Abstract
Purpose
The aim of this study was to compare the clinical results between single and multiple Er,Cr:YSGG laser applications as an adjunct to scaling and root planing (SRP) in periodontal maintenance patients with residual periodontal pockets.
Methods
This study was a split-mouth, double-blind, randomized clinical trial with 17 periodontal maintenance patients who presented two single-rooted teeth with probing depth (PD) of 5–9 mm and bleeding on probing (BOP). The teeth were randomly assigned to group A (single Er,Cr:YSGG application + SRP) and group B (multiple Er,Cr:YSGG application + SRP). Presence of plaque, BOP, PD, relative probing attachment level (RPAL), and relative gingival recession (RGR) was evaluated at baseline, 3 months, and 6 months after treatment by one calibrated examiner.
Results
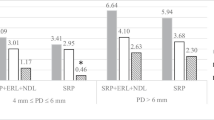
The results showed no statistically significant differences in PD reduction between groups at 3 months (group A: 1.06 ± 1.09 mm vs. group B: 1.00 ± 1.12 mm) and 6 months (group A: 1.18 ± 1.47 mm vs. group B: 1.00 ± 1.22 mm) compared with the baseline. At 3 months after treatment, the RPAL in group A had a gain (0.65 ± 1.06 mm) while group B was at a loss (0.06 ± 0.83 mm). At 6 months, the RPAL changes between 2 groups showed no statistically significant differences. Only in group B, wherein RGR had a statistically significant increase at 3 months (1.00 ± 0.94 mm) and 6 months (0.71 ± 0.69 mm) after treatment. However, this showed no statistically significant difference when compared with group A.
Conclusion
Both single and multiple adjunctive Er,Cr:YSGG applications to SRP in periodontal maintenance patients with residual periodontal pockets demonstrated PD reduction. Only the single laser application group showed clinical attachment level gain, and the multiple application group resulted in an increased gingival recession. However, there are no statistically significant differences between the two treatment modalities in all clinical parameters at 6 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
After the completion of active periodontal treatment, supportive periodontal therapy (SPT) is necessary to maintain periodontal health and prevent the recurrence of disease [1]. The residual probing pocket depth ≥ 6 mm is a risk indicator for tooth loss and progression of periodontitis during SPT [2]. Lang et al. [3] studied the indicator of periodontal stability, wherein the absence of BOP was a reliable predictor for maintenance periodontal health and the negative predictive value was 98%. Moreover, Lindhe et al. [4] recommended that loss of attachment level at least 2 mm was a predictor of recurrent periodontitis. During 10 years of SPT, the study reported 43.1% of recurrent periodontitis patients. The percentage of recurrent periodontal cases was similar in compliance and erratic compliance patients. When recurrent periodontitis was observed during SPT, non-surgical treatment should be the first choice of treatment, but further surgical procedure may be necessary [5].
Currently, laser has been used in periodontal pocket therapy because of its characteristics which include tissue penetration, tissue ablation, hemostasis, disinfection, detoxification effects, and biostimulation. Therefore, objectives of laser in pocket therapy include promoting periodontal tissue regeneration by debridement, decontamination, and increased bleeding in the bone defect favorable to periodontal regeneration [6]. Laser therapy as an adjunct to conventional mechanical treatment during SPT probably promotes the healing process by removing pocket epithelial lining in the residual periodontal pocket and detoxification root surface without producing a smear layer [7].
Several studies used a laser to promote periodontal regeneration by removing epithelium which retards epithelial downgrowth [8,9,10,11,12]. Rossmann et al. [8] compared open flap debridement (OFD) with OFD and epithelial removal by carbon dioxide, CO2 laser in experimentally induced periodontitis in monkeys. The results showed that keratinized epithelium migrated into sulcus at 14-day specimens in OFD sites whereas OFD + CO2 laser sites did not have epithelial lining along sulcus until 28 days after treatment. Epithelial removal by means of the conventional technique was compared with the conventional technique combined with a CO2 laser. The results showed that laser removed the sulcular epithelium more completely than the conventional technique [13].
