Abstract
The transdermal route offers advantages for delivery of peptides and proteins. However, these polar and large molecules do not permeate the skin barrier well. Various enhancement methods have been employed to address this problem. Iontophoresis is one of the methods that shows promise but its application to peptide delivery has yet to be fully explored. This study investigates the effects of different molecular properties and iontophoretic conditions on the skin permeation of peptides. In this study, the permeation of alanine-tryptophan dipeptide (MW 276 Da), alanine–alanine–proline–valine tetrapeptide (MW 355 Da), Argireline® (Acetyl hexapeptide-3, MW 889 Da) and Triptorelin acetate (decapeptide, MW 1311 Da) through excised human skin under passive or iontophoretic current of 0.4 mA was investigated. The effects of pH change (3.0–7.4, to provide different net negative, neutral, and positive charges) to the peptide, donor concentration (1–10 mg/ml), background electrolyte (34–137 mM NaCl and/or 5–20 mM HEPES) and current direction (anodal vs cathodal) were also studied. Peptides were analysed by high-performance liquid chromatography or liquid scintillation counting. Iontophoresis led up to a 30 times increase in peptide permeation relative to passive permeation for the peptides. Electroosmosis was an important determinant of the total flux for the high molecular weight charged peptides. Electrorepulsion was found to be considerable for low molecular weight charged moieties. Permeation was decreased at lower pH, possibly due to decreased electroosmosis. Results also showed that 10 times increase in donor peptide concentration increases permeation of peptides by about 2–4 times and decreases iontophoretic permeability coefficients by about 2.5–5 times. The addition of extra background electrolyte decreased the iontophoretic permeation coefficient of peptides by 2–60 times. This study shows that iontophoretic permeation of peptides is affected by a number of parameters that can be optimized for effective transdermal peptide delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many proteins and peptides have been identified that have therapeutic potential for skin conditions [1], cardiovascular disease, Parkinson's disease, Alzheimer's disease, depression, anxiety, attention deficit hyperactivity disorder and many other disorders. Poor oral bioavailability has led to ongoing research for a convenient and noninvasive delivery method. The transdermal route offers different advantages and potential for protein and peptide delivery if the considerable barrier to permeation presented by the stratum corneum can be overcome [2]. Proteins and peptides present a significant challenge to successful transdermal delivery due to the size and complexity of their molecular structure. In addition, most are hydrophilic and often exist in a charged state; thus, passive skin diffusion across the highly structured lipid domains of the stratum corneum is unlikely to be effective. To overcome the skin's barrier to peptides and proteins delivery, different enhancement methods have been employed over the last decades, amongst which iontophoresis looks promising.
A number of commercial iontophoretic devices have been available for transdermal delivery although their market penetration has been limited by cost and technical issues. Iontophoresis involves the use of a mild electrical current (up to 0.5 mA/cm2) to drive charged and uncharged molecules across the skin. The iontophoretic electrical potential acts as an external force to push ionized drug molecules across the skin (electromigration). Cathodal iontophoresis is applied to repel a negatively charged drug from the negative electrode across an epidermal membrane, whilst anodal iontophoresis is used for positively charged drug molecules [3]. Electroosmosis also plays an important role in iontophoretic drug delivery: it produces bulk fluid flow in the membrane and occurs when a voltage difference is imposed across a charged membrane. This fluid stream carries all cargos (ions or neutral species) dissolved within it and always flows in the same direction as the flow of counterions (i.e. ions of opposite charge to the membrane charge) [4]. Human skin is negatively charged above about pH 4 and counterions are positive ions at this condition; thus, electroosmotic flow occurs from anode to cathode [4]. The rate of electroosmosis depends on solvent volume flux and concentration of the cargo. Dependency of electroosmosis on molecular weight is expected to be lower than other mechanisms, as discussed later in this paper. There have been a number of detailed analyses of the mechanistic aspects of iontophoresis and iontophoretic enhancement [5, 6], and a recent review provides an excellent summary of the mathematical models developed to describe iontophoretic transport [7].
Proteins and peptides are usually charged at physiological pH or can be rendered charged by altering pH and are therefore considered ideal candidates for iontophoretic delivery. In addition to their charge, other factors such as molecular weight and mobility of molecules are reported to affect the iontophoretic permeation of peptides. A number of groups have investigated the parameters that influence iontophoresis. Marro et al. [8] concluded that electromigration and electroosmotic transport contributed more than 90 % to the iontophoretic delivery of the ionized drugs (not peptides) lidocaine, quinine and propranolol, and provided a more detailed examination of the iontophoretic transport of lidocaine [9]. Green et al. [10] reported that the normalized iontophoretic flux of anionic tripeptides (maximum molecular weight 400 Da) was independent of lipophilicity but may be inversely related to molecular weight. Our previous work shows that charge may be more important than size, especially when transport is electroosmotic. Green et al. [11] suggested that other ions in solution can contribute to iontophoretic transport of amino acids, a topic that is investigated further in the current paper. Turner and Guy [12] visualized the transport of one peptide, calcein, but did not look at transport mechanisms. The iontophoretic transport of the peptide like drug aminolevulinic acid and the influence of ionic strength, pH and pH-related instability has previously been investigated [13–16]. Our previous work provided a more comprehensive examination of different solutes [17]; however, that work was limited in that the series of solutes studied were mainly classical drug like molecules.
