Abstract
Laparoscopic liver resections are frequently performed for peripheral lesions located in the antero-inferior segments. Resection of postero-superior segments is more demanding and dangerous than other segmentectomies, resulting in a longer operation time and increased blood loss. To reduce technical challenges, some authors advocated a modified surgical approach for these segments with the patient placed in the left lateral decubitus with the right arm suspended and suggested technical variations like the use of an additional intercostal trocar, the placement of one or two additional trans-thoracic trocars, a hand-assisted approach or a hybrid method with a median laparotomy. In the present series of 88 patients from four hepatobiliary centers with high volume of activity in Italy, a standard lithotomic position has been routinely used without the need for left lateral decubitus or semi-prone position and through abdominal wall without use of trans-thoracic trocars. This approach allows a more comfortable use of the Pringle maneuver that we used routinely in hepatic resection for PS segments; and, a very short time is needed for conversion, whenever it is required. In our series, laparoscopic resection of liver tumors located in the postero-superior segments of the liver with a total abdominal approach is technically feasible and safe with short-term results similar to other laparoscopic liver resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decade, laparoscopic liver resections (LLR) have been increasingly performed worldwide [1]. Results from a systematic review indicated that LLR are associated with reduced blood loss, less analgesics requirement and shorter length of hospital stay, despite similar complication rates and oncological outcomes as compared with open hepatectomies [2, 3]. Moreover, in a recent retrospective analysis of liver resections for benign tumors, also quality of life in the first year after LLR was proved to be improved compared with open surgery [4].
In the world review by Nguyen, minor hepatectomies, including segmentectomies and wedge resections, were the most commonly performed procedures (45 %) whereas major hepatectomies accounted for only 16 % of the entire group of laparoscopic hepatectomies [2]. These findings were also confirmed by Aldrighetti in a large national survey regarding minimally invasive liver resections and collecting data from 39 centers in Italy: indeed, out of 1391 laparoscopic liver resections (excluding conversions) 1269 cases (86.9 %) of minor liver resections were recorded [5].
LLR included in the literature series are frequently performed for the treatment of peripheral lesions located in the so-called “laparoscopic segments”, i.e., the antero-inferior segments (2, 3, 4b, 5 and 6) according to the Louisville statements [1]. Other recommendations to schedule a patient to laparoscopic liver resection include solitary, peripherally located lesions with size of less than 5 cm [1].
To our knowledge, no comparative studies assessing the possible benefits of LLR compared to open surgery for lesions located in the postero-superior (PS) segments (7, 8, 4a) have been reported so far [1, 6].
In particular, resection of segments 7 and 8 could be more demanding and potentially more dangerous than other segmentectomies, resulting in a longer operation time and increased blood loss as found in the series of Ishizawa [7]. Such “demanding” segmentectomies should be performed only by surgeons with advanced experience both in open and minimally invasive surgery [7].
To reduce technical challenges, some authors advocated a modified surgical approach for these segments with the patient placed in the left lateral decubitus with the right arm suspended and suggested technical variations like the use of an additional intercostal trocar [7], the placement of one or two additional trans-thoracic trocars [8], a hand-assisted approach [9] or a hybrid method with a median laparotomy [10].
The aim of the present study was to analyze surgical technique of resections performed for lesions located in PS segments, focusing on safety and feasibility of these procedures in the standard lithotomic position and a totally abdominal approach.
Materials and methods
From January 2005 to February 2014, a total of 88 consecutive patients underwent LLR for lesions located in segments 7 and 8 at four hepatobiliary centers with high volume of activity in Italy (Unit of Hepatobiliary Surgery and Liver Transplant Center, “Cardarelli” Hospital Naples, HPB Surgery and Liver Transplantation Unit University of Modena and Reggio Emilia Modena, Multiorgan Transplantation Program General Surgery and Transplantation Unit San Camillo Hospital Rome and Hepatobiliary Surgery, Department of Surgery San Raffaele Hospital Milan).
Patients with any of the following characteristics were excluded from the analysis: major hepatectomies, multiple lesions involving anterior or left segments. Data from these patients were collected at each center in a prospective database and are now retrospectively reviewed.