Er,Cr:YSGG laser with 2780-nm wavelength can penetrate energy into more shallow tissue because of higher absorption coefficient in water than other lasers [14]. Pavone et al. [15] studied the effect of Er,Cr:YSGG in periodontal treatment. Periodontitis in rats was induced then divided into 4 groups: (1) control (non-treatment) group; (2) scaling and root planing (SRP) group; (3) laser treatment group; (4) laser treatment following SRP group. Seven days after treatment, a laser with or without SRP showed statistically more bone formation at the furcation area when compared with the SRP group. Nonetheless, the results on the 30th day demonstrated no significant difference in bone formation among the treatment groups. It was suggested that Er,Cr:YSGG in periodontal treatment resulted in bone formation. Kelbauskiene et al. [16] compared the clinical results after treatment between SRP with and without Er,Cr:YSGG. Laser was used for removing outer and inner epithelium lining and repeated with the same laser treatment procedure once a week for 3–4 weeks. The outcome was evaluated at 3 months, 6 months, and 12 months. After 12 months, laser treatment as an adjunct to the SRP group was presented with greater probing depth reduction, more clinical attachment level gain, and less percentage of BOP index than the SRP group. However, plaque index and gingival recession had no difference between groups.
Previous clinical studies with Er,Cr:YSGG laser were studies on single application [17, 18]. Since Er,Cr:YSGG laser can retard the sulcular epithelium up to 7 days [19], it is interesting to investigate if the removal of epithelium every 7 days up to 1 month will enhance better healing. The objective of this study was to compare the clinical results between single and multiple Er,Cr:YSGG laser applications as an adjunct to SRP in SPT patients with residual periodontal pockets.
Materials and methods
The study was a split-mouth, double-blind, randomized clinical trial. The study protocol was reviewed and approved by the Ethics Review Committee for Human Research at the Faculty of Dentistry and Faculty of Pharmacy, Mahidol University (MU-DT/PY-IRB 2016/030.0806). Informed consent was obtained from all participating subjects.
Nineteen patients with residual periodontal pocket after completion of periodontal treatment from the Periodontics Clinic, Faculty of Dentistry, Mahidol University, were selected.
Inclusion criteria were as follows: (1) received SPT ≤ 12 months; (2) had two single-rooted teeth with probing depth (PD) of 5–9 mm and BOP; and (3) full mouth plaque score < 30% [20].
Exclusion criteria included the following: (1) systemic diseases affecting periodontal healing, (2) using of medications affecting periodontal tissue, (3) pregnancy and lactation, (4) using systemic antibiotics and anti-inflammatory drugs within the previous 3 months, (5) smoker, (6) hopeless tooth [21], (7) abutment tooth, (8) thin gingival biotype, and (9) non-compliance.
Randomization of treated teeth to each group was performed after the first visit. A research assistant randomly assigned the tooth into group A (single Er,Cr:YSGG + SRP) or group B (multiple Er,Cr:YSGG + SRP).
Clinical measurement and data collection
One blinded and calibrated examiner (NW) carried out all the measurements. Inter-examiner reliability testing was compared with an experienced periodontist (TTB). Intra-examiner reliability testing was performed in five new patients. The variation between the repeated measurement within ± 1 mm and 90% of agreement were accepted. The percentages of inter-examiner testing and intra-examiner reliability testing were 93.33% and 96.67%, respectively.
The clinical parameters were recorded at baseline, 3 months, and 6 months after treatment using a periodontal probe (PCP UNC 15, Hu-Friedy) by the same examiner. The variables recorded were as follows: (1) presence/absence of supragingival plaque at the gingival margin (score 1/0); (2) presence/absence of bleeding on probing (BOP) (score 1/0). The following clinical parameters were measured with personalized acrylic stent: (3) PD; (4) relative probing attachment level (RPAL) measured from the apical border of the stent to the most apical part of the sulcus; (5) relative gingival recession (RGR) measured from the apical border of the stent to gingival margin.
