Abstract
Minimally invasive liver surgery has evolved rapidly. While anterior segments were the first performed in the initial implementation phases, posterosuperior segments have traditionally been considered as the “difficult segments.” Recent advances and new conceptions in liver anatomy have led to the definition of liver gates in order to achieve easy and reproducible anatomical hepatectomies by selectively clamping first and second-order pedicles. The right posterior sectionectomy is one of the most complex laparoscopic liver resections as it involves a second-order pedicle clamping, full right hepatic vein exposure, and complex positioning and liver mobilization. Herein we report our experience and technical recommendations for performing minimally invasive right posterior sectionectomy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The liver pedicles are the critical structures within the liver parenchyma that contain both bile ducts, artery, and portal veins surrounded by the Glissonean sheet. Access to the liver pedicles is necessary for liver surgery. The traditional approach to accessing the liver pedicles has been through a Glissonean approach, which includes incision in the Glissonean sheet and individual exposure, control, and section of the portal vein, hepatic artery, and bile duct. However, extra-Glissonean approaches have gained popularity in recent years due to their potential to reduce bleeding and improve surgical outcomes.
One of the most widely used extra-Glissonean approaches is the so-called Takasaki approach. This technique was developed by Dr. Koji Takasaki in Japan in the early 2000s and has since been adopted by liver surgeons worldwide. The Takasaki approach involves accessing the liver pedicles from outside the Glissonean capsule by dissecting along the plane between the liver and the pedicle keeping the capsule intact. From a practical point of view, the Takasaki approach may offer potential advantages over the traditional Glissonean approach. The main one is the standardization and avoidance of individual dissection. This may lead to reduced bile leaks and iatrogenic damage of other pedicles [1,2,3]. Very recently, a manuscript from Sugioka established the gate theory as a feasible and practical approach to Glissonean pedicles by identifying six gates in the liver from which, in an extra-Glissonean way, primary and secondary pedicles could be encircled to perform left and right hemihepatectomies (from Gate 3 to 1, and from Gate 4 to 6, respectively) and left lateral, medial, right anterior, and right posterior sectionectomies (from Gate 2 to 1, 3 to 4, 4 to 5, and 5 to 6, respectively) [4]. Several studies have investigated the efficacy and safety of the Takasaki approach. Glissonean approach has been reported safe and feasible for minimally invasive liver resections with several reported advantages compared to the conventional hilar approach [5].
2 The Laparoscopic Right Posterior Sectionectomy
The laparoscopic right posterior sectionectomy is a minimally invasive surgical procedure for the removal of the right posterior section of the liver which is composed of segments 6 and 7. These are the so-called posterior segments of the liver and were traditionally considered as more difficult and a potential contraindication for minimally invasive approach. However, laparoscopic right posterior sectionectomy offers several advantages over traditional open surgery. Several studies have demonstrated that laparoscopic right posterior sectionectomy compared to open is associated with a shorter operating time, less blood loss, faster recovery time, and a lower incidence of postoperative complications compared to open surgery [6,7,8]. A recent subgroup analysis of the OSLO-COMET randomized trial demonstrated that in the setting of patients undergoing laparoscopic or open-liver resection of colorectal liver metastases in the posterosuperior segments, laparoscopic surgery was associated with shorter hospital stay and comparable perioperative outcomes [9]. Nevertheless, laparoscopic right posterior sectionectomy is not without its challenges. The laparoscopic approach requires specialized training and expertise, and not all patients are suitable candidates for the procedure. In addition, the laparoscopic approach may be more technically challenging in patients with obesity or previous abdominal surgery, and a proper learning curve is mandatory. It has been recently reported that the learning curve in the posterosuperior segments is estimated to be 40 procedures for wedge and 65 for anatomical resections [10].
3 Technical Standardization of Laparoscopic Right Posterior Sectionectomy (Video)
Laparoscopic right posterior sectionectomy can be well standardized by considering extra-Glissonean approach and root dissection of hepatic vein. In our Department, unless a need for hilar approach which may involve hilar dissection of right posterior structures due to tumor close to the confluence, our steps are the following:
-
1.
Placing Pringle on the left side of the patient or in the theoretical further Pfannenstiel incision by using a chest tube and a long tape [11]. We recommend this technique rather than the Huang’s loop technique to keep a firm countertraction to properly dissect the right posterior pedicle.
-
2.
