, it does not pose any significant risks to newborns. However, in about 10% of term and 25% of preterm infants, serum bilirubin levels can reach dangerously high levels that require treatment [2].
Diagnosis and management of hyperbilirubinemia requires measurement of serum bilirubin levels, which is the current gold standard at most hospitals in the world. Blood sampling for measuring serum bilirubin level involves painful procedures which can have long-term negative consequences in the vulnerable extremely preterm newborn. Iatrogenic blood loss secondary to laboratory tests is a common cause of anemia of prematurity and need for blood transfusions [3].
Transcutaneous bilirubin (TcB) devices estimate serum bilirubin noninvasively. These devices work by directing light into the skin of the neonate and measuring the intensity of specific wavelengths returned. The number of wavelengths varies depending on the TcB device. These devices have been shown to correlate well with serum bilirubin levels in term and near-term infants [4,5,6]. The American Academy of Pediatrics recommends the use of TcB devices for the evaluation of jaundice in infants ≥35 weeks’ gestation [7].
Hyperbilirubinemia in preterm infants can be severe and protracted compared to term babies due to delayed maturation of hepatic conjugation and uptake mechanisms. There is an increase in enterohepatic recirculation of bilirubin due to delays in initiation and advancement of enteral feeds which limits intestinal motility and bacterial colonization [1,2,3,4,5,6,7].
Although the current TcB guidelines are widely used in the newborn nursery setting, there are no specific guidelines for TcB use in the extremely preterm population cared for in the neonatal intensive care unit (NICU). There is paucity of data on the accuracy of TcB measurements in preterm infants undergoing phototherapy. The primary purpose of screening newborns with TcB measurements as suggested by Maisels et al. is to help the clinician to decide when to obtain a total serum bilirubin (TSB) measurement that, in turn, might suggest the need for phototherapy [7,8,9,10].
The primary objective of this study was to 1) measure TcB levels in very preterm newborns; 2) compare TcB levels to TSB levels drawn at similar timepoints and 3) monitor TcB levels with or without phototherapy in this population.
Methods
This prospective multicenter study was conducted at eight Level III and IV NICUs in California between November 2018 to August 2020. Infants with congenital malformations, chromosomal abnormalities or direct hyperbilirubinemia were excluded. Maternal and neonatal characteristics included were gestational age, birth weight, race/ethnicity, morbidities, mortality, Glucose 6 phosphate dehydrogenase (G6PD) enzyme testing, the need for exchange transfusion, TcB and TSB values during the first 2–3 weeks of life (including whether they were on phototherapy at the time). Infants were stratified into three gestational age (GA) subgroups (<25 weeks, 25.0–27.6 weeks and 28.0–30.0 weeks), and four birth weight subgroups (≤750 g, 751–1000 g, 1000–1250 g, and >1250 g) respectively to study the correlation between TcB and TSB levels.
TSB measurements were performed in the hospital clinical laboratory with the Synchron Diazo method (Beckman Coulter, Fullerton, CA, USA). TcB measurements were obtained using the Konica Minolta Dräger Air-Shields JM-105 jaundice meter (Draeger Medical, Telford, PA, USA). One center utilized the BiliChek (Philips BiliChek) transcutaneous jaundice meter. Nursing staff in the NICU were trained to use the transcutaneous bilimeter prior to study initiation and appropriate quality control measures were followed on a regular basis. TcB measurements were obtained within 30–60 min of a TSB measurement during routine clinical care. Three independent measurements were obtained, and the maximum of the three values recorded was used as the TcB measurement in this study. Neonates with TSB readings in the phototherapy range received phototherapy as per the individual standard unit guidelines. Patients were treated with continuous phototherapy by LED phototherapy unit in all centers. The NeoBLUE LED phototherapy system provides an initial intensity of 35 mW/cm2/nm at the high setting and 15 mW/cm2/nm at the low setting. The Bili Eclipse TM, (Philips Respironics, Murrysville, PA, USA) a commercial photo-opaque patch was utilized to shield the area of skin on the sternum or forehead when phototherapy was instituted. TSB and TcB measurements were repeated 24 h after phototherapy was terminated to assess for rebound levels. Subsequent measurements were performed as per clinician’s discretion on the study infants until 2–3 weeks of age. The study was approved by each hospitals’ Human Investigation Review Committee and because of the noninvasive nature of the measurement, the committees approved a waiver of consent.
