Abstract
Uterine sarcomas are rare, highly malignant tumours comprising < 1 % of all gynaecologic malignancies. To evaluate clinical presentation, histolopathologic pattern and outcome of uterine sarcomas presenting to a tertiary referral centre over an 8 year period (2004–2012). All histologically proven uterine sarcomas were retrospectively analysed. Clinical presentation, histology, treatment and outcome were analysed. Mean age was 42 years. Predominant histopathology was endometrial stromal sarcoma (n = 13); 9 were low grade, carcinosarcoma (n = 8) and leiomyosarcoma (n = 2). Fourteen patients had Stage I disease, 3 Stage II, 4 Stage III and 2 were Stage IV at presentation. Patients with disease confined to uterus received no adjuvant treatment (61 %). Of these, 11 were endometrial stromal sarcoma (7 were low grade) and 3 were carcinosarcomas. Four patients received adjuvant EBRT following hysterectomy (17 %). Two patients who presented with metastases received palliative chemotherapy. Mean follow-up period was 46 months (0–86 months). Eleven patients (47 %) developed disease recurrence. Seven (30 %) had local recurrence, while 4 (17 %) developed pulmonary metastases. A total of eight patients died and all deaths were within 1 year of recurrence. The only prognostic factor that correlated with survival was the stage of disease at diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine sarcomas are highly malignant tumours which account for <1 % of gynaecologic malignancies and 2–5 % of all uterine malignancies. In spite of intensive treatment, local recurrence and distant metastases are common. Overall survival is poor with 5-year survival rates of 50–70 % for Stage 1 disease and dismal rates of 0–20 % for remaining stages [1]. Three main pathologic subgroups are recognised, the commonest being leiomyosarcoma (55 %), carcinosarcoma formerly known as malignant mixed mullerian tumour (30 %), and endometrial stromal sarcoma (15 %). The strongest prognostic factor for all subgroups is the stage at diagnosis [2–4]. Separate staging systems exist for endometrial stromal sarcoma and leiomyosarcomas while carcinosarcoma follows that of endometrial carcinoma and is now considered as high grade endometrial cancer [5]. Total abdominal hysterectomy with bilateral salpingooophorectomy is the standard initial treatment. The importance of lymph node dissection varies by tumour histology. Routine pelvic and/or paraaortic lymphadenectomy is not useful in women with leiomyosarcoma or undifferentiated endometrial sarcoma, while the role of lymphadenectomy in ESS is unclear. Selective paraaortic node dissection may be done [6]. Adjuvant therapy is of doubtful benefit. In leiomyosarcoma, adjuvant external beam radiotherapy reduces the incidence of local recurrence, but does not change the overall survival as these patients often fail distally [7]. Hormonal therapy for ESS has been tried with limited benefit [8]. Given the low incidence, current data on uterine sarcomas depend on case reports and small retrospective case series. We present here our experience of uterine sarcoma at the Department of Surgical Oncology, Centre for Oncology, Govt. Royapettah Hospital, Chennai, India, which is a tertiary referral centre, over an 8 year period from 2004 to 2012.
Objectives
To evaluate clinical presentation, histolopathologic pattern and outcome of uterine sarcomas.
Patients and Methods
Retrospective analysis of all histologically proven uterine sarcomas treated at the Government Royapettah Hospital, Chennai, India, from August 2004 to July 2012 in Department of Surgical Oncology was undertaken and case records reviewed. Age incidence, clinical symptoms, signs at presentation and histopathologic diagnosis were analysed. Stage of disease was determined in leimyosarcomas and ESS using the FIGO staging classification: Stage I – sarcoma confined to the uterine corpus, stage II – sarcoma confined to corpus and cervix, stage III – sarcoma confined to the pelvis, and stage IV – extrapelvic sarcoma while carcinosarcomas were staged as for endometrial cancers. Treatment details were recorded. Patient’s follow up details were retrieved from hospital records and defaulted patients were contacted by telephonic conversation to assess outcome.
