Abstract
Purpose
Drugs with higher molecular charges generally show higher flux enhancement when electromigration is the main mechanism in transdermal iontophoresis. This study evaluated the effect of decreasing the formulation pH to increase the positive charges of pramipexole dihydrochloride (PXCl) on its iontophoretic transport across skin.
Methods
In vitro transdermal iontophoresis of PXCl in buffer solution isotonized with either sodium chloride or mannitol were performed in a pH range of 3.0–7.0. Experiments of iontophoresis under symmetric condition with respect to donor and receiver pH and passive transport of the drugs after pretreatment with iontophoresis were conducted to investigate the transport mechanism involved.
Results
Iontophoretic permeation of PXCl was pH-dependent in drug solution isotonized with mannitol. The iontophoretic flux of PXCl with valence z = +2 at pH 3.0 was half of that of PXCl with z = +1 at pH 7.0. The results suggest that the decrease in PXCl delivery at higher valence at pH 3 was mainly due to pH-dependent selectivity of PX ion permeation across the skin and not electroosmosis.
Conclusions
Skin permselectivity is a significant factor for iontophoretic transport of PXCl, and reducing formulation pH to increase the positive charges on PX ions did not enhance PXCl delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pramipexole (PX), an aminothiazole derivative, is a selective dopamine receptor agonist. It has been widely used as a first-line drug for the treatment of early and advanced Parkinson’s disease due to its long-term efficacy, safety, and tolerability (1,2). PX dihydrochloride (PXCl) is the salt form of PX in commercial drug products. Oral administration of dopamine agonists often cause fluctuations in plasma concentration resulting in pulsatile dopaminergic stimulation and poor patient compliance in Parkinson’s disease patients suffering from motor symptoms and dysphagia (3). Therefore, an alternative route for PX is desired for continuous and more patient-friendly drug delivery to improve symptomatic treatment of the drug and patient compliance (4,5). PX contains two ionizable amine groups (primary amine and secondary amine with pKa of 5.0 and 9.6, respectively) on its structure (6). It has a molecular weight of 211.33 g/mol and is available as dihydrochloride salt possessing good aqueous solubility and a net positive charge at physiological pH. Thus, PX cannot permeate across the skin effectively unless penetration enhancement is accomplished in the delivery of the drug. Among the skin penetration enhancement techniques (7,8) such as chemical penetration enhancer, prodrug approach, carrier systems and iontophoresis, iontophoresis is a promising method due to its significant flux enhancement on ionic drugs (9) and the potential of programmable delivery taking advantage of the multiple charges on PX ion.
Transdermal iontophoresis is an effective method to deliver ionized or charged compound across skin using an electric field as an external driving force (9). For iontophoresis, transport enhancement of ionic permeants is a result of electromigration, electroosmosis and electric field-induced skin alteration (10). Several factors affecting iontophoretic drug transport include pH of the donor solution, drug concentration, solution ionic strength, current intensity and type of current (9,10). In theory, the transport efficiency depends on the fraction of the applied current carried by the ion of interest. The fraction of current carried by a particular ion is described by its transference number (ti) and can be calculated by Eq. 1 (11):
where μ is the electrophoretic mobility, z is the valence, and c is the concentration for ions i and j, respectively.
Formulation pH has a significant influence on the ionization of drug and skin related to transport enhancement due to electromigration and electroosmosis in transdermal iontophoresis. A change in solution pH in transdermal iontophoresis affects the net positive valence of PX ions and the degree of skin ionization and subsequently the contribution of electromigration, electroosmosis and skin permselectivity to the iontophoretic drug transport (12,13,14). Previously, Kalaria et al. (15,16) investigated the mechanism of iontophoretic transport of PXCl across pig and human skin and found that electromigration is a predominant transport mechanism for PXCl iontophoresis with minimum contribution from electroosmosis. In theory, when electromigration is the main mechanism in transdermal iontophoresis with small contribution from electroosmosis, drugs with higher molecular charges are expected to provide higher flux enhancement due to the increase in their electrophoretic mobilities. In other words, for drugs with the multiple charges such as PX ion (positive charges of +1 and +2 with respect to the two values of pKa), it is expected that PX ion with a net valence of +2 at pH 3 would provide higher flux than PX ion with a net valence of +1 at pH 7. Therefore, it is reasonable to investigate whether adjusting the pH of PX solution to increase its valence would enhance the iontophoretic delivery of PXCl, which has not been systematically studied.
The objective of this study was to determine the influence of pH on iontophoretic transport of PXCl due to drug ionization (molecular charges of +1 and +2). As would be shown in the present study, the iontophoretic flux of PXCl with net valence of +2 at pH 3.0 was lower than that of PXCl with net valence of +1.5 at pH 5.0, which in turn was lower than that with net valence of +1 at pH 7.0. Therefore, another objective was to investigate the mechanism of the slower PX ion transport observed at pH 3.0 and the faster transport at pH 7.0 under the influence of formulation pH. In this study, anodal iontophoresis experiments at pH ranging from 3.0 to 7.0 were conducted with constant direct current of 0.5 mA/cm2. Passive permeation experiments without iontophoresis were the control for comparison. As the ion composition of drug formulation affects the transference numbers of ions and subsequently transdermal iontophoretic transport of PXCl, iontophoresis experiments were performed as a function of pH in buffer solution isotonized with sodium chloride (NaCl) in comparison with that in buffer solution isotonized with mannitol to investigate the ion competition effect. Acetaminophen (AP), a neutral drug permeant, was concomitantly delivered with PXCl by iontophoresis to determine the contribution of electromigration and electroosmosis to the iontophoretic transport of PXCl. Passive transport of PXCl and AP was measured at different pH conditions after iontophoresis pretreatment to evaluate skin permselectivity to PX ions and its effect on pH-dependent iontophoretic transport.