By pulling the gallbladder toward the medial side, access to Gates 5 and 6 can be obtained. We advocate to try to get access keeping Laennec’s capsule intact. In fatty livers it is not easy to be obtained. This procedure is usually performed by observing the Rouviere’s sulcus and dissecting it on its origin on both sides [12].
-
3.
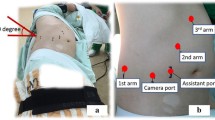
Encircling and clamping the right posterior pedicle. This process may be slightly complex depending on the intrinsic anatomy of the right posterior pedicle (Fig. 17.1).
-
4.
After clamping the pedicle, indocyanine green is administered IV in order to demarcate ischemic line. Before proceeding to any demarcation, it is strongly advisable to perform exhaustive ultrasonic exploration and double check that this is the desired transection line. After superficial demarcation, artifacts may be observed in the ultrasound exploration. We also do not recommend to perform any kind of section at this moment. This is because of the potential damage that may be caused to right anterior or S1 pedicle. We recommend to perform the section of the right posterior pedicle when parenchymal transection is advanced and a safer section is ensured.
-
5.
After checking the transection line, it is recommended to fully mobilize the right lobe of the liver from triangular and coronary ligaments. It is also necessary to fully detach it from IVC and reach up to the confluence of IVC and right hepatic vein. Careful dissection and transection of the hepatocaval ligament should be performed. At this stage, several problem may happen, including tears in the liver surface due to discrepant pull-push movements and mainly bleeding from IVC or during isolation of hepatocaval ligament of RHV. We strongly recommend to get a 3/0 4/0 polypropylene stitch ready as well as thrombin-derived hemostatic agents for a rapid control.
-
6.
When reaching up to the RHV, our preferred technique is to make a root approach of the RHV with a dorsoventral and cephalo-caudal dissection by using the tip of the ultrasonic dissector. This approach has several advantages over anterior approach. First, it allows identification of the main trunk of the RHV avoiding multiple clips of bifurcated branches to the right posterior sector; the second real advantage is that damage to the vein is far more limited with this approach. This effect was widely reported by Honda et al. This group reported that root approach and dissection of hepatic veins may cause small bleeding from tiny branches in a so called “pull up injury,” rather than a “split” injury on anterior approaches. Pull-up injuries are easy to be controlled as they are tiny holes in the vein surface. On the contrary, split injuries are tears which are far more difficult to be controlled as they are large injuries due to the dissection mechanism and direction [13, 14].
-
7.
When the full main trunk of RHV is exposed, clip and section of its main branches to segments 6 and 7 is easily performed. At this moment, parenchymal transection may be quite advanced, and access to the previous bulldog placed in the right posterior pedicle may be easier to grant insertion of hem-o-locks or staplers in a proper direction to avoid damage to right anterior pedicle. At this stage, portal pedicle section is recommended and safer.
-
8.
By performing this root venous approach, at this stage, transection of the anterior surface of the liver is easier to be performed, and few important branches may be found. The final step would be to proceed to the transection of the right hepatic vein mostly by using endostapler.
-
9.
Two main important difficulties must be considered during any step of the right posterior sectionectomy:
-
First difficulty: In the event that the tumor may be too close to the bifurcation between the right anterior and right posterior pedicles, extra-Glissonean approach may not be the best option as resection margins may be compromised. We recommend to locate the Rouviere’s sulcus, open the Glissonean sheet, and make individual section of the artery, portal vein, and bile duct.
-
Second difficulty: Depending on the ribs positioning and BMI, it may be quite difficult to access the upper part of segment 7. In this case, it has been reported the use of transthoracic trocars (up to two) to be able to bring the camera to the right sided abdominal trocars and use the transthoracic ones for dissection. In this case, 10-mm ones should be closed at the end of the procedure to prevent pneumothorax [14].
-
4 Conclusions
Approaching the right posterior sector is one of the most difficult ones in minimally invasive liver surgery. As reported in most of the currently used difficulty scoring systems, this resection can be considered as advanced or expert. Our technique is an easy and reproducible way of performing a right posterior sectionectomy including extra-Glissonean approach, ICG demarcation, and root dissection of the right hepatic vein.
5 Summary and Key Points
-
A well-defined preoperative imaging protocol is strongly advisable in order to have a surgical mapping. In this sense, 3D models and virtual reconstructions may help accuracy and surgical strategy (Fig. 17.2).