Treatment
All subjects were treated by an experienced periodontist (TTB). Full mouth SRP was done except two single-rooted teeth included in this study. To avoid patient’s bias, all studied teeth were treated under local anesthesia (2% mepivacaine, 1:100,000 epinephrine). An Er,Cr:YSGG device (Waterlase, Biolase, USA) with a wavelength of 2780 nm was used as follows [22]: The laser system was set to a power output of 1.5 W, pulse of 30 Hz, 40% air, 50% water, and H-mode. The outer gingival epithelium was removed from gingival margin down to the width at least equal to PD by Radial Firing Perio Tip (RFPT) 5 tip of 14 mm in length. Then, the inner epithelial lining was removed from the gingival margin down to the bottom of the sulcus. The laser tip was led in parallel paths with the root surface. Ultrasonic (P5 Newtron®XS, Acteon, Switzerland) and hand instruments (Gracey curette) were used to remove calculus and root planing. The produced smear layer on the root surface by conventional treatment was removed by laser application. Then, the laser system changed the setting to a power output of 1.5 W, pulse of 30 Hz, 10% air, 10% water, and H-mode for inducing blood coagulation. After that, the treated site was compressed with moist gauze. At the end of the 1st visit, studied teeth were divided into group A (single Er,Cr:YSGG application + SRP) (Fig.1) and group B (multiple Er,Cr:YSGG application + SRP). Only in group B were same procedures performed once a week for outer and inner epithelium removal with reducing 1 mm, 2 mm, and 3 mm of initial probing depth length at 2nd, 3rd, and 4th week respectively (Fig.2).
Statistical analysis
Statistical analysis was performed using SPSS for Windows version 21. The null hypothesis was rejected at a 0.05 level of significance. Intergroup and intragroup differences of PD, RPAL, and RGR were analyzed by the Friedman test. Both GBI and PI between intergroup and intragroup were compared by related sample McNemar’s test. The different changes after treatment between groups were compared with the Wilcoxon matched-pairs signed-rank test.
Results
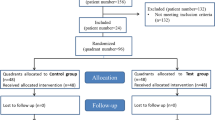
A total of 19 patients were examined; two patients dropped out: one had to use antibiotics and the other failed to attend the evaluation appointment (Fig. 3). Of the 17 remaining patients, the mean age was 52 ± 8.64 years, 15 females and 2 males. Presence of plaque and PD at baseline had no statistically significant differences (p > 0.05) between the two groups (Tables 1 and 3).
All patients had a mild post-operative burning sensation for 1–2 days, and one patient had sensitive teeth after the first laser treatment, but all symptoms were gradually relieved.
A percentage of sites with the presence of plaque in groups A and B were unchanged throughout the study, and no statistically significant differences between groups (Table 1) were found. Meanwhile, a percentage of sites with the presence of BOP in both groups were lower at 3 months compared with baseline and it slightly increased at 6 months. There were no statistically significant differences either at 3 months or 6 months between the two groups (Table 2).
Mean PD reductions at 3- and 6-month follow-up in groups A and B were significantly different from baseline (p < 0.005) in both groups and no statistically significant differences between groups at all the time points (p > 0.005). The RPAL after treatment in group A had a gain (0.82 ± 1.29 mm) which was significantly different from baseline while group B was at a gain (0.29 ± 1.10 mm) which is clinically insignificant (Table 3). The RPAL changes were not statistically different between groups (p > 0.05). Although increased RGR was distinct in group B, there were no statistically significant differences between groups (p > 0.05) (Table 4).
Discussion
Previous clinical studies reported using the Er,Cr:YSGG laser for non-surgical periodontal treatment. One study reported that single laser application as an adjunct to SRP improved PD reduction and there was a gain in clinical attachment level compared with SRP alone [18]. On the aspect of epithelial retardation, multiple laser application may enhance periodontal healing. The results of the present study have demonstrated that mean PD reduction and lower BOP were observed in both groups and there were no statistically significant differences between groups. The difference in RPAL between baseline and 6 months after treatment reached statistical significance throughout the study in only the single laser treatment group, but an increased gingival recession was found in multiple laser treatment group. However, there are no statistically significant differences between the two treatment modalities in all clinical parameters at 6 months.
Only one patient reported tooth hypersensitivity of both treated teeth after the 1st visit of treatment, but the symptom was relieved within a week. During the 2nd–4th week post-treatment, none of the patients reported any symptoms. Tooth hypersensitivity possibly resulted from SRP. Fischer et al. [23] reported dentin hypersensitivity after supragingival and subgingival scaling and the symptom had a tendency to decrease 2 weeks after the subgingival scaling. In addition, Er,Cr:YSGG application may not be a cause of hypersensitivity with regard to scanning electron microscopy evaluation after applying Er,Cr:YSGG laser to the root surface showed melt peritubular dentin and reduced tubular entrance diameter. This may explain sensitivity reduction [24].