Results
Of the 9342 new gynaecological cancers diagnosed during this 8 year period, 1944 were uterine malignancies. A total of 23 cases of uterine sarcoma were diagnosed. Mean age of patients was 42.6 years (range 34–69 years) (Table 1). Thirteen patients had Endometrial stromal sarcoma (57 %), 8 had carcinosarcoma (35 %) and 2 patients had leiomyosarcoma (8 %). The main presenting symptoms were abnormal vaginal bleeding, low abdominal pain and mass effect (which includes abdominal mass, mass protruding per vaginum, urinary symptoms and infertility) (Table 2).
All patients underwent surgery following evaluation. All patients underwent total abdominal hysterectomy with bilateral salpingo oophorectomy. In three cases, the surgical procedure included omentectomy. Two patients were referred following hysterectomy (preoperatively diagnosed as leiomyoma), one with recurrence at the vault, vagina in the 2nd month following surgery and one patient with lung metastases 4 months after surgery. In all, there were 14 patients with Stage I disease, 3 with Stage II, 4 with stage III and 2 patients with Stage IV (Table 3). Patients with disease confined to the uterus received no adjuvant treatment (61 %). Of these, 11 were endometrial stromal sarcoma of which 7 were low grade. Three were carcinosarcomas. Four patients received adjuvant external beam radiotherapy following hysterectomy (17 %) [3 cases of carcinosarcoma and one case of leiomyosarcoma]. Two patients who presented with metastases received palliative chemotherapy. Of these one was leiomyosarcoma and the other was carcinosarcoma.
Follow-up
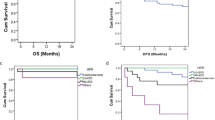
Mean follow-up period was 46 months (0–86 months). Patients were on follow up monthly for the first year, once in 2 months in the second year and three monthly thereafter. Chest X-ray or abdominal and pelvic computed tomographies were performed as indicated by clinical symptoms to rule out recurrent or metastatic disease. Median disease-free survival was 42 months (range 0–84 months). Eleven patients (47 %) had disease recurrence (Table 4). Seven patients (30 %) had local recurrence, 6 in the pelvis and one in the vagina, while 4 patients (17 %) had distant metastases to the lungs. Histologically, 7 cases of ESS, 3 cases of carcinosarcoma and one case of leiomyosarcoma recurred. A total of eight patients (35 % of all cases and 82 % of all recurrences) died of the disease and all deaths were within 1 year of recurrence.
Discussion
Most studies of uterine sarcomas report an incidence of 55 % for leiomyosarcoma, this being the commonest, carcinosarcomas stand second at 30 % and endometrial stromal sarcoma are least common (15 %) [2, 9, 10]. In the present study, endometrial stromal sarcoma (69 %) was the commonest, followed by carcinosarcoma (26 %) and leiomyosarcomas being the least common (5 %). One possible explanation for this distribution may be the fact that as endometrial stromal sarcomas present with symptoms of abnormal vaginal bleeding and postmenopausal bleeding, the suspicion of malignancy is high and warrant a referral to our unit, whereas most leiomyosarcomas are diagnosed postoperatively having initially been diagnosed as leiomyomas and are treated by gynaecologists.
The commonest presenting symptom was abnormal vaginal bleeding which led to earlier referral and diagnosis. Patients however did not have a better prognosis, underlining the aggressive nature of the disease.
In patients diagnosed at an earlier stage with disease confined to the uterus, surgery alone can be curative consisting of total abdominal hysterectomy with bilateral salpingo oophorectomy [11]. Currently no standard therapy has been recommended for patients with advanced disease and our patients underwent additional debulking wherever possible which included omentectomy in three cases.
Adjuvant chemotherapy is of doubtful proven benefit [2]. Doxorubicin and gemcitabine have been tried with variable results in leiomyosarcoma. Ifosfamide, cisplatin and paclitaxel have been used in carcinosarcoma [12]. Hormonal therapy with GnRH analogues, aromatase inhibitors-megesterol acetate, letrozole, medroxyprogesterone acetate have been used in endometrial stromal sarcoma but numbers studied are too small to make conclusions. None of the patients in our series received adjuvant chemotherapy as its benefit remains doubtful at best. Adjuvant pelvic radiation has a significant reduction of recurrences within the radiation treatment field but no alteration in survival [