Abstract
Background
Bromodomain and extra-terminal (BET) proteins regulate transcription of lipoprotein and inflammatory factors implicated in atherosclerosis. The impact of BET inhibition on atherosclerosis progression is unknown.
Methods
ASSURE was a double-blind, randomized, multicenter trial in which 323 patients with angiographic coronary disease and low high-density lipoprotein cholesterol (HDL-C) levels were randomized in a 3:1 fashion to treatment with the BET protein inhibitor RVX-208 200 mg or placebo for 26 weeks. Plaque progression was measured with serial intravascular ultrasound imaging. Lipid levels, safety, and tolerability were also assessed.
Results
During treatment, apolipoprotein (apo)A-I increased by 10.6 % with placebo (P < 0.001 compared with baseline) and 12.8 % with RVX-208 (P < 0.001 compared with baseline), between groups P = 0.18. HDL-C increased by 9.1 % with placebo (P < 0.001 compared with baseline) and 11.1 % with RVX-208 (P < 0.001 compared with baseline), between groups P = 0.24. Low-density lipoprotein cholesterol (LDL-C) decreased by 17.9 % with placebo (P < 0.001 compared with baseline) and 15.8 % with RVX-208 (P < 0.001 compared with baseline), between groups P = 0.55. The primary endpoint, the change in percent atheroma volume, decreased 0.30 % in placebo-treated patients (P = 0.23 compared with baseline) and 0.40 % in the RVX-208 group (P = 0.08 compared with baseline), between groups P = 0.81. Total atheroma volume decreased 3.8 mm3 in the placebo group (P = 0.01 compared with baseline) and 4.2 mm3 in the RVX-208 group (P < 0.001 compared with baseline), P = 0.86 between groups. A greater incidence of elevated liver enzymes was observed in RVX-208-treated patients (7.1 vs. 0 %, P = 0.009).
Conclusion
Administration of the BET protein inhibitor RVX-208 showed no greater increase in apoA-I or HDL-C or incremental regression of atherosclerosis than administration of placebo.
Trial Registration
ClinicalTrials.gov identifier—NCT01067820.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
RVX-208 had no incremental effect on lipids compared with placebo. |
RVX-208 had no incremental effect on plaque regression. |
The impact of RVX-208 on cardiovascular outcomes remains to be determined. |
1 Introduction
Persistent cardiovascular risk despite widespread use of established medical therapies has stimulated interest in developing new strategies for secondary prevention in patients with coronary artery disease. Favorable findings from human [1] and animal [2] population studies have resulted in considerable interest in development of agents that promote greater levels or activity of high-density lipoproteins (HDLs). However, to date, the success of HDL-cholesterol (HDL-C)-raising therapies in randomized controlled trials has been disappointing [3–5], with the exception of infusing delipidated forms of HDL [6–8].
The induction of endogenous synthesis of apolipoprotein A-I (apoA-I), the major protein associated with HDL particles, represents a novel approach to lipid modification. Enhanced hepatic synthesis of apoA-I should theoretically generate new HDL particles, resulting in greater biological activity of HDL. Preliminary studies of the bromodomain and extra-terminal (BET) inhibitor RVX-208 demonstrated increased apoA-I and HDL-C levels [9] and enhanced systemic cholesterol efflux activity [10]. The BET family of proteins plays an important role in transcriptional regulation and has been implicated in a variety of disease processes. As a result, these effects of RVX-208 have the theoretical potential to favorably affect atherosclerotic plaque.
Intravascular ultrasonography (IVUS) has been successfully employed in clinical trials to evaluate the impact of medical therapies on progression of coronary atherosclerosis [6, 11–17]. These studies have demonstrated that infusion of HDL mimetics has a beneficial impact on plaque progression [6–8]. Accordingly, the objective of the ASSURE (ApoA-I Synthesis Stimulation and Intravascular Ultrasound for Coronary Atheroma Regression Evaluation) study was to determine the 26-week impact of the BET protein inhibitor RVX-208 on the burden of coronary atherosclerosis in patients with coronary disease and low HDL-C levels.
2 Methods
2.1 Study Design
ASSURE was a prospective, randomized, multicenter, double-blind clinical trial [18]. The trial was designed by the Cleveland Clinic Coordinating Center for Clinical Research (C5Research) in collaboration with the Executive Steering Committee and the sponsor. The study protocol was approved by the institutional review board at each site. Patients provided written informed consent prior to study entry.