Surgical technique
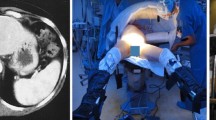
Under general anesthesia, patients were placed in a supine position with the first surgeon between patient’s legs (a left lateral decubitus position of 15°–25° was employed) and one assistant on each side. All the patients were placed in anti-Trendelenburg position. After the introduction of a 12-mm umbilical port using an open technique, continuous carbon dioxide pneumoperitoneum was induced at a pressure limit of 12 mmHg. A four-trocar configuration was generally used: two 5- to 12-mm trocars were introduced in the right and left flank (two transverse fingers above the umbilical line) and another (5 mm) in the xiphoid region (Fig. 1). In all the cases an intraoperative laparoscopic ultrasonography was performed to confirm the number and the extension of the lesions and their positions in relation to the main intrahepatic structures.
The hepatic pedicle was systematically encircled with a sling in case of requirement of Pringle maneuver.
Then, mobilization of the right liver was performed by dividing the right lateral hepatic and the triangular ligaments. Dissection of the round ligament was generally avoided to preserve its function of suspensory element. Resection was carried out by means of bipolar forceps and dissection devices, according to surgeons’ preference, following a resection plane that was previously demarked thanks to the aid of the ultrasound guide. The liver parenchyma was thinned until collateral veins and main pedicles were isolated and eventually divided by means of vascular staplers or clips. Intermittent pedicle clamping was performed, whenever required, via an accessory trocar in the left flank on the anterior axillary line; a 10/15-min clamping period, followed by 5 min of reperfusion, was used: presence of underlying liver parenchymal impairment did not constitute a contraindication to Pringle maneuver [11–13].
The specimens were placed in a plastic retrieval bag and extracted via an accessory Pfannenstiel incision or through a previous laparotomy line in the case of colorectal metastases. The surgical field was irrigated and checked for bleeding or bile leakage. A Jackson–Pratt-like drainage was placed on the raw surface of the liver whenever required. Occasionally a hemostatic matrix (Floseal©) was used to control minor bleeding centrally on the resection area. The use of laparoscopic stitches to control for deep bleeding control was generally avoided.
Outcome analysis
Patients and disease characteristics were recorded. Outcome was evaluated in terms of intraoperative outcomes (blood loss, transfusion rate, conversion rate) and postoperative results. Complications were reviewed for 90 days following surgery and graded retrospectively according to Clavien–Dindo classification of surgical complications [14]. Mortality was defined as any death occurring during the 90 days following surgery or within the same hospitalization.
Statistics
The average values are expressed as mean ± standard deviation from the mean or as median and range when appropriate. Statistical analysis was performed using SPSS software version 18.0 (SPSS Inc, Chicago, IL).
Results
Diagnosis breakdown is reported in Table 1. Among 88 patients in the study group, 46 had a hepatocellular carcinoma (HCC): most of these lesions raised within underlying cirrhosis (Child–Pugh score A5 in all patients) with no portal hypertension, no ascites and a platelet count >100 × 109/L.
Twenty-five cases of colorectal metastases and 7 cases of benign lesions were included.
Type of resections according to Brisbane nomenclature [15] and involved segments are shown in Table 1.
Mean lesion diameter was 3.3 cm (SD 1.6 cm). Conversion rate was 11.4 % (10/88) in all cases related to a severe bleeding.
Mean operative time was 204.4 min (SD 65.8 min) with a mean blood loss of 206.2 ml (SD 164.6 ml). No patient required intraoperative transfusion of packed red cell.
The intermittent Pringle maneuver was used in all patients with a mean length of 30.1 min (SD 15.5 min). Recovery of bowel function was registered after a mean of 1 day following surgery, while oral food intake was restored during the second postoperative day in all the patients.
Mean length of postoperative hospital stay was 4 days [registered (r.): 3–10].
The morbidity rate was 10.08 % (9/88 patients). According to Clavien–Dindo classification [14], 2 patients had a grade I (2.2 %), 5 patients had a grade II (5.7 %) and 2 patients (2.2 %) a grade III complication (Table 2). In particular, no patient developed postoperative ascites, allowing to remove surgical drain a median of 3 days after surgery. Mortality was nil.
Postoperative serum AST, ALT and total bilirubin levels were normal after 5 and 30 days following surgery in all the patients.
Discussion
The laparoscopic approach was proved to improve the outcomes of patients undergoing hepatic surgery in terms of reduced postoperative pain, less operative trauma, and shorter hospital stay with faster functional recovery and better quality of life, as compared to open surgery, despite comparable oncological results [4, 16]. The mean length of stay after laparoscopic surgery is 1–3 days compared with 9 days after open resection [2, 17]. Some reports suggest that the lower complication rate and the shorter length of stay after LLR might be related to a very selective inclusion criterion for laparoscopic group, leading to the recruitment of a population with favorable characteristics, like the absence of previous liver surgery [2, 6].