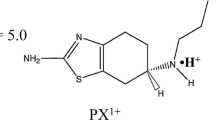
In this study, a wider range of peptides, varying both in size and charge, was investigated. The influence of molecular size of peptides, the direction of applied current and the effect of formulation parameters such as concentration, pH and presence of competing ions on the iontophoretic delivery of five peptides (Fig. 1) across human epidermal membrane in vitro were investigated. The peptides investigated were 5-aminolevulinic acid (small peptide-like drug), a model dipeptide (L-Ala-L-Trp), a therapeutic tetrapeptide L-Ala-L-Ala-L-Pro-L-Val, a cosmetic hexapeptide (acetyl-hexapeptide-3 or Argireline®) and a therapeutic decapeptide (triptorelin acetate). These molecules provide a wide molecular weight range of 130–1,300 and different net charges of negative, neutral and positive. Where possible, peptides with potential therapeutic relevance have been chosen, as discussed below.
5-Aminolevulinic acid (ALA) is a small molecular weight (131.1 g/mol), highly polar, hydrophilic (pKa 4.0 and 8.4) molecule. It is the intermediate in heme biosynthesis and is the precursor of protoporphyrin IX, which is strongly fluorescent and undergoes photobleaching rapidly producing singlet oxygen. Consequently, ALA is used as an endogenous photosensitizer in photodynamic therapy for a range of non-melanoma skin cancers like basal cell carcinoma, squamous cell carcinoma, actinic keratoses and Bowen's disease, and in photo diagnosis [18]. ALA-PDT requires a long administration period of approximately 4 h at the skin surface to provide homogenous delivery at the target site. Chemical and physical penetration enhancement techniques have been investigated to improve the skin penetration of ALA [13–15, 19–23].
L-Ala-L-Trp (alanine–tryptophan, called Ala-Trp in this manuscript) is a model dipeptide molecule (molecular weight 275.9 g/mol), hydrophilic (alanine pKa 2.34 and 9.69, tryptophan pKa 2.28 and 9.39), log P 0.61 ± 0.52.
L-Ala-L-Ala-L-Pro-L-Val (alanine–alanine–proline–valine; AAPV) is a small molecular weight (355.4 g/mol), hydrophilic (logP −0.45 ± 0.65) tetrapeptide. It fits the P-P1 subsites of elastase and inhibits human neutrophil elastase (HNE). HNE acts as a pro-inflammatory agent that is implicated in a number of conditions including rheumatoid arthritis, psoriasis, atopic dermatitis and allergic contact dermatitis. Peptidic HNE inhibitors have a common hydrophobic peptide sequence which partially mimics certain amino acid sequences found in elastin [24].
AC-Glu-Glu-Met-Gln-Arg-Arg-NH2 (EEMQRR; acetyl hexapeptide-3; Argireline®) is a synthetic peptide (molecular weight 888.6 g/mol and log P −4.5 ± 0.95) that has been incorporated into cosmeceutical products for anti-ageing properties [25]. It is designed from the N-terminal end of the protein SNAP-25 that inhibits Ca2+-dependent catecholamine release from chromaffin cells [26]. It acts by downregulation of muscle action and is applied to reduce wrinkles around the eyes.
p-Glu-His-Trp-Ser-Tyr-[D-Trp]-Leu-Arg-Pro-Gly-NH2 (EHWSYWLRPG; triptorelin available as acetate and pamoate) is a synthetic gonadotropin-releasing hormone agonist and a long-acting LHRH analogue (molecular weight, 1,311.5 g/mol; pKa, 7.2, 9.5, 12; and log P 0.3 ± 1.41). It is marketed as a sustained release injection for treatment of infertility, endometriosis and hormone-responsive cancers. Transdermal delivery of triptorelin has been attempted with considerable success [27–29].
Materials and methods
Materials
All chemicals and reagents listed below were used as supplied: 5-aminolevulinic acid hydrochloride (ALA) (A3785 ∼98 %), L-alanyl-L-tryptophan (05400 ≥ 99 %), N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid (HEPES) (H3375 ≥99.5 % titration) and fluorescamine (F9015 ≥98 %) were purchased from Sigma-Aldrich (Sydney, NSW, Australia). AAPV (AV-4-NH2, P100401-SY121097, ≥96 % purity), acetyl-hexapeptide-3 (Ac-ER-6, 54947, ≥95 % purity) and triptorelin acetate (HG-9, 5773-63-4, ≥98 % purity) were purchased from GL Biochem Ltd (Shanghai, China). Phosphate buffer saline was prepared according to United States Pharmacopeia. Sodium chloride (NaCl) was from Asia Pacific Speciality Chemicals Ltd (Seven Hills, NSW, Australia), analytical grade potassium chloride (KCl) and sodium hydroxide (NaOH) were purchased from Merck Pty Ltd. (Darmstadt, Germany), and boric acid was purchased from Ajax Finechem (Taren Point, NSW, Australia). Analytical grade acetonitrile was purchased from JT Baker (Philipsburg, NJ, USA) and trifluoroacetic acid (TFA) from Sigma-Aldrich (Sydney, NSW Australia). Triethylamine was from Fluka Chemika (Switzerland) and orthophospohoric acid from Ajax Finechem (Australia). Silver (Ag) wire (99.99 %, 1 mm diameter) was obtained from Sigma-Aldrich and purified deionized Milli-Q water from Millipore (North Ryde, NSW Australia).