Patients aged at least 18 years were eligible if they demonstrated at least one 20 % stenosis on clinically indicated coronary angiography and a target vessel for imaging with less than 50 % obstruction. Patients were required to have a low HDL-C level (≤45 mg/dl in females, ≤40 mg/dl in males) within the 60 days prior to enrolment and receive treatment with either atorvastatin 10–40 mg daily or rosuvastatin 5–20 mg daily during the study. Patients treated with another statin agent were switched to rosuvastatin prior to randomization. Patients were excluded if they were receiving either a fibrate or nicotinic acid at a dose of at least 250 mg daily, had uncontrolled hypertension, or had heart failure, severe renal dysfunction, or liver disease.
Patients meeting the inclusion criteria underwent randomization in a 3:1 ratio via interactive voice response system to treatment with RVX-208 100 mg or placebo administered twice daily for 26 weeks. Patients were seen in the clinic every 2 weeks for the first 8 weeks and then every 3 weeks for the remainder of the study.
2.2 Acquisition and Analysis of Ultrasound Images
Following coronary angiography, baseline IVUS was performed. Previous reports have described the methods of image acquisition and analysis [6, 11–17]. Imaging was performed in a single artery using either the s5™ (Volcano, Sacramento, CA, USA) or iLab™ (Boston Scientific, Boston, MA, USA) systems and screened by the core laboratory at the C5Research. Patients meeting prespecified requirements for image quality were eligible for randomization. After 26 weeks of treatment, patients underwent a second ultrasonographic examination in the same artery with the same imaging system. Using digitized images, personnel, who were unaware of the treatment status and time sequence of paired imaging, performed measurements of the lumen and external elastic membrane in images within a matched artery segment. The accuracy and reproducibility of this method have been reported previously [19].
The primary efficacy measure, percent atheroma volume (PAV), was calculated as follows
where EEMarea is the cross-sectional area of the external elastic membrane and Lumenarea is the cross-sectional area of the lumen. The change in PAV was calculated as the PAV at 26 weeks minus the PAV at baseline. A secondary measure of efficacy, normalized total atheroma volume (TAV), was calculated as follows:
where the average plaque area in each image was multiplied by the median number of images analyzed in the entire cohort to compensate for differences in segment length between subjects. The efficacy measure of change in normalized TAV was calculated as the TAV at 26 weeks minus the TAV at baseline. The efficacy measure of change in atheroma volume in the most diseased sub-segment was calculated in the 10-mm segment containing the greatest plaque burden at baseline. Regression was defined as a decrease in PAV or TAV from baseline.
2.3 Biochemical Measures
A central laboratory performed all biochemical determinations (ACM, Rochester, NY, USA; and York, UK). Lipid profiles were determined by enzymatic assay. Levels of apoA-I were determined by turbidimetric immunoassay (Boston Heart Diagnostics, Framingham, MA, USA). Lipoprotein particle number and size were measured with nuclear magnetic resonance (LipoScience, Raleigh, NC, USA) as previously described [20]. Particle concentrations of lipoprotein subclasses of different sizes were calculated from the measured amplitudes of their spectroscopically distinct lipid methyl signals. Lipoprotein levels and safety laboratory measurements were obtained and any adverse reactions recorded at each study visit. High-sensitivity C-reactive protein (CRP) was determined by nephelometry.
2.4 Statistical Analysis
Categorical variables are summarized using frequencies, while laboratory parameters are reported as median and interquartile range (IQR). The primary endpoint was the change in PAV from baseline to 26 weeks post-randomization within the RVX-208 treatment arm and was tested using the Wilcoxon signed-rank test. A similar test was performed separately on the placebo group. The median percent change in laboratory parameters from baseline to 26 weeks within and between treatment groups was tested using the Wilcoxon signed-rank test. Although the study was not sufficiently powered to detect differences between treatment groups, an analysis of covariance (ANCOVA) on ranked data was performed with treatment group as a factor and baseline value as a covariate. The safety analysis of laboratory abnormalities and cardiovascular events was tested using either Chi-squared or Fisher’s exact test.
A sample size of 186 was selected to provide 85 % power to detect a decrease from baseline in PAV of 0.6 % with a standard deviation of 2.7 % in the active RVX-208-treated group. An additional 62 patients were planned to be randomized into the placebo group. With an anticipated non-completion rate of 20 %, a total of 310 patients were planned for enrollment into the trial.
All reported P values are two-sided.
The lead academic investigator (SJN) wrote the manuscript and vouches for the accuracy and completeness of the data and the analyses. While the Executive Steering Committee and C5Research had confidentiality agreements with the sponsor, the study contract specified that a copy of the study database be provided to C5Research for independent analysis and granted the academic authors the unrestricted rights to publish the results.
