Abstract
Purpose of Review
Emotion regulation and the manner in which it is comprised play a key role in the motivation for drugs and alcohol. As such, the bio-behavioral processes underpinning aspects of emotion regulation behavior may provide expedient targets for treatment development. This review will examine some of the robust emotional, psychophysiological, and neurobiological adaptations that sub-serve affect regulation behaviors during early abstinence from addiction and assess their potential as targets for treatment development.
Recent Findings
During early abstinence from addiction, individuals report problems with emotional awareness and impulse control during distress as well as enhanced, persistent negative mood in the face of acute psychological stress. In line with this, psychophysiological research studies have used non-affective indices of emotional awareness to show poor interoceptive accuracy. Moreover, imaging research has highlighted hypofunctional prefrontal circuitry in regulatory brain regions and amygdala/insula adaptations that are also compatible with decrements in emotional awareness, enhanced provoked dysphoria and decreased impulse control. There is also some evidence to suggest that targeting these indices of emotion regulation behavior using mindfulness-based meditation and medication therapies may be effective in improving outcome.
Conclusions
The biological construct of emotion regulation has helped to provide an important heuristic framework within which to develop novel treatment markers. However, there remains a need for more contextual and situational-based research to achieve a more holistic understanding of emotion regulation for improved clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Substance use disorders affect approximately 20 million people in the USA and may result in devastating consequences, with drug overdose leading to over 70,000 deaths in the USA in 2017 [1]. A key concept necessary for both clinicians and researchers to understand is what underlies the chronic, relapsing nature of the illness. Burgeoning research indicates that emotion regulation and the manner in which it is compromised may play a key role in the initiation, maintenance, and outcome of addictive disorders. As such, emotion regulation and the bio-behavioral processes underpinning emotion regulation may provide vital predictors of relapse vulnerability, and, hence, expedient targets for therapeutic development.
Common definitions of emotion regulation relate to the way in which humans control their experience and expression of emotion under distress by employing strategies such as suppression, repression, and cognitive reappraisal [2]. Notably, these strategies are psychologically effortful and, during highly charged or stressful situations, may induce a conflict in regulatory goals, shifting attention towards more immediate and often pleasure-seeking goals [3,4,5]. This conflict may in turn jeopardize volitional behavior through loss of impulse control [6] and is highly pertinent to processes underlying compulsive drug use and alcohol-seeking behavior. For example, motivation for drugs and alcohol at various stages of the addiction cycle are impacted by aspects of emotion regulation which include sensitization of the core stress systems of the brain [7, 8], difficulty engaging in regulatory brain systems (behavioral inhibition), and the interaction of these processes in order to appropriately manage affective and dysphoric states prevalent during early and protracted withdrawal [9,10,11]. In addition to this, individual differences in positive and negative urgency [12], the many facets of impulsivity [13,14,15,16] and emotional awareness [17], may play a further role in mediating these processes.
In light of this, the most comprehensive measure of emotion regulation to date is the Difficulties in Emotion Regulation Scale (DERS) [18] which was developed in order to consolidate and integrate these complexities and present emotion regulation as a higher-order construct. Within this model, lower-order constructs were identified which broadly included emotional awareness, emotional expression, and control of emotion (impulse control) under stressful circumstances, which were shown to effectively discriminate between addicted populations and controls [19, 20]. As such, the scientific construct of emotion regulation as applied to addiction research has tended to broadly emphasize the sensitization and managing of mood states and their inherent role as motivators or regulators [19,20,21,22], awareness of emotion, and the independent ability to regulate both cognitively and emotionally.
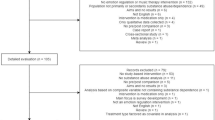
Increasingly, emotion regulation is being seen as having tremendous heuristic value in substance use prevention [23] highlighting the importance of elucidating bio-behavioral indices of emotion regulation as valid targets for treatment intervention. In the current review, we therefore examine studies that have helped to characterize some of the subjective, psychophysiological, and neurobiological indices of emotion regulation and related behaviors during early abstinence from addiction. We also assess whether these bio-behavioral markers reflect effective measures of clinical outcome and hence represent viable targets for treatment development. In addition we highlight the need for a more holistic understanding of emotion regulation in order to fully leverage the potential of emotion regulation as a personalized construct with optimal clinical application.
Subjective Indices of Emotion Regulation
Findings from several studies suggest that emotion (dys)regulation effects outcome in substance users due to coping-related issues. For example, the global construct of emotion regulation in the DERS has been shown to be associated solely with coping-oriented motivations for use in cannabis users, rather than other motives including sociability [24]. Similarly these findings have been supported by more recent studies showing the same global index of the DERS to be associated with coping motives for opioid use in methadone-maintained individuals [25]. As such, with regard to assessing subjective emotion regulation and emotion regulation-related behaviors during early abstinence, we focus predominantly on research that has either administered the DERS, which explores the construct in the context of distress or examines subjective affect in response to psychological stress.
Sensitization of negative emotion during stress
One of the major aspects of emotion regulation is the ability to successfully manage or cope with affective processes which, during early abstinence from addiction, may be hampered by the sensitization of negative emotions brought about by allostatic adaptions within core neural stress systems [26, 27]. Several studies measuring subjective and emotional response to a 5-min personalized psychological stressor have shown that sensitized stress, anxiety, anger, sadness, and fear are reported by early abstinent alcohol-dependent individuals [20, 21, 28], cocaine-dependent individuals [29, 30], comorbid cocaine and alcohol-dependent individuals [26], and opioid-dependent individuals compared with controls. Furthermore, these studies have also highlighted the temporal persistence of this dysphoric state, where, compared with controls, individuals in early abstinence from alcohol and cocaine remain significantly dysphoric for up to 1-h post exposure to a 5-min acute stressor [31]. Notably, this persistent dysphoric state has been shown to occur concurrently with increased craving, an attenuated ability to cognitively regulate, and has been prospectively associated with relapse [32, 33].
