Abstract
Background
Resistance training holds promise for nursing home residents to prevent further disabilities, falls, and fractures. Free weight as well as machine training may offer an efficient option to improve physical performance, but the feasibility of these training regimes among elderly who require continuous institutional care is still open.
Aims
(1) To examine the feasibility of a 3-month machine vs. free weight strength training program in institutionalized older adults, and (2) to determine the effects on physical performance.
Methods
This study is a two-arm, single-blind, randomized controlled feasibility study within a nursing home. 45 institutionalized elderly men and women (aged 83.8 ± 8.0, 12 men, 33 women) were randomly divided into two groups. The two groups completed either a free weight (FWT) or machine training (MT) for 12 weeks, twice per week, 45–60 min per session, in an individually supervised format. Performance was assessed with the 11-step stair-climbing test, 10-m walk test, Timed Up and Go Test (TUG), 30-s Chair Rising Test (CRT), grip strength, body mass index.
Results
Indices of feasibility showed a recruitment and adherence rate of 53.6 and 87.5%, respectively. 35.6% of the participants dropped out after several weeks for personal reasons, illness, medical visits, or hospital stays. After the program no significant differences on motor performance were found between MT and FWT. However, there were significant improvements for both training groups on the TUG and the CRT.
Conclusions
The present pilot study showed that it is feasible to conduct a strength training program in institutionalized participants. The more robust changes in motor function could serve as a basis for large randomized clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Living in a nursing home is accompanied by a progressive decline in physical activity. Buckinx et al. [1] showed that nursing home residents walk less than 1700 steps per day, which is considerably less than the 10,000 steps recommended by the WHO. A vicious cycle is created when reduced physical activity as well as increases in sedentariness is followed by decreased walking speed, muscle strength, endurance, and loss of co-ordination; this is often among others the result of fatigue, bed rest, fear of falling, and a progressive loss of muscle mass and muscle strength [2]. Specifically, a decrease in muscle function has been identified as an independent predictor of hospitalization, disability, and death [3]. The seriousness of this problem is further demonstrated by the high prevalence of muscle loss (sarcopenia; 40%; [4, 5]) among older adults living in nursing homes [6].
The loss of muscle mass has been reported to decline gradually by 1–2% each year from the fourth decade. There is evidence that the loss of muscle strength, especially explosive force, is much higher than the loss of muscle mass [7], declining by 3–3.5% each year from the age of 50–60 years, culminating in a 50% loss across the lifespan [8]. It was established that the reason for serious injuries was primarily connected to a loss of ability to perform movements at high speed in combination with delayed reactions of the upper and lower limbs in the event of a fall [9]. Reduced strength in the lower limbs results in a reduction in gait speed, balance, stair-climbing ability and the ability to rise from a chair [1, 10]. In addition, the loss of muscle mass is commonly associated with loss of bone density, which leads to a high risk of hip fractures [11].
Several studies have recently focused on training programs for elderly people and on how to delay, stop or reverse muscle loss as well as power, especially in terms of age-related muscle changes and the ensuing consequences (for in-depth reviews see [12–16]). Law et al. [13] conclude that a well-designed, progressive resistance training program with moderate to high exercise intensity results in profound enhancements in muscle mass and muscle strength in healthy, community-dwelling older adults; however, there is still no definitive gold standard prescription for resistance training exercise for mobility outcomes [15].
In spite of these positive effects only few interventions have focused on frail individuals or individuals with impaired physical ability as well as nursing home residents, although this is where the most significant improvements are expected [17–21]. A recent review by Valenzuela [21] focusing on older adults in nursing homes found significant improvements in muscle strength and functional performance outcomes, including chair stand, stair climbing, gait speed, balance and functional capacity following progressive resistance training exercise. These improvements occurred despite advanced age, presence of chronic diseases, extremely sedentary habits and functional disabilities [21]. Furthermore, strength training in frail older adults has been shown to improve bone density [22], cardiometabolic health [23], and cognitive impairment [24, 25]. Essential precondition for successful interventions have been linked to higher intensities [26–28], supervision, and progression in resistance training [29].