Materials and Methods
Materials
PX and AP were purchased from Xi’an Lyphar Biotech Co. (Shaanxi, China) and Bengbu Bayi Pharmaceutical Co., Ltd. (Anhui, China), respectively. The hydrochloride salt of PX was prepared by a procedure described by Balicki et al. (17) with some modifications. PXCl monohydrate with a molecular weight of 302.06 g/mol were analyzed by elemental analysis and high-performance liquid chromatography (HPLC). PXCl monohydrate was used in this study. NaCl and trisodium citrate dihydrate (C6H5Na3O7·2H2O) were supplied by Carlo Erba Reagent (Milan, Italy). Citric acid (C6H8O7) and sodium azide (NaN3) were obtained from Sigma-Aldrich (St. Louis, Missouri). D-mannitol, sodium dihydrogen orthophosphate (NaH2PO4) and disodium hydrogen orthophosphate (Na2HPO4) were available from Ajax Finechem (New South Wales, Australia). HPLC grade acetronitrile was supplied by Honeywell Burdick and Jackson (Ulsan, Korea). Triethylamine was obtained from Merck (Hesse, Germany). Phosphoric acid was provided by J.T.Baker® (Central Valley, Pennsylvania). Agarose was purchased from Life Technologies Corporation (Carisbad, California). Silver sheet (99% purity) was purchased from a local precious metal alloy manufacturer in Bangkok, Thailand. Potassium chloride was provided by VWR Prolabo BDH chemicals (Flemish Brabant, Belgium). Buffer solutions of 0.01 M citrate buffer (pH 3.0 and 5.0) and 0.01 M phosphate buffer (pH 6.0 and 7.0) were prepared by mixing appropriate amounts of buffering agents in water: C6H8O7 and C6H5Na3O7·2H2O for citrate buffer and NaH2PO4 and Na2HPO4 for phosphate buffer, respectively. These buffer solutions were utilized to prepare the drug solution. Phosphate-buffered saline pH 7.4 (PBS) consisting of 0.01 M phosphate buffer and 0.142 M NaCl was used to prepare skin and serve as a simulated physiological fluid in the receiver chamber for transport study. All buffer solutions were preserved by 0.02% (w/v) NaN3. The pH of each buffer solution was checked with a pH meter (Inlab®; Mettler-Toledo International Inc., Columbus, Ohio).
Skin Preparation
Human skin of female aged 22–68 years old was obtained from abdominoplastic surgical operations (Department of Surgery, Yanhee International Hospital, Thailand). Human epidermal membrane (HEM) was prepared by heat separation technique (18). Briefly, all residual subcutaneous fat was removed with surgical scissors. Subsequently, the skin was immersed in PBS at 60°C for 1 min. The epidermis was carefully peeled off from the underlying dermis using plastic forceps. The HEM was soaked in PBS, blotted dry, wrapped in aluminum foil and stored at −20°C for later use. This protocol was approved by the committee on human rights related to human experimentation, Mahidol University, Thailand (COE. No. MU-DT/PY-IRB 2018–058.2911).
Preparation of Isotonic Solution of PXCl
Briefly, either 1 or 10 mg/ml PXCl isotonic solution was prepared by dissolving PXCl monohydrate in each buffer solution (i.e., 0.01 M citrate buffer pH 3.0, 0.01 M citrate buffer pH 5.0, 0.01 M phosphate buffer pH 6.0 and 0.01 M phosphate buffer pH 7.0). NaCl or mannitol was added in each solution to adjust the tonicity. The concentrations of NaCl in the NaCl isotonized PXCl solutions of pH 5.0, 6.0 and 7.0 were 0.142, 0.145 and 0.143 M, respectively. The concentrations of mannitol in the mannitol isotonized PXCl solutions of pH 3.0, 5.0 and 7.0 were 0.269, 0.256 and 0.257 M, respectively. The pH of the drug solution was adjusted to the desired pH by adding 1 M NaOH or 1 M HCl. PXCl was freely soluble in the buffer solutions of citrate buffer pH 3.0 and 5.0 and phosphate buffer pH 6.0 and 7.0 (solubility from 140 mg/ml to >300 mg/ml at pH 7.0 to pH 3.0, respectively) determined in a separate PXCl solubility study.
Transport Studies: General Setup
In vitro drug transport of PXCl across HEM was studied in vertical Franz diffusion cells. Prior to the experiments, HEM samples were cut into ~4 × 4 cm2 and allowed to hydrate in PBS at 4°C in a refrigerator overnight. HEM was mounted on the diffusion cells with an effective area of 1.77 cm2. The stratum corneum faced upward to the donor chamber and the viable epidermis faced the receiver chamber of the diffusion cells. A regenerated cellulose membrane (Spectra/Por®4 MWCO 12,000-14,000, Spectrum Laboratories, Inc., Rancho Dominguez, California) was placed between the viable epidermis side of the HEM sample and the receiver chamber. Prior to starting the experiment, the skin was equilibrated with PBS for 1 h. The integrity of HEM was ensured by electrical resistance measurement according to Ohm’s law. The electrical resistance of the supporting cellulose membrane was negligible compared to the skin; cellulose membrane resistance was comparable to that of the buffer solution and had no significant effect on the reading of skin resistance. In addition, there was no significant difference of drug permeability coefficient between transport experiment across HEM with and without supporting cellulose membrane in a preliminary study. HEM with electrical resistance ≥15–20 kΩ·cm2 was reported to have good integrity (19,20). Therefore, only the HEM with initial electrical resistance ≥20 kΩ·cm2 was used in the experiment. After assembly of the diffusion cells, 1 ml of drug solution was pipetted into the donor chamber. The precise amount of buffer solution (~5 ml) was added into the receiver chamber and continuously stirred with a magnetic stirrer. HEM temperature was maintained at 32 ± 1°C by a thermostat heater (Safety Thermostat 911 model, PolyScience, Niles, Illinois).
Anodal iontophoresis experiments (anode electrode in the donor) were performed by applying electric current across the HEM with an iontophoresis device (ActivaDose®II model, ActivaTek™, ActivaTek, Inc., Gilroy, California). Ag and AgCl electrodes were placed in each glass scintillation vial containing 0.3 M NaCl. The electrodes were connected to donor and receiver chambers by salt bridges to avoid the interactions between PXCl and the electrodes during iontophoresis (electrochemical reactions at the electrodes). The salt bridges were prepared by dissolving 2% (w/v) agarose in 0.3 M NaCl and filling a silicone tube with the agarose solution (21). A direct current of 0.5 mA/cm2 was applied continuously for 6 h and post-iontophoresis study was continued until 24 h.
During the transport experiments, samples of 300 μl were withdrawn from the receiver chamber at predetermined time intervals (i.e., 0, 1, 2, 3, 4, 5, 6, 9, 12, 18 and 24 h) unless stated otherwise. The same volume of fresh PBS was added back to the receiver chamber to maintain a constant volume. The samples were diluted with the mobile phase and then analyzed by HPLC. The integrity of HEM was also determined at the end of each experiment.