The selection of “less challenging” patients, often requiring small non-anatomical resections in peripheral segments or left lateral sectionectomy as their first hepatectomy is a feature of many series.
Moreover, historical indications for laparoscopic liver resection were small, solitary, and easily accessible peripheral (segments 2–6) lesions [1].
After the continuous and progressive training both in general laparoscopic and open liver surgery, an evolution from relatively modest peripheral wedge resections to left lateral sectionectomies and then to formal right hepatectomies was experienced; despite this, even most specialized institutions still underline the difficulty of posterior segmental resections: indeed, only a small number of patients resected laparoscopically for lesions located in the segments 7 and 8 were reported [1, 2, 18, 19].
More recently, outcomes from small cohorts of patients have been published, focusing on laparoscopic liver resection for complex posterior and superior lesions in segments 7 and 8: even in this setting technical feasibility has been reported, despite notoriously poor operative exposure and difficult bleeding control [20].
These formerly restricted areas have now been more widely explored, thanks to technological improvement and surgeons’ learning curve, while preserving oncological principles and profile of safety and efficacy in high-volume centers [21, 22].
Exposure of surgical field, liver mobilization and working instruments manipulation may be particularly challenging during segmentectomies and wedge resections for lesions located in PS segments. Moreover, the transection line is more frequently curved or angulated, making liver parenchymal dissection more difficult.
Additionally, the enforced angle of transection imposed by the ribs frequently leads to an unnecessarily generous anterior margin to achieve a radical (R0) resection: as a consequence, some authors have abandoned a pure laparoscopic approach due to the rate of conversion for bleeding and the difficulties to achieve an R0 margin [21].
On the contrary, when a pure laparoscopic approach is pursued, the surgeon may be induced to perform a formal right hepatectomy rather than a more demanding procedure like right posterior sectionectomy or segmentectomies of 7 and 8. Nevertheless, recent trend toward parenchymal sparing techniques in open liver surgery has pushed in the direction of a more conservative attitude also in the laparoscopic approach [23, 24].
In this series we observed a mean tumor-free margin of about 10 mm with no cases of R1 resection.
In trained centers, LLR of PS segments was not associated with increased morbidity when compared with LLR of anterolateral segments and similar results were shown also in terms of intraoperative and postoperative outcomes [7, 20, 21, 25]. In a paper by Kazaryan, the only statistically significant difference found was regarding the minimal distance from the resection line to the tumor (3 mm for resections of PS segments vs. 8 mm in other segments, p = 0.003) [25]. It should be taken into consideration that these results are altered by a more extensive use of vascular staplers when resection of PS segments is required: indeed, parenchymal crushing by the cartridge reduces the depth of resection margins [26]. More recently Postriganova et al. have also reported the effect of dissection devices that can narrow the resection margin due to thermal necrosis [27]. This seems to be an isolated report from the literature; indeed this observation did not lead to a higher rate of tumor-involved resection margins, to a higher rate of recurrence within the liver, or to a poorer survival in patients with resections of lesions located in PS segments [27]. Our results are similar in terms of resection margins with probably more narrow margins compared to other less demanding laparoscopic segmentectomies but without R1 resections.
The most important issue approaching LLR is patient’s position and trocars placement.
In the present series a standard lithotomic position has been routinely used without the need for left lateral decubitus or semi-prone position, and even trocars placement was regularly performed through abdominal wall without use of trans-thoracic trocars as proposed by Ikeda [28].
This approach allows a more comfortable use of the Pringle maneuver that we used routinely in hepatic resection for PS segments; and a very short time is needed for conversion, whenever it is required.
According to what was suggested by Cho [20], routine pedicle clamping for LLR of poster-lateral segments was adopted in the present series, given its benefits in terms of blood loss reduction during a liver resection for technical demanding segments without any detrimental consequence for liver function and long-term results [29].
Chiow et al. compared outcome of patients undergoing a resection of a single lesion in segments 7 and/or 8 with an intercostal trans-thoracic trocars (8 patients) with patients scheduled for a standard pure laparoscopic approach (11 patients) [30]. They concluded that both techniques were complementary: however, in the pure laparoscopic group median lesion diameter was bigger (26 mm r.: 10–50 mm vs. 20 mm r.: 6–34) even without statistical difference as well as the resection margins, (6 mm r.: 5–0.28 vs. 3.5 mm r.: 1–11) suggesting a selection bias with patients with a major risk of R1 resections performed by the intercostal approach [30].