Quantitative analysis
The quantitative analysis of all peptides was by reverse phase high-performance liquid chromatography (HPLC), and liquid scintillation counting was used for ALA. ALA belongs to the class of alpha amino ketones with a weak chromophoric carbonyl group and is therefore unsuitable for quantification by ultraviolet (UV) absorption spectroscopy [22]. The chromatographic system consisted of an Agilent 1100 series equipped with a quaternary pump (G1311A), autosampler (G1313A), solvent-degasser (G1312A) with a photo diode array detector/fluorescence detector (G1321A). Separation was achieved on a Phenomenex Jupiter C18 300A column (5 μm, 150 mm × 4.6 mm) with a guard column (wide pore C18). Peak integration was undertaken on a personal computer using Chemstation A08.01 software. All standards and samples were prepared at room temperature. The radiolabelled samples were analysed on a liquid scintillation counter (Packard LSC; Canberra, CT, AUS).
The HPLC mobile phase consisted of water and acetonitrile buffered with TFA, triethylamine or phosphoric acid. The ratio of aqueous phase to organic phase was dependent on the compound: 30:70 (0.1 % TFA). For Ala-Trp a linear gradient system, aqueous (0.045 % TFA)/acetonitrile (0.036 % TFA) from 10 to 100 % (UV detection at 210 nm), for AAPV a gradient system, aqueous (0.1 % TFA)/acetonitrile (0.1 % TFA) from 5 to 20 % (UV detection at 220 nm), for acetyl hexapeptide 90:10 (0.05 % TFA) isocratic system (UV detection at 210 nm) and for triptorelin 75:25 (20 mM triethylamine and 50 mM phosphoric acid) isocratic system (UV detection at 280 nm). The R.S.D of repeatability was less than 1 % and the lowest limit of quantification was in the range of 12 to 320 ng for all the peptides assayed.
Radiolabelled ALA (0.5 μCi/diffusion cell) were mixed with scintillation cocktail (Emulsifier safe, PerkinElmer, Waltham, MA, USA) and analysed for radioactivity.
Skin preparation
Ethical approval for using human skin was obtained from the Human Research Ethics Committee of Curtin University prior to the study. Full thickness human skin (abdominal section) excised from female patients following abdominoplasty surgery at Perth hospitals was used. Skin was prepared by removing the subcutaneous tissue by dissection then isolating the epidermal membranes from human skin by the heat separation method [30] where the full thickness human skin was immersed in water at 60 °C for 1 min. The epidermal membrane was then teased off the dermis, placed onto aluminum foil with the stratum corneum layer facing upward, air-dried and then stored at −20 °C (for not more than 2 months) until required.
Iontophoretic in vitro permeation studies
All iontophoresis experiments were conducted across human epidermal membrane using Pyrex glass side-by-side diffusion cells, enabling permeation across skin sections of cross-sectional area 0.95 cm2; donor and the receptor volume of 1.8 ± 0.1 mL. The membrane was allowed to equilibrate for 1 h in a water bath maintained at 35 ± 0.5 °C. Membrane integrity was then determined by visual inspection over a bright light and by electrical resistance (in kilo ohms) measurement using a digital portable LCR multimeter (TH2821/A/B, Changzhou Tonghui Electronic Co Ltd, Jiangsu Province, China). The measurements were taken by immersing the silver–silver chloride (Ag/AgCl) electrode attached to the probe lead tips, one each in the donor and receptor compartments. Membranes exhibiting an electrical resistance less than 20 kΩ were rejected.
The receptor compartment was always filled with electrolyte solution (20 mM HEPES + 137 mM NaCl) and the pH adjusted to 7.4. The donor compartment consisted of ALA, Ala-Trp, AAPV, acetylhexapeptide-3 or triptorelin acetate prepared with water or receptor electrolyte solution at various concentrations and the pH adjusted according to the appropriate study.
A constant iontophoretic current of 0.4 mA was supplied through Ag/AgCl eletrode by a custom-built power supply unit (Art Electro NSW, Australia) for 2 h unless otherwise stated. Passive diffusion cells were treated in the same way but without the electrodes. Samples were collected from the receptor compartment and replaced with fresh prewarmed electrolyte solution throughout the experimental period. The data was plotted as mean cumulative amount permeating to the receptor compartment versus time and transdermal permeation flux (J) was calculated over the linear portion of the plot. For passive permeation studies, permeability coefficients (K p) were calculated as flux/donor concentration based on Fick's first law. In iontophoretic studies, considering the Nernst–Planck equation (J total = J passive + J EM + J EO), apparent or total iontophoretic permeability coefficients (concentration-normalized iontophoretic flux) were calculated using total flux. This covers passive, electomigration and electroosmosis contributions. Pure iontophoretic K p that covers electromigration and electroosmosis was calculated as total iontophoretic K p − Passive K p. Note that transport number was not used here as this value applies to electromigration only.