Some clinical studies reported using the Er,Cr:YSGG laser as an adjunct to SRP compared with SRP alone. Magaz et al. [17] reported on a comparative study between SRP by curette and SRP followed by Er,Cr:YSGG laser application. Six months after treatment, PD reduction and GR were shown in both groups, but there were no differences between groups. However, more clinical attachment level (CAL) gain was found in the SRP group. In contrast, a study on using Er,Cr:YSGG as an adjunct to SRP in SPT patients found different results. The SRP combination with Er,Cr:YSGG showed more PD reduction and CAL gain than SRP alone at 3 months after treatment [18]. The advantages of combined Er,Cr:YSGG application with SRP were reported in several studies. Er,Cr:YSGG laser with the Radial Firing Perio Tip (RFPT) showed the significant reduction of bacterial load of Prevotella intermedia, Tannerella forsythia, Treponema denticola, Fusobacterium nucleatum, Porphyromonas gingivalis (Pg), and Aggregatibacter actinomycetemcomitans (Aa) in the periodontal pocket up to 6 months [25]. In addition, qualitative analysis in bacterial distribution after laser therapy (combined Er,Cr:YSGG and 940 nm diode) showed that Aa was not detected at 6 months compared with SRP. Pg was present in 10 out of 25 lased cases vs. 23 out of 24 SRP cases [26]. This also resulted in significantly better both clinical and microbiological improvement compared with SRP alone [27]. And no smear layer was observed with Er,Cr:YSGG laser while it was seen with ultrasonic and hand instruments [28].
Multiple Er,Cr:YSGG application as an adjunct to SRP was reported in two studies. Kelbauskiene et al. [16] used Er,Cr:YSGG once a week for 3–4 weeks. The results showed PD reduction and CAL gain, but the gingival margin level did not change. In addition, another study reported similar results that used Er,Cr:YSGG 3 cycles every three days [29]. The present study is the first study to compare single and multiple applications as an adjunct to SRP. The results show PD reduction in both treatment modalities without a difference. But single application had RPAL gain while multiple applications resulted in no RPAL change from baseline. On the contrary, the present study shows increased RGR after treatment in the multiple application group. However, the RGR changes between the 2 groups showed no statistically significant differences. The results from the present study were different from previous studies possibly due to those studies being done in new patients with more inflammation. Therefore, the outcomes of treatment were more distinct.
Multiple applications of laser treatment for 4 weeks in this study demonstrated 1-mm increased gingival recession. The healing process of surrounding tissues may be disturbed by repeated lasing. Wang et al. [30] studied the healing process by histological examination in bone and soft tissue of rabbit jaws after irradiated with Er,Cr:YSGG laser. They found that the alveolar mucosa had complete healing on the seventh day but the reconstruction of collagen fiber was not complete at 28 days. Further study should investigate the results of multiple laser applications only at the outer surface without disturbing the healing process in the gingival sulcus.
SRP by conventional technique produced a smear layer at the interface between the root surface and the fibrin and impeded physical linkage [31]. Fekrazad et al. [32] found that treatment with Er,Cr:YSGG laser as a root conditioning for removing the smear layer increased fibroblast attachment more than when using the EDTA. Additionally, in vitro study demonstrated that the laser increased gingival fibroblast proliferation than without the radiation group [33]. Combination of Er,Cr:YSGG and ultrasonic scaler also improved fibroblast adhesion on the root surface more than with laser or ultrasonic scaler alone [34].
The aforementioned studies used the Er,Cr:YSGG with the MZ laser tip in adjunct to traditional SRP [16, 17, 29]. In contrast, the present study used RFPT which is taper in shape. The company claimed that this produced the primary radial emission (80%) of laser energy with a straight emission (20%) and got better access for the periodontal pockets [22].
The percentage of teeth with BOP after laser treatment was reduced in both groups and conformed to other studies. The percentage of teeth with the presence of plaque of both groups was constant throughout the study. It implied that the outcomes of laser treatment did not result from the patient’s plaque control. Moreover, acrylic stents were used for repeated measurement and this created the reference point for accurate measurement.