In the majority of the resistance training studies in frail older individuals and/or individuals living in nursing homes, the exercises were performed using, wrist and ankle weights [30], functional exercises without machines [31], elastic bands [32, 33] or seated weight training machines [34–37]. All these studies in this population differ greatly with respect to the parameters that were addressed, the load standards (training sessions per week, number of series, number of repetitions, training intensity, etc.), the training methods, the duration of the study and the tested group of subjects. Even more important, according to the theory of specificity [38], the closer the movement patterns during training are to the desired activity, free weight strength training has been shown to be more effective than fixed-form exercises in improving performances in both physically active individuals [39]. Only few studies have examined if free weight strength training programs are appropriate and efficient for healthy, community-dwelling older adults [40, 41]. For example, Schott and Knobl [41] compared the effects of free weight training with machine training in a group of 32 men and women aged 60–86 years. They show that (1) dynamic strength gains from 6 months of resistance training in older individuals are sustainable (not entirely lost even after 6 weeks of detraining); (2) these effects are specifically related to the exercises performed in the training program (free weights vs. machine); (3) adoption of maintenance-level moderate-intensity training significantly attenuates the decline in dynamic strength of previously trained muscles; and (4) free weights training improves the overall functional capacity of older adults.
However, it remains unclear whether machine- or free weight training would be feasible and effective among those with substantial physical disabilities as well. The purpose of the present 12-week blinded RCT was to examine (1) whether older adults requiring continuous institutional care can tolerate machine- or free weight training, and (2) whether machine- or free weight training has the potential to maintain or even improve physical performance in this clinically relevant group. The present trial is a pilot study, which primarily assessed the feasibility of machine- or free weight training and sought challenges and obstacles in implementing machine- or free weight training among frail nursing home residents.
Method
Experimental design and recruitment
A randomized, controlled, two-group, pre-post, and single-blinded (on the patients side) pilot study following the CONSORT statement [42] was performed to test the feasibility and effectiveness of strength training programs using either free weights or machines in older people.
Participant recruitment and assessment occurred over a 2-month period. The nursing home was approached about participation due to their availability of an onsite gym via phone. The Principal Investigator (PI) met with the director of the nursing home, and explained the purpose and design of the study. Following the confirmation of the director to conduct the study, patient files were controlled against the inclusion criteria by the Head of the Sport Department. Eligible individuals (n = 195) were approached by the research assistant (BJ) and the Head of the Sport Department, who informed them about the project, and requested an expression of interest to participate. 39 individuals declined due to personal reasons (e.g., no time, no motivation to participate in a program across 12 weeks), 111 individuals did not meet the inclusion criteria.
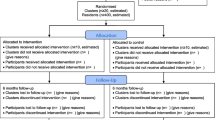
Prior to the initial assessment, the remaining 45 eligible participants were randomized to either the free weight training group (FWT) or the machine training group (MT) by a research administrator. All subjects had performed their specific exercises; there was no control group. The first day of testing included a review of the patient’s medical history, and familiarization with the performance testing. One week later, patients reported for the second day of testing. All assessments were completed by blinded research assistants one-on-one with each participant. Timed motor performance of specific ADLs and strength were measured (11-step stair-climbing test, 10-m walk test, Timed Up and Go Test, 30-s Chair Rising Test, grip strength). Subjects were familiarized with the resistance training techniques. Participants were blinded to group assignment before baseline measurements, after which all participants were informed of their assignment. The ADLs and strength were retested at 12 weeks after the initial testing phase. The study flow diagram is outlined in Fig. 1.
Participants
45 nursing home residents aged 61–95 years (mean age 83.8 ± 8.0) were chosen from a nursing home in Freiburg, Germany. The nursing home had 195 residents. Residents who were ambulatory and had only minor cognitive disorders (MMSE ≥24) that would not affect their ability to follow instructions were able to participate in the study. The exclusion criteria were artificial prosthesis, participation in any physical therapies other than those routinely provided in the nursing home, any symptom that a medical examiner deemed as warranting exclusion, and any disease that contraindicated the exercise program or required special care (e.g., coronary artery disease, thrombosis, moderate or severe bone, lung or renal diseases).