Influence of concentration
The donor compartment consisted of Ala-Trp at 3.6 and 36 mM (1 and 10 mg/ml), AAPV at 2.84 and 28.4 mM (1 and 10 mg/ml), acetylhexapeptide-3 at 1.13 and 11.3 mM (1 and 10 mg/ml) and triptorelin at 0.77 and 7.7 mM. The donor solutions were prepared in water (adjusted with HCl or NaOH for pH thus providing ions for iontophoretic transport) or 20 mM HEPES + 137 mM NaCl. The receptor compartment consisted of 20 mM HEPES + 137 mM NaCl at pH 7.4.
Influence of pH
The donor solution pH was maintained at physiological pH 7.4 or at pH levels 6.0, 5.5, 5.0 and 3 using 0.1 or 0.01 M sodium hydroxide (NaOH) and/or 0.1 or 0.01 M hydrochloric acid (HCl) solutions. The net electrical charges of peptides were calculated at all pH levels using Calculator Plugins for structure property prediction and calculation, Marvin 6.0.0, 2013, ChemAxon (http://www.chemaxon.com).
Influence of background electrolyte
The donor solutions of Ala-Trp, AAPV and triptorelin were prepared in water (adjusted with HCl or NaOH for pH) or receptor electrolyte solutions (20 mM HEPES + 137 mM NaCl). The donor solution for acetylhexapeptide-3 (EEMQRR) was prepared at six different combinations (20, 10, 5 mM HEPES + 137, 68.5, 34.2 mM NaCl, respectively, and 137, 68.5 and 34.2 mM NaCl alone).
Influence of direction of current
For anodal iontophoresis, active cells received the silver electrode in the donor compartment and silver chloride electrode in the receptor compartment, and vice versa for cathodal iontophoresis.
Statistical analysis
The permeation data for ALA was analysed using SPSS 16.0 for Windows (SPSS Inc., Chicago IL). The data for other peptides were analysed using The Mixed Procedure in SAS version 9.1 for Windows (SAS Institute Inc., Cary, NC, USA). The Mann–Whitney U test (one-tailed) was used to determine significant differences between all parameters.
Results
Table 1 provides the passive and iontophoretic flux and permeability coefficients of peptides with neutral or positive net charges under anodal iontophoresis. The results show that iontophoresis has been able to increase permeability coefficient of these peptides by about 7–27 times. Table 1 shows that, except for ALA, irrespective of the molecular weight (300–1,300 Da) and charge (0 to 1.1) of the corresponding peptides, the iontophoretic permeability coefficients of di, tetra, hexa and decapeptides are similar (12–17 × 10−3 cm/h). As the iontophoretic permeability is similar regardless of their differences in physicochemical properties, this might suggest that electroosmosis is the main driving force for iontophoresis of these molecules
Influence of charge and pH
Table 2 provides the effects of pH on charge and iontophoretic permeation of peptides. The iontophoretic permeability coefficient of Ala-Trp showed a significant increase (P < 0.0001) from 0.4 to 13 × 10−3 cm/h when the pH was decreased from 7.4 to pH 5.5. In contrast, the iontophoretic permeability coefficient of AAPV reduced significantly from 18 × 10−3 cm/h at pH 7.4 to 0.4 × 10−3 cm/h (P < 0.0001) at pH 3.0 and no change at pH 5.5 (18 × 10−3 cm/h). Acetylhexapeptide-3 also demonstrated a significantly reduced iontophoretic permeability coefficient from 17 × 10−3 cm/h at pH 7.4 to 4.8 × 10−3 cm/h at pH 5.0 (P < 0.0001).
Influence of concentration
The effect of donor peptide concentration is presented in Table 3. A 10× increase in donor concentration of Ala-Trp, from 3.6 to 36 mM (from 1 to 10 mg/ml) at pH 5.5 resulted in a 4.2× increase in iontophoretic flux but reduced the iontophoretic permeability coefficient from 13.0 to 5.5 × 10−3 cm/h. A 10× increase in donor concentration of acetylhexapeptide-3 from 1 to 10 mg/ml at physiological pH, resulted in a 2.5× increase in the iontophoretic epidermal flux but decreased the permeability coefficient by about four times. The same trend was observed for triptorelin where a 2× increase in flux and 5× decrease in iontophoretic permeability coefficient was observed after a 10× increase in the peptide concentration (Table 3).
Influence of background electrolyte
The presence of HEPES and Na+ ions significantly reduced the iontophoretic delivery of all peptides (Tables 4 and 5). A 14× reduction in iontophoretic permeability coefficient of Ala-Trp resulted from the donor solution of 20 mM HEPES and 137 mM NaCl at pH 5.5 compared to water (adjusted with HCl or NaOH for pH). A less pronounced reduction of less than 2× in the iontophoretic permeability coefficient of AAPV, EEMQRR and Triptorelin occurred with 20 mM HEPES and 137 mM NaCl (Table 4).