Further longitudinal studies are needed. In addition, histological evaluation in healing after non-surgical periodontal treatment by Er,Cr:YSGG should be conducted.
Conclusion
Both single and multiple Er,Cr:YSGG applications result in PD reduction while only single laser application result gained attachment level and multiple application group result increased RGR. However, there are no statistically significant differences between the two treatment modalities.
References
Shick RA (1981) Maintenance phase of periodontal therapy. J Periodontol 52(9):576–583
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Brägger U, Zwahlen M, Lang NP (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35(8):685–695
Lang NP, Adler R, Joss A, Nyman S (1990) Absence of bleeding on probing: an indicator of periodontal stability. J Clin Periodontol 17(10):714–721
Lindhe J, Haffajee AD, Socransky SS (1983) Progression of periodontal disease in adult subjects in the absence of periodontal therapy. J Clin Periodontol 10(4):433–442
Chace R (1977) Retreatment in periodontal practice. J Periodontol 48(7):410–412
Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, Romanos GE, Taniguchi Y, Sasaki KM, Zeredo JL, Koshy G, Coluzzi DJ, White JM, Abiko Y, Ishikawa I, Izumi Y (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000 68(1):217–269
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontol 2000 36:59–97
Rossmann JA, McQuade MJ, Turunen DE (1992) Retardation of epithelial migration in monkeys using a carbon dioxide laser: an animal study. J Periodontol 63(11):902–907
Israel M, Rossmann JA, Froum SJ (1995) Use of the carbon dioxide laser in retarding epithelial migration: a pilot histological human study utilizing case reports. J Periodontol 66(3):197–204
Rossmann JA, Israel M (2000) Laser de-epithelialization for enhanced guided tissue regeneration: a paradigm shift? Dent Clin N Am 44(4):793–809
Romanos GE, Henze M, Banihashemi S, Parsanejad HR, Winckler J, Nentwig GH (2004) Removal of epithelium in periodontal pockets following diode (980 nm) laser application in the animal model: an in vitro study. Photomed Laser Surg 22(3):177–183
Nevins ML, Camelo M, Schupbach P, Soo-Woo K, Kim DM, Nevins M (2012) Human clinical and histologic evaluation of laser-assisted new attachment procedure. Int J Periodontics Restorative Dent 32(5):497–507
Centty IG, Blank LW, Levy BA, Romberg E, Barnes DM (1997) Carbon dioxide laser for de-epithelialization of periodontal flaps. J Periodontol 68(8):763–769
Cobb CM, Low SB, Coluzzi DJ (2010) Lasers and the treatment of chronic periodontitis. Dent Clin N Am 54(1):35–53
Pavone C, Perussi LR, Oliveira GJPL, Scardueli CR, Cirelli JA, Cerri PS, Junior EM, Spolidorio LC, Marcantonio RAC (2015) Effect of Er,Cr:YSGG laser application in the treatment of experimental periodontitis. Lasers Med Sci 30(3):993–999
Kelbauskiene S, Baseviciene N, Goharkhay K, Moritz A, Machiulskiene V (2011) One-year clinical results of Er,Cr:YSGG laser application in addition to scaling and root planing in patients with early to moderate periodontitis. Lasers Med Sci 26(4):445–452
Magaz V, Alemany A, Alfaro F, Molina J (2016) Efficacy of adjunctive Er, Cr:YSGG laser application following scaling and root planing in periodontally diseased patients. Int J Periodontics Restorative Dent 36(5):715–721
Sappipattana Y, Teparat-Burana T (2019) Efficacy of adjunctive Er, Cr :YSGG laser application to scaling and root planing in periodontal maintenance patients with residual periodontal pockets. Laser Dent Sci 3:169–174
Perussi LR, Pavone C, de Oliveira GJ, Cerri PS, Marcantonio RA (2012) Effects of the Er,Cr:YSGG laser on bone and soft tissue in a rat model. Lasers Med Sci 27(1):95–102