Emotional awareness and regulation
Two prior studies from our own laboratory using the Difficulties in Emotion Regulation Scale [18] (DERS; Gratz and Roemer, 2004) showed that on admission to inpatient treatment, cocaine-dependent individuals were less able to acknowledge and/or have a clear understanding of their emotions [20]. They also reported significant difficulties with impulse control during stress and with regard to developing effective emotional strategies (i.e. they would be more likely to believe that little could be done to change an emotionally stressful situation). In a subsequent study, alcohol dependent individuals similarly reported significant affective issues on admission to treatment, including poor emotional awareness and impulse control [19]. Notably, while improvements regarding clarity and awareness of emotion were observed following 4 weeks of inpatient treatment and abstinence, both cocaine and alcohol dependent individuals were still reporting difficulties with stress-related impulsive control upon completion of treatment [19, 20]. This is consistent with our studies showing decrements in cognitive control in the face of acute stress following 4 weeks of abstinence [34]. Other studies have additionally highlighted persistent problems with the emotional awareness and understanding constructs of the DERS 1 month from alcohol treatment discharge [35]
Similar findings were observed in a group of cocaine-dependent individuals following 4 weeks of inpatient treatment and abstinence, who were administered the MSCEIT [36, 37]. While a measure of emotional intelligence, the test does comprise measures pertaining to emotional strategizing which include the ability to understand emotional causes and complexities both within themselves and others as well as regulate emotions [38]. Notably, 1 week prior to treatment discharge, cocaine-dependent individuals demonstrated attenuated ability to emotionally strategize, which was also associated with an increase in self-reported impulse control problems [37]. This again is consistent with more recent studies indicating difficulties with both emotional awareness and regulation in individuals with substance use disorder [39] as well as studies that have associated elevations in alcohol-related consequences with similar emotion regulation constructs using the DERS in college students [40] .
Implications for treatment
Current research examining subjective indices of emotion regulation has shown that certain behaviors pertinent to emotion (dys)-regulation including impulse control in the face of stress, an inability to emotionally strategize as well as sensitized negative mood and anxiety, persist 4–5 weeks into protracted abstinence [19,20,21, 41]. Additionally, research demonstrating the role that emotion dysregulation plays in coping-related motivations for drug and alcohol use [24, 25, 42, 43] highlights the importance of assessing provoked emotional sensitization during protracted abstinence as a potential target for relapse prevention. In view of this, studies from our own laboratory that have administered adrenergic agents, such as prazosin and guanfacine, to target sensitized anxiety and negative affect as well as cognitive control processes during stress, have demonstrated some promise with regard to attenuating alcohol, cocaine, and nicotine craving inside the laboratory [44, 45] and relapse outside of the laboratory [46].
Psychophysiological Indices of Emotion Regulation
In the last decade, several studies using heart rate tracking, heart rate sensitivity, and heart rate variability have been used to ascertain interoceptive indices of the internal state and have also been important in characterizing non-affective aspects of emotional awareness in addicted populations. As emotional regulation includes awareness of one’s emotion [2], it is not unreasonable to assume that viscero-afferent feedback or awareness of bodily internal state may provide a non-affective index of emotion regulation [47] during abstinence from addiction. In line with this, impaired interoception may reflect salient motivational processes similar to those associated with relapse, including sensitized anxiety, negative mood, as well as the manifestation of craving [48]. Moreover, the association between interception and ability to understand and regulate emotions has been well established in the literature [49, 50]. As such, psychophysiological markers of interoception may provide easily quantifiable measures of emotion regulation. In support of this, Paulus and Stewart [51] describe how optimal cognitive control of emotion occurs not just as a function of regulatory competence but also in the context of intensity of interoceptive afferents which may be robustly altered during “deprivation” states [52], such as abstinence. One’s ability to identify and access internal sensory cues, or interoceptive changes [53, 54] may therefore be key to characterizing some of the subjective emotion regulation-related experiences that occur during abstinence. In turn, they may also represent implicit markers underlying the relationship between emotion regulation processes and the maintenance or avoidance of substance use during stress.
Heartbeat detection and discrimination
Several experimental and clinical paradigms have been designed to quantify interceptive awareness, including heartbeat tracking and discrimination. For example, interoceptive accuracy using heartbeat perception performance has been shown to be reduced in 2-week abstinent individuals with alcohol use disorder compared with healthy controls. In the same study, accuracy was also negatively associated with levels of self-reported alcohol craving sensations [55]. Poor interoceptive accuracy has also been reported in smokers compared with non-smokers [56], and discrepancy has been observed between high self-reported interoceptive sensibility (tendency to focus on internal bodily sensations) alongside poor interoceptive accuracy in individuals with alcohol use disorder compared with healthy controls [57•]. While these findings are consistent with the previously cited studies identifying self-reported difficulties with emotional awareness during early abstinence from alcohol and cocaine [29, 35], few studies have directly assessed the link between interoceptive accuracy and subjective emotion regulation ability. One recent study by Jakubczyk et al. [57•] did however demonstrate an association between interoception, as measured by the heartbeat tracking Schandry test [58] and the DERS in individuals with alcohol use disorder compared with controls. Findings indicated that high interoceptive accuracy was significantly associated with improved acceptance of negative emotions and high levels of interoceptive sensibility were linked to elevated impulse control difficulties during stress as well as lower emotional awareness [57•]. Findings also support the potential for interoceptive psychophysiological measures to reflect emotional awareness in addicted populations.
Implications for treatment
While there is evidence to show that physiological markers of internal state may be able to provide effective measures of emotional awareness, more research is clearly required to fully comprehend their clinical validity and impact on compulsive drug and alcohol seeking. For example, while some interoception research has highlighted the potential for poor interoceptive (emotional) awareness to represent a risk factor, (possibly via dampened perceptions of intoxication), other studies have presented poor interoception as being protective from craving [59]. In the latter scenario, it is postulated that high interoceptive (emotional) awareness may lead to the greater experience of aversive or craving states associated with withdrawal [60]. Despite this lack of clarity, several studies have highlighted the importance of interoceptive awareness training with regard to relapse prevention and as a means of improving both emotion regulation and treatment outcome in individuals with substance use disorders [61,62,63,64,65]. Teaching interoceptive awareness skills via mindfulness-based approaches during outpatient treatment has also been shown to be well received and lead to improvements in emotion regulation (self-report and psychophysiological indices), abstinence, depressive symptoms, and craving [62, 63].
Heart rate variability
Heart rate variability (HRV) is also thought to be another non-affective physiological index of emotion regulation capacity due to the fact both are sub-served by common overlapping brain circuitry [4, 66, 67]. For example, the Neurovisceral Integrative Model (NIM; [68]) proposes that overlapping subcortical-cortical neural circuitry (ventromedial prefrontal/anterior cingulate and amygdala [69]) is responsible for both adaptive inhibitory function and the regulation of autonomic system reactivity [70]. Hence, vagally mediated HRV may serve to reflect not only cardiovascular health but additionally represent the flexibility of central regulatory processes and the extent to which they are able to exert control over peripheral autonomic activity. In support of this, many studies have shown low resting state HRV and dysregulated phasic HRV in response to emotionally evocative stimuli to be associated with emotion regulation difficulties [71,72,73]. These have included less of an ability to suppress unwanted thoughts [74] as well as greater day to day difficulties with emotional clarity and impulse control [66] in both healthy and clinical populations.