3 Results
3.1 Subject Characteristics
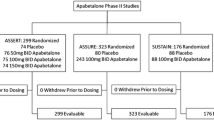
The disposition of patients in the study is summarized in Fig. 1. From 30 September 2011 to 25 September 2012, at 60 centers, 676 patients were screened, with 244 patients randomized to the RVX-208 group and 80 to the placebo group. After 26 weeks of treatment, 281 patients (87.0 %) remained in the study and had IVUS imaging that permitted measurement of atheroma burden at baseline and follow-up. Of these patients, 208 were in the RVX-208 group and 73 in the placebo group. No significant differences were observed between the treatment groups in demographic characteristics, medication use, and laboratory values at baseline (Table 1). No significant differences were observed in baseline characteristics and laboratory values between those patients who completed the study and those who did not. The dose of rosuvastatin (13.8 ± 5.4 vs. 13.2 ± 5.6 mg, P = 0.54) and atorvastatin (29.1 ± 11.4 vs. 27.7 ± 11.7 mg, P = 0.60) did not differ in placebo- or RVX-208-treated patients, respectively. The rate of statin discontinuation did not differ between placebo and RVX-208 groups during the study (14.1 vs. 20.0 %, P = 0.27).
Disposition of patients in study. The final disposition of patients in each group includes all patients assigned to study drug. Patients who withdrew from the study include those discontinued due to subject or physician decision. Adverse events include discontinuation due to adverse events or abnormal laboratory or electrocardiographic results
3.2 Biochemical Measurements
Table 2 summarizes the percentage change of laboratory values for the 281 patients who completed the trial. During the 26 weeks of treatment, apoA-I increased 10.6 % (P < 0.001 compared with baseline) in the placebo group and 12. 8% (P < 0.001 compared with baseline) in the RVX-208 group, between groups P = 0.18. HDL-C increased by 9.1 % (P < 0.001 compared with baseline) in the placebo group and 11.1 % (P < 0.001 compared with baseline) in the RVX-208 group, between groups P = 0.24. Low-density lipoprotein cholesterol (LDL-C) levels decreased by 17.9 % with placebo (P < 0.001 compared with baseline) and 15.8 % with RVX-208 (P < 0.001 compared with baseline), between groups P = 0.55. There were no incremental reductions in other atherogenic lipid parameters or high-sensitivity CRP with RVX-208 compared with placebo. There were no significant differences in nuclear magnetic resonance-derived measures of HDL particle concentrations between the treatment and placebo groups.
3.3 Intravascular Ultrasound Endpoints
Table 3 summarizes the change in IVUS efficacy measures. Greater measures of total atheroma volume [199.9 mm3, 95 % confidence interval (CI) 154.4–258.3 vs. 154.8 mm3, 95 % CI 118.1–209.7; P < 0.001] and atheroma volume in the most diseased 10-mm segment (61.6 mm3, 95 % CI 41.9–82.9 vs. 50.7 mm3, 95 % CI 37.1–70.4; P = 0.05), but not percent atheroma volume (38.1 %, 95 % CI 33.4–44.3 vs. 36.2 %, 95 % CI 30.2–44.8; P = 0.11) were observed in the RVX-208 group. The primary endpoint, change in PAV within the RVX-208 group, decreased by 0.40 % (P = 0.08 compared with baseline). PAV decreased by 0.30 % (P = 0.23 compared with baseline) in the placebo group, between groups P = 0.81. TAV decreased by 3.8 mm3 (P = 0.01 compared with baseline) and 4.2 mm3 (P < 0.001 compared with baseline) in the RVX-208 group, between groups P = 0.86. Atheroma volume in the 10-mm sub-segment that contained the greatest disease burden at baseline decreased by 1.3 mm3 (P = 0.01 compared with baseline) in the placebo group and 2.2 mm3 (P < 0.001 compared with baseline) in the RVX-208 group, between groups P = 0.79. Changes in the primary efficacy parameter, PAV, stratified according to prespecified subgroups are summarized in Fig. 2. There was no evidence of statistical heterogeneity, suggesting a differential effect of RVX-208 in different subgroups.