Statistical analysis
Descriptive statistics were performed for the entire population. We estimated means and standard deviation of the differences between TcB and TSB measurements. Coefficient of variation was calculated for TcB measurements. The correlation between the highest measured TcB level and TSB was assessed with Pearson’s Correlation analysis. Bland-Altman analysis was used to show the differences against the mean of the two methods. Differences between TcB and TSB values were compared based on gestational age, birth weight, infant’s chronological age and maternal race and ethnicity. Factors affecting the TcB and TSB correlation were compared using independent sample t-test and ANOVA. Multivariate linear regression analysis was performed for significant factors. The IBM SPSS statistical software version 27 was used for the data analysis.
Results
One hundred and forty-one extremely preterm infants between 224/7 and 300/7 weeks of gestation were included. There were 755 paired TcB and TSB measurements obtained from these infants from day of life 0 through day of life 18. Baseline characteristics of the study population are shown in Table 1. The mean coefficient of variation among the three values recorded with each TcB measurement was 10.9% for TcB values >5. To minimize variability related to dispersion we used the highest measured TcB levels for all comparisons. One center (24 infants, 174 measurements) used the BiliChek bilimeter whereas the other 7 centers (117 infants, 581 measurements) used the Drager bilimeter to measure TcB levels. The mean TcB using BiliChek bilimeter read 2.85 mg/dl higher than TSB (p < 0.001) suggesting poor correlation. Pearson correlation coefficient comparing TcB and TSB levels in BiliChek group was 0.506.
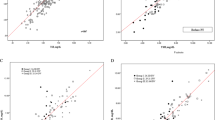
Further analysis was done for infants in which the Drager bilimeter was used to measure TcB levels. There was a strong direct linear correlation (r = 0.786, p < 0.001) between TSB and TcB values as shown in Fig. 1. TSB values ranged from 0 to 12.6 mg/dl and the TcB values ranged from 0 to 14.2 mg/dl. TSB was predicted with a high degree of accuracy at TSB = 2.37 + 0.54 (TcB) levels (r2 = 0.617). Bland Altman plot revealed agreement between TSB and TcB values as shown in Fig. 2. Bias line showed TSB was 0.33 mg/dl higher than TcB with the majority of points falling in ±1.96 SD of the difference between TSB and TcB.
Subgroup analysis showed the strong correlation was consistent across all three gestational age subgroups (r = 0.757, r = 0.795, r = 0.773) as shown in Fig. 3. All four birth weight groups also showed good correlation between TSB and TcB levels (r = 0.726, r = 0.740, r = 0.894, r = 0.610) (data not shown). All race/ethnic groups including Asian infants (r = 0.808) showed strong correlation. Correlation was stronger in infants more than 1 week of age (r = 0.828) compared to younger infants (r = 0.749) (data not shown).
A total of 274 TcB measurements were taken while the infants were receiving phototherapy. Correlation was similar whether infants were receiving phototherapy (r = 0.785) or not (r = 0.779) as shown in Fig. 4. Independent sample t-test comparing mean difference for infants not receiving phototherapy showed TcB to be 0.07 mg/dl lower than TSB compared to infants receiving phototherapy where TcB read 0.62 mg/dl lower than TSB levels. We found disparities in only 2.5% paired TcB and TSB measurements in which TSB read higher than 2 mg/dl from TcB levels and infants needed phototherapy based on TSB levels but not with TcB levels. None of the infants had testing done for G6PD deficiency. None of the study infants had severe hyperbilirubinemia requiring an exchange transfusion.