In LLR of postero-lateral segments, as already reported by some authors the conversion rate was higher compared to procedures performed in other liver segments [7, 20].
In a series of LLR by Cho, four conversions were described and three of these (10.7 % of the series, 75 % of conversions) occurred in candidates to postero-lateral segments resections [20].
In the series by Ishizawa, ten out of 62 laparoscopic segmentectomies involved segments 7 and 8 with 10 % of conversion rate for prolonged operative time. In the same paper in seven segmentectomies for postero-lateral segments performed with the patient in lateral decubitus, a pneumoperitoneum leak into the pleural space at the site of intercostal trocar occurred and evacuation through an 18-gauge angiocatheter was necessary: anyway, placement of a prophylactic chest tube was never required nor lung injuries and postoperative pneumothorax occurred [7].
Similarly Lee [31] described no postoperative morbidity related to bleeding, biliary leakage, pneumonia, and pneumothorax in 5 patients with lesion located in segments 7 and 8 approached by trans-thoracic access though two additional intercostal ports placed at the 7th and 9th intercostal spaces.
In this series, a conversion rate of 11.4 % with a mean operative time of 204 min was observed.
The experience reported by Ishisawa is similar (180–240 min for segment VII and 132–240 min for segment VIII) [7].
In the present series, we observed a mean blood loss of 206.2 ml (SD 164.6) comparable to those reported by most of the authors.
Furthermore, in our series postoperative AST, ALT and total bilirubin were back to normal levels 5 and 30 days after surgery in all the patients with no evidence of postoperative ascites.
The list of complications, according to Dindo–Clavien classification, is reported in Table 2.
In Dokmak’s experience, the risk of biliary fistula after an anatomical S8 resection is higher compared with a right hepatectomy (20 vs. 6 %; p = 0.07) [32]. Although in the Ishisawa experience there is no mention of bile leakage (in present experience one case is reported) we think that avoiding an intercostal trocar can somehow protect patients from the risk of bilio-pleural fistula [7].
As far as the instrument of dissection concerns, the use of the harmonic scalpel, (that we routinely use in laparoscopic liver surgery as well as most of centers performing LLR) seems to be associated with an increased risk of biliary fistula compared with the clamp crushing technique that is unusable with a laparoscopic approach.
Kim [33] compared two groups of patients based on the technique of resection in open surgery: harmonic scalpel [53 % (n = 79)] versus clamp crushing [47 % (n = 70)]. The use of the harmonic scalpel was associated with a significant increase in biliary fistulas [24 % (n = 19) vs. 7 % (n = 5); p = 0.01] [33].
So, we consider that a trans-thoracic approach may lead to a risk for bilio-pleuric fistula.
Dissection by means of Cavitron Ultrasonic Surgical Aspirator (CUSA; Integra Lifesciences, Plainsboro, NJ, USA) might reduce this incidence.
However, in a recent study comparing ultrasonic device and a bipolar compression device the incidence of bile leak after LLR was similar (0/19 vs. 1/35, p = 0.531) [34].
Some authors suggested the hand-assisted or hybrid methods to better address technical challenges reported for LLR of postero-lateral segments: in the series by Soyama, an 8 cm upper midline laparotomy was performed, with 4/105 patients (4 %) (2 surgical site infection and 2 postoperative ileus) suffering from morbidity related to the laparotomy [10].
We do not feel to recommend this approach because some of the advantages of LLR can be lost: laparotomy-related complications and consequent increased requirement for postoperative analgesics, and a higher risk of postoperative intra-abdominal adhesions. Furthermore, it has been repeatedly proved that laparoscopic approach results in less disruption of the abdominal wall collateral circulation and less fluid shifts from exposure of the peritoneal cavity with a lower incidence of postoperative ascites in cirrhotic patients compared to open surgery: this benefit could be lost due to the need of midline laparotomy [35–39].
According to some other surgeons, we believe that the hand-assisted method or hybrid techniques have a limited role [25, 40] except in a very early phase of a training program in LLR.