Despite these findings, there remains a dearth of studies exploring these psycho-physiological substrates of emotion regulation in substance abusers [62, 75]. This is surprising given that craving may be associated with low resting HRV [76, 77] and high HRV response to cues. One recent study did however examine the ability of respiratory sinus arrhythmia (RSA; heart rate variability across the respiratory cycle) to predict emotion dysregulation and health outcomes in a sample of women in community outpatient treatment for substance use disorders. Findings indicated that while higher resting RSA was robustly associated with increased interoceptive awareness skills, it did not correlate with substance use or mindfulness skills [62]. In two other studies, blunted HRV during negative emotion regulation was associated with opioid misuse [78] and duration of opioid use in a sample of female opioid-treated chronic pain patients at risk for OUD [76]. Blunted HRV was also linked to negative emotion-induced craving in the same sample of women [76]. Conversely, Claisse et al. [79] found that increased HRV following emotional induction was associated with increased craving in both short- and long-term alcohol abstainers.
Implications for treatment
Further research is clearly required to fully comprehend the clinical validity and reliability of psychophysiological measures, such as HRV. However, there is some evidence to show that inducing high amplitude oscillations in heart rate (or HRV), via resonance breathing, meditative practice, or biofeedback techniques, may strengthen functional connectivity in regions associated with emotion regulation [69]. In particular, improving HRV via resonance breathing has been established as a successful intervention for several disorders with emotion regulation as a key feature [80] and has shown some efficacy in substance use populations. A recent proof of concept study by Bates et al. [81] did find that resonance breathing increased activation in regulatory regions of the brain associated with behavioral control and regulation of cognitive and emotional processing, including the bilateral medial prefrontal, anterior, and posterior cingulate, in a range of drinkers. Several studies have also indicated the potential for HRV biofeedback therapy to reduce stress, anxiety and craving in inpatients with alcohol use disorder, immediately following intervention [82], 1 month later [83] and 1 year later [84].
Neurobiological Indices of Emotion Regulation
Other potential neurobiological indices of emotion (dys)-regulation have included neural and endocrine changes that have been observed during early and protracted abstinence from substance use. In support of research that has highlighted subjective and physiological markers of emotion regulation, adaptations have been observed in central and peripheral systems that are linked to sensitized dysphoric states, attenuated regulatory function, and viscero-affective sensations. While these are wide-ranging neuroendocrine systems that potentially underpin a broad range of goal-oriented behaviors including distraction, decision-making, planning, etc., links have been made between changes within these systems and emotional awareness, elevations in affective sensitivity, and affective dysregulation during stress.
Upregulation of HPA-SAM circuitry
Upregulation of CRF and adrenergic systems may highlight a potential emotion regulation-related mechanism that may be an important target for therapeutic intervention. For example, overactive hypothalamic CRH [85, 86] as well as elevations in peripheral adrenal sensitivity (cortisol/ACTH ratios), centrally recruited dynorphin, NE [21, 31, 87], noradrenergic signaling [88, 89], and upregulated NE-CRF feed-forward loops [90] have consistently been observed in early abstinent alcohol and substance abusing individuals and further deemed a risk factor for relapse [91, 92]. Notably, these adaptations have also been known to reflect persistent negative emotional states during early abstinence, as well as anxiety and anxiety disorders [21, 85,86,87]. In addition, elevations in prefrontal norepinephrine are known to impair attentional processes that are key to the stopping and monitoring components of cognitive and affective control [93, 94] by attenuating salient “signals” and increasing irrelevant “noise” [95,96,97]. Notably, adrenergic medications which attenuate sympathetic overdrive, such as prazosin, have been shown to improve emotion regulation-related behaviors. This has included reducing sensitized and persistent anxiety, negative mood, and alcohol craving [98] and improving cognitive regulation [99, 100] during stress.
Hypofunctional prefrontal circuitry
During early abstinence from substance use, changes within the prefrontal cortex have typically been observed where ventromedial and anterior cingulate circuits that support regulatory function become hypofunctional [101, 102]. Notably, recent neuroimaging analysis in individuals with AUD has shown that activation of overlapping prefrontal cognitive control circuits (including the dlPFC, vlPFC and dmPFC) is recruited during a regulation of craving task and an affect regulation (reappraisal) task [103] confirming the intrinsic interconnection between (dys)regulation within cognitive, emotional, and behavioral domains [104].
In view of this, several functional imaging studies have measured prefrontal activity in drug and alcohol users during early abstinence, while performing cognitive control tasks typically interpreted as prototypical indicators of impulse control in many neuropsychiatric conditions including cocaine dependence [105,106,107]. Findings have shown that attenuated activity in regulatory circuits are linked to impulse control aspects of emotion regulation as well as relapse outcomes. For example, Li et al. [108] showed hypo-activation of the rostral anterior cingulate cortex (rACC) during a stop signal task to be linked to elevations in the DERS impulse control scale during early abstinence from cocaine [109]. Decreased error-related activations of the dorsal anterior cingulate cortex and impaired dorsolateral activation [110] during stop signal inhibitory control paradigms have also been associated with a shorter time to relapse and greater alcohol urges, respectively, in early abstinence alcohol-dependent individuals. Similarly, activation of regulatory regions including the ventromedial prefrontal cortex, left posterior cingulate cortex, and right striatum during stroop performance has been shown to predict longer periods of reported abstinence in treatment-seeking cocaine-dependent individuals [111].
Implications for treatment
Notably, targeting these hypofrontal mechanisms, via both medication and behavioral intervention, has had tremendous impact on substance use outcomes, potentially via the improvement of emotion regulation-related behaviors. For example, the Monoamine Transporter Inhibitor modafinil has demonstrated improvement in impulsive decision-making in alcohol-dependent patients by enhanced coupling of prefrontal control regions with ventral striatal regions associated with reward coding [112]. Similarly, the alpha2a adrenergic agonist, guanfacine, has been shown to improve cognitive control processes [44] and increase regional blood flow in regulatory ventromedial circuits of the PFC during acute stress in comorbid substance users during early abstinence [45]. In the same sample of individuals, guanfacine was also shown to attenuate sensitized and persistent negative mood, anxiety, and craving for cocaine, alcohol, and nicotine following acute stress exposure [113]. With regard to behavioral therapies, the success of many mindfulness-based interventions has also been attributed to the strengthening of prefrontally mediated cognitive control circuitry [114], as well as improving both interoception and emotion regulation [115]. For example, one study showed that improvement of self-control abilities in emotion regulation and stress reduction was associated with elevated ACC/mPFC activity following mindfulness training in smokers with alcohol use disorder [116•].