-
Extra-Glissonean access is safe in right posterior sectionectomy. It is strongly advisable to create countertraction with the Pringle tourniquet and move between Gates 5 and 6 in order to control the right posterior pedicle.
-
Hepatic vein dissection should be performed from a dorsoventral and cephalon-caudal approach to avoid severe injuries.
-
ICG is strongly recommended to create anatomical precise resection, including intersectorial planes.
References
Takasaki K, Kobayashi S, et al. Gurisonsho syori ni yoru atara- sii keitouteki kan setujojutu (New anatomic liver resection using Glissonean approach). Syujutu (Operation). 1986;40:7–14. [published in Japanese].
Takasaki K. Kan migi kuiki setujo -uyou koukuiki setujo- (Right Posterior Segmentectomy). Syujutu (Operation). 1993;47:465–71. [published in Japanese].
Takasaki K. Glissonean pedicle transection method for hepatic resection: a new concept of liver segmentation. J Hepato-Biliary-Pancreat Surg. 1998;5(3):286–91.
Sugioka A, Kato Y, Tanahashi Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec’s capsule: proposal of a novel comprehensive surgical anatomy of the liver. J Hepatobiliary Pancreat Sci. 2017;24(1):17–23.
Morimoto M, Tomassini F, Berardi G, Mori Y, Shirata C, Abu Hilal M, et al. Glissonean approach for hepatic inflow control in minimally invasive anatomic liver resection: a systematic review. J Hepatobiliary Pancreat Sci. 2022;29(1):51–65.
Scuderi V, Barkhatov L, Montalti R, Ratti F, Cipriani F, Pardo F, et al. Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg. 2017;104(6):751–9.
van der Heijde N, Ratti F, Aldrighetti L, Benedetti Cacciaguerra A, Can MF, D’Hondt M, et al. Laparoscopic versus open right posterior sectionectomy: an international, multicenter, propensity score-matched evaluation. Surg Endosc. 2021;35(11):6139–49.
Rhu J, Kim S-J, Choi G-S, Kim JM, Joh J-W, Kwon CHD. Laparoscopic versus open right posterior sectionectomy for hepatocellular carcinoma in a high-volume center: a propensity score matched analysis. World J Surg. 2018;42(9):2930–7.
Aghayan DL, Fretland ÅA, Kazaryan AM, Sahakyan MA, Dagenborg VJ, Bjørnbeth BA, et al. Laparoscopic versus open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB (Oxford). 2019;21(11):1485–90.
Berardi G, Aghayan D, Fretland ÅA, Elberm H, Cipriani F, Spagnoli A, et al. Multicentre analysis of the learning curve for laparoscopic liver resection of the posterosuperior segments. Br J Surg. 2019;106(11):1512–22.
Rotellar F, Pardo F, Bueno A, Martí-Cruchaga P, Zozaya G. Extracorporeal tourniquet method for intermittent hepatic pedicle clamping during laparoscopic liver surgery: an easy, cheap, and effective technique. Langenbeck’s Arch Surg. 2012;397(3):481–5.
Monden K, Alconchel F, Berardi G, Ciria R, Akahoshi K, Miyasaka Y, et al. Landmarks and techniques to perform minimally invasive liver surgery: a systematic review with a focus on hepatic outflow. J Hepatobiliary Pancreat Sci. 2022;29(1):66–81.
Honda G, Kurata M, Okuda Y, Kobayashi S, Tadano S, Yamaguchi T, et al. Totally laparoscopic hepatectomy exposing the major vessels. J Hepatobiliary Pancreat Sci. 2013;20(4):435–40.
Okuda Y, Honda G, Kurata M, Kobayashi S, Sakamoto K, Takahashi K. A safe and valid procedure for pure laparoscopic partial hepatectomy of the most posterosuperior area: the top of segment 7. J Am Coll Surg. 2015;220(3):e17–21.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ciria, R., Rufián, B., Ayllón, M.D., Briceño, J. (2023). Right Posterior Hepatectomy (Segment VI + VII). In: Ielpo, B., Rosso, E., Anselmo, A. (eds) Glissonean Pedicles Approach in Minimally Invasive Liver Surgery. Springer, Cham. https://doi.org/10.1007/978-3-031-35295-9_17
Download citation
DOI: https://doi.org/10.1007/978-3-031-35295-9_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35294-2
Online ISBN: 978-3-031-35295-9
eBook Packages: MedicineMedicine (R0)