Prespecified subgroup analysis of the primary endpoint, change in percent atheroma volume from baseline in the RVX-208 treatment group to week 26. Apo apolipoprotein, HDL high-density lipoprotein, HDL-C HDL-cholesterol, hs-CRP high-sensitivity C-reactive protein, IQR interquartile range, PAV percent atheroma volume
3.4 Clinical and Laboratory Adverse Events
Reasons for study discontinuation, laboratory abnormalities, and investigator-reported clinical events are summarized in Table 4. A greater number of discontinuations due to adverse events were observed in the RVX-208 group (3.7 vs. 2.5 %). Elevations of hepatic transaminases greater than three times the upper limit of normal occurred more frequently in the RVX-208 group (7.0 vs. 0 %, P = 0.009). No episode of liver enzyme elevation was accompanied by an increase in bilirubin levels above the upper limit of normal. All episodes of liver enzyme elevation were observed between 4 and 8 weeks of treatment and resolved spontaneously when study drug administration continued. No significant differences in cardiovascular events were observed between the groups (13.8 % in the placebo treatment group vs. 7.4 % in the RVX-2008 group, P = 0.09).
4 Discussion
The ASSURE study evaluated the early impact of a BET protein inhibitor previously reported to increase endogenous synthesis of apoA-1. While modest increases in apoA-I and HDL-C and a decrease in LDL-C from baseline were observed with RVX-208, these changes did not differ from the placebo group. Furthermore, while reductions from baseline in plaque burden were observed in the RVX-208 group, these effects did not differ from changes observed in placebo-treated patients. These data demonstrate that RVX-208 treatment did not result in any measureable incremental benefit on plaque regression for patients with coronary artery disease and low HDL-C levels.
While there is considerable interest in the discovery of new anti-atherosclerotic agents for patients with coronary disease, their clinical development is challenging. Selection of appropriate efficacy biomarkers is critical in the early evaluation of new compounds, in order to focus on agents with the greatest likelihood of success in large and expensive outcome trials. However, to date, no biomarker has consistently predicted clinical benefit for HDL-raising strategies. While substantial interest has focused on measures of HDL functionality [21, 22], none of these techniques are validated to the point that they can reliably determine the potential efficacy of new agents.
Since the expected effects of HDL-modifying strategies involve stimulation of reverse cholesterol transport, the current study and other efforts have employed techniques that measure changes in plaque burden as a measure of their potential benefits. This approach is supported by observations that measurements of coronary plaque burden using IVUS are associated with cardiovascular outcomes [23]. With evidence of enhanced systemic cholesterol efflux capacity in preliminary studies [10], we anticipated that RVX-208 might promote incremental regression of atherosclerotic plaque on serial IVUS evaluation compared with background therapy. However, RVX-208 did not demonstrate an incremental benefit on plaque burden and was accompanied by liver enzyme elevations compared with placebo.
The lack of additional efficacy of RVX-208 is disappointing and surprising, given promising earlier findings. In fact, the lipid changes observed with RVX-208 were similar to those reported in prior studies, yet they paralleled changes in the placebo group, resulting in no incremental benefit on plaque burden. Despite prior evidence of enhanced cholesterol efflux capacity [10] and accumulation of larger, cholesterol-rich HDL particles [9], we observed no incremental effect on HDL-associated measures compared with placebo. This is particularly striking since patients had low HDL cholesterol levels at baseline. The lack of a robust incremental impact on systemic measures of HDL presaged the failure of RVX-208 to promote greater plaque regression in well-treated patients. This finding may possibly reflect either a lack of efficacy of RVX-208 or the inability to improve on benefits produced by statins and other background therapies. It should be particularly noted that the lipid changes in the placebo group were unexpected and may have contributed to the lack of benefit on plaque burden with RVX-208 in this study.
Enhanced endogenous expression of apoA-I is an attractive approach to the therapeutic modification of HDL function. Finding an agent that selectively upregulates hepatic apoA-I expression, without effects on other proteins, has proven daunting. The lipid changes in previous studies of RVX-208 were consistent with enhanced lipid mobilization. However, given the lack of any discernible incremental effect on HDL with RVX-208 in ASSURE I, the absence of a favorable impact on atherosclerotic plaque should not be interpreted as a failure of the HDL hypothesis. Ongoing clinical trials will evaluate the potential cardiovascular efficacy of other mechanisms that target HDL. While it is possible that HDL may be present in a dysfunctional form in patients with coronary disease and a high prevalence of concomitant risk factors [24], whether this may have contributed to any lack of incremental benefit on plaque burden is uncertain. The prior observations that RVX-208 increases large HDL particles would suggest that HDL is intact, although this requires ongoing validation.