Discussion
We found that TcB levels correlated strongly with TSB values (r = 0.786) in this multicenter study of extremely preterm infants less than 30 weeks gestation in California NICU’s. TcB levels were noted to be affected by the type of bilirubinometer, gestational age, birth weight, chronological age, and phototherapy. We found a strong correlation across all gestation age subgroups (r = 0.757, r = 0.795 and r = 0.773 in <25 weeks, 25–27 weeks, 28–30 weeks respectively) and birth weight subgroups and before (r = 0.834), during (r = 0.796) and after (r = 0.772) phototherapy. Even though our population was racially diverse, we did not see any significant difference based on race/ethnicity in this cohort of extremely preterm infants.
To study the use of TcB and practices surrounding jaundice, Bhatt and colleagues conducted a survey of 150 California NICU’s in 2017 [11]. They found that TcB screening is only used in 28% of NICU’s. Only 7% (11/150) of NICU’s used TcB measurements in preterm infants. They noted practice variations across various NICU levels of care in regard to bilirubin screening practices and utilization of phototherapy. They were unable to make any recommendations for TcB screening for infants <28 weeks or for infants 28-34 weeks gestation due to limited studies [11]. This prospective multicenter study was pursued by the California Association of Neonatologists research group investigators as a follow-up to that survey to assess the utility of TcB measurements in the extremely preterm population.
There has been a reasonable interest in the use of TcB in preterm infants for screening purposes due to its non-invasive nature and cost reduction benefits. A systematic review by Nagar et al., showed that the TcB devices reliably estimated bilirubin levels in preterm infants and could be used in clinical practice to reduce blood sampling. They found that the JM-103 Drager device showed better precision than the BiliChek device [4]. In our study, we found similar results with the Drager bilimeter showing better correlation results than the Bilichek bilimeter used by only one center. Subsequent meta-analysis by the same group showed the TcB devices are much less accurate in estimating TSB levels in infants when receiving phototherapy as compared to their documented accuracy in the pre-phototherapy period in late preterm and term infants. This review did not provide specific details as to the accuracy or the use of TcB in the preterm population [2]. Maisels et al., conducted a prospective study in preterm infants less than 35 weeks gestation to define a TcB measurement that will prompt the clinician to obtain a blood sample for TSB to assess the need for phototherapy. This study provided practical guidelines to support routine use of TcB screening for infants of <35 weeks but did not have enough data for extremely preterm infants less than 28 weeks gestation [8]. Another prospective study by Chawla et al., also showed good correlation between Tcb and TSB in preterm low birth weight neonates, but they excluded infants <28 weeks of gestation [12, 13]. In our study, we found good correlation and agreement between TcB and TSB in all gestational age and birth weight subgroups of extremely preterm infants less than 30 weeks gestation.
There are only a few studies that evaluated the use of TcB in infants receiving phototherapy and have shown conflicting results. The alteration of bilirubin molecule in the skin or the rich vascular supply of the skin could interfere with the measurement of TcB while the infant is receiving phototherapy [14,15,16,17]. This has prompted investigators to use a skin patch to shield part of the area from phototherapy [18,19,20,21]. One study showed poor correlation between TcB and TSB during and after phototherapy, but the BiliChek bilimeter was used for this measurement [18]. We found similar poor correlation results with the Bilicheck meter used by one of our study centers compared to the Drager Bilimeter. Another study included term and late preterm infants and found that by using the skin patch, there was good correlation between TSB and TcB and the maximum difference of 0.27 mg/dl was noted at 48 h using Drager Bilimeter. The authors, however, acknowledged the lack of data on extremely preterm infants and the patient population was predominantly Caucasian neonates [19]. In our study, the use of skin patch on all study infants while undergoing phototherapy might have contributed to the good correlation. In a recent study by Pendse et al., there was a good correlation with TSB after initiation of phototherapy. (r = 0.918, P < 0.001). Interestingly, TcB at 28–32 weeks of gestation (r = 0.97) was better correlated with TSB than those at 32–37 weeks (r = 0.88). The correlation was better for neonates <72 h old (r = 0.96) than those >72 h of age (r = 0.82). They acknowledged that small numbers of eligible preterm infants as a study limitation [15]. In our study, we found good correlation in infants receiving phototherapy and those not receiving phototherapy. In contrast to few other studies, we found the correlation was better for infants more than a week old compared to younger infants [22]. The reason for this discrepancy is unclear. We speculate that this could be due to the effects of phototherapy, skin maturity, skin pigmentation and racial/ethnic factors related to our study population.