Amygdala/insular hyperactivation
The insular cortex is thought to be the “hub” for interoceptive processing [51] receiving sensory and interoceptive afferents from outside and inside of the body, respectively, and reciprocal connections from the amygdala and extended amygdala as well as regulatory regions of the PFC [117]. Indeed, extensive studies within a wide range of substance users have shown dysregulated insula activation to occur during exposure to drug cue, reward, and stress and, as a function of abstinence, severity of use as well as craving [59, 60]. Taken together, there is some agreement that insular activity is attenuated during cognitive control and decision-making tasks [118,119,120,121] as well as longer periods of abstinence [122], while hyperactive during reward-related processes such as cue exposure [123]. There is also some evidence to show that these adaptations are associated with craving and relapse in smokers [124], amphetamine-dependent individuals [118], and cocaine-dependent individuals [125, 126]. While the insular processes a complex interchange of environmental and internal stimuli, its role in interoceptive processing, emotional awareness and craving is relatively well established [65]. Furthermore, there is also burgeoning evidence to suggest that it may be a possible therapeutic focus for the reduction of craving in mindfulness-based interventions [51] and transcranial magnetic stimulation [127, 128].
Similarly, the amygdala is intrinsic to emotional processing and emotional intensity [129, 130], and several studies have highlighted the role of increased D2 reactivity in the amygdala with negative affect. A recent PET study using the radiotracer [18F], fallypride, also indicted how increased signaling through D2-type receptors within the amygdala may play a pivotal role in the cognitive control of negative emotions, measured using the DERS, in both healthy controls and methamphetamine users [131].
Future Directions
While many of these studies have served to highlight some of the bio-behavioral indices of emotion regulation as well as the potential for these adaptations to represent possible treatment targets, the clinical application of standardized emotion regulation approaches in the development of treatment and prevention programs remains somewhat lacking [75]. To date, only one study has assessed the efficacy of an Affect Regulation Training (ART) treatment on outcome in individuals with alcohol use disorder, despite emotion regulation processes mediating the efficacy of several behavioral therapies on abstinence maintenance [132, 133] and despite it being considered a core clinical dimension in substance use treatment [133, 134]. One reason for this may be related to the fact that much of the emotion regulation research to date has broadly been applicable to the individual-based models of addiction, rather than social or situational models.
For example, Simon and West [135] postulate that the core elements of both individual and social models of addiction include variation pertaining to the “capability” (psychological or physical), “motivation” (reflective or automated internal processes), and “opportunity” (physical and social environmental factors) to engage in addictive behavior. As shown in the current review, much research to date has predominantly targeted the capability and motivational aspects of addiction, where a range of bio-behavioral assessments have been made regarding changes in individual capacity for emotional awareness, motivation, regulation strategies, and control of behavioral impulses. However, in terms of a more holistic understanding of emotion regulation, there is a need to determine how “opportunity”-related social and situational factors may effect emotion regulation processes and interact with individual indices of emotion regulation pertaining to capacity (strategies, awareness) and motivation (craving, sensitized negative mood).
In support of this, several theoretical models interpret effective emotion regulation as an interplay between individual-strategy-situational patterns [136,137,138,139] and the ability to utilize flexible emotion regulation strategies within changing situational contexts. Despite this, the emphasis on shifting contextual factors and within person assessment has not been adequately examined. While several studies have assessed the effects of acute stress on emotion regulation processes [29, 34, 140] and have indicated that selective improvements occur during treatment [29, 140],there remains a dearth of information regarding the longevity of such improvements following treatment discharge, as well as changes in emotion (dys) regulation over time and within certain (social and physical) environments. In terms of between-person variation, how cultural, societal, and dispositional differences contribute to these processes also needs to be considered [139]. A recent study by Bradizza et al. [141], for example, reported that emotion dysregulation problems (as measured by the DERS) were only observed in AUD individuals with at least two or more co-occurring disorders, providing salient information for the development of more targeted therapies.
From a similar perspective, Roos and Witkiewitz [142••] suggest that the slow progress in understanding “self-regulation” as a mechanism of behavioral change (MOBC) in addiction therapies may be due to a lack of focus on context. They additionally propose a contextual model where self-regulation as a MOBC is dependent upon both immediate ever-changing situational context (internal state and external cues) and a less changeable broader context (disposition, environment, major life events). Moreover, in support of similar theoretical models of emotion regulation [136, 138], they also proposed that assessing these contextual perspectives can be facilitated by studying both between and within participant adaptations using concentrated longitudinal measurements, such as ecological momentary assessment (EMA) [142••].
Conclusions
Taken together, research has shown that early abstinence from addiction is characterized by robust emotional, physiological, and neurobiological adaptations that sub-serve aspects of emotion regulation behavior. These predominantly include tonic cardiovascular dysregulaton, overactivity of CRH, and locus coeruleus–norepinephrine (LC–NE) circuits, hypofrontality within prefrontal regulatory brain regions (including the ventromedial PFC and anterior cingulate (ACC)), and amygdala/insula adaptations. Notably, extensive research has shown that addiction-related changes within these systems are linked to poor emotional awareness, enhanced provoked dysphoria, and decreased impulse control in the face of stress [143,144,145]. In addition, this body of research has provided an excellent heuristic framework within which to develop effective treatment markers, with the potential to be targeted by a range of medication and behavioral relapse interventions, including mindfulness meditation and medications therapies. In particular, adrenergic medications such as guanfacine and prazosin, as well as partial nicotinic agonists, such as varenacline, have improved clinical outcomes by targeting prefrontal and amygdala-insula indices of emotion regulation, respectively [45, 146,147,148,149]. Similarly, psychophysiological measures of heart beat detection and HRV could potentially represent easily modifiable measures of improved interoception, emotional awareness, emotion regulation, and abstinence, following mindfulness-based therapies and during resonance breathing techniques. While these findings are encouraging, our current understanding of emotion regulation processes may still be constrained by a dearth of context and situational-based research paradigms, and more longitudinal research is warranted in order to achieve a more holistic understanding of emotion regulation for improved clinical application.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(8):807–16.
Gross JJ, John OP. Wise emotion regulation. 2002.
Tice DM, Bratslavsky E, Baumeister RF. Emotional distress regulation takes precedence over impulse control: If you feel bad, do it! J Pers Soc Psychol. 2001;80(1):53.
Thayer JF, Åhs F, Fredrikson M, Sollers JJ III, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36(2):747–56.
Lane AM, Beedie CJ, Jones MV, Uphill M, Devonport TJ. The BASES expert statement on emotion regulation in sport. J Sports Sci. 2012;30(11):1189–95.
Kuhl J. Action versus state orientation: psychometric properties of the action control scale (ACS-90). Volition Personal: Action Versus State Orient. 1994;47:56.
Wichers M, Barge-Schaapveld D, Nicolson N, Peeters F, De Vries M, Mengelers R, et al. Reduced stress-sensitivity or increased reward experience: the psychological mechanism of response to antidepressant medication. Neuropsychopharmacology. 2009;34(4):923–31.