Table I summarizes the conditions of the permeation experiments investigated in the present study. The skin permeation studies consisted of iontophoretic transport experiments and passive transport studies after skin pretreated with iontophoresis. The details for each experiment were described in the following sections.
Transport Studies: pH Effect
The iontophoretic drug transport experiments under the asymmetric pH conditions (donor and receiver chambers had the different pH, Table I) were conducted in the Franz diffusion cells as described in the “Transport studies: general setup” section. The asymmetric condition provided data mimicking the situations in transdermal delivery in practice. Iontophoretic skin permeation of PXCl was first studied using 1 mg/ml PXCl in citrate buffer pH 5.0, phosphate buffer pH 6.0 and phosphate buffer pH 7.0 isotonized with NaCl as the donor solution to investigate the effect of pH on iontophoretic transport of PXCl. In another experiment, the donor solutions contained 1 mg/ml PXCl and 2.27 mg/ml AP in citrate buffer pH 3.0, citrate buffer pH 5.0 and phosphate buffer pH 7.0 isotonized with mannitol to examine the effect of ion composition in the drug solution on the transport hindrance/enhancement of PXCl as a function of pH. AP was included in the PXCl solution to determine the electromigration and electroosmosis contributing to iontophoretic transport of PXCl (15). The receiver solution was PBS. Passive diffusion experiments of 1 mg/ml PXCl in citrate buffer pH 5.0, phosphate buffer pH 6.0 and phosphate buffer pH 7.0 isotonized with NaCl were performed to serve as the baseline references to determine iontophoretic transport enhancement. PXCl was found to be stable with no detectable degradation under current application of 0.5 mA/cm2 for 6 h and storage at pH 3.0–7.0 for a week as shown by the greater than 90% recovery of PXCl after current application and storage in a separate study (data not shown).
Transport Studies: Iontophoresis Pretreatment
To investigate PXCl transport across iontophoresis-altered skin without the influence of iontophoresis as the driving force, passive transport experiments were performed after HEM was pretreated with iontophoresis under the asymmetric condition (Table I). Another purpose of the iontophoresis pretreatment was to provide passive PXCl fluxes that might otherwise be difficult to measure (e.g., undetectable) without the pretreatment. In the pretreatment experiment, the donor solutions of pH 3.0 and pH 7.0 were studied to examine the influence of skin permselectivity on drug transport. The donor chamber was filled with a buffer solution isotonized with mannitol at pH 3.0 or pH 7.0 without the drug. Anodal iontophoresis with constant current of 0.5 mA/cm2 was applied for 6 h in the same manner as the iontophoretic transport experiment. After switching off the current, the donor solution was removed and replaced by drug solution of the same pH isotonized with mannitol. The drug solutions used in the study contained either 1 mg/ml or 10 mg/ml PXCl and 2.27 mg/ml AP. PBS was used as the receiver solution. Passive delivery of PXCl and AP after iontophoresis pretreatment was then measured. As the passive transport of PXCl was expected to be low, the amounts of PXCl permeated across the skin from the drug solutions were determined at predetermined time intervals: (i) 36, 40, 44 and 48 h for the drug solution containing 1 mg/ml PXCl and (ii) 12, 15, 18, 21 and 24 h for the drug solution containing 10 mg/ml PXCl after pretreatment.
Transport Studies: Symmetric Condition
In iontophoretic transport study of PXCl under the symmetric condition (donor and receiver chambers had the same pH), pH 3.0 condition in both donor and receiver chambers was studied (Table I). The symmetric condition provided the data to study the transport mechanism of PXCl when the pH across HEM (from the donor to receiver) was constant. In the experiment, citrate buffer pH 3.0 isotonized with mannitol and citrate buffer pH 3.0 isotonized with NaCl were added in the donor and receiver chambers, respectively, to equilibrate HEM for 2 h. After equilibration, 1 ml of drug solution in citrate buffer pH 3.0 isotonized with mannitol containing 1 mg/ml PXCl and 2.27 mg/ml AP was added in the donor chamber. A precise amount of citrate buffer pH 3.0 isotonized with NaCl (~5 ml) was added into the receiver chamber. Anodal iontophoresis with constant direct current of 0.5 mA/cm2 was conducted for 6 h. The data from the experiment under the symmetric condition were compared with the asymmetric condition (i.e., pH 3.0 and pH 7.4 in donor and receiver chambers, respectively).
Determination of Electromigration and Electroosmosis Contribution to the Iontophoretic Transport of PXCl as a Function of pH
The electromigration and electroosmosis contribution to the iontophoretic transport of PXCl were determined by co-iontophoretic delivery of PXCl with AP (15). The steady-state flux (J) and permeability coefficient (P) were determined by using Eq. 2 and 3 (8,22):
where J was calculated from the straight line portion of the cumulative permeated amount (Q) curve of either PXCl or AP per unit area (A) against time (t) over the 6-h iontophoresis period and C is the donor solution concentration of drug.
The total iontophoretic flux (Jtotal) of a drug molecule is related to the fluxes due to electromigration (JEM), electroosmosis (JEO), and passive delivery (Jpassive). For the small value of passive delivery of PXCl due to its polar nature, Jpassive was considered to be negligible. Thus, JEM and JEO of PXCl were determined by Eq. 4 and 5, respectively (15):
where v is the average solvent flow velocity due to electroosmosis, Jtotal and JAP are steady-state fluxes of PXCl and AP across HEM and CPXCl and CAP are the donor solution concentration of PXCl and AP, respectively. It should be noted that JEO calculated by eq. 5 is an apparent value. For anodal iontophoresis with skin at pH 5.0 and 7.0 (electroosmosis enhanced transport), JEO is an accurate representation of PXCl electroosmotic flux. For anodal iontophoresis with skin at pH 3.0, JEO for PXCl is expected to be a negative value (from cathode to anode) that can be described by the Peclet number related to the apparent value obtained from Eq. 5 (see electroosmotic flux discussed in Results and Discussion).
