Abstract
Purpose
The aim of this study was to evaluate the efficacy of using Er,Cr:YSGG laser in an adjunct to scaling and root planing (SRP + Er,Cr:YSGG) in periodontal maintenance patients with residual periodontal pockets.
Materials and methods
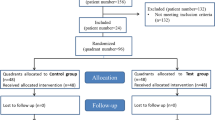
This study is a double-blind randomized controlled clinical trial and a split-mouth design. Fifteen periodontal maintenance patients with two single-rooted teeth with probing depth (PD) ≥ 5 mm in two different quadrants were randomly assigned to scaling and root planing (SRP) as a control group or SRP + Er,Cr:YSGG as test group. Plaque index (PI), bleeding on probing (BOP), PD, relative probing attachment level (RPAL), and relative gingival recession (RGR) were evaluated at baseline, 3 months and 6 months after treatment by one calibrated examiner.
Results
At 6 months after treatment, PDs were statistically significantly reduced in both SRP (0.9 ± 0.6 mm) and SRP + Er,Cr:YSGG (1.1 ± 0.7 mm) compared with pretreatment PD (p < 0.05). Only SRP + Er,Cr:YSGG demonstrated statistically significant probing attachment level (PAL) gained at 6 months after treatment (0.8 ± 0.6 mm; p < 0.05). Gingival recession (GR) statistically significantly increased in SRP + Er,Cr:YSGG 3 months after the treatment (0.5 ± 0.5 mm; p < 0.05). Nevertheless, there were no statistically significant differences between the 2 treatment modalities regarding PD reduction, PAL gain, or GR at 6 months after treatment.
Conclusions
Only SRP + Er,Cr:YSGG demonstrated statistically significant PAL gained at 6 months after treatment (0.8 ± 0.6 mm; p < 0.05); however, there were no statistically significant differences between the 2 treatment modalities regarding PD reduction, PAL gain, or GR at 6 months after treatment in maintenance patients with residual periodontal pockets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Periodontitis causes the loss of periodontium resulted in pocket formation and attachment loss. After active periodontal therapy, regularly attended and performed maintenance care shows successful long-term results [1, 2]. The goals of periodontal maintenance following the completion of active periodontal therapy are (1) to prevent the recurrence and progression of periodontal disease; (2) to reduce the incidence of tooth loss; and (3) to increase the probability of detecting and treating, in a timely manner, other diseases or conditions found within the oral cavity [3]. Previously treated areas might show periodontal breakdown. Residual deep pockets during the periodontal maintenance have a risk of progression of periodontitis and tooth loss [4]. Various treatment protocols for recurrent periodontitis during periodontal maintenance are suggested such as adjunctive of local and systemic antibiotics [5, 6]. Laser has been proposed to use in nonsurgical therapy due to its favorable hemostatic, bactericidal, sulcular debridement, scaling the root surfaces, and biostimulation effect [7]. Nevertheless, some laser systems are not suitable for periodontal therapy [8, 9]. Recently, the erbium-chromium-yttrium-scandium-gallium-garnet (Er,Cr:YSGG) laser with 2780-nm wavelength is introduced for periodontal therapy due to its ability of hard and soft tissue ablation as well as no thermal side effect [7, 10, 11]. Er,Cr:YSGG laser application demonstrated greater bone formation than scaling and root planning with curettes in the treatment of experimental periodontitis [12]. Clinical results of Er,Cr:YSGG laser application in addition to scaling and root planning (SRP) in the patients with periodontitis showed statistically significant more probing depth (PD) reduction and clinical attachment level (CAL) gain than SRP at 1-year [13] and 2-year [14] evaluations. In contrast, Magaz et al. reported no improvement regarding PD reduction or CAL gain with Er,Cr:YSGG in conjunction with SRP [15].
The aim of the present double-blinded, split-mouth randomized controlled clinical trial was to evaluate the efficacy of Er,Cr:YSGG laser in adjunct to SRP in periodontal maintenance patients with residual periodontal pockets.