Stansbury K, Gunnar MR. Adrenocortical activity and emotion regulation. Monogr Soc Res Child Dev. 1994;59(2–3):108–34.
Koob GF, Le Moal M. Addiction and the brain antireward system. Annu Rev Psychol. 2008;59:29–53.
Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363–71.
Tomarkenand JA, Keener AD. Frontal brain asymmetry and depression: a self-regulatory perspective. Cognit Emot. 1998;12(3):387–420.
Smith GT, Cyders MA. Integrating affect and impulsivity: the role of positive and negative urgency in substance use risk. Drug Alcohol Depend. 2016;163:S3–S12.
Herman AM, Critchley HD, Duka T. The impact of Yohimbine-induced arousal on facets of behavioural impulsivity. Psychopharmacology. 2019;236(6):1783–95.
Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146(4):348–61.
Caswell AJ, Bond R, Duka T, Morgan MJ. Further evidence of the heterogeneous nature of impulsivity. Personal Individ Differ. 2015;76:68–74.
Jentsch JD, Ashenhurst JR, Cervantes MC, James AS, Groman SM, Pennington ZT. Dissecting impulsivity and its relationships to drug addictions. Ann N Y Acad Sci. 2014;1327:1.
Pivarunas B, Conner BT. Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14.
Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of sthe difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
Fox H, Hong K, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. 2008;33(2):388–94.
Fox H, Axelrod S, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007;89(2–3):298–301.
Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM. Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology. 2009;34(5):1198–208.
Herman AM, Critchley HD, Duka T. Risk-taking and impulsivity: the role of mood states and interoception. Front Psychol. 2018;9:1625.
Berking M, Wupperman P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry. 2012;25(2):128–34.
Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: association with coping-oriented marijuana use motives among current marijuana users. Subst Use Misuse. 2008;43(11):1653–65.
Gold AK, Stathopoulou G, Otto MW. Emotion regulation and motives for illicit drug use in opioid-dependent patients. Cogn Behav Ther. 2020;49(1):74–80.
Fox HC, Jackson ED, Sinha R. Elevated cortisol and learning and memory deficits in cocaine dependent individuals: relationship to relapse outcomes. Psychoneuroendocrinology. 2009;34(8):1198–207.
Koob GF, Schulkin J. Addiction and stress: an allostatic view. Neurosci Biobehav Rev. 2019;106:245–62.
Breese GR, Sinha R, Heilig M. Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse. Pharmacol Ther. 2011;129(2):149–71.
Fox HC, Hong K-IA, Siedlarz K, Sinha R. Enhanced sensitivity to stress and drug/alcohol craving in abstinent cocaine-dependent individuals compared to social drinkers. Neuropsychopharmacology. 2008;33(4):796–805.
Back SE, Brady KT, Jackson JL, Salstrom S, Zinzow H. Gender differences in stress reactivity among cocaine-dependent individuals. Psychopharmacology. 2005;180(1):169–76.
Fox HC, Talih M, Malison R, Anderson GM, Kreek MJ, Sinha R. Frequency of recent cocaine and alcohol use affects drug craving and associated responses to stress and drug-related cues. Psychoneuroendocrinology. 2005;30(9):880–91.
Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Arch Gen Psychiatry. 2006;63(3):324–31.
Weiss F. Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharmacol. 2005;5(1):9–19.
Sinha R. Modeling stress and drug craving in the laboratory: implications for addiction treatment development. Addict Biol. 2009;14(1):84–98.
Ottonello M, Fiabane E, Pistarini C, Spigno P, Torselli E. Difficulties in emotion regulation during rehabilitation for alcohol addiction: correlations with metacognitive beliefs about alcohol use and relapse risk. Neuropsychiatr Dis Treat. 2019;15:2917–25.
Mayer JD, Salovey P, Caruso DR, Sitarenios G. Measuring emotional intelligence with the MSCEIT V2. 0. Emotion. 2003;3(1):97.
Fox HC, Bergquist KL, Gu P, Sinha R. Interactive effects of cumulative stress and impulsivity on alcohol consumption. Alcohol Clin Exp Res. 2010;34(8):1376–85.
Fox HC, Bergquist KL, Casey J, Hong KA, Sinha R. Selective cocaine-related difficulties in emotional intelligence: relationship to stress and impulse control. Am J Addict. 2011;20(2):151–60.
Dingle GA, Neves DC, Alhadad SS, Hides L. Individual and interpersonal emotion regulation among adults with substance use disorders and matched controls. Br J Clin Psychol. 2018;57(2):186–202.
Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, Williams TJ. Alcohol use and alcohol-related consequences: associations with emotion regulation difficulties. Am J Drug Alcohol Abuse. 2014;40(2):125–30.
Sinha R, Fox HC, Hong K-iA, Hansen J, Tuit K, Kreek MJ. Effects of adrenal sensitivity, stress-and cue-induced craving, and anxiety on subsequent alcohol relapse and treatment outcomes. Arch Gen Psychiatry. 2011;68(9):942–52.
Chandley RB, Luebbe AM, Messman-Moore TL, Ward RM. Anxiety sensitivity, coping motives, emotion dysregulation, and alcohol-related outcomes in college women: a moderated-mediation model. J Stud Alcohol Drugs. 2014;75(1):83–92.
Simons RM, Hahn AM, Simons JS, Murase H. Emotion dysregulation and peer drinking norms uniquely predict alcohol-related problems via motives. Drug Alcohol Depend. 2017;177:54–8.
Fox H, Sofuoglu M, Sinha R. Guanfacine enhances inhibitory control and attentional shifting in early abstinent cocaine-dependent individuals. J Psychopharmacol. 2015;29(3):312–23.
Fox HC, Anderson GM, Tuit K, Hansen J, Kimmerling A, Siedlarz KM, et al. Prazosin effects on stress-and cue-induced craving and stress response in alcohol-dependent individuals: preliminary findings. Alcohol Clin Exp Res. 2012;36(2):351–60.
Smith RJ, Aston-Jones G. α2 adrenergic and imidazoline receptor agonists prevent cue-induced cocaine seeking. Biol Psychiatry. 2011;70(8):712–9.
Füstös J, Gramann K, Herbert BM, Pollatos O. On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Soc Cogn Affect Neurosci. 2013;8(8):911–7.
Gray MA, Critchley HD. Interoceptive basis to craving. Neuron. 2007;54(2):183–6.
Kever A, Pollatos O, Vermeulen N, Grynberg D. Interoceptive sensitivity facilitates both antecedent-and response-focused emotion regulation strategies. Personal Individ Differ. 2015;87:20–3.
Damasio AR. Descartes’ error: emotion, rationality and the human brain. 1994.