Drug Content Analysis
Modified reverse phase HPLC methods (23) were used to assay PXCl and AP. The HPLC system consisted of an Agilent 1200 series quaternary pump, degasser, autosampler, UV-Vis diode array detector (Agilent Technologies, Inc., Santa Clara, California) and Hypersil™ BDS C18 column with a guard column (5 μm particle size, 150 mm × 4.6 mm; Thermo Fisher Scientific Inc., Waltham, Massachusetts). The mobile phase comprised acetonitrile and aqueous phase at the ratio of 3:97 (v/v). The aqueous phase contains 0.5% (v/v) triethylamine in water with its pH adjusted to 6.0 by phosphoric acid. The flow rate and injection volume were 1.0 ml/min and 50 μl, respectively. The HPLC assay was performed at room temperature. The detection wavelengths for PXCl and AP were set at 262 and 245 nm, respectively. Standard solutions at appropriate concentration ranges were used to prepare the calibration curve in the mobile phase. The linearity of calibration curves for PXCl and AP were in the range of 0.20–6.41 μg/ml (R2 = 0.999) and 0.16–10.01 μg/ml (R2 = 1.000). The limit of detection (LOD) and limit of quantitation (LOQ) for PXCl were 0.03 and 0.10 μg/ml, respectively. For AP, the LOD and LOQ were 0.02 and 0.07 μg/ml, respectively.
Data Analysis
The results were expressed as the mean ± standard deviation (SD). The statistical comparison was evaluated using either independent t-test or one-way ANOVA followed by multiple comparisons (e.g., Turkey and Dunnett method). The level of significant difference was considered at p value <0.05.
Results
Effect of pH on PXCl Iontophoretic Delivery
PX has two pKa (i.e., 5.0 and 9.6 for primary amine substituted in thiazole ring and secondary amine on the structure, respectively) indicating that PX acquires valence of +1 and + 2 when the drug ionizes with decreasing pH. Therefore, the valence of PX ions in the drug solution was controlled by the solution pH (as shown in the equilibrium conditions in Fig. 1). The extent of ionization of PX ions at each pH was calculated using Eqs. 6–8 (24) and summarized in Table II. Consequently, the pH of drug solution would affect PX iontophoretic transport across skin.
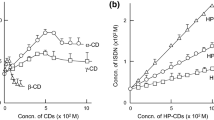
Figure 2a shows the permeation profiles of PXCl across HEM from different pH solutions isotonized with NaCl by iontophoresis in comparison with passive diffusion. The data show that passive permeation of PXCl across the HEM was low and iontophoresis significantly enhanced drug transport at each pH studied (p < 0.05; independent t-test). After 24 h passive permeation, the amounts of PXCl permeated across HEM from the drug solutions at pH 5.0, 6.0, and 7.0 were 0.58 ± 0.88, 1.38 ± 2.11, and 0.29 ± 0.27 μg/cm2, respectively. Using iontophoresis, the amounts of PXCl permeated across HEM at pH 5.0, 6.0, and 7.0 were 90 ± 22, 84 ± 14, and 102 ± 34 μg/cm2 after the 6 h current application, corresponding to J(1–6 h) of 15.3 ± 3.0, 13.9 ± 4.4, and 18.9 ± 6.7 μg/cm2·h, respectively. The amounts of PXCl permeated across HEM during iontophoresis were at least two orders of magnitude larger than those of passive permeation. The results in the figure also show no significant difference in permeated amounts and J(1–6 h) of PXCl at pH 5.0, 6.0, and 7.0 during iontophoresis (p > 0.05; one-way ANOVA).
Cumulative amount of PXCl permeated across HEM from 1 mg/ml drug solution isotonized with (a) NaCl and (b) mannitol. Symbols: pH 3.0 (triangles); pH 5.0 (circles); pH 6.0 (squares) and pH 7.0 (diamonds). Closed symbols and open symbols with solid line represent the permeation profiles of PXCl transported by passive diffusion and iontophoresis, respectively. Direct current density of 0.5 mA/cm2 was applied continuously for 6 h to PXCl solution. Each point and bar represent the mean ± SD (n = 3–4).
Figure 2b presents the permeation profiles of PXCl across HEM during iontophoresis with the drug solution isotonized with mannitol. PXCl fluxes increased significantly when the concentrations of the current-competing background ions were reduced by replacing NaCl with mannitol, a neutral molecule for adjusting the tonicity. The data also show the effect of drug solution pH on iontophoretic transport of PXCl. Although no pH effect was observed for the drug solution isotonized with NaCl (Fig. 2a), solution pH significantly affected iontophoretic transport of PX ions from the drug solution isotonized with mannitol in a pH-dependent manner. With the mannitol isotonized system, iontophoretic transport of PXCl in pH 3.0 solution was performed because 99% of PX ions have valence of +2 under this condition (Table II); this provided a closer examination of the pH effect on iontophoretic transport of PX ion at the higher net +2 valence. In the figure, the highest J(1–6 h) occurred in the pH 7.0 solution (69.7 ± 7.9 μg/cm2·h) followed by pH 5.0 solution (46.6 ± 5.6 μg/cm2·h) and pH 3.0 solution (34.3 ± 3.6 μg/cm2·h), respectively. This result was different from the prediction of electrotransport theory that reducing solution pH to increase the positive charges on PX ions should enhance its flux in anodal iontophoresis.
To compare the data with electrotransport theory, Fig. 3 presents the theoretical calculations using Eq. 1 (11,25,26). The plots show the estimated transference numbers normalized by valence (ti/z) of PX ions, co-ions and counterions in the drug solution versus pH. The theoretical calculations show that the use of NaCl for isotonicity adjustment significantly reduces the ti/z values of PX ions in the drug solution. When replacing NaCl with mannitol, the ti/z values of PX ions in the drug solution increase, which is consistent with the experimental data in Fig. 2a and b. However, different from the experimental data, the calculations show that the highest ti/z values of PX ions should occur at pH 3. This is investigated later in the “Discussion” section.