In conclusion, laparoscopic resection of liver tumors located in the postero-lateral segments of the liver is technically feasible and safe with short-term results similar to other LLR. In our opinion a standard lithotomic position, as usually adopted in LLR performed for lesions located in “laparoscopic segments” allows the surgeon to be more confident with the surgical field and vision, minimizing the risk of complication related to different approaches and with the possibility of a more rapid and simple conversion to open surgery whenever needed.
References
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil C, Belghiti J, Strasberg S, Chari RS (2009) World consensus conference on laparoscopic surgery the international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg 250:825–830
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection—2804 patients. Ann Surg 250:831–841
Abu Hilal M, Di Fabio F, Abu Salameh M, Pearce NW (2012) Oncological efficiency analysis of laparoscopic liver resection for primary and metastatic cancer: a single-center UK experience. Arch Surg 147:42–48
Giuliani A, Migliaccio C, Ceriello A, Aragiusto G, La Manna G, Calise F (2014) Laparoscopic vs. open surgery for treating benign liver lesions: assessing quality of life in the first year after surgery. Updates Surg 66:127–133
Aldrighetti L, Cipriani F, Ratti F, Casciola L and Calise F, on behalf of the Italian National Survey Group (2012) The Italian experience in minimally invasive surgery of the liver: a national survey. In: Calise F, Casciola L (eds) Minimally, surgery of the liver. Springer, Milan, pp 295–312
Bueno A, Rotellar F, Benito A, Martí-Cruchaga P, Zozaya G, Hermida J, Pardo F (2014) Laparoscopic limited liver resection decreases morbidity irrespective of the hepatic segment resected. HPB (Oxford) 16:320–326
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Ogiso S, Conrad C, Araki K, Nomi T, Anil Z, Gayet B (2015) Laparoscopic transabdominal with transdiaphragmatic access improves resection of difficult posterosuperior liver lesions. Ann Surg (Epub ahead of print)
Herman P, Kruger JAP, Perini MV, Coelho FF, Lupinacci RM (2013) Laparoscopic hepatic posterior sectionectomy: a hand-assisted approach. Ann Surg Oncol 20:1266
Soyama A, Takatsuki M, Adachi T, Kitasato A, Torashima Y, Natsuda K, Tanaka T, Yamaguchi I, Tanaka S, Kinoshita A, Kuroki T, Eguchi S (2014) A hybrid method of laparoscopic-assisted open liver resection through a short upper midline laparotomy can be applied for all types of hepatectomies. Surg Endosc 28:203–211
Viganò L, Capussotti L, De Rosa G, De Saussure WO, Mentha G, Rubbia-Brandt L (2013) Liver resection for colorectal metastases after chemotherapy: impact of chemotherapy-related liver injuries, pathological tumor response, and micrometastases on long-term survival. Ann Surg 258:731–740
Capussotti L, Nuzzo G, Polastri R, Giuliante F, Muratore A, Giovannini I (2003) Continuous versus intermittent portal triad clamping during hepatectomy in cirrhosis. Results of a prospective, randomized clinical trial. Hepatogastroenterology 50:1073–1077
Nuzzo G, Giuliante F, Giovannini I, Vellone M, De Cosmo G, Capelli G (2001) Liver resections with or without pedicle clamping. Am J Surg 181:238–246
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Belgihiti J, Clavien PA, Gadzijev E, Garden JO, Lau WY, Makuuchi M, Strong RW (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford) 2:333–339
Zhou Y, Xiao Y, Wu L, Li B, Li H (2013) Laparoscopic liver resection as a safe and efficacious alternative to open resection for colorectal liver metastasis: a meta-analysis. BMC Surg 113:44. doi:10.1186/147124821344
Jensen LS, Mortensen FV, Iversen MG, Jørgensen A, Kirkegaard P, Kehlet H (2009) Liver surgery in Denmark 2002–2007. Ugeskr Laeger 171:1365–1368
Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, Marvin M, Ravindra KV, Mejia A, Lainas P, Franco D, Cherqui D, Buell JF, Gamblin TC (2009) Minimally invasive liver resections for metastatic colorectal cancer. A multi-institutional, international report of safety, feasibility and early outcome. Ann Surg 250:842–848
Schultz NA, Larsen PN, Klarskov B, Plum LM, Frederiksen HJ, Christensen BM, Kehlet H, Hillingsø JG (2013) Evaluation of a fast-track programme for patients undergoing liver resection. Br J Surg 100:138–143
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumours located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumour location. Surgery 144:32–38