Informed written consent was obtained from organizations or caregivers prior to the beginning of testing, and by the participants themselves, who were told that they could opt out at any time. All procedures were in accordance with the Declaration of Helsinki with ethical standards, legal requirements and international norms.
Measures
Feasibility
The primary feasibility outcomes included eligibility rate, recruitment rate, measurement completion rate, loss to follow-up, and adherence. Eligibility rate was defined as the total number of patients screened, divided by the total number eligible. Recruitment rate was defined as the number of patients recruited from those eligible. Loss to follow-up was defined as participants who were withdrawn or dropped out. Adherence to the exercise intervention was measured by the number of sessions attended out of 24. A 70% attendance rate for the training sessions was set as the definition for being adherent to the training program [43].
Physical performance
Physical performance was assessed with the Timed Up and Go Test (time in seconds to get out of chair, walk eight feet, round a pylon, and return to be seated in chair; TUG) [44], the 30-s Chair Rise Test (number of unassisted chair stands performed in 30 s; CRT) [45], the 10-m walk test (average of two trials) [46], the 11-step stair-climbing test (time in seconds to climb 11 risers of stairs as fast as possible) [47], and grip strength (left and right hand with a Jamar dynamometer) [48].
Body composition
Anthropometric measurements were made by standardized procedures. Weight and height were measured for each subject, and BMI was calculated from these values.
Residents’ care level
Residents’ care level serves as an indicator for their need of assistance with activities of daily living (ADL). It is assessed by the German Health Insurance Medical Service (MDK), varies from 0 no need of care (i.e., need for assistance required for less than 90 min per day on average) to 3 in constant need of care (i.e., need for assistance required around the clock, on average at least for 5 h per day) [49].
Intervention
In accordance with ACSM guidelines for strength training, participants allocated in both intervention groups enrolled in two weekly non-consecutive exercise sessions for 12 weeks. Each session lasted approximately 45–60 min, and started and ended with a low-intensity warm-up and cool-down period (∼5 to 7 min each) consisting mainly of stretching exercises involving all major muscle groups. The training was performed in small groups with three to six participants, always under a close supervision of two exercise specialists, who provided guidance and adequate instructions to ensure that the exercises were performed properly and safely. All intervention sessions were conducted in the same in-house gym. Participants were accompanied from the ward for the training supervised by a caretaker or the therapist. The goal was for all participants in the intervention groups to perform a total of 24 exercise sessions.
Strength exercises focused on upper and lower limb strengthening to activate large muscle groups known to contribute to gait speed, balance, mobility, and upper body stability. The MT protocol consisted of five exercises: leg press, latissimus pull down, elbow and shoulder extension (dip), and back extensor (Proxomed; Compass®). Training was initiated at 50% of the eight repetition maximum (8RM), a measure of muscle strength, at a training volume in the 1st set of 18–20 repetitions. Training intensity was increased in the 2nd set as tolerated to 75–80% of the 8RM. For the FWT protocol, subjects performed two sets of 10–12 repetitions using dumbbells (weight range 1–7 lbs). Between the sets, participants had to rest for about 1 minute. The lifts used for FWT sessions engaged similar muscle groups compared to the MT sessions. The weights for both groups were regularly increased to elicit a rating of perceived exertion equal to 12 (between light and somewhat hard) using the Borg Rate of Perceived Exertion scale (range 6–20).
Data analysis
Data were analyzed using a 2 × 2 analysis of co-variance to evaluate group (FWT vs MT) and time (T1 vs T2) differences controlled for age and gender. Within-group changes are expressed as pre–post-effect sizes (ES), which represents the difference between the follow-up and baseline mean values divided by SD of the given outcome variable [50]. Data were then evaluated using paired t tests to determine if significant changes occurred in response to exercise. All results are presented as mean ± standard deviation, and data were considered significant when p ≤ 0.05.
Results
Demographic profiles and baseline differences of the participants
There were no significant differences in the demographic profiles of the participants who remained in the study and those who dropped out (all p > 0.05). The mean age of the 29 remaining participants was 84.1 ± 8.3 years (range 61–95 years) with the majority of them being oldest-old adults (85+ years, 69.0%). The majority of participants was female (69.0%), and needs a minimum of 90 min of support daily in two areas of basic care (n = 11; level of care 1) or a minimum of three times daily assistance in basic care (n = 12; level of care 2). There were significant differences in age and height between both experimental groups (Table 1).