Materials and methods
Seventeen periodontal maintenance patients at the Faculty of Dentistry, Mahidol University, Thailand, were recruited to the study. Inclusion criteria were the following:
-
Age ≥ 18 years
-
Periodontal maintenance patients with no surgical periodontal therapy during the last 12 months
-
At least two single-rooted teeth with probing depth (PD) ≥ 5 mm in two different quadrants
Exclusion criteria were the following:
-
Systemic diseases that effect on the progression and compromise healing of periodontal diseases
-
Use of medications that induce gingival enlargement or bisphosphonate
-
Pregnancy
-
Systemic antibiotics or anti-inflammatory drugs taken within previous 3 months and 6 months after the treatment
-
Smokers
-
Hopeless teeth
The study protocol was approved by the Faculty of Dentistry/Faculty of Pharmacy, Mahidol University Institutional Review Board (COA.No.MU-DT/PY-IRB 2016/013.1502). Patients who met the above criteria were informed about the study and had to sign the informed consent. Informed consent was obtained from all individual participants included in the study.
Oral hygiene instructions were given to the patients until plaque score < 40% before starting the treatment.
Clinical measurements and data collection
Clinical parameters were recorded at baseline, 3 months, and 6 months after treatment by one calibrated examiner who had intra-examiner calibration performed and showed 94.7% reproducibility as well as was different from the clinician performing the treatment. The customized stent was fabricated with acrylic resins. A groove was made into the stent to ensure the same position of the periodontal probe. Plaque index (PI) [16] was recorded using the following scale: 0 = no plaque; 1 = plaque detected only by probing on the tooth surface; 2 = plaque can be seen with the naked eyes, moderate accumulation of plaque; 3 = abundant plaque. Gingival bleeding index (GBI) recorded a positive finding of bleeding on probing (BOP) [17]. Periodontal probe (PCPUNC15; Hu-Friedy, Chicago, IL, USA) was used with a stent at the deepest PD in each tooth to measure PD from the gingival margin to the base of the pocket, and relative gingival recession (RGR) from the lower border of the stent to gingival margin. Relative probing attachment level (RPAL) was calculated from PD+RGR.
Treatment
The teeth were randomly assigned to scaling and root planing (SRP) as a control group or SRP + Er,Cr:YSGG (test) prior to the treatment by a computer software program that generates the random sequence. The patients and the examiner were blinded from the type of treatment. All of the treatment was performed by another operator. Local anesthesia was given with 2% mepivacaine with epinephrine 1:100,000, both the test and control groups.
In the test group, the Er,Cr:YSGG laser device (Waterlase, Biolase, USA) and Radial Firing Perio Tip (RFPT5) were used. The treatment sequences were performed: (1) removal of outer pocket gingival epithelium from the free gingival margin to a depth equal to the pocket depth by Er,Cr:YSGG (Fig. 1), (2) removal of inner epithelial lining to the depth of the pocket by Er,Cr:YSGG, (3) scaling and root planing with ultrasonic scaler (P5 Newtron®XS, Acteon, Switzerland) and Gracey curettes (Hu-Friedy, Chicago, IL, USA) to remove calculus and to smoothen cementum, (4) removal of smear layer, residual calculus, degranulation, and induce blood coagulation by Er,Cr:YSGG (Fig. 2), (5) compress the gingival tissue against the root surface with wet gauze 3–5 min. For the control group, the same treatment steps were performed without activating the laser device. Maintenance periodontal therapy was given in the remaining teeth.
Professional supra-gingival tooth cleaning was performed by the examiner at 3 months and 6 months after treatment.
Statistical analysis
Statistical analysis was achieved by statistical software SPSS for Windows Version 21. The normality of the data was analyzed according to the Shapiro–Wilk test. The mean values and standard deviations of PD, RPAL, and RGR were calculated. PD, RPAL, and RGR were compared between each group and changed during the follow-up using Friedman test. McNemar’s test was used to PI and GBI between each group and changed over time. All statistical tests were considered significant at p < 0.05. The final change of PD, RPAL, and RGR were compared between the 2 groups with Wilcoxon matched-pairs signed-ranks test.