Paulus MP, Stewart JL, Haase L. Treatment approaches for interoceptive dysfunctions in drug addiction. Front Psychiatry. 2013;4:137.
Schulz A, Vögele C. Interoception and stress. Front Psychol. 2015;6:993.
McGlone F, Wessberg J, Olausson H. Discriminative and affective touch: sensing and feeling. Neuron. 2014;82(4):737–55.
Craig A. Significance of the insula for the evolution of human awareness of feelings from the body. Ann N Y Acad Sci. 2011;1225(1):72–82.
ÇÖL IA, SÖNMEZ MB, Vardar ME. Evaluation of interoceptive awareness in alcohol-addicted patients. Nöro Psikiyatri Arşivi. 2016;53(1):17.
Hina F, Aspell JE. Altered interoceptive processing in smokers: evidence from the heartbeat tracking task. Int J Psychophysiol. 2019;142:10–6.
• Jakubczyk A, Trucco EM, Klimkiewicz A, Skrzeszewski J, Suszek H, Zaorska J, Nowakowska M, Michalska A, Wojnar M, Kopera M. Association between Interoception and emotion regulation in individuals with alcohol use disorder front psychiatry 2020. Findings from this paper demonstrate a significant relationship between aspects of emotion regulation (as measured by the DERS) and interoceptive accuracy (as measured by heartbeat tracking).
Schandry R. Heart beat perception and emotional experience. Psychophysiology. 1981;18(4):483–8.
Naqvi NH, Rudrauf D, Damasio H, Bechara A. Damage to the insula disrupts addiction to cigarette smoking. Science. 2007;315(5811):531–4.
Verdejo-Garcia A, Clark L, Dunn BD. The role of interoception in addiction: a critical review. Neurosci Biobehav Rev. 2012;36(8):1857–69.
Morissette SB, Tull MT, Gulliver SB, Kamholz BW, Zimering RT. Anxiety, anxiety disorders, tobacco use, and nicotine: a critical review of interrelationships. Psychol Bull. 2007;133(2):245–72.
Price CJ, Thompson EA, Crowell SE, Pike K, Cheng SC, Parent S, et al. Immediate effects of interoceptive awareness training through mindful awareness in body-oriented therapy (MABT) for women in substance use disorder treatment. Subst Abus. 2019;40(1):102–15.
Price C, Smith-DiJulio K. Interoceptive awareness is important for relapse prevention: perceptions of women who received mindful body awareness in substance use disorder treatment. J Addict Nurs. 2016;27(1):32–8.
Noël X, Brevers D, Bechara A. A neurocognitive approach to understanding the neurobiology of addiction. Curr Opin Neurobiol. 2013;23(4):632–8.
Paulus MP, Stewart JL. Interoception and drug addiction. Neuropharmacology. 2014;76:342–50.
Williams DP, Cash C, Rankin C, Bernardi A, Koenig J, Thayer JF. Resting heart rate variability predicts self-reported difficulties in emotion regulation: a focus on different facets of emotion regulation. Front Psychol. 2015;6:261.
Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol. 2015;98(2):338–50.
Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–16.
Mather M, Thayer JF. How heart rate variability affects emotion regulation brain networks. Curr Opin Behav Sci. 2018;19:98–104.
Hansen AL, Johnsen BH, Sollers JJ, Stenvik K, Thayer JF. Heart rate variability and its relation to prefrontal cognitive function: the effects of training and detraining. Eur J Appl Physiol. 2004;93(3):263–72.
Tull MT, Gratz KL, Latzman RD, Kimbrel NA, Lejuez C. Reinforcement sensitivity theory and emotion regulation difficulties: a multimodal investigation. Personal Individ Differ. 2010;49(8):989–94.
Geisler FC, Vennewald N, Kubiak T, Weber H. The impact of heart rate variability on subjective well-being is mediated by emotion regulation. Personal Individ Differ. 2010;49(7):723–8.
Aldao A, Mennin DS. Paradoxical cardiovascular effects of implementing adaptive emotion regulation strategies in generalized anxiety disorder. Behav Res Ther. 2012;50(2):122–30.
Gillie BL, Thayer JF. Individual differences in resting heart rate variability and cognitive control in posttraumatic stress disorder. Front Psychol. 2014;5:758.
Kelly TH, Bardo MT. Emotion regulation and drug abuse: implications for prevention and treatment. Drug Alcohol Depend. 2016;163:S1–2.
Garland EL, Reese SE, Bedford CE, Baker AK. Adverse childhood experiences predict autonomic indices of emotion dysregulation and negative emotional cue-elicited craving among female opioid-treated chronic pain patients. Dev Psychopathol. 2019;31(3):1101–10.
Quintana DS, Guastella AJ, McGregor IS, Hickie IB, Kemp AH. Heart rate variability predicts alcohol craving in alcohol dependent outpatients: further evidence for HRV as a psychophysiological marker of self-regulation. Drug Alcohol Depend. 2013;132(1–2):395–8.
Garland EL, Bryan CJ, Nakamura Y, Froeliger B, Howard MO. Deficits in autonomic indices of emotion regulation and reward processing associated with prescription opioid use and misuse. Psychopharmacology. 2017;234(4):621–9.
Claisse C, Cottencin O, Ott L, Berna G, Danel T, Nandrino J-L. Heart rate variability changes and emotion regulation abilities in short-and long-term abstinent alcoholic individuals. Drug Alcohol Depend. 2017;175:237–45.
Hassett AL, Radvanski DC, Vaschillo EG, Vaschillo B, Sigal LH, Karavidas MK, et al. A pilot study of the efficacy of heart rate variability (HRV) biofeedback in patients with fibromyalgia. Appl Psychophysiol Biofeedback. 2007;32(1):1–10.
Bates ME, Lesnewich LM, Helton SG, Gohel S, Buckman JF. Resonance paced breathing alters neural response to visual cues: proof-of-concept for a neuroscience informed adjunct to addiction treatments. Front Psychiatry. 2019;10:624.
Penzlin A, Siepmann M. Herzratenvariabilitäts (HRV)-gestütztes Biofeedbacktraining reduziert Trinkverlangen (Craving) und Angst bei alkoholabhängigen Patienten. Suchttherapie. 2015;16(S 01):S_46_01.
Teeravisutkul P, Chumchua V, Saengcharnchai P, Leelahanaj T. Stress and craving reduction under treatment with heart rate variability biofeedback and the Phramongkutklao model among patients with alcohol use disorder. Psychol Res Behav Manag. 2019;12:619–27.
Penzlin AI, Barlinn K, Illigens BM-W, Weidner K, Siepmann M, Siepmann T. Effect of short-term heart rate variability biofeedback on long-term abstinence in alcohol dependent patients–a one-year follow-up. BMC Psychiatry. 2017;17(1):325.