Feasibility
195 patients were assessed for eligibility, 84 (43.1%) were eligible, and 45 (53.6%) were recruited. 16 participants discontinued training during the study period (35.6%). Participants dropped out after several weeks for personal reasons, illness, medical visits, or hospital stays. In MT the loss to follow-up was 39.1%. In FWT, 31.8% were lost to follow-up (see also Fig. 1).
Intervention adherence
There were 24 sessions in each of the strength training regimes. On average, the participants (n = 29) attended 91.1 and 83.9% in the FWT and MT groups, respectively (see also Fig. 1). No adverse effects in any of the training sessions were observed.
Physical performance
Mean changes in BMI and physical performance in the FWT and MT groups are shown in Table 2. There was only a significant difference for grip strength (left hand) at baseline between FWT and MT. For those who completed the 3-month study (n = 29), the trend of change was further analyzed. Results indicated that some of the functional fitness indicators [30-s chair rise, F(1,25) = 5.09, p = 0.033, η 2 = 0.169; Timed Up and Go Test, F(1,21) = 3.14, p = 0.091, η 2 = 0.130] of both experimental group participants improved significantly. However, in almost all participants, substantial improvements in physical performance were evident (see Fig. 2). ES of Δ post–pre revealed higher values for MT in 10-m gait, stair climbing, and TUG, while the FWT revealed higher values for chair rise and grip strength, showing that after different strength training regimes different aspects of physical performance improved. No significant effects for age or gender were observed.
Discussion
The purpose of the study was to determine the feasibility of a machine vs free weight training program and to perform an exploratory analysis concerning the effects of such programs on physical performance, and body composition in institutionalized patients. Because this was a pilot study using a small sample size, the results should be considered preliminary and viewed with caution. Still, the current results could serve as a basis for future larger randomized clinical trials.
These individuals basically represent a potential target group for exercise programs with a focus on resistance training, but they are also very heterogeneous in terms of medical conditions, disabilities and treatments. Therefore, the study was realized in small groups which contributed to their feasibility. The feasibility was determined by the participation rate of the training sessions (>70%), the drop-out rate (<35%), the absence of unrequested adverse effects as well as (people) following the training instructions. The recruitment rate of 53% and the drop-out rate of 35.6% can be compared with other studies. The average training participation of 88% can be rated quite highly. This quote is above the values of other studies [51] and is highly promising for further studies. Starting the training with low intensity and the progressive increase throughout the training period helped the participants to avoid unrequested adverse effects such as sore muscles, state of exhaustion or experience of failure. This approach prevents participant, especially nursing home residents with low sense of self-esteem and little external locus of control, from breaking off too soon [52]. Encouraging the participants and giving individual feedback helped to have high training participation. This approach takes plenty of time but with the support of volunteers and members of the family it would be possible to offer a regular and structured program.
Equivalent to previous studies of similar length, duration, and intensity [52–56] the participants of both training groups could, to some extent, achieve substantial performance increases. The strongest effect for both resistance training programs was seen on the 30-s Chair Rise Test and the Timed Up and Go Test. The MT group seemed to improve their performance more than the FWT group, which seems to be driven by the higher number of males and the younger age in this group; however, there were neither significant time × group interactions nor any significant influences of the covariates age and gender. Not surprisingly, participants with no need or minor need of care outperformed those who exhibit an extreme or constant need of care, especially on the mobility tasks [57]. Positive effects of both training regimes even on the group with extreme or constant need were found. Although statistically insignificant, the trends in the individual data confirm the clinical importance of this pilot study.