Molecular investigations revealed that RVX-208 increased hepatic apoA-I expression via bromodomain and extra-terminal protein inhibition. Resulting derepression of the genetic sequence coding for apoA-1 led to an increase in protein synthesis [25]. As a result, this compound represents the first epigenetic foray into the metabolic treatment of cardiovascular disease. It will be of interest to see whether other epigenetic therapeutic approaches to the modification of cardiometabolic risk proceed into clinical development.
A number of limitations of the current study should be noted. All patients presented for a clinically indicated coronary angiogram. Whether similar findings would have been observed in asymptomatic individuals is unknown. The study was shorter in duration than previous IVUS evaluations of oral therapies. Whether a favorable impact of RVX-208 might be observed during a longer period of follow-up is beyond the scope of this study. The current analysis evaluated the impact of RVX-208 on plaque volume and not plaque morphology. Patients requiring treatment with the highest doses of atorvastatin and rosuvastatin were excluded, thus the impact of RVX-208 in combination with potent statin therapy, which promotes marked disease regression [26], remains unknown. While no significant differences in patient characteristics were observed between the groups at baseline, the potential effect of residual confounding cannot be excluded. We did observe that several baseline measures of plaque burden were greater in the RVX-208-treated group. Previous studies have demonstrated greater regression in patients with higher baseline plaque volume [27]. Accordingly, a greater degree of regression with RVX-208 might have been anticipated in this setting, but was not observed. The ASSURE study was not powered to definitively evaluate the impact of RVX-208 on cardiovascular events, which would require evaluation via a large clinical outcomes trial.
In the quarter century following the introduction of statins to clinical practice, the search to identify new strategies to achieve greater cardiovascular risk reductions has been intensive yet unsuccessful. Ongoing residual risk [28] with current approaches and intolerance in some patients [29] emphasizes the need to develop new agents to reduce cardiovascular risk. In the current study, we did not observe an incremental effect on protective lipid parameters and atherosclerotic plaque burden with RVX-208. The search to identify a strategy that promotes HDL functionality and improve cardiovascular outcomes continues.
References
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease.The Framingham Study. Am J Med. 1977;62:707–14.
Badimon JJ, Badimon L, Galvez A, Dische R, Fuster V. High density lipoprotein plasma fractions inhibit aortic fatty streaks in cholesterol-fed rabbits. Lab Invest. 1989;60:455–61.
AIM-HIGH Investigators, Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, McBride R, Teo K, Weintraub W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67.
Schwartz GG, Olsson AG, Abt M, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367:2089–99.
HPS2-THRIVE Collaborative Group, Landray MJ, Haynes R, Hopewell JC, Parish S, Aung T, Tomson J, Wallendszus K, Craig M, Jiang L, Collins R, Armitage J. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–12.
Nissen SE, Tsunoda T, Tuzcu EM, et al. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290:2292–300.
Tardif JC, Gregoire J, L’Allier PL, et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297:1675–82.
Waksman R, Torguson R, Kent KM, et al. A first-in-man, randomized, placebo-controlled study to evaluate the safety and feasibility of autologous delipidated high-density lipoprotein plasma infusions in patients with acute coronary syndrome. J Am Coll Cardiol. 2010;55:2727–35.
Nicholls SJ, Gordon A, Johansson J, et al. Efficacy and safety of a novel oral inducer of apolipoprotein A-I synthesis in statin-treated patients with stable coronary artery disease a randomized controlled trial. J Am Coll Cardiol. 2011;57:1111–9.
Bailey D, Jahagirdar R, Gordon A, et al. RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo. J Am Coll Cardiol. 2010;55:2580–9.
Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004;291:1071–80.
Nissen SE, Nicholls SJ, Sipahi I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006;295:1556–65.
Nissen SE, Nicholls SJ, Wolski K, et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA. 2008;299:1561–73.
Nissen SE, Nicholls SJ, Wolski K, et al. Effect of rimonabant on progression of atherosclerosis in patients with abdominal obesity and coronary artery disease: the STRADIVARIUS randomized controlled trial. JAMA. 2008;299:1547–60.
Nissen SE, Tardif JC, Nicholls SJ, et al. Effect of torcetrapib on the progression of coronary atherosclerosis. N Engl J Med. 2007;356:1304–16.
Nissen SE, Tuzcu EM, Brewer HB, et al. Effect of ACAT inhibition on the progression of coronary atherosclerosis. N Engl J Med. 2006;354:1253–63.
Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA. 2004;292:2217–25.
Nicholls SJ, Gordon A, Johannson J, et al. ApoA-I induction as a potential cardioprotective strategy: rationale for the SUSTAIN and ASSURE studies. Cardiovasc Drugs Ther. 2012;26:181–7.