To investigate the effects of electrolytes type and concentration, the influence of different HEPES (10 and 5 mM) + NaCl (68.5 and 34.2 mM) systems and different NaCl solutions alone (137, 68.5 and 34.2 mM) were studied for EEMQRR iontophoretic permeation. The iontophoretic permeability coefficient data for all donor solutions is presented in Table 5 in comparison to base system. The results clearly indicate that a high concentration of ions in the delivery vehicle reduces the iontophoretic permeability coefficient of EEMQRR. The extent of reduction was more for NaCl alone (11–57×) in comparison to HEPES-containing systems (less than 2× reduction). The permeability reduction effects of background electrolytes were also concentration-dependent and the effect increased with increase in electrolyte concentration (Table 5).
Influence of direction of current: anodal vs cathodal
The direction of the current can influence the iontophoretic skin permeation depending on the predominant charge carrier. The iontophoretic permeability coefficient of AAPV and acetylhexapeptide-3 that permeated human epidermis under the influence of anodal versus cathodal current is presented in Table 6. The direction of current did not influence iontophoretic delivery of AAPV. In contrast, the iontophoretic permeability coefficient of acetylhexapeptide-3 under cathodal current was similar to passive delivery [(1.2 ± 0.3) × 10−3 cm/h] compared to (17 ± 2) × 10−3 cm/h with anodal current.
Discussion
The mechanisms involved in the iontophoretic enhancement of skin permeation of drugs are electrorepulsion (electromigration), electroosmosis and changes in skin permeability (skin damage) due to electrical current [4]. The similarity of iontophoretic permeability coefficients for different molecules (molecular weight range 300–1,300 Da and charge 0 to 1.1; Table 1) in the present investigation might show the important role of electroosmosis in peptides penetration. For example, triptorelin has a positive net charge of about +1 at pH 7.4. Therefore, at least theoretically, a good contribution from electromigration over electroosmosis is expected for this molecule from anodal iontophoresis. However, the present data might suggest that iontophoretic permeation of triptorelin is mainly due to electroosmosis. Considering this argument, the electroosmotic volume flux in the conditions used in the present study was calculated to be about 10–17 μl/cm2/h. An electroosmotic flow of up to 37 μl/cm2/h in hairless mouse skin was reported by Pikal and Shah [31, 32]. However, as discussed later, the presence of other mechanisms, including electrorepulsion, cannot be dismissed specially for low molecular weight peptides.
Table 2 shows the effects of pH on iontophoretic permeation of peptides. pH affects permeation of drugs in iontophoresis in different ways. The pH of the donor solution plays an important role in ionization of molecules (their electromigration) and the charge of the skin (skin permselectivity) and therefore electroosmosis [33]. The pH of the solution can also affect the chemical stability of peptides and proteins, as was previously reported for ALA [16, 21]. The isoelectric point (pI) of skin is about 4–5 [34] and skin shows negative charges at pH levels above this value and positive charges at lower pH levels. Bath et al. [35] showed that electroosmotic flow is highly pH-dependent and is from anode to cathode at pH levels >3.5 and from cathode to anode at pH levels <3.5. They also showed that anodal electroosmosis increases with pH increase above 3.5 and cathodal electroosmosis increases with pH decrease below 3.5.
Ala-Trp is neutral at pH 5.5 and becomes negatively charged when the pH is increased to 7.4. The sharp decrease in permeability of Ala-Trp from 13 to 0.4 can be explained by electromigration in an opposite direction to that of electroosmosis. This might show the importance of electroosmosis for permeation of AAPV and electromigration for permeation of Ala-Trp. Such behaviour might be due to the difference in their molecular weight, indicating that electroosmosis is important for higher molecular weights and electromigration for lower molecular weights. However, we cannot dismiss the importance and the role of electromigration at these conditions.
The iontophoretic permeability coefficient of EEMQRR decreased from 17 × 10−3 cm/h at pH 7.4 to 4.8 × 10−3 cm/h (close to its passive permeation) at pH 5. For AAPV, the iontophoretic permeability coefficient decreased from 18 × 10−3 cm/h at 7.4 to 0.4 × 10−3 cm/h at pH 3.0. These reductions happen in spite of the positive charges of these molecules (0.2 and 0.9 for EEMQRR and AAPV, respectively) at lower pH levels (Table 2) that is expected to increase the flux through electrorepulsion. This shows the importance of electroosmosis in the permeation of these higher molecular weight peptides. This has been reported for thyrotropin-releasing hormone [36], where greater iontophoretic transport was achieved in its unionized form at pH 8 by electroosmosis than at pH 4 where it is 99 % cationic. These effects can be attributed to the reverse in skin permselectivity from cationic to anionic at acidic pH, and electroosmosis occurs from cathode to anode.
Increasing the donor peptide concentration increased the iontophoretic flux of the peptides, but the flux increase was not equivalent to the increase in concentration. A 10× increase in the peptide concentration resulted in only two to four times increase in flux, indicating 2.5–5× decrease in the iontophoretic permeability coefficients (Table 3). Delgado-Charro et al. [37] showed that when drugs neutralize the skin charge, increased drug concentration decreases the permeability through decreased and even reversal of electroosmosis. This might explain in part the present data. However, the same group suggested that when electrorepulsion is the major mechanism, the iontophoretic permeability coefficient is expected to stay constant (linear relationship between concentration and flux). Thus another explanation is the possible iontophoretic charge saturation, as was reported for LHRH and two analogues [38].