Transference number of PX ions, co-ions and counterions present in the drug solution isotonized with (a) NaCl or (b) mannitol versus pH. Symbols:  , H+;
, H+;  , PX+;
, PX+;  , PX2+;
, PX2+;  , Na+;
, Na+;  , C6H7O7-;
, C6H7O7-;  , C6H6O72-;
, C6H6O72-;  , C6H5O73-;
, C6H5O73-;  , H2PO4-;
, H2PO4-;  , HPO42-;
, HPO42-;  , Cl-;
, Cl-;  , N3-. Electrophoretic mobilities in Eq. 1 were calculated using μ = DzF/RT and μi/μj = Dizi/Djzj , where μ, D and z are the electrophoretic mobility, diffusion coefficient and valence of the ion, F is the Faraday constant, R is the universal gas constant, T is temperature, and subscripts i and j represent ion species i and H+ ion, respectively (25). The diffusion coefficients of the ions and H+ ion electrophoretic mobility were obtained from references (25, 26). PX diffusion coefficient was estimated using the diffusion coefficients of molecules with similar molecular sizes based on the relationship D = kT/6πηr, where r is the hydrodynamic radius, k is the Boltzmann constant and η is the solvent viscosity (25)
, N3-. Electrophoretic mobilities in Eq. 1 were calculated using μ = DzF/RT and μi/μj = Dizi/Djzj , where μ, D and z are the electrophoretic mobility, diffusion coefficient and valence of the ion, F is the Faraday constant, R is the universal gas constant, T is temperature, and subscripts i and j represent ion species i and H+ ion, respectively (25). The diffusion coefficients of the ions and H+ ion electrophoretic mobility were obtained from references (25, 26). PX diffusion coefficient was estimated using the diffusion coefficients of molecules with similar molecular sizes based on the relationship D = kT/6πηr, where r is the hydrodynamic radius, k is the Boltzmann constant and η is the solvent viscosity (25)
Contribution of Electromigration and Electroosmosis to Iontophoretic Transport of PXCl
The contributions of JEO and JEM to the iontophoretic flux of PXCl as a function of pH using drug solution isotonized with mannitol were summarized in Table III. The highest values of both JEO and JEM were obtained at pH 7.0 (2.01 ± 0.52 μg/cm2·h and 67.7 ± 7.5 μg/cm2·h, respectively) followed by pH 5.0 (1.20 ± 0.25 μg/cm2·h and 45.4 ± 5.6 μg/cm2·h, respectively) and pH 3.0 (0.11 ± 0.06 μg/cm2·h and 37.8 μg/cm2·h, respectively). Electromigration was 97 to 110% of the total flux of PXCl during iontophoresis, and electroosmotic flux was not greater than 10% of electromigration flux in the pH range studied. The result is in agreement with the earlier studies by Kalaria et al. (15,16) at pH 5.3 under similar anodal iontophoresis condition that electromigration is the main mechanism for transdermal iontophoretic delivery of PXCl.
Passive Transport of PXCl and AP after Skin Pretreated with Iontophoresis
Table IV summarizes the passive delivery of PXCl and AP across HEM from donor solutions of pH 3.0 and 7.0 after the membrane was pretreated with iontophoresis to investigate skin permselectivity, i.e., the partitioning of positively charged PX ions into positively and negatively charged HEM at pH 3.0 and 7.0, respectively. Assuming that the barrier properties of HEM after iontophoresis pretreatment were similar to those during iontophoresis, the results can be used to investigate the enhancement mechanisms of PXCl iontophoretic transport. In the experiment using 1 mg/ml PXCl, passive transport of PXCl at pH 3.0 was undetectable. Consequently, the LOD for PXCl was used to estimate the maximum value possible of PXCl permeation at this pH for comparison. To analyze the data, the flux and permeability coefficient of AP were used as the internal reference under each condition and the ratio of PXCl to AP permeability coefficients was determined. A significant change in the difference in permeability coefficients between PXCl and AP (i.e., the P ratio) with respect to pH changes would indicate the effect of membrane permselectivity for PXCl due to charge-charge interaction at pH 3.0 and 7.0. The data show that the passive transport of PXCl at pH 7.0 was faster than that at pH 3.0 for both 1 mg/ml and 10 mg/ml conditions (p < 0.05, independent t-test). When donor pH increased from 3.0 to 7.0, the P ratios increased by at least 13-fold and approximately 4-fold for the 1 mg/ml and 10 mg/ml PXCl solutions, respectively.
Iontophoretic PXCl Transport across HEM under Symmetric Condition
Table V summarizes the iontophoretic transport of PXCl and AP in citrate buffer pH 3.0 isotonized with mannitol in the asymmetric and symmetric permeation studies. The iontophoretic transport of PXCl (J and JEM) under symmetric condition (18.4 ± 2.4 μg/cm2·h and 17.6 ± 1.4 μg/cm2·h, respectively) was approximately 2-fold smaller than that under asymmetric condition (34.3 ± 3.6 μg/cm2·h and 34.2 ± 3.6 μg/cm2·h, respectively) (p < 0.05, independent t-test). No change in the AP transport and JEO was observed between the asymmetric (0.24 ± 0.14 μg/cm2·h and 0.11 ± 0.06 μg/cm2·h, respectively) and symmetric (0.25 ± 0.09 μg/cm2·h and 0.10 ± 0.04 μg/cm2·h, respectively) conditions.
Discussion
Iontophoresis-Enhanced Transdermal Delivery of PXCl and Effect of pH
Transdermal iontophoresis is a promising technique which utilizes an electric field as the driving force to enhance the transport of charged and uncharged drugs across skin. Iontophoretic drug transport is influenced by several factors such as pH and ion composition of the drug solution. The pH of a solution has a significant effect on iontophoretic transport of ionic drugs because it governs the degree of drug ionization as well as the charges in skin membrane (9). PX is a weak base with two pKa values (i.e., 5.0 and 9.6). The drug completely ionizes at pH below 7.6 and the ability of PXCl to permeate across skin is low by passive transport (Fig. 2a). Therefore, the application of electric current can increase skin permeation of PXCl. The result in this study is consistent with iontophoresis-enhanced transport for effective transdermal delivery of a charged molecule, and iontophoretic transport of PXCl is mainly a result from electromigration whereas the effects of electroosmosis and passive transport are small (9).
The efficiency of an ion as a charge carrier during an electrotransport process can be evaluated by the transference number of the ion (11). Increasing the valence of the target ion (Eq. 1) provides a higher transference number and subsequently more efficient iontophoretic transport. Thus, increasing the valence of positively charged PX, a function of the donor pH (Fig. 1 and Table II), could improve its iontophoretic transport. To compare the results between the drug solutions isotonized with NaCl and mannitol, the low transference number of PX ion in the solution isotonized with NaCl (Fig. 3a), which contained relatively high concentration of Na+ (~0.16 M) and Cl− ions (~0.15 M) to PX ions (3.31 mM) is in general agreement with electrotransport theory; i.e., drug transference number is usually low when there is a relatively high concentration of current-competing ion compared to that of the drug in iontophoretic delivery (10,11). The fraction of current carried by PX ions during iontophoresis is low and inadequate to observe a significant difference in iontophoretic transport of PXCl as a function of pH under these conditions (Fig. 2a). In addition to the ion competition effect, solution ionic strength impacts the electrophoretic mobilities of ions. The higher ionic strength of the drug solution isotonized with NaCl would decrease ion electrophoretic mobilities (Onsager theory on ion conductivity) and affect ions of larger sizes and higher valence more than small monovalent ions (27,28). Avoiding extraneous electrolyte for tonicity adjustment allows cationic PX to be delivered efficiently by iontophoresis. In the present study, pH-dependent iontophoretic transport of PXCl was observed when NaCl was replaced by mannitol for isotonicity adjustment (Fig. 2b) supporting that the insignificant pH effect on the iontophoretic transport of PXCl in the solution isotonized with NaCl could be attributed to these factors.