Fox HC, Sinha R. Sex differences in drug-related stress-system changes: implications for treatment in substance-abusing women. Harvard Rev Psychiatry. 2009;17(2):103–19.
Sher L. Combined dexamethasone suppression-corticotropin-releasing hormone stimulation test in studies of depression, alcoholism, and suicidal behavior. TheScientificWorldJournal. 2006;6:1398–404.
Ehrenreich H, Schuck J, Stender N, Pilz J, Gefeller O, Schilling L, et al. Endocrine and hemodynamic effects of stress versus systemic CRF in alcoholics during early and medium term abstinence. Alcohol Clin Exp Res. 1997;21(7):1285–93.
Smith RJ, Aston-Jones G. Noradrenergic transmission in the extended amygdala: role in increased drug-seeking and relapse during protracted drug abstinence. Brain Struct Funct. 2008;213(1–2):43–61.
Fitzgerald PJ. Elevated norepinephrine may be a unifying etiological factor in the abuse of a broad range of substances: alcohol, nicotine, marijuana, heroin, cocaine, and caffeine. Subst Abuse : Res Treatm. 2013;7:171–83.
Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatr. 2007;164(8):1149–59.
Koob GF. Alcoholism, corticotropin-releasing factor, and molecular genetic allostasis. Biol Psychiatry. 2008;63(2):137–8.
Koob GF. Neurobiological substrates for the dark side of compulsivity in addiction. Neuropharmacology. 2009;56(Suppl 1):18–31.
Aston-Jones G, Gold JI. How we say no: norepinephrine, inferior frontal gyrus, and response inhibition. Biol Psychiatry. 2009;65(7):548–9.
Aston-Jones G, Cohen JD. An integrative theory of locus coeruleus-norepinephrine function: adaptive gain and optimal performance. Annu Rev Neurosci. 2005;28:403–50.
Marek GJ, Aghajanian GK. 5-HT2A receptor or alpha1-adrenoceptor activation induces excitatory postsynaptic currents in layer V pyramidal cells of the medial prefrontal cortex. Eur J Pharmacol. 1999;367(2–3):197–206.
Arnsten AF. Development of the cerebral cortex: XIV. Stress impairs prefrontal cortical function. J Am Acad Child Adolesc Psychiatry. 1999;38(2):220–2.
Birnbaum S, Gobeske KT, Auerbach J, Taylor JR, Arnsten AF. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266–74.
Milivojevic D, Milovanovic SD, Jovanovic M, Svrakic DM, Svrakic NM, Svrakic SM, et al. Temperament and character modify risk of drug addiction and influence choice of drugs. Am J Addict. 2012;21(5):462–7.
Taylor FB, Lowe K, Thompson C, McFall MM, Peskind ER, Kanter ED, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59(7):577–81.
Knauber J, Müller W. Subchronic treatment with prazosin improves passive avoidance learning in aged mice: possible relationships to α 1-receptor up-regulation. J Neural Transm. 2000;107(12):1413–26.
Li C-sR, Sinha R. Inhibitory control and emotional stress regulation: neuroimaging evidence for frontal–limbic dysfunction in psycho-stimulant addiction. Neurosci Biobehav Rev. 2008;32(3):581–97.
Volkow ND. Medications for opioid use disorder: bridging the gap in care. Lancet. 2018;391(10118):285–7.
Suzuki S, Mell MM, O’Malley SS, Krystal JH, Anticevic A, Kober H. Regulation of craving and negative emotion in alcohol use disorder. Biol Psychiatry: Cognit Neurosci Neuroimaging. 2020;5(2):239–50.
Wills TA, Sandy JM, Yaeger AM, Cleary SD, Shinar O. Coping dimensions, life stress, and adolescent substance use: a latent growth analysis. J Abnorm Psychol. 2001;110(2):309–23.
Fillmore MT, Rush CR. Impaired inhibitory control of behavior in chronic cocaine users. Drug Alcohol Depend. 2002;66(3):265–73.
Li C-sR, Milivojevic V, Kemp K, Hong K, Sinha R. Performance monitoring and stop signal inhibition in abstinent patients with cocaine dependence. Drug Alcohol Depend. 2006;85(3):205–12.
Garavan H, Hester R. The role of cognitive control in cocaine dependence. Neuropsychol Rev. 2007;17(3):337–45.
Li C-SR, Kosten TR, Sinha R. Sex differences in brain activation during stress imagery in abstinent cocaine users: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57(5):487–94.
Li C-SR, Yan P, Sinha R, Lee T-W. Subcortical processes of motor response inhibition during a stop signal task. Neuroimage. 2008;41(4):1352–63.
Li CR, Luo X, Yan P, Bergquist K, Sinha R. Altered impulse control in alcohol dependence: neural measures of stop signal performance. Alcohol Clin Exp Res. 2009;33(4):740–50.
Brewer JA, Worhunsky PD, Carroll KM, Rounsaville BJ, Potenza MN. Pretreatment brain activation during stroop task is associated with outcomes in cocaine-dependent patients. Biol Psychiatry. 2008;64(11):998–1004.
Schmaal L, Goudriaan A, Joos L, Dom G, Pattij T, van den Brink W, et al. Neural substrates of impulsive decision making modulated by modafinil in alcohol-dependent patients. Psychol Med. 2014;44(13):2787–98.
Fox HC, Seo D, Tuit K, Hansen J, Kimmerling A, Morgan PT, et al. Guanfacine effects on stress, drug craving and prefrontal activation in cocaine dependent individuals: preliminary findings. J Psychopharmacol. 2012;26(7):958–72.
Garland E, Froeliger B, Howard M. Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Front Psychiatry. 2014;4:173.
Witkiewitz K, Lustyk MKB, Bowen S. Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychol Addict Behav. 2013;27(2):351–65.
• Tang Y-Y, Tang R, Posner MI. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug Alcohol Depend. 2016;163:S13–S8. This study is important in demonstrating that mindfulness training increases activity within the ACC/mPFC, and improves both emotion regulation and stress reduction. It highlights that emotion dysregulation and hypofrontality in smokers may be an important therapeutic target.
Gogolla N. The insular cortex. Curr Biol. 2017;27(12):R580–R6.
Paulus MP, Tapert SF, Schuckit MA. Neural activation patterns of methamphetamine-dependent subjects during decision making predict relapse. Arch Gen Psychiatry. 2005;62(7):761–8.
Kaufman JN, Ross TJ, Stein EA, Garavan H. Cingulate hypoactivity in cocaine users during a GO-NOGO task as revealed by event-related functional magnetic resonance imaging. J Neurosci. 2003;23(21):7839–43.
Nestor LJ, Ghahremani DG, Monterosso J, London ED. Prefrontal hypoactivation during cognitive control in early abstinent methamphetamine-dependent subjects. Psychiatry Res Neuroimaging. 2011;194(3):287–95.