These findings indicate that a loss of strength as one gets older is not only the result of the biological aging process, but, if one ignores illness and accidents, the specific consequence of physical inactivity and/or sedentariness. It has been proven that increasing the muscle power of older adults results in a functional improvement and reduces the incidence of disability [9]. There is evidence to suggest that strength can be trained up to a very high age and, therefore, the loss of autonomy can be delayed or even avoided all together. However, there is still a huge research deficit with regard to which training program (small devices or machines) is more effective for maintaining or improving day-to-day skills among untrained and trained elderly people, and the impact of strength training on fine motor skills. It has been proven that the lower extremities of healthy elderly people profit particularly from free weight training [41]. In this study involving 32 healthy trained adults aged between 60 and 86, increases of 30–115% were achieved depending on the muscle group and training methods. To what extent this complex training form is feasible for elderly nursing home residents, who are mentally, cognitively and physiologically weaker, has to our knowledge not been addressed so far. This is, however, important because any form of complexity, variation, changes in activity and environment are perceived as disruptive and are a source of stress, which could lead to a lack of acceptance of the activity, in this case the training.
Study limitations
There are, however, a number of limitations to be considered when interpreting the results. First, the restricted sample size limits us from producing clear-cut conclusions and prohibits us from generalizing the present findings to a larger population. We concede that 45 participants assessed represented a recruitment rate of only 53.6% of the participants initially thought to be eligible for the study and only about 23.1% of the facility’s population. However, this rate of uptake is not uncommon in these kinds of studies [58]. Second, due to the lack of a control group, the possibility that other factors in addition to two resistance programs contributed to the improved physical performance cannot be ruled out. Third, the assessment of muscle power and muscle strength using machines was not considered in this study, although additional data suggest that muscle power is a strong determinant of physical performance and mobility skills in older adults [59]. Finally, no follow-up period was included in this pilot study. However, a follow-up with a control group should be incorporated in future studies to show that the progressive deterioration for seniors spending most of their time in a sedentary mode could be prevented.
Conclusions
Despite the limitations, both resistance training programs had high feasibility, compliance, and may be effective for preventing decline in the functional and cognitive status [60], and even improving physical performance of institutionalized older adults. Future studies using larger samples, longer intervention periods, and follow-up assessments are needed to clarify the specific effectiveness of the training programs.
References
Buckinx F, Mouton A, Reginster JY et al (2017) Relationship between ambulatory physical activity assessed by activity trackers and physical frailty among nursing home residents. Gait Posture 54:56–61
De Vries NM, Staal JB, van der Wees PJ et al (2016) Patient-centred physical therapy is (cost-)effective in increasing physical activity and reducing frailty in older adults with mobility problems: a randomized controlled trial with 6 months follow-up. J Cachexia Sarcopenia Muscle 7:422–435
Newman AB, Kupelian V, Visser M et al (2006) Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci 61:72–77
Abellan van Kan G (2009) Epidemiology and consequences of sarcopenia. J Nutr Health Aging 13:708–712
Cruz-Jentoft AJ, European Working Group on Sarcopenia in Older People et al (2010) Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Senior H, Henwood T, Beller E et al (2015) Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas 82:418–423
Manini TM, Clark BC (2012) Dynapenia and aging: an update. J Gerontol A Biol Sci Med Sci 67:28–40
Eriksen CS, Garde E, Reislev NL et al (2016) Physical activity as intervention for age-related loss of muscle mass and function: protocol for a randomised controlled trial (the LISA study). BMJ Open 6:e012951. doi:10.1136/bmjopen-2016-012951
Pereira A, Izquierdo M, Silva AJ et al (2012) Effects of high-speed power training on functional capacity and muscle performance in older women. Exp Gerontol 47:250–255