The present results show that the presence of 20 mM HEPES + 137 mM NaCl reduced the iontophoretic permeability coefficient of peptides (Table 4). The highest reduction was for Ala-Trp (about 14×). Other peptides showed about 2× difference regardless of their charges and molecular weight. To further investigate the effects of addition of background electrolytes, the effects of 5–20 mM HEPES and 34–137 mM NaCl was investigated for the hexapeptide (EEMQRR: Table 5). The presence of co-ions and counterions revealed a linear trend in the permeation of acetyl hexapeptide-3, with the linear reduction in concentration of co-ions and counterions present (20, 10, 5 mM HEPES with 137, 68.5, 34.2 mM NaCl, respectively). Significantly lower amounts of acetyl hexapeptide-3 permeated when the peptide donor solution was prepared in NaCl (137, 68.5, 34.2 mM) alone. Results show that the reduction effects of added electrolyte are both electrolyte type- and concentration-dependent. In agreement with the present data, Bellantone et al. [39] demonstrated a reduction in benzoate flux by more than half in the presence of equimolar amounts of sodium chloride. Cázares-Delgadillo et al. [40] presented a similar observation with cytochrome C-A, a 12.4-kDa protein. The iontophoretic delivery of the macromolecule was reduced 3.9-fold when the sodium ion concentration increased to 170 mM. These effects can be related to the effects of added electrolytes on both electrorepulsion and also electroosmosis, as described below.
Essentially, addition of a background electrolyte, buffer or substance that can increase the ionic strength of the formulation increases the competition between the charge carriers and can affect iontophoretic drug flux [41]. Electrolytes can also affect electroosmotic flow. It has been demonstrated that increasing the electrolyte ionic strength in the electrode chambers (relative to the physiological level present beneath the tissue) decreased mannitol extraction (i.e. decreased electroosmosis) [42]. They demonstrated that regardless of the mechanism (electrorepulsion or electroosmosis), the concentration of the electrolyte should be at its optimum level to allow charge transfer whilst at the same time not neutralize the skin charge and not prevent the drug carrying the charge. A minimum amount of electrolyte, however, must be present in order to provide the required electrochemistry of the system.
Table 6 presents the effects of direction of the current on the permeation of two peptides. AAPV shows a similar flux from both anodal and cathodal concentration, in spite of its negative charge. This might show the importance of both electrorepulsion and electroosmosis for permeation of AAPV. However, acetyl hexapeptide-3 is benefiting from electroosmosis due to lack of charge and high molecular weight, therefore showing a high anodal flux and a low cathodal permeation (Table 6).
The peptides were chosen here to provide a series with increasing molecular weight and different charges. Figure 2 shows the relationship between iontophoretic permeability coefficient and molecular weight and molecular charge for the peptides used in the present investigation. It has been reported that iontophoretic permeation of drugs decreases with increased molecular size [11, 17, 43, 44]. However, the size-dependency for iontophoretic permeation varies with the mechanism and the size-dependency of electroosmosis is expected to be lower than that of passive diffusion or electrorepulsion [5]. pH-dependency and charge-dependency of iontophoretic permeation is also expected to vary under different mechanisms. Using the ionic mobility pore model, Roberts et al. [43] correlated the molecular weight of the peptides with their iontophoretic permeability coefficient. The same has been reported with experimental evidence using small molecular weight local anaesthetics. The ionic mobility pore model identified ionic mobility and molecular size to be the major predictors of iontophoretic permeability. Ionic mobility of a molecule depends on its pKa, molecular weight and conductivity.
Here and on the basis of the mechanisms described above, iontophoretic permeation of higher weight molecular weight peptides, AAPV (tetrapeptide), Argireline (hexapeptide) and Triptorelin (decapeptide) was analysed against their molecular weight using linear regression, and a line with a negative slope of 0.0002 was observed (Fig. 3). Such relationship has been reported in the literature, with Green et al. [10, 11] reporting a negative slope of 0.002 for cathodal iontophoresis of a series of amino acids. Similarly DelTerzo et al. [45] reported a negative slope of 0.006 for alkanoic acids and Phipps et al. [46] reported a negative slope of 0.003 for inorganic cationic drugs. Based on the free volume model by Yoshida et al. [47, 48], a mean slope of 0.0032 was interpreted to give an average free volume equivalent to the molecular volume of an ionized solute with molecular weight of 135.
Conclusion
This investigation showed that transdermal permeation of peptides is a complex process and is affected by molecular weight, charge, donor pH, donor drug concentration, background electrolytes and direction of the iontophoresis. The relative importance of electroosmosis and electrorepulsion depends on the molecular weight of the peptide, pH of the environment and molecular charge. In the current study, electroosmosis played an important role in the permeation of higher molecular weight peptides, even when they are charged, while lower weight peptides were affected more by electromigration. The present data clearly shows that these different parameters need to be adjusted for optimized peptide delivery.
References
Namjoshi S, Cacetta R, Benson HA. Skin peptides: biological activity and therapeutic opportunities. J Pharm Sci. 2008;97:2524–42.
Benson HA, Namjoshi S. Proteins and peptides: strategies for delivery to and across the skin. J Pharm Sci. 2008;97:3591–610.