Various studies have looked at the different sites for TcB measurements. One study found the interscapular site showed the best correlation in preterm infants and another study found better correlation with forehead site while undergoing phototherapy [23,24,25]. In our study, sternum and forehead sites were utilized and found to have consistent correlation, although we did not compare the various sites of measurement.
While none of our study infants required an exchange transfusion, only 0.25% of extremely low birth weight infants were reported to have received an exchange transfusion in the Neonatal Research Network study [26]. Even though that study was published over a decade ago, it is reassuring to note that none of the preterm infants studied in the current period had markedly elevated serum bilirubin levels that required exchange transfusion. This is likely due to early use of new, more effective LED lights to provide phototherapy and improved detection of mothers with antibody sensitization (i.e., Rh disease).
Previous studies have found variations in TcB nomograms in term infants across various population groups that reflect differences in bilirubin metabolism [27]. In our study, we did not find any differences in the TcB readings in our ethnically diverse population of extremely preterm infants. It is possible that factors influencing bilirubin levels may be different in extremely preterm versus term infants. Although we attempted to collect data on G6PD testing, it was interesting to note that study centers did not order testing on the babies and so the data was not available. The lack of G6PD testing in the study centers highlights the difference in physician care practices surrounding jaundice evaluation and testing in extremely preterm infants compared to term and late preterm infants.
Few studies evaluating the quantitative reduction in blood sampling using TcB measurements showed that the use of TcB in jaundiced term and preterm babies >32 weeks gestation resulted in a 38.5% reduction in blood draws compared to a TSB test [28, 29]. There are no such studies to date in extremely preterm infants. As neonatal stress in the NICU is related to unfavorable neurodevelopmental outcomes, focusing on alleviating pain and noxious stimuli from blood draws and minimal handling could make a difference in the infant’s overall outcomes. Future studies should target to study the cost-effectiveness of this non-invasive approach to bilirubin measurements in the NICU setting and improvement in neurodevelopmental outcomes from the reduction in painful procedures.
Strengths of this study include a large population of extremely preterm infants less than 30 weeks gestation. The centers include a few regional and several community-level NICUs in California and provide a diverse preterm population of infants. Ours is also one of the very few studies to evaluate the use of TcB in infants undergoing phototherapy. We also collected data on infants until 2–3 weeks of age and evaluated information about the effects of chronological age on TcB measurements compared to other studies evaluating infants mostly in the first few days of life. We used robust data analysis using both correlation testing and Bland-Altman methods.
Limitations of our study include the use of two different Bilimeters with one study center using BiliChek that showed a significant discrepancy in paired TcB and TSB measurements. We obviated this issue by performing a subgroup analysis of the TcB values obtained only from the Drager JM bilimeter. We emphasize the issue of inter-meter variation as an important factor that needs to be considered when performing TcB measurements in the NICU. Although our paired TcB and TSB measurements from all seven centers showed strong correlation overall, we are unable to comment on the accuracy of the individual Drager bilimeter devices used by each center. Since the TSB and TcB measurements were obtained within a 30–60 min time period with most samples obtained within the 30 min period, we do not expect the rate of TSB rise impact the correlation between the two measurements. We did not collect detailed data on maternal factors and infant’s respiratory and hemodynamic factors that could influence the TcB values and are unable to provide information on the effect of these factors.