An interesting finding in the present study was the opposite effect of pH on iontophoretic transport of PXCl in drug solution isotonized with mannitol (Fig. 2b) compared to the trend predicted by electrotransport theory (Fig. 3b). The theory suggests that the iontophoretic transport of PXCl should be most efficient in the drug solution of pH 3.0 among the pH studied when the valence of PX ion increases. In this respect, the following factors are considered: (i) the decrease in iontophoretic transport due to the change in electroosmosis (29,30) and (ii) the hindrance of drug transport due to the decrease in partitioning of drug into the charged skin membrane as a result of charge-charge interactions (skin cation permselectivity) (30,31,32). PXCl was stable with no detectable degradation under the conditions studied as shown by the greater than 90% recovery of PXCl after iontophoresis application (data not shown), which could be attributed to the use of the salt bridges in the present study.
Contribution of Electroosmosis to the Iontophoretic Transport of PXCl as a Function of pH
Since the human skin has pI value of approximately 4.8 (14), the skin becomes net positively charged at solution pH lower than the pI (different from its negatively charged state at physiological pH above the pI) (14). The charge density of the skin transport pathways is a continuous function with respect to pH. When the pH decreases from pH 7.0 to 3.0, the skin transport pathways change from net negatively charged to positively charged. For anodal iontophoresis, decreasing donor solution pH would decrease the electroosmosis contribution to iontophoretic enhancement of cationic drug transport (29). At pH below the pI value, electroosmosis has a negative impact on anodal iontophoretic transport enhancement. This phenomenon is supported by the results of AP showing larger electroosmosis contribution at pH 7.0 compared to that at pH 5.0 and the retardation effect of electroosmosis at pH 3.0 (Table III). Assuming skin pI of 4.8 and interpolation to estimate the AP flux at this pH, the Peclet numbers of electroosmosis were determined to be −3.5 and 1.6 at pH 3.0 and pH 7.0, respectively, using the electroosmosis enhancement theory (33,34). Although this observation is in agreement with the smaller PXCl flux enhancement at pH 3.0 compared with that at pH 7.0 in the present study, the effect of electroosmosis in the studied pH range is relatively small as compared to electromigration and cannot be used to explain the pH-dependent PXCl data. The present AP results are consistent with (i) the transport theory that the contribution of electroosmosis is generally small for a small ionic permeant in transdermal iontophoresis (10,35) and (ii) the findings at pH 5.3 in previous studies (15,16). It should be noted that the present data interpretation did not take into account specific interactions between PX and skin (e.g., PX binding) and assumed that the ions are point charges. Therefore, the iontophoretic transport behaviors of other multivalent cationic drugs could be different from those of PX observed in this study.
PX Ion Permeation at pH below Skin pI and Mechanism of pH-Dependent PX Permeation
Skin behaves as a permselective membrane to ionic compounds (36). This skin property is one of the determinants for ion permeation across skin during iontophoresis (37). The skin can be positively or negatively charged depending on the pH and composition of formulation in contact with the skin (pI = 4.8). PX, as a cationic drug, can interact with the skin via charge-charge interactions. Considering the charge-charge interactions between the skin and cationic PX when the solution pH is below or above skin pI, skin permselectivity could significantly hinder the iontophoretic transport of PX at pH 3 (when solution pH < skin pI) or facilitate iontophoretic transport at pH 7 (when solution pH > skin pI). To investigate the charge-charge interactions in skin transport, passive transport experiments (without the impact of the electric field on PX permeation) were performed at pH 3.0 and pH 7.0 after the skin was pretreated with iontophoresis. The pH 3.0 and 7.0 conditions were selected so the transport of PXCl across the negatively and positively charged skin (at pH 7.0 and pH 3.0, respectively) could be compared. The lower permeability of skin to PXCl at pH 3.0 than pH 7.0 under both PXCl concentrations (Table IV) can be attributed to the decrease in drug partitioning into the skin via charge-charge interaction between PXCl and the positively charged skin. The larger effect observed at the lower PXCl concentration (increase in P ratio difference of >13-fold at 1 mg/ml from ~4-fold at 10 mg/ml) is consistent with the stronger charge-charge interactions (thicker Debye– Huckel layer) at the lower ionic strength in 1 mg/ml drug solution (28,38). The data are consistent with the negatively charged skin providing preferential permeation of PX+ ions at pH 7. When the skin becomes positively charged at pH 3.0, the membrane repels the positively charged PX, resulting in transport hindrance. Such charge-charge interactions and the corresponding effects are commonly observed in ion transport across biological membranes (11,39). Although the exact locations of the iontophoretic transport pathway and charge-charge interactions between the cationic PX and skin are not known, previous studies have provided information on this topic (40,41,42,43). In the present study, the decrease in electromigration (iontophoretic transport) with the decrease in donor solution pH is consistent with this skin permselectivity effect, which is likely to be a key factor in the iontophoretic transport of PXCl.