Delgado-Charro MB, Guy RH. Iontophoresis: application in drug delivery and noninvasive monitoring. In: Hadgraft J, Guy RH, editors. Transdermal drug delivery. New York: Marcel Dekker; 2003. p. 199–225.
Pikal MJ. The role of electroosmotic flow in transdermal iontophoresis. Adv Drug Deliv Rev. 2001;46:281–305.
Guy RH, Kalia YN, Delgado-Charro MB, Merino V, Lopez A, Marro D. Iontophoresis: electrorepulsion and electroosmosis. J Control Rel. 2000;64:129–32.
Abla N, Naik A, Guy RH, Kalia YN. Contributions of electromigration and electroosmosis to peptide iontophoresis across intact and impaired skin. J Control Rele. 2005;108:319–30.
Gratieri T, Kalia YN. Mathematical models to describe iontophoretic transport in vitro and in vivo and the effect of current application on the skin barrier. Adv Drug Deliv Rev. 2013;65:315–29.
Marro D, Kalia YN, Delgado-Charro MB, Guy RH. Contributions of electromigration and electroosmosis to iontophoretic drug delivery. Pharm Res. 2001;18:1701–8.
Marro D, Kalia YN, Delgado-Charro MB, Guy RH. Optimizing iontophoretic drug delivery: identification and distribution of the charge-carrying species. Pharm Res. 2001;18:1709–13.
Green PG, Hinz RS, Kim A, Szoka Jr FC, Guy RH. Iontophoretic delivery of a series of tripeptides across the skin in vitro. Pharm Res. 1991;8:1121–7.
Green PG, Hinz RS, Cullander C, Yamane G, Guy RH. Iontophoretic delivery of amino acids and amino acid derivatives across the skin in vitro. Pharm Res. 1991;8:1113–20.
Turner NG, Guy RH. Iontophoretic transport pathways: dependence on penetrant physicochemical properties. J Pharm Sci. 1997;86:1385–9.
Lopez RF, Bentley MV, Begona Delgado-Charro M, Guy RH. Optimization of aminolevulinic acid delivery by iontophoresis. J Control Rel. 2003;88:65–70.
Lopez RF, Bentley MV, Delgado-Charro MB, Guy RH. Iontophoretic delivery of 5-aminolevulinic acid (ALA): effect of pH. Pharm Res. 2001;18:311–5.
Lopez RF, Bentley MV, Delgado-Charro MB, Salomon D, van den Bergh H, Lange N, et al. Enhanced delivery of 5-aminolevulinic acid esters by iontophoresis in vitro. Photochem Photobiol. 2003;77:304–8.
Krishnan G, Roberts MS, Grice J, Anissimov YG, Benson HA. Enhanced transdermal delivery of 5-aminolevulinic acid and a dipeptide by iontophoresis. Biopolymers. 2011;96:166–71.
Lai PM, Roberts MS. An analysis of solute structure–human epidermal transport relationships in epidermal iontophoresis using the ionic mobility: pore model. J Control Rel. 1999;58:323–33.
Gerscher S, Connelly JP, Griffiths J, Brown SB, MacRobert AJ, Wong G, et al. Comparison of the pharmacokinetics and phototoxicity of protoporphyrin IX metabolized from 5-aminolevulinic acid and two derivatives in human skin in vivo. Photochem Photobiol. 2000;72:569–74.
Bodde HE, Roemele PE, Star WM. Quantification of topically delivered 5-aminolevulinic acid by lontophoresis across ex vivo human stratum corneum. Photochem Photobiol. 2002;75:418–23.
Ferreira DM, Saga YY, Aluicio-Sarduy E, Tedesco AC. Chitosan nanoparticles for melanoma cancer treatment by photodynamic therapy and electrochemotherapy using aminolevulinic acid derivatives. Curr Med Chem. 2013;20:1904–11.
Krishnan G, Grice JE, Roberts MS, Benson HA, Prow TW. Enhanced sonophoretic delivery of 5-aminolevulinic acid: preliminary human ex vivo permeation data. Skin Res Technol. 2013;19:e283–9.
Namjoshi S, Caccetta R, Edwards J, Benson HA. Liquid chromatography assay for 5-aminolevulinic acid: application to in vitro assessment of skin penetration via dermaportation. J Chromatogr B. 2007;852:49–55.
Mikolajewska P, Donnelly RF, Garland MJ, Morrow DI, Singh TR, Iani V, et al. Microneedle pre-treatment of human skin improves 5-aminolevulininc acid (ALA)- and 5-aminolevulinic acid methyl ester (MAL)-induced PpIX production for topical photodynamic therapy without increase in pain or erythema. Pharm Res. 2010;27:2213–20.
Hornebeck W, Moczar E, Szecsi J, Robert L. Fatty acid peptide derivatives as model compounds to protect elastin against degradation by elastases. Biochem Pharmacol. 1985;34:3315–21.
Blanes-Mira C, Clemente J, Jodas G, Gil A, Fernandez-Ballester G, Ponsati B, et al. A synthetic hexapeptide (Argireline) with antiwrinkle activity. Int J Cosmet Sci. 2002;24:303–10.