Results
Patient characteristic at baseline
Of the 17 patients enrolled, 15 patients completed the study. Two patients were lost during the follow-up period. Ten patients were women (66.7%), and five were men (33.3%). The mean age was 57.7 ± 9.8 years. No adverse event was noted during the study.
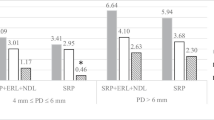
At baseline, no differences could be found between SRP and SRP + Er,Cr:YSGG groups regarding PI, GBI, PD, RPAL, or RGR (Figs. 3 and 4; Table 1).
Three months after treatment
PI and GBI were not statistically significantly different from baseline in both groups as well as between groups even though the number of sites with BOP decreased in both groups (Figs. 3 and 4).
Although a significant mean PD reduction could be observed only in the SRP + Er,Cr:YSGG group between baseline (5.5 ± 0.6 mm) and 3 months after treatment (4.6 ± 0.9 mm) (p < 0.05), no statistically significant difference was observed between both groups (Table 1).
At 3 months after treatment, the mean RPAL in the SRP + Er,Cr:YSGG group showed a gain of 0.4 ± 0.6 mm, while the SRP group showed a loss of 0.1 ± 0.7 mm. However, no statistically significant difference was shown neither at 3 months follow-up compared to baseline in both groups nor between the 2 treatment modalities (Table 1).
RGR showed no statistically significant difference compare to baseline in the SRP group. But SRP + Er,Cr:YSGG group showed statistically significant increased RGR (0.5 ± 0.5 mm) after treatment. The RGR changes showed no statistically significant difference between the 2 groups (Table 1).
Six months after treatment
PI was not statistically significantly different from baseline in both groups. GBI showed a continuous decrease in both groups, but it was not statistically significantly different either from 3 or 6 months after treatment (Figs. 3 and 4).
Table 1 shows the clinical parameters: PD, RPAL, and RGR. PD showed a continuous decrease in both groups. Both SRP and SRP + Er,Cr:YSGG groups showed statistically significant difference in PD reduction from baseline (p < 0.05); however, when a comparison of PD reduction between groups was made, no statistically significant difference was observed (Table 2).
When compared with the baseline, only PAL gain (0.8 ± 0.6 mm) in the SRP + Er,Cr:YSGG group showed statistically significant difference (p < 0.05). Nevertheless, there was no statistically significant difference observed between the 2 groups in PAL change (Table 2).
RGR showed no statistically significant difference either compared to baseline (Table 1) or between the 2 treatment modalities (Table 2).
Discussion
The present study aimed to evaluate the efficacy of adjunct Er,Cr:YSGG laser compared with SRP in periodontal maintenance patients with residual periodontal pockets. All 15 patients showed an acceptable oral hygiene throughout the study. The periodontal wound healing depends on the cell types repopulating the wound area. If the epithelial cells migrate to the wound area, a long junctional epithelium will result [18]. Periodontal ligament cells repopulating the wound area form new attachment. Therefore, to achieve new attachment, the pocket epithelium and outer epithelium need to be removed in order to retard epithelial migration [19]. Er,Cr:YSGG laser showed better biocompatible condition in periodontal-diseased root surfaces than curettes regarding the attachment of periodontal ligament fibroblasts [20]. And there was a tendency of greater periodontal ligament attachment with Er,Cr:YSGG laser than ultrasonic scaler [21]. Thus, the advantage of Er,Cr:YSGG application compared with conventional scaling and root planing is to retard epithelial migration and facilitate periodontal ligament attachment. In addition, previous studies demonstrated that smear layer after root instrumentation inhibited new attachment [22, 23] which formed after smear layer was removed [22, 24]. Ito et al. [25] showed that Nd:YAG demonstrated the ability to remove smear layer after root planing. In addition, laser has an advantage in bactericidal effect. Akiyama et al. [26] demonstrated that Er:YAG was able to kill periodontopathic bacteria on root surfaces better than ultrasonic scaler. Even though there is no histologic wound healing report with Er,Cr:YSGG application, Pavone et al. [13] demonstrated greater bone formation than SRP in the treatment of experimental periodontitis.