Schoenhagen P, Sapp SK, Tuzcu EM, et al. Variability of area measurements obtained with different intravascular ultrasound catheter systems: Impact on clinical trials and a method for accurate calibration. J Am Soc Echocardiogr. 2003;16:277–84.
Mora S, Otvos JD, Rifai N, Rosenson RS, Buring JE, Ridker PM. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation. 2009;119:931–9.
Khera AV, Cuchel M, de la Llera-Moya M, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364:127–35.
Bhattacharyya T, Nicholls SJ, Topol EJ, et al. Relationship of paraoxonase 1 (PON1) gene polymorphisms and functional activity with systemic oxidative stress and cardiovascular risk. JAMA. 2008;299:1265–76.
Nicholls SJ, Hsu A, Wolski K, et al. Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol. 2010;55:2399–407.
Otocka-Kmiecik A, Mikhailidis DP, Nicholls SJ, Davidson M, Rysz J, Banach M. Dysfunctional HDL: a novel important diagnostic and therapeutic target in cardiovascular disease? Prog Lipid Res. 2012;51:314–24.
http://www.resverlogix.com/programs/clinical-cardiovascular-program/rvx-208-clinical-program/rvx-208-moa.html. Accessed 7 Sept 2015.
Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med. 2011;365:2078–87.
Puri R, Nissen SE, Ballantyne CM, et al. Factors underlying regression of coronary atheroma with potent statin therapy. Eur Heart J. 2013;34:1818–25.
Libby P. The forgotten majority: unfinished business in cardiovascular risk reduction. J Am Coll Cardiol. 2005;46:1225–8.
Banach M, Rizzo M, Toth PP, et al. Statin intolerance—an attempt at a unified definition. Position paper from an International Lipid Expert Panel. Arch Med Sci AMS. 2015;11:1–23.
Acknowledgments
Data Safety Monitoring Board: Peter Ganz (Chair), Eva Lonn, Gregory Schwartz, Danielle Brennan.
Intravascular Ultrasound Core Laboratory Staff: William Magyar, Jordan Andrews, Eva Balazs, Anne Colagiovanni, Teresa Fonk, Karilane King, Erin Mayock, Roman Poliszczuk, Rhiannon Regal, Jill Rusticelli.
Additional contributions: We thank Craig Balog, BS, C5Research statistical support. Helen Street and Kim Nguyen at Resverlogix and Deirdre Albertson and Alla Sharorodskaya at inVentiv for their role in study coordination.
Investigators: Argentina: Sanatorio Allende Hipolito, Córdoba (E. Moreyra, MD), Hospital Privado, Córdoba (M. Ballarino, MD), Instituto de Cardiología de Corrientes, Corrientes Capital (J. Baccaro, MD), Sanatorio Parque S. A. Privado,Córdoba (H. Luquez, MD), Instituto de diagnóstico y tratamiento de afecciones cardiovasculares, La Plata (D. Grinfeld, MD), ICBA Instituto Cardiovascular de Buenos Aires, Ciudad de Buenos Aires (L. Padilla, MD), Instituto DAMIC SRL, Córdoba (A. Lorenzatti, MD), Sanatorio San Lucas, San Isidro (G. Marchetti, MD), Clinica Chutro SRL, Córdoba (H. Jure, MD), Sanatorio Güemes,Ciudad de Buenos Aires (M. Bettinotti, MD); Belgium: Universitair Ziekenhuis Antwerpen, Edegem (C. Vrints, MD), Ziekenhuis Oost Limburg, Genk (M. Vrolix, MD), Universite Catholique de Louvain, Brussels (J. Renkin, MD), Centre Hospitalier Universitaire de Charleroi, Charleroi (J. Lalmand, MD); Brazil: Instituto do Coração do Triângulo Mineiro, Uberlândia (R. Vieira Botelho, MD), Hospital Cardiológico Costantini, Curitiba (Costantino Roberto Costantini Frack, MD), Instituto do