Conducting iontophoresis experiment under a symmetric condition with respect to the donor and receiver chambers can provide additional insights into the transport mechanisms during iontophoresis. Under the asymmetric condition, membrane pH could be influenced by the pH in the donor and receiver solutions. As membrane pH is the determining factor of PX ionization and membrane iontophoretic transport, the pH of the receiver solution (pH 7.4) could affect membrane transport and mask the pH effect of the donor solution in the present study (32,44). Under the symmetric condition, the data can be interpreted without the complication of a pH gradient in skin membrane under the asymmetric condition (i.e., donor pH 3.0, receiver pH 7.4, and skin pH between 3.0 and 7.4). The present study showed that PXCl transport decreased when the pH of the environment in the membrane decreased due to the symmetric condition of pH 3.0 (i.e., due to the decrease in the pH of the receiver solution), whereas the AP transport and JEO in both asymmetric and symmetric permeation studies were essentially the same (Table V). The results in the present study suggest that electroosmosis in the membrane was not significantly affected by the receiver solution pH under the conditions studied, similar to those observed in a previous study (32). Electroosmosis was mainly controlled by the donor solution pH. The decrease in the pH in the membrane, if any, due to the decrease in pH of the receiver solution under the symmetric condition (vs. the asymmetric condition) leads to a further decrease in the flux of PXCl; this effect is consistent with the decrease of PXCl permeation due to skin permselectivity when pH decreases. This rejects the notion that the lack of iontophoretic enhancement under the asymmetric condition (pH 3.0 donor solution and pH 7.4 receiver solution) was a result of the membrane pH being significantly influenced by the receiver solution. At the same time, this supports the conclusion that skin permselectivity due to charge-charge interactions between cationic PX and the skin could be a main factor contributing to the observed iontophoresis results of PXCl. When the skin gradually changed from net negatively charged to slightly negatively charged and then positively charged, the highest Jtotal was observed at pH 7.0 followed by 5.0 and 3.0, respectively, as a result from the different magnitudes of cation permselectivity of skin to cationic PX.
Conclusion
The present study demonstrates that the iontophoretic transport of PXCl was influenced by the pH and the presence of competing ions for the electric current in the donor solution. Iontophoresis of PXCl solution buffered at pH 7.0 and isotonized with mannitol provided the highest PX flux among the conditions studied. Decreasing the solution pH to increase the net valence of positively charged PX ion has a negative impact on its iontophoretic transport. The results from the analyses of electroosmosis, iontophoretic drug transport under symmetric condition, and the pH effect on passive permeation of PXCl after iontophoresis pretreatment suggest that the pH-dependent characteristic of PXCl transport during iontophoresis was mainly related to cation-permselectivity of the skin rather than the effect of electroosmosis. Skin permselectivity, consisting of drug to membrane pathway partitioning via charge-charge interactions, could play a major role in the electrotransport of PXCl at pH below the skin pI. This observation is different from the belief that electroosmosis is the major cause of the slower anodal iontophoretic transport of cationic drugs when the pH is below the skin pI.
Acknowledgments and Disclosures
This research was financially supported by the Thailand Research Fund (TRF) through the Royal Golden Jubilee (RGJ) Ph.D. Program (Grant No. PHD/0210/2559) to Kamchai Saepang and supported in part by BRAND’S Health Research Awards 2019 to Doungdaw Chantasart.
Abbreviations
- AP:
-
Acetaminophen
- c :
-
Concentration for ion
- J EM :
-
Electromigration flux
- J EO :
-
Electroosmosis flux
- μ :
-
Electrophoretic mobility
- HPLC:
-
High performance liquid chromatography
- HEM:
-
Human epidermal membrane
- HCl:
-
Hydrochloric acid
- pI:
-
Isoelectric point
- LOD:
-
Limit of detection
- LOQ:
-
Limit of quantitation
- J Passive :
-
Passive delivery flux
- P :
-
Permeability coefficient
- PBS:
-
Phosphate buffered saline
- PXCl:
-
Pramipexole dihydrochloride
- PX:
-
Pramipexole
- J :
-
Steady-state flux
- NaCl:
-
Sodium chloride
- NaOH:
-
Sodium hydroxide
- v :
-
Solvent flow velocity due to electroosmosis
- SD:
-
Standard deviation
- J total :
-
Total iontophoretic flux
- t i :
-
Transference number
- z :
-
Valence for ion
References
Keränen T, Tuhkasaari M, Kuusisto H. Long-term retention rate of pramipexole in the treatment of Parkinson’s disease. Eur J Clin Pharmacol. 2009;65(9):955–6.
Wong KS, Lu CS, Shan DE, Yang CC, Tsoi TH, Mok V. Efficacy, safety, and tolerability of pramipexole in untreated and levodopa-treated patients with Parkinson's disease. J Neurol Sci. 2003;216(1):81–7.
Antonini A, Barone P, Ceravolo R, Fabbrini G, Tinazzi M, Abbruzzese G. Role of pramipexole in the management of Parkinson’s disease. CNS Drugs. 2010;24(10):829–41.
Olanow CW, Obeso JA, Stocchi F. Continuous dopamine-receptor treatment of Parkinson's disease: scientific rationale and clinical implications. Lancet Neurol. 2006;5(8):677–87.
Nutt JG. Continuous dopaminergic stimulation: is it the answer to the motor complications of levodopa? Mov Disord. 2007;22(1):1–9.
Mirapex Product Monograph [Internet]. Canada: Boehringer Ingelheim (Canada) Ltd.; 2020 [updated 2020 March 19; cited 2020 July 20]. Available from: https://www.boehringer-ingelheim.ca/sites/ca/files/documents/mirapexpmen.pdf.
Barry BW. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur J Pharm Sci. 2001;14(2):101–14.
Naik A, Kalia YN, Guy RH. Transdermal drug delivery: overcoming the skin’s barrier function. Pharm Sci Technol Today. 2000;3(9):318–26.
Kalia YN, Naik A, Garrison J, Guy RH. Iontophoretic drug delivery. Adv Drug Deliv Rev. 2004;56(5):619–58.
Li SK, Hao J, Liddell MR. Electrotransport across membranes in biological media: Electrokinetic theories and applications in drug delivery. In: Becker S, Kuznetsoy A, editors. Transport in Biological Media. Philadelphia: Elsevier; 2013. p. 417–54.
Phipps JB, Gyory JR. Transdermal ion migration. Adv Drug Deliv Rev. 1992;9(2–3):137–76.
Siddiqui O, Roberts MS, Polack AE. The effect of iontophoresis and vehicle pH on the in-vitro permeation of lignocaine through human stratum corneum. J Pharm Pharmacol. 1985;37(10):732–5.
Green PG, Hinz RS, Cullander C, Yamane G, Guy RH. Iontophoretic delivery of amino acids and amino acid derivatives across the skin in vitro. Pharm Res. 1991;8(9):1113–20.
Marro D, Guy RH, Delgado-Charro MB. Characterization of the iontophoretic permselectivity properties of human and pig skin. J Control Release. 2001;70(1–2):213–7.