The results of the present study demonstrated that both treatment modalities were effective in PD reduction in the maintenance patients at 6 months. PAL significantly gains only with adjunct Er,Cr:YSGG laser to SRP at 6 months after treatment. Comparing the results between the 2 treatment modalities, no significant differences could be found regarding PD reduction and PAL changes. The adjunct Er,Cr:YSGG laser to SRP does not improve the efficacy significantly although there was a tendency of greater PD reduction and PAL gain. This is in accordance with Magaz et al. [15] who demonstrated the efficacy of adjunctive application of Er,Cr:YSGG laser following SRP was not different from SRP alone. On the contrary, some investigations demonstrated significantly greater PD reduction and PAL gain with the application of Er,Cr:YSGG laser in addition to SRP [13, 14]. These 2 studies evaluated adjunctive Er,Cr:YSGG laser application to treat the early to severe periodontitis during initial periodontal therapy, while this present study was for the treatment of maintenance patients. It is possible to explain in part that the inflammation was much less in the maintenance patients until the differences were not demonstrated. Furthermore, one study used Er,Cr:YSGG laser application repeatedly with an average of 3 appointments in addition to SRP [13]. Since Rossman et al. [27] reported that epithelialization was retarded by at least 7 days using carbon dioxide laser compared with flap debridement in monkeys, multiple applications of Er,Cr:YSGG laser in order to retard apical epithelial migration may be more beneficial than single application. Further studies are needed both clinically and histologically.
Conclusion
Only SRP + Er,Cr:YSGG demonstrated statistically significant probing attachment level (PAL) gained at 6 months after treatment (0.8 ± 0.6 mm; p < 0.05); however, there were no statistically significant differences between the 2 treatment modalities regarding PD reduction, PAL gain, or GR at 6 months after treatment in maintenance patients with residual periodontal pockets.
References
Knowles JW, Burgett FG, Nissle RR, Shick RA, Morrison EC, Ramfjord SP (1979) Results of periodontal treatment related to pocket depth and attachment level. Eight years. J Periodontol 50(5):225–233
Rosling B, Serino G, Hellstrom MK, Socransky SS, Lindhe J (2001) Longitudinal periodontal tissue alterations during supportive therapy. Findings from subjects with normal and high susceptibility to periodontal disease. J Clin Periodontol 28(3):241–249
Parameter on periodontal maintenance (2000) J Periodontol 71(5-s):849–850
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Bragger U, Zwahlen M, Lang NP (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35(8):685–695
Tonetti MS, Lang NP, Cortellini P, Suvan JE, Eickholz P, Fourmousis I, Topoll H, Vangsted T, Wallkamm B (2012) Effects of a single topical doxycycline administration adjunctive to mechanical debridement in patients with persistent/recurrent periodontitis but acceptable oral hygiene during supportive periodontal therapy. J Clin Periodontol 39(5):475–482
Serino G, Rosling B, Ramberg P, Hellström MK, Socransky SS, Lindhe J (2001) The effect of systemic antibiotics in the treatment of patients with recurrent periodontitis. J Clin Periodontol 28(5):411–418
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontol 2000 36(1):59–97
Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Izumi Y (2009) Application of lasers in periodontics: true innovation or myth? Periodontol 2000 50:90–126
Schwarz F, Aoki A, Sculean A, Becker J (2009) The impact of laser application on periodontal and peri-implant wound healing. Periodontol 2000 51:79–108