Hester R, Nestor L, Garavan H. Impaired error awareness and anterior cingulate cortex hypoactivity in chronic cannabis users. Neuropsychopharmacology. 2009;34(11):2450–8.
Chiang-shan RL, Luo X, Sinha R, Rounsaville BJ, Carroll KM, Malison RT, et al. Increased error-related thalamic activity during early compared to late cocaine abstinence. Drug Alcohol Depend. 2010;109(1–3):181–9.
Stewart JL, Flagan TM, May AC, Reske M, Simmons AN, Paulus MP. Young adults at risk for stimulant dependence show reward dysfunction during reinforcement-based decision making. Biol Psychiatry. 2013;73(3):235–41.
Janes AC, Pizzagalli DA, Richardt S, Frederick BD, Chuzi S, Pachas G, et al. Brain reactivity to smoking cues prior to smoking cessation predicts ability to maintain tobacco abstinence. Biol Psychiatry. 2010;67(8):722–9.
Garavan H, Pankiewicz J, Bloom A, Cho J-K, Sperry L, Ross TJ, et al. Cue-induced cocaine craving: neuroanatomical specificity for drug users and drug stimuli. Am J Psychiatr. 2000;157(11):1789–98.
Kilts CD, Schweitzer JB, Quinn CK, Gross RE, Faber TL, Muhammad F, et al. Neural activity related to drug craving in cocaine addiction. Arch Gen Psychiatry. 2001;58(4):334–41.
Volkow ND, Boyle M. Neuroscience of addiction: relevance to prevention and treatment. Am J Psychiatr. 2018;175(8):729–40.
Lupi M, Martinotti G, Santacroce R, Cinosi E, Carlucci M, Marini S, et al. Transcranial direct current stimulation in substance use disorders: a systematic review of scientific literature. J ECT. 2017;33(3):203–9.
Garavan H, Pendergrass JC, Ross TJ, Stein EA, Risinger RC. Amygdala response to both positively and negatively valenced stimuli. Neuroreport. 2001;12(12):2779–83.
Frank D, Dewitt M, Hudgens-Haney M, Schaeffer D, Ball B, Schwarz N, et al. Emotion regulation: quantitative meta-analysis of functional activation and deactivation. Neurosci Biobehav Rev. 2014;45:202–11.
Okita K, Ghahremani DG, Payer DE, Robertson CL, Dean AC, Mandelkern MA, et al. Emotion dysregulation and amygdala dopamine D2-type receptor availability in methamphetamine users. Drug Alcohol Depend. 2016;161:163–70.
Maffei C, Cavicchioli M, Movalli M, Cavallaro R, Fossati A. Dialectical behavior therapy skills training in alcohol dependence treatment: findings based on an open trial. Subst Use Misuse. 2018;53(14):2368–85.
Cavicchioli M, Movalli M, Maffei C. Difficulties with emotion regulation, mindfulness, and substance use disorder severity: the mediating role of self-regulation of attention and acceptance attitudes. Am J Drug Alcohol Abuse. 2019;45(1):97–107.
Kober H, Bolling D. Emotion regulation in substance use disorders. Handb Emotion Regul. 2014;2:428–46.
Simon R, West R. Models of addiction and types of interventions: an integrative look. Int J Alcohol Drug Res. 2015;4(1):13–20.
Aldao A, Sheppes G, Gross JJ. Emotion regulation flexibility. Cogn Ther Res. 2015;39(3):263–78.
Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59(1):20–8.
•• Doré BP, Silvers JA, Ochsner KN. Toward a personalized science of emotion regulation. Soc Personal Psychol Compass. 2016;10(4):171–87. This paper is important in highlighting the role of situational factors in the deployment of emotion regulation strategies. The paper proposes a framework to help determine what emotion regulation strategies might be most beneficial for a given person in a given situation.
Kobylińska D, Kusev P. Flexible emotion regulation: how situational demands and individual differences influence the effectiveness of regulatory strategies. Front Psychol. 2019;10:72.
Fox HC, Bergquist KL, Hong KI, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcohol Clin Exp Res. 2007;31(3):395–403.
Bradizza CM, Brown WC, Ruszczyk MU, Dermen KH, Lucke JF, Stasiewicz PR. Difficulties in emotion regulation in treatment-seeking alcoholics with and without co-occurring mood and anxiety disorders. Addict Behav. 2018;80:6–13.
•• Roos CR, Witkiewitz K. A contextual model of self-regulation change mechanisms among individuals with addictive disorders. Clin Psychol Rev. 2017;57:117–28. This paper suggests that an understanding of self-regulation as a MOBC in addiction treatment as been hampered by a lack of attention to contextual factors. A contextual model of self-regulation change mechanisms is proposed pertaining to both immediate and broader contextual factors.
Lijffijt M, Kenemans JL, Verbaten MN, van Engeland H. A meta-analytic review of stopping performance in attention-deficit/hyperactivity disorder: deficient inhibitory motor control? J Abnorm Psychol. 2005;114(2):216–22.
Fishbein DH, Hyde C, Eldreth D, Paschall MJ, Hubal R, Das A, et al. Neurocognitive skills moderate urban male adolescents’ responses to preventive intervention materials. Drug Alcohol Depend. 2006;82(1):47–60.
Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44–79.
Fox HC, Milivojevic V, Blaine S, Sinha R. Stress system sensitivity and emotion regulation in early abstinence from substance use disorders—targets for medications development. Neurobiology of Abnormal Emotion and Motivated Behaviors: Elsevier; 2018. p. 120–41.
McKee LG, Duprey EB, O’Neal CW. Emotion socialization and young adult internalizing symptoms: the roles of mindfulness and emotion regulation. Mindfulness. 2019:1–8.
Arnsten AF, Raskind MA, Taylor FB, Connor DF. The effects of stress exposure on prefrontal cortex: translating basic research into successful treatments for post-traumatic stress disorder. Neurobiol Stress. 2015;1:89–99.
Sutherland MT, Carroll AJ, Salmeron BJ, Ross TJ, Stein EA. Insula’s functional connectivity with ventromedial prefrontal cortex mediates the impact of trait alexithymia on state tobacco craving. Psychopharmacology. 2013;228(1):143–55.
Acknowledgments
This work was supported in part by NIH Grants: K02-AA023566 (Fox), R21- AA024880 (Fox).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Emotion and Addiction
Rights and permissions
About this article
Cite this article
Fox, H.C., Karim, A. & Syed, S.A. Bio-Behavioral Indices of Emotion Regulation: Potential Targets for Treatment in Addiction. Curr Addict Rep 7, 333–343 (2020). https://doi.org/10.1007/s40429-020-00330-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-020-00330-y