Badersten A, Nilvéus R, Egelberg J (1990) Scores of plaque, bleeding, suppuration and probing depth to predict probing attachment loss: 5 years of observation following nonsurgical periodontal therapy. J Clin Periodontol 17(2):102–107
McGuire MK (1991) Prognosis versus actual outcome: a long-term survey of 100 treated periodontal patients under maintenance care. J Periodontol 62(1):51–58
Biolase Technology, Regenerative Er,Cr:YSGG Periodontitis ai Regimen (REPaiR), Waterlase® Brochure, Irvine, Calif, USA, 2017. http://scanlase.fi/wp-content/uploads/REPaiR.pdf
Fischer C, Wennberg A, Fischer RG, Attstrom R (1991) Clinical evaluation of pulp and dentine sensitivity after supragingival and subgingival scaling. Endod Dent Traumatol 7(6):259–265
Gholami GA, Fekrazad R, Esmaiel-Nejad A, Kalhori KA (2011) An evaluation of the occluding effects of Er;Cr:YSGG, Nd:YAG, CO(2) and diode lasers on dentinal tubules: a scanning electron microscope in vitro study. Photomed Laser Surg 29(2):115–121
Gutknecht N, Betteray CV, Ozturan S, Vanweersch L, Franzen R (2015) Laser supported reduction of specific microorganisms in the periodontal pocket with the aid of an Er,Cr:YSGG laser: a pilot study. Sci World J. https://doi.org/10.1155/2015/450258
Ciurescu C, Vanweersch L, Franzen R, Gutknecht N (2018) The antibacterial effect of the combined Er,Cr:YSGG and 940 nm diode laser therapy in treatment of periodontitis: a pilot study. Laser Dent Sci 2:43–51
Ciurescu CE, Cosgarea R, Ciurescu D, Gheorghiu A, Popa D, Franzen R, Arweiler NB, Sculean A, Gutknecht N (2019) Adjunctive use of InGaAsP and Er,Cr:YSGG lasers in nonsurgical periodontal therapy: a randomized controlled clinical study. Quintessence Int 50(6):436–447
Ezzat A, Maden I, Hilgers RD, Gutknecht N (2018) In vitro study: conventional vs. laser (Er,Cr:YSGG) subgingival scaling and root planing; morphologic analysis and efficiency of calculus removal using macroscopic, SEM and laser scanning. Laser Dent Sci 2:81–87
Gupta M, Lamba A, Verma M, Faraz F, Tandon S, Chawla K, Koli D (2013) Comparison of periodontal open flap debridement versus closed debridement with Er,Cr:YSGG laser. Aust Dent J 58(1):41–49
Wang X, Zhang C, Matsumoto K (2005) In vivo study of the healing processes that occur in the jaws of rabbits following perforation by an Er,Cr:YSGG laser. Lasers Med Sci 20(1):21–27
Polson A, Proye M (1983) Fibrin linkage: a precursor for new attachment. J Periodontol 54(3):141–147
Fekrazad R, Lotfi G, Harandi M, Ayremlou S, Kalhori KAM (2015) Evaluation of fibroblast attachment in root conditioning with Er, Cr:YSGG laser versus EDTA: a SEM study. Microsc Res Tech 78(4):317–322
Talebi-Ardakani MR, Torshabi M, Karami E, Arbabi E, Rezaei EZ (2016) In vitro study of Er:YAG and Er, Cr:YSGG laser irradiation on human gingival fibroblast cell line. Acta Med Iran 54(4):251–255
Fekrazad R, Lotfi G, Harandi M, Ayremlou S, Kalhori AMK, Gholami GA, Nokhbatolfoghahaei H (2017) Comparing fibroblast attachment in root surface scaling with Er, Cr:YSGG laser versus ultrasonic scaler: SEM study. Microsc Res Tech 80(8):917–922
Funding
This study was supported by the Faculty of Dentistry, Mahidol University Research Fund.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Nuttha Watchanasanout, and Thitiwan Teparat-Burana. The first draft of the manuscript was written by Nuttha Watchanasanout, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Faculty of Dentistry/Faculty of Pharmacy, Mahidol University, Institutional Review Board (COA.No.MU-DT/PY-IRB 2016/030.0806).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watchanasanout, N., Teparat-Burana, T. Single versus multiple adjunctive Er,Cr:YSGG application to scaling and root planing in periodontal maintenance patients with residual periodontal pockets. Laser Dent Sci 4, 187–193 (2020). https://doi.org/10.1007/s41547-020-00105-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-020-00105-8