Coração, São Paulo (P. Lemos, MD), Santa Casa de Misericórdia de Porto Alegre, Porto Alegre (V. Correia deLima, MD), Hemodinâmica Meridional, Cariacica (B. Moulin Machado, MD), Centro de Pesquisa em Cardiologia da Via Médica, Goiânia (W. Kunz Sebba Barroso de Souza, MD), Hospital do Coração do Brasil, Brasília (A. Gomes Taques Fonseca, MD), Instituto Dante Pazzanese de Cardiologia, São Paulo (J. de Ribamar Costa Junior, MD); Hungary: Szent-Györgyi Albert Klinikai Központ, Szeged (I. Ungi, MD), Semmelweis Egyetem Kardiológiai Közpon, Budapest (B. Merkely, MD), Pécsi Tudományegyetem, Pécs (I. Horvath, MD), Fővárosi Önkormányzat Bajcsy-Zsilinszky Kórház, Budapest (B. Nagybaczoni, MD), Honvédkórház - Állami Egészségügyi Központ, Budapest (R. Kiss, MD), Budai Irgalmasrendi Kórhá, Budapest (A. Zsoldos, MD); Netherlands: Onze Lieve Vrouwe Gasthuis, Amsterdam, (J. P. Herrman, MD), Isala Klinieken, Zwolle (M. Gosselink, MD), St. Antonius Ziekenhuis, Niewegein (B. Rensing, MD), Catharina Ziekenhuis, Eindhoven (C. Joost Botman, MD), Maasstad Ziekenhuis, Rotterdam (P. Smits, MD), Maastricht Universitair Medisch Centrum, Maastricht (A. Moens, MD), Canisius Wilhelmina Ziekenhuis, Nijmegen (A. J. M. Oude Ophuis, MD), Medisch Spectrum Twente, Enschede (C. Von Birgelen, MD), Medisch Centrum Alkmaar, Alkmaar (A. A. C. M. Heestermans, MD); Poland: Samodzielna Pracownia Hemodynamiki, Krakow (D. Dudek, MD), Klinika Kardiologii Inwazyjnej, Warszawa (R. Gil, MD), Zakład Kardiologii Inwazyjnej, Katowice (A. Ochala, MD), Oddział Strukturalnych Chorób Serca Samodzielny Publiczny Szpital Kliniczny, Katowice (G. Smolka, MD), Instytut Kardiologii, Warszawa (A. Witkowski, MD); Russia: Acad. V. I. Shumakov, Moscow (V. Chestukhin, MD), St. Petersburg State Healthcare Institution, Saint Petersburg (L. Shcheglova, MD),
Russian Cardiology Research-and-Production Complex, Moscow (V. Kukharchuk MD, M. Ruda, MD, and F. Ageev, MD), 3 Central Military Clinical Hospital, Moscow (V. Ivanov, MD), Tyumen Department of South-Ural Scientific Center of RAMS, Tyumen (S. Shalaev, MD), A. N. Bakulev of RAMS Cardiosurgery Institution, Moscow (S. Matskeplishvili, MD), Scientific Research Cardiology Institute of Sibirian Branch of RAMS,Tomsk (O. Koshelskaya, MD), FSI Federal Center of Heart, Blood and Endocrinology, St. Petersburg (M. Karpenko, MD), FSI State Scientific Research Center of Preventive Medicine of Rosmedtechnologies, Moscow (V. Mazaev, MD), Orenburg State Medical Academy of Roszdrav, Orenburg (R. Sayfutdinov, MD); Spain: Hospital de Meixoeiro, Vigo (A. Iniguez, MD), Hospital Clinico Universitario Virgen de la Victoria, Málaga (J. Maria Hernandez, MD), Hospital de Cabueñes, Gijón (J. Rondan, MD), Hospital Universitari Germans Trias i Pujol, Barcelona (J. Mauri, MD), Hospital Universitario La Paz, Madrid (R. Moreno, MD), Hospital de Galdakao-Usansolo, Galdakao (J. Ramon Rumoroso, MD), Hospital General Universitario Santa Lucia, Cartagena (F. Pico, MD), Hospital Universitari de Bellvitge, Barcelona (A. Cequier, MD), Hospital Clinico Universitario San Carlos, Madrid (F. Alfonso, MD), Hospital Clínico Universitario de Santiago, Santiago de Compostela (R. Trillo, MD), Hospital Vall d’Hebrón, Barcelona (B. Blanco, MD), Hospital Universitario Marqués de Valdecilla, Santander (J. Zueco, MD).