In conclusion, our study showed that TcB is a useful screening tool for monitoring jaundice in extremely preterm infants. Our study showed good correlation across various gestational age, birth weight and racial subgroups as well as with and without phototherapy and advanced chronological age. Future large, randomized clinical trials are needed to study the application of this technology to reduce blood draws and number of painful procedures as well as decrease costs in the NICU setting. Additional studies will be needed to develop TcB nomograms to project the rise in bilirubin trajectory and need for intervention similar to those published for late preterm and term Infants.
Data availability
Complete de-identified study data that underlie the results reported in the manuscript will be available upon request. Data requests should be directed to the corresponding author.
References
Mitra S, Rennie J. Neonatal Jaundice: Aetiology, diagnosis and treatment. Br J Hosp Med. 2017;78:699–704.
Nagar G, Vandermeer B, Campbell S, Kumar M. Effect of Phototherapy on the Reliability of Transcutaneous Bilirubin Devices in Term and Near-Term Infants: A Systematic Review and Meta-Analysis. Neonatology 2016;109:203–12.
Counsilman CE, Heeger LE, Tan R, Bekker V, Zwaginga JJ, Te Pas AB, et al. Iatrogenic blood loss in extreme preterm infants due to frequent laboratory tests and procedures. J Matern Fetal Neonatal Med. 2021;34:2660–65.
Nagar G, Vandermeer B, Campbell S, Kumar M. Reliability of transcutaneous bilirubin devices in preterm infants: a systematic review. Pediatrics 2013;132:871–81.
Schmidt ET, Wheeler CA, Jackson GL, Engle WD. Evaluation of transcutaneous bilirubinometry in preterm neonates. J Perinatol. 2009;29:564–9.
Engle WD, Jackson GL, Engle NG. Transcutaneous bilirubinometry. Semin Perinatol. 2014;38:438–51.
Maisels MJ, Kring E. Transcutaneous bilirubin levels in the first 96 h in a normal newborn population of > or =35 weeks’ gestation. Pediatrics. 2006;117:1169–73.
Maisels MJ, Coffey MP, Kring E. Transcutaneous bilirubin levels in newborns <35 weeks’ gestation. J Perinatol. 2015;35:739–44.
Maisels MJ. Transcutaneous bilirubin measurement: does it work in the real world? Pediatrics 2015;135:364–6.
Maisels MJ, Watchko JF, Bhutani VK, Stevenson DK. An approach to the management of hyperbilirubinemia in the preterm infant less than 35 weeks of gestation. J Perinatol. 2012;32:660–4.
Bhatt DR, Kristensen-Cabrera AI, Lee HC, Weerasinghe S, Stevenson DK, Bhutani VK, et al. Transcutaneous bilirubinometer use and practices surrounding jaundice in 150 California newborn intensive care units. J Perinatol. 2018;38:1532–5.
Chawla D, Jain S, Kaur G, Sinhmar V, Guglani V. Accuracy of transcutaneous bilirubin measurement in preterm low-birth-weight neonates. Eur J Pediatr. 2014;173:173–9.
Chawla D. Transcutaneous Bilirubin for Screening of Significant Jaundice in Very Preterm Neonates. Indian J Pediatr. 2019;86:4.
Raba AA, O’Sullivan A, Miletin J. Transcutaneous bilirubinometry during and after phototherapy in preterm infants: a prospective observational study. BMJ Paediatr Open. 2020;16:4.
Pendse A, Jasani B, Nanavati R, Kabra N. Comparison of Transcutaneous Bilirubin Measurement with Total Serum Bilirubin Levels in Preterm Neonates Receiving Phototherapy. Indian Pediatr. 2017;54:641–3.
Cucuy M, Juster-Reicher A, Flidel O, Shinwell E. Correlation between transcutaneous and serum bilirubin in preterm infants before, during, and after phototherapy. J Matern Fetal Neonatal Med. 2018;10:1323–6.
Bhargava V, Tawfik D, Niebuhr B, Jain SK. Transcutaneous bilirubin estimation in extremely low birth weight infants receiving phototherapy: A prospective observational study. BMC Pediatr. 2018;18:22.