Cho JY, Han HS, Yoon YS, Shin SH (2008) Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc 22:2344–2349
Fong Y, Gonen M, Rubin D, Radzyner M, Brennan MF (2005) Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg 242:540–544 (discussion 544–547)
Bismuth H (2014) A new look on liver anatomy: needs and means to go beyond the Couinaud scheme. J Hepatol 60:480–481
Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K (2014) Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma: a case-controlled study with propensity score matching. J Gastrointest Surg 18:1994–2002
Kazaryan AM, Røsok BI, Pavlik Marangos I, Rosseland AR, Edwin B (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25:3881–3889
Buell JF, Gayet B, Han HS, Wakabayashi G, Kim KH, Belli G, Cannon R, Saggi B, Keneko H, Koffron A, Brock G, Dagher I (2013) Evaluation of stapler hepatectomy during a laparoscopic liver resection. HPB (Oxford) 15:845–850
Postriganova N, Kazaryan AM, Røsok BI, Fretland Å, Barkhatov L, Edwin B (2014) Margin status after laparoscopic resection of colorectal liver metastases: does a narrow resection margin have an influence on survival and local recurrence? HPB (Oxford) 16:822–829
Ikeda T, Toshima T, Harimoto N, Yamashita Y, Ikegami T, Yoshizumi T, Soejima Y, Shirabe K, Maehara Y (2014) Laparoscopic liver resection in the semiprone position for tumors in the anterosuperior and posterior segments, using a novel dual-handling technique and bipolar irrigation system. Surg Endosc 28:2484–2492
Giuliante F, Ardito F, Pulitanò C, Vellone M, Giovannini I, Aldrighetti L, Ferla G, Nuzzo G (2010) Does hepatic pedicle clamping affect disease-free survival following liver resection for colorectal metastases? Ann Surg 252:1020–1026
Chiow AK, Lewin J, Manoharan B, Cavallucci D, Bryant R, O’Rourke N (2015) Intercostal and transthoracic trocars enable easier laparoscopic resection of dome liver lesions HPB (Oxford) 17:299–303
Lee W, Han HO, Yoon YS, Cho JY, Choi YR, Shin HK (2014) Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 21:E65–E68
Dokmak S, Agostini J, Jacquin A, Cauchy F, Farges O, Belghiti J (2012) High risk of biliary fistula after isolated segment VIII liver resection. World J Surg 36:2692–2698
Kim J, Ahmad SA, Lowy AM, Buell JF, Pennington LJ, Soldano DA, James LE, Matthews JB, Hanto DW (2003) Increased biliary fistulas after liver resection with the harmonic scalpel. Am Surg 69:815–819
Mbah NA, Brown RE, Bower MR, Scoggins CR, McMasters KM, Martin RCG (2012) Differences between bipolar compression and ultrasonic devices for parenchymal transection during laparoscopic liver resection. HPB (Oxford) 14:126–131
Cannon RM, Saggi B, Buell JF (2014) Evaluation of a laparoscopic liver resection in the setting of cirrhosis. HPB (Oxford) 16:164–169
Dagher I, Belli G, Fantini C, Laurent A, Tayar C, Lainas P, Tranchart H, Franco D, Cherqui D (2010) Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg 211:16–23
Giuliani A, Migliaccio C, Surfaro G, Ceriello A, Defez M (2012) Short-and long-term follow-up. In: Calise F, Casciola L (eds) Minimally, surgery of the liver. Springer, Milan, pp 167–173
Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G (2010) Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 102:82–86
Ettorre GM, Laurenzi A, Lionetti R, Santoro R, Lepiane P, Colasanti M, Colace L, Piselli P, Puoti C, D’Offizi G, Antonini M, Vennarecci G (2014) Laparoscopic liver resections in normal and cirrhotic livers: a retrospective analysis in a tertiary hepato-biliary unit. Dig Liver Dis 46:353–357
Dagher I, Proske JM, Carloni A, Richa H, Tranchart H, Franco D (2007) Laparoscopic liver resection: results for 70 patients. Surg Endosc 21:619–624
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standard
All procedures performed in this study involving human participant were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human participants and/or animals
No animals but only human participants were engaged in our study protocol.
Informed consent
For this type of study (retrospective) formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giuliani, A., Aldrighetti, L., Di Benedetto, F. et al. Total abdominal approach for postero-superior segments (7, 8) in laparoscopic liver surgery: a multicentric experience. Updates Surg 67, 169–175 (2015). https://doi.org/10.1007/s13304-015-0305-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-015-0305-4