Hakki SS, Berk G, Dundar N, Saglam M, Berk N (2009) Effects of root planing procedures with hand instrument or erbium, chromium:yttrium–scandium–gallium–garnet laser irradiation on the root surfaces: a comparative scanning electron microscopy study. Lasers Med Sci 25(3):345–353
Kimura Y, Yu DG, Fujita A, Yamashita A, Murakami Y, Matsumoto K (2001) Effect of erbium, chromium:YSGG laser on canine mandibular bone. J Periodontol 72(9):1178–1182
Pavone C, Perussi LR, de Oliveira GJ, Scardueli CR, Cirelli JA, Cerri PS, Junior EM, Spolidorio LC, Marcantonio RA (2015) Effect of Er,Cr:YSGG laser application in the treatment of experimental periodontitis. Lasers Med Sci 30(3):993–999
Kelbauskiene S, Baseviciene N, Goharkhay K, Moritz A, Machiulskiene V (2011) One-year clinical results of Er,Cr:YSGG laser application in addition to scaling and root planing in patients with early to moderate periodontitis. Lasers Med Sci 26(4):445–452
Dyer B, Sung EC (2012) Minimally invasive periodontal treatment using the Er,Cr: YSGG laser. A 2-year retrospective preliminary clinical study. Open Dent J 6:74–78
Magaz VR, Alemany AS, Alfaro FH, Molina JN (2016) Efficacy of adjunctive Er,Cr:YSGG laser application following scaling and root planing in periodontally diseased patients. Int J Periodontics Restorative Dent 36(5):715–721
Silness J, Loe H (1964) Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odont Scand 22:121–135
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Melcher AH (1976) On the repair potential of periodontal tissues. J Periodontol 47:256–260
Nyman S, Lindhe J, Karring T, Rylander H (1982) New attachment following surgical treatment of human periodontal disease. J Clin Periodontol 9(4):290–296
Hakki SS, Korkusuz P, Berk G, Dundar N, Saglam M, Bozkurt B, Purali N (2010) Comparison of Er,Cr: YSGG laser and hand instrument on the attachment of periodontal ligament fibroblasts to periodontally diseased root surfaces: an in vitro study. J Periodontol 81(8):1216–1225
Kerdmanee K, Laosrisin N (2015) PDL fibroblasts attachment to root surfaces treated by ultrasonic debridement and Er,Cr:YSGG laser. SWU Dent J 8(1):38–48
Polson AM, Frederick GT, Ladenheim S, Hanes PJ (1984) The production of a root surface smear layer by instrumentation and its removal by citric acid. J Periodontol 55(8):443–446
Aleo JJ, De Renzis FA, Farber PA (1975) In vitro attachment of human gingival fibroblast to root surface. J Periodontol 46(11):639–645
Polson AM, Proye MP (1982) Effect of root surface alterations on periodontal healing. II. Citric acid treatment of denuded root. J Clin Periodontol 9(6):441–454
Ito K, Nishikata J, Murai S (1993) Effects of Nd:YAG laser radiation on removal of a root surface smear layer after root planing: a scanning electron microscopic study. J Periodontol 64(6):547–552
Akiyama F, Aoki A, Miura-Uchiyama M, Sasaki KM, Ichinose S, Umeda M, Ishikawa I, Izumi Y (2011) In vitro studies of the ablation mechanism of periodontopathic bacteria and decontamination effect on periodontally diseased root surfaces by erbium:yttrium–aluminum–garnet laser. Lasers Med Sci 26(2):193–204
Rossman JA, McQuade MJ, Turunen DE (1992) Retardation of epithelial migration in monkeys using a carbon dioxide laser: an animal study. J Periodontol 63:902–907
Funding
This study was supported by the Faculty of Dentistry, Mahidol University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Faculty of Dentistry/Faculty of Pharmacy, Mahidol University Institutional Review Board (COA.No.MU-DT/PY-IRB 2016/013.1502). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sappipattana, Y., Teparat-Burana, T. Efficacy of adjunctive Er,Cr:YSGG laser application to scaling and root planing in periodontal maintenance patients with residual periodontal pockets. Laser Dent Sci 3, 169–174 (2019). https://doi.org/10.1007/s41547-019-00062-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-019-00062-x