Kalaria DR, Patel P, Merino V, Patravale VB, Kalia YN. Controlled iontophoretic delivery of pramipexole: electrotransport kinetics in vitro and in vivo. Eur J Pharm Biopharm. 2014;88(1):56–63.
Kalaria DR, Singhal M, Patravale V, Merino V, Kalia YN. Simultaneous controlled iontophoretic delivery of pramipexole and rasagiline in vitro and in vivo: transdermal polypharmacy to treat Parkinson’s disease. Eur J Pharm Biopharm. 2018;127:204–12.
Balicki R, Sypniewski M, Ciesielska A, Szelejewski W, Zagrodzka J, Cieplucha G, inventors; Instytut Farmaceutyczny, assignee. Process for the preparation of pramipexole base and/or its salts. United States patent US 20090105483. 2009 Apr 23.
Kligman AM, Christophers E. Preparation of isolated sheets of human stratum corneum. Arch Dermatol. 1963;88(6):702–5.
Chantasart D, Sa-Nguandeekul P, Prakongpan S, Li SK, Higuchi WI. Comparison of the effects of chemical permeation enhancers on the lipoidal pathways of human epidermal membrane and hairless mouse skin and the mechanism of enhancer action. J Pharm Sci. 2007;96(9):2310–26.
Kasting GB, Bowman LA. DC electrical properties of frozen, excised human skin. Pharm Res. 1990;7(2):134–43.
Charoenputtakun P, Li SK, Ngawhirunpat T. Iontophoretic delivery of lipophilic and hydrophilic drugs from lipid nanoparticles across human skin. Int J Pharm. 2015;495(1):318–28.
Dutet J, Delgado-Charro MB. Transungual iontophoresis of lithium and sodium: effect of pH and co-ion competition on cationic transport numbers. J Control Release. 2010;144(2):168–74.
Malenović A, Janić-Stojanović B, Vemić A, Ivanović D, Medenica M. Validation of a column liquid chromatographic method for the analysis of pramipexole and its five impurities. J AOAC Int. 2010;93(4):1102–12.
Kim CJ. Ionic equilibrium. Advanced Pharmaceutics: Physicochemical Principles. Boca Raton: CRC Press; 2004. pp. 45–112.
Atkins P, Paula J. Molecules in motion. Physical Chemistry. UK: Oxford University Press; 2010. pp. 745–81.
Vanýsek P. Ionic conductivity and diffusion at infinite dilution. In: Haynes WM, editor. CRC Handbook of Chemistry and Physics. 93rd ed. Boca Raton: CRC Press; 2012. p. 77–9.
Craane-van Hinsberg WHM, Bax L, Flinterman NHM, Verhoef J, Junginger HE, Boddé HE. Iontophoresis of a model peptide across human skin in vitro: effects of iontophoresis protocol, pH, and ionic strength on peptide flux and skin impedance. Pharm Res. 1994;11(9):1296–300.
Smith KA, Hao J, Li SK. Effects of ionic strength on passive and iontophoretic transport of cationic permeant across human nail. Pharm Res. 2009;26(6):1446–55.
Volpato NM, Santi P, Colombo P. Iontophoresis enhances the transport of acyclovir through nude mouse skin by electrorepulsion and electroosmosis. Pharm Res. 1995;12(11):1623–7.
Nugroho AK, Li L, Dijkstra D, Wikström H, Danhof M, Bouwstra JA. Transdermal iontophoresis of the dopamine agonist 5-OH-DPAT in human skin in vitro. J Control Release. 2005;103(2):393–403.
Burnette RR, Ongpipattanakul B. Characterization of the permselective properties of excised human skin during iontophoresis. J Pharm Sci. 1987;76(10):765–73.
Lai PM, Roberts MS. Epidermal iontophoresis: II. Application of the ionic mobility-pore model to the transport of local anesthetics. Pharm Res. 1998;15(10):1579–88.
Peck KD, Srinivasan V, Li SK, Higuchi WI, Ghanem AH. Quantitative description of the effect of molecular size upon electroosmotic flux enhancement during iontophoresis for a synthetic membrane and human epidermal membrane. J Pharm Sci. 1996;85(7):781–8.
Li SK, Ghanem AH, Higuchi WI. Pore charge distribution considerations in human epidermal membrane electroosmosis. J Pharm Sci. 1999;88(10):1044–9.
Pikal MJ. The role of electroosmotic flow in transdermal iontophoresis. Adv Drug Deliv Rev. 2001;46(1–3):281–305.
La Count TD, Kasting GB. Human skin is permselective for the small, monovalent cations sodium and potassium but not for nickel and chromium. J Pharm Sci. 2013;102(7):2241–53.
Roberts MS, Lai PM, Anissimov YG. Epidermal iontophoresis: I. development of the ionic mobility-pore model. Pharm Res. 1998;15(10):1569–78.
Peck KD, Ghanem AH, Higuchi WI, Srinivasan V. Improved stability of the human epidermal membrane during successive permeability experiments. Int J Pharm. 1993;98(1–3):141–7.
Hao J, Li SK. Mechanistic study of electroosmotic transport across hydrated nail plates: effects of pH and ionic strength. J Pharm Sci. 2008;97(12):5186–97.
Turner NG, Guy RH. Iontophoretic transport pathways: dependence on penetrant physicochemical properties. J Pharm Sci. 1997;86(12):1385–9.
Uitto OD, White HS. Electroosmotic pore transport in human skin. Pharm Res. 2003;20(4):646–52.
Chizmadzhev YA, Indenbom AV, Kuzmin PI, Galichenko SV, Weaver JC, Potts RO. Electrical properties of skin at moderate voltages: contribution of appendageal macropores. Biophys J. 1998;74(2):843–56.
Chizmadzhev YA, Kuzmin PI, Weaver JC, Potts RO. Skin appendageal macropores as a possible pathway for electrical current. J Investig Dermatol Symp Proc. 1998;3(2):148–52.
Ackaert OW, Van Smeden J, De Graan J, Dijkstra D, Danhof M, Bouwstra JA. Mechanistic studies of the transdermal iontophoretic delivery of 5-OH-DPAT in vitro. J Pharm Sci. 2010;99(1):275–85.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saepang, K., Li, S.K. & Chantasart, D. Effect of pH on Iontophoretic Transport of Pramipexole Dihydrochloride across Human Epidermal Membrane. Pharm Res 38, 657–668 (2021). https://doi.org/10.1007/s11095-021-03001-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-021-03001-3