Connelly DM (2000) Resisted exercise training of institutionalized elderly adults for improved strength and functional mobility: a review. Top Geriatr Rehabil 15:6–27
Morley JE, Anker SD, von Haehling S (2014) Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology—update 2014. J Cachexia Sarcopenia Muscle 5:253–259
Lacroix A, Hortobagyi T, Beurskens R et al (2017) Effects of supervised versus unsupervised training programs on balance and muscle strength in old adults: a systematic review and meta-analysis. Sports Med. doi:10.1007/s40279-017-0747-6
Law TD, Clark L, Clark B (2016) Resistance exercise to prevent and manage sarcopenia and dynapenia. Annu Rev Gerontol Geriatr 36:205–228
McKinnon NB, Connelly DM, Rice CL et al (2017) Neuromuscular contributions to the age-related reduction in muscle power: mechanisms and potential role of high velocity power training. Ageing Res Rev 35:147–154
Papa EV, Dong X, Hassan M (2017) Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review. Clin Interv Aging 12:955–961
Straight CR, Lindheimer JB, Brady AO et al (2016) Effects of resistance training on lower-extremity muscle power in middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med 46:353–364
Bauman A, Merom D, Bull FC et al (2016) Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote “Active Aging”. Gerontologist 56:S268–S280
Cadore EL, Rodriguez-Manãs L, Sinclair A et al (2013) Effects of different exercise interventions on risk of falls, gait ability and balance in physically frail older adults. A systematic review. Rejuvenation Res 16:105–114
De Labra C, Guimaraes-Pinheiro C, Maseda A et al (2015) Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr 15:154. doi:10.1186/s12877-015-0155-4
Izquierdo M, Cadore EL (2014) Muscle power training in the institutionalized frail: a new approach to counteracting functional declines and very late life disability. Cur Med Res Opin 30:1385–1390
Valenzuela T (2012) Efficacy of progressive resistance training interventions in older adults in nursing homes: a systematic review. J Am Med Dir Assoc 13:418–428
Kemmler W, Haberle L, von Stengel S (2013) Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos Int 24:1937–1950
Yang Z, Scott CA, Mao C et al (2014) Resistance exercise versus aerobic exercise for type 2 diabetes: a systematic review and meta-analysis. Sports Med 44:487–499
Chung C, Thilarajah S, Tan D (2016) Effectiveness of resistance training on muscle strength and physical function in people with parkinson’s dsease: a systematic review and meta-analysis. Clin Rehabil 30:11–23
Gates N, Fiatarone Singh MA, Sachdev PS et al (2013) The effect of exercise training on cognitive function in older adults with mild cognitive impairment: a meta-analysis of randomized controlled trials. Am J Geriatr Psychiatry 21:1086–1097
Borde R, Hortobagyi T, Granacher U (2015) Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med 45:1693–1720
Raymond MJ, Bramley-Tzerefos RE, Jeffs KJ et al (2013) Systematic review of high-intensity progressive resistance strength training of the lower limb compared with other intensities of strength training in older adults. Arch Phys Med Rehabil 94:1458–1472
Steib S, Schoene D, Pfeifer K (2010) Dose-response relationship of resistance training in older adults: a meta-analysis. Med Sci Sport Exerc 42:902–914
Gordon BA, Benson AC, Bird SR et al (2009) Resistance training improves metabolic health in type 2 diabetes: a systematic review. Diabetes Res Clin Pract 83:157–175
Baum EE, Jarjoura D, Polen AE et al (2003) Effectiveness of a group exercise program in a long-term care facility: a randomized pilot trial. J Am Med Dir Assoc 4:74–80
Giné-Garriga M, Guerra M, Unnithan VB (2013) The effect of functional circuit training on self-reported fear of falling and health status in a group of physically frail older individuals: a randomized controlled trial. Aging Clin Exp Res 25:329–336
Kim H, Suzuki T, Kim M et al (2015) Effects of exercise and milk fat globule membrane (MFGM) supplementation on body composition, physical function, and hematological parameters in community-dwelling frail Japanese women: a randomized double blind, placebo-controlled, follow-up trial. PLoS One 10(2) doi:10.1371/journal.pone.0116256
Venturelli M, Lanza M, Muti E et al (2010) Positive effects of physical training in activity of daily living-dependent older adults. Exp Aging Res 36:190–205
Binder EF, Yarasheski KE, Steger-May K et al (2005) Effects of progressive resistance training on body composition in frail older adults: results of a randomized, controlled trial. J Gerontol A Biol Sci Med Sci 60:1425–1431
Cadore EL, Casas-Herrero A, Zambom-Ferraresi F et al (2014) Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age (Dordr) 36:773–785