Murli L, Thukral A, Sankar MJ, Vishnubhatla S, Deorari AK, Paul VK, et al. Reliability of transcutaneous bilirubinometry from shielded skin in neonates receiving phototherapy: A prospective cohort study. J Perinatol. 2017;37:182–7.
Costa-Posada U, Concheiro-Guisán A, Táboas-Ledo MF, González-Colmenero E, González-Durán ML, Suarez-Albo M, et al. Accuracy of transcutaneous bilirubin on covered skin in preterm and term newborns receiving phototherapy using a JM-105 bilirubinometer. J Perinatol. 2020;40:226–31.
De Luca D, Dell’Orto V. Patched skin bilirubin assay to monitor neonates born extremely preterm undergoing phototherapy. J Pediatr. 2017;188:122–7.
Fonseca R, Kyralessa R, Malloy M, Richardson J, Jain SK. Covered skin transcutaneous bilirubin estimation is comparable with serum bilirubin during and after phototherapy. J Perinatol. 2012;32:129–31.
Rubio A, Epiard C, Gebus M, Deiber M, Samperiz S, Genty C, et al. Diagnosis Accuracy of Transcutaneous Bilirubinometry in Very Preterm Newborns. Neonatology. 2017;111:1–7.
Arman D, Topcuoğlu S, Gürsoy T, Ovalı F, Karatekin G. The accuracy of transcutaneous bilirubinometry in preterm infants. J Perinatol. 2020;40:212–8.
Yaser A, Tooke L, Rhoda N. Interscapular site for transcutaneous bilirubin measurement in preterm infants: a better and safer screening site. J Perinatol. 2014;34:209–12.
Jeon J, Lim G, Oh KW, Lee NM, Park HW, Chung ML. The forehead is a better site than the sternum to check transcutaneous bilirubin during phototherapy in sick infants. BMC Pediatr. 2020;20:548.
Morris BH, Oh W, Tyson JE, Stevenson DK, Phelps DL, O’Shea TM, et al. NICHD Neonatal Research Network. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N. Engl J Med. 2008;359:1885–96.
Kaplan M, Bromiker R. Variation in transcutaneous bilirubin nomograms across population groups. J Pediatr. 2019;208:273–8.
Konana OS, Bahr TM, Strike HR, Coleman J, Snow GL, Christensen RD. Decision accuracy and safety of transcutaneous bilirubin screening at intermountain healthcare. J Pediatr. 2021;228:53–57.
Van den Esker-Jonker B, den Boer L, Pepping RM, Bekhof J. Transcutaneous bilirubinometry in jaundiced neonates: A randomized controlled Trial. Pediatrics. 2016;138:e2016–2414.
Acknowledgements
The authors thank Dr. Jeffrey Maisels for his expert input and guidance. The authors thank Joanne Kuller, Clinical nurse specialist, UCSF Benioff Children’s Oakland & Marcie Portillo, Neonatal Research Institute, Sharp Mary Birch Women & Children’s Hospital for their assistance with the data collection process at their respective centers. We also would like to thank Dr. Robert Kahle, Past President, California Association of Neonatologists (CAN) and CAN Research Committee members for their support with this study.
Funding
The authors received no funding to conduct this study.
Author information
Authors and Affiliations
Contributions
MNS, RR and DRB conceptualized and designed the study. MNS designed the study protocol, data collection documents and coordinated the study. AK, PJ, MFV, MC, VP, HT, RCT, VA and MN collected study data. MB analyzed study data and created tables and figures for the study. MNS wrote the initial version of the manuscript and MB, RR, AK, PJ, VA, RCT, HT, VP, MV, DRB, MC & MN critically reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sankar, M.N., Ramanathan, R., Joe, P. et al. Transcutaneous bilirubin levels in extremely preterm infants less than 30 weeks gestation. J Perinatol 43, 220–225 (2023). https://doi.org/10.1038/s41372-022-01477-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01477-4
- Springer Nature America, Inc.