Blanes-Mira C, Merino JM, Valera E, Fernandez-Ballester G, Gutierrez LM, Viniegra S, et al. Small peptides patterned after the N-terminus domain of SNAP25 inhibit SNARE complex assembly and regulated exocytosis. J Neurochem. 2004;88:124–35.
Nicoli S, Rimondi S, Colombo P, Santi P. Physical and chemical enhancement of transdermal delivery of triptorelin. Pharm Res. 2001;18:1634–7.
Nicoli S, Santi P, Couvreur P, Couarraze G, Colombo P, Fattal E. Design of triptorelin loaded nanospheres for transdermal iontophoretic administration. Int J Pharm. 2001;214:31–5.
Schuetz YB, Naik A, Guy RH, Vuaridel E, Kalia YN. Transdermal iontophoretic delivery of triptorelin in vitro. J Pharm Sci. 2005;94:2175–82.
Kligman A, Christophers E. Preparation of isolated sheets of human stratum corneum. Arch Dermatol. 1963;88:70–3.
Pikal MJ, Shah S. Transport mechanisms in iontophoresis. III. An experimental study of the contributions of electroosmotic flow and permeability change in transport of low and high molecular weight solutes. Pharm Res. 1990;7:222–9.
Pikal MJ, Shah S. Transport mechanisms in iontophoresis. II. Electroosmotic flow and transference number measurements for hairless mouse skin. Pharm Res. 1990;7:213–21.
Mudry B, Guy RH, Begona Delgado-Charro M. Prediction of iontophoretic transport across the skin. J Control Rel. 2006;111:362–7.
Green PG. Iontophoretic delivery of peptide drugs. J Control Rel. 1996;41:33–48.
Bath BD, Scott ER, Phipps JB, White HS. Scanning electrochemical microscopy of iontophoretic transport in hairless mouse skin. Analysis of the relative contributions of diffusion, migration, and electroosmosis to transport in hair follicles. J Pharm Sci. 2000;89:1537–49.
Huang YY, Wu SM, Wang CY. Response surface method: a novel strategy to optimize iontophoretic transdermal delivery of thyrotropin-releasing hormone. Pharm Res. 1996;13:547–52.
Delgado-Charro MB, Rodrfguez-Bayon AM, Guy RH. Iontophoresis of nafarelin: effects of current density and concentration on electrotransport in vitro. J Control Rel. 1995;35:35–40.
Miller LL, Kolaskie CJ, Smith GA, Rivier J. Transdermal iontophoresis of gonadotropin releasing hormone (LHRH) and two analogues. J Pharm Sci. 1990;79:490–3.
Bellatone NH, Rim S, Francoeur ML, Rasadi B. Enhanced percutaneous absorption via iontophoresis I. Evaluation of an in vitro system and transport of model compounds. Int J Pharm. 1986;30:63–72.
Cazares-Delgadillo J, Naik A, Ganem-Rondero A, Quintanar-Guerrero D, Kalia YN. Transdermal delivery of cytochrome C–A 12.4 kDa protein across intact skin by constant-current iontophoresis. Pharm Res. 2007;24:1360–8.
Mudry B., Guy R.H., Delgado-Charro M.B. Iontophoresis. In: Touitou E., Barry B.A., editors. Transdermal Delivery. Boca Raton: CRC; 2006.
Santi P, Guy RH. Reverse iontophoresis—Parameters determining electroosmotic flow: I. pH and ionic strength. J Control Rel. 1996;38:159–65.
Roberts MS, Lai PM, Anissimov YG. Epidermal iontophoresis: I. Development of the ionic mobility-pore model. Pharm Res. 1998;15:1569–78.
Lai PM, Roberts MS. Epidermal iontophoresis: II. Application of the ionic mobility-pore model to the transport of local anesthetics. Pharm Res. 1998;15:1579–88.
DelTerzo S, Behl CR, Nash RA. Iontophoretic transport of a homologous series of ionized and nonionized compounds: influence of hydrophobicity and mechanistic interpretation. Pharm Res. 1989;6:89–90.
Phipps JB, Padmanabhan RV, Lattin GA. Iontophoretic delivery of model inorganic and drug ions. J Pharm Sci. 1989;78:365–9.
Yoshida NH, Roberts MS. Structure–transport relationships in transdermal iontophoresis. Adv Drug Deliv Rev. 1992;9:239–64.
Yoshida NH, Roberts MS. Solute molecular size and transdermal iontophoresis across exised human skin. J Control Rel. 1993;25:177–95.
Acknowledgments
The authors would like to thank Dr Tom A Robertson, University of South Australia, for his calculation of peptides net charges and related discussions. GK acknowledges a Curtin University Postgraduate Scholarship. This work was financially supported by grants from an Australian Research Council Linkage Grant and from the National Health & Medical Research Council of Australia.
Conflict of interest
All authors declare they have no conflict of interest related to this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnan, G., Roberts, M.S., Grice, J. et al. Iontophoretic skin permeation of peptides: an investigation into the influence of molecular properties, iontophoretic conditions and formulation parameters. Drug Deliv. and Transl. Res. 4, 222–232 (2014). https://doi.org/10.1007/s13346-013-0181-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-013-0181-8