Author contributions
Drs. Nicholls and Nissen and the Cleveland Clinic Coordinating Center for Clinical Research had full and independent access to all of the data in the study. Dr. Nicholls takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Nicholls and Nissen and Ms. Wolski and Borgman were responsible for study concept and design. Drs. Nicholls, Puri, Uno, Herrman, Merkely, and Kataoka and Ms. Borgman take responsibility for data acquisition. Drs. Nicholls, Nissen, Ballantyne, Barter, Brewer, Kastelein, Puri, Uno, Kataoka, Hu, Herrman, and Merkely and Ms. Wolski and Ms. Borgman analysed and interpreted the data. Drs. Nicholls and Nissen and Ms. Wolski drafted the manuscript. Drs. Nicholls, Nissen, Ballantyne, Barter, Brewer, Kastelein, Puri, Uno, Kataoka, Hu, Herrman, and Merkely and Ms. Wolski and Ms. Borgman provided critical revision of the manuscript for important intellectual content. For the purpose of the academic interpretation of the study, Ms. Wolski and Dr. Hu performed all primary statistical analyses of the study that were used for the manuscript. Ms. Wolski is an employee of the Cleveland Clinic Coordinating Center for Clinical Research. Dr. Hu is a faculty member within the Department of Quantitative Health Sciences at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. Drs. Nicholls and Nissen obtained funding for the study. Ms. Borgman provided administrative support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
The study was funded by Resverlogix Corporation.
Role of the Sponsor
The sponsor, Resverlogix Corporation, participated actively in designing the study, developing the protocol, and providing logistical support during the trial. Monitoring of the study was performed by a contract research organization, inVentiv Health Inc., under contract with the sponsor. The sponsor maintained the trial database. Statistical analysis was performed by statisticians employed by inVentiv, although the analysis employed by the manuscript represent those performed by the academic statisticians (Ms. Wolski, Dr. Hu). After completion of the trial, as specified in the study contract, a complete copy of the database was transferred to the Cleveland Clinic Coordinating Center for Clinical Research, where analyses were verified by independent statisticians, Kathy Wolski, MPH and Bo Hu, PhD. The manuscript was prepared by the corresponding author and modified after consultation with co-authors. The sponsor was permitted to review the manuscript and suggest changes, but the final decision on content was exclusively retained by the academic authors.
Financial disclosures
The study was sponsored by Resverlogix Corporation. SJN reports receiving research support from AstraZeneca, Novartis, Eli Lilly, Anthera, LipoScience, Roche, and Resverlogix and has received honoraria or been a consultant for AstraZeneca, Roche, Esperion, Abbott, Pfizer, Merck, Takeda, LipoScience, Omthera, Novo-Nordisk, Sanofi-Aventis, Atheronova, Anthera, CSL Behring, and Boehringer. HBB is a consultant for Merck, AstraZeneca, Eli Lilly, Roche, Amgen, and Sanofi. CMB has received research support from Abbott, Amarin, Amgen, Eli Lilly, GlaxoSmithKline, Genentech, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi-Synthelabo, Takeda, the National Institutes of Health, and the American Heart Association, is a consultant for Abbott, Aegerion, Amarin, Amgen, Arena, Cerenis, Esperion, Genentech, Genzyme, Kowa, Merck, Novartis, Omthera, Pfizer, Resverlogix, Regeneron, Roche, and Sanofi-Synthelabo and serves on the speaker’s bureau for Abbott. PJB has received research grants from Merck and Pfizer, received honoraria from Amgen, AstraZeneca, ISIS, Kowa, Merck, Novartis, Pfizer, and Roche and serves on advisory boards for AstraZeneca, CSL Behring, Kowa, Eli Lilly, Merck, Novartis, Pfizer, and Roche. JJPK has received research support from the Dutch Heart Foundation (2010T082) and has received honoraria or has been a consultant for AstraZeneca, Novartis, Eli Lilly, Anthera, Roche, Resverlogix, Pfizer, Merck, Omthera, Sanofi-Aventis, Regeneron, Amgen, AtheroNova, CSL Behring, Boehringer Ingelheim, Aegerion, the Medicines Company, Isis Pharmaceuticals, Genzyme, Amarin, Xenon Pharma, Servier, and Cerenis. SEN has received research support from AstraZeneca, Eli Lilly, Pfizer, Takeda, Sankyo, and Sanofi-Aventis. He has consulted for a number of pharmaceutical companies without financial compensation. All honoraria, consulting fees, or any other payments from any for-profit entity are paid directly to charity, so that neither income nor any tax deduction is received. No assistance in the preparation of this article is to be declared. RP, KU, YK, MB, JRH, BM, BH, and KW have no potential conflicts to disclose.
Rights and permissions
About this article
Cite this article
Nicholls, S.J., Puri, R., Wolski, K. et al. Effect of the BET Protein Inhibitor, RVX-208, on Progression of Coronary Atherosclerosis: Results of the Phase 2b, Randomized, Double-Blind, Multicenter, ASSURE Trial. Am J Cardiovasc Drugs 16, 55–65 (2016). https://doi.org/10.1007/s40256-015-0146-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-015-0146-z