Fisher NM, Pensergast DR, Calkins E (1991) Muscle rehabilitation in impaired elderly nursing home residents. Arch Phys Med Rehabil 72:181–185
Sullivan DH, Wall PT, Bariola JR et al (2001) Progressive resistance muscle strength training of hospitalized frail elderly. Am J Phys Med Rehabil 80:503–509
Campos GE, Luecke TJ, Wendeln HK et al (2002) Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol 88:50–60
Augustsson J, Esko A, Thomee R et al (1998) Weight training of the thigh muscles using closed vs. open kinetic chain exercises: a comparison of performance enhancement. J Orthop Sports Phys Ther 27:3–8
Brill PA, Probst JC, Greenhouse DL et al (1998) Clinical feasibility of a free-weight strength-training program for older adults. J Am Board Fam Pract 11:445–451
Schott N, Knobl O (2004) The effects of free weights training for older adults. J Aging Phys Act 12:413–414
Schulz KF, Altman DG, Moher D et al (2011) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 9:672–677
van Tulder M, Furlan A, Bombardier C et al (2003) Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 28:1290–1299
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Rikli R, Jones J (2001) Senior fitness test. Human Kinetics, Champaign
Watson MJ (2002) Refining the ten-meter walking test for use with neurologically impaired people. Physiotherapy 88:386–397
Bennell K, Dobson F, Hinman R (2011) Measures of physical performance assessments. Arthritis Care Res 63:S350-S370
Roberts HC, Syddall H, Sparkes J et al (2014) Grip strength and its determinants among older people in different healthcare settings. Age Ageing 43:241–246
Udsching P, Udsching B, Schütze B et al (2010) SGB XI: soziale Pflegeversicherung; Kommentar. Beck, München
Rhea MR (2004) Determining the magnitude of treatment effects in the strength training research through the use of the effect size. J Strength Cond Res 18:918–920
Nyman SR, Victor CR (2011) Older people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic review. Age Ageing 40:430–436
Bossers WJ, Scherder E, Boersma F et al (2014) Feasibility of a combined aerobic and strength training program and its effects on cognitive and physical function in institutionalized dementia patients. A pilot study. PLoS One 9:e2018. doi:10.1371/journal.pone.0097577
Fiatarone MA, Marks EC, Ryan ND et al (1990) High intensity-strength training in nonagenarians. JAMA 263:3029–3034
Krist L, Dimeo F, Keil T (2013) Can progressive resistance training twice a week improve mobility, muscle strength, and quality of life in very elderly nursing-home residents with impaired mobility? A pilot study. Clin Interv Aging 8:443–448
McMurdo ME, Rennie LM (1993) A controlled trial of exercise by residents of old people’s homes. Age Ageing 22:11–15
Sauvage LR, Myklebust BM, Crow-Pan J et al (1992) A clinical trial of strengthening and aerobic exercise to improve gait and balance in elderly male nursing home residents. Am J Phys Med Rehabil 71:333–342
Machacova K, Vankova H, Volicer L et al (2015) Dance as prevention of late life functional decline among nursing home residents. J App Gerontol. doi:10.1177/0733464815602111
Fien S, Henwood T, Climstein M et al (2016) Feasibility and benefits of group-based exercise in residential aged care adults: a pilot study for the GrACE programme. PeerJ 4:e2018. doi:10.7717/peerj.2018
Bean JF, Kiely DK, LaRose S et al (2010) Are changes in leg power responsible for clinically meaningful improvements in mobility in older adults? J Am Geriatr Soc 58:2363–2368
González-Colaço Harmand M, Meillon C, Rullier L et al (2014) Cognitive decline after entering a nursing home: a 22-year follow-up study of institutionalized and noninstitutionalized elderly people. J Am Med Dir Assoc 15:504–508
Acknowledgements
The authors would like to acknowledge Boris Troll for his assistance with the supervision of the participants. Furthermore, we would like to thank the residents of the nursing home for their assistance and participation in this project.
Author information
Authors and Affiliations
Contributions
BJ and NS contributed to the conception and the design of the experiment. Both authors analyzed and interpreted the data and prepared the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the author(s) or on any organization with which the author(s) is/are associated.
Rights and permissions
About this article
Cite this article
Johnen, B., Schott, N. Feasibility of a machine vs free weight strength training program and its effects on physical performance in nursing home residents: a pilot study. Aging Clin Exp Res 30, 819–828 (2018). https://doi.org/10.1007/s40520-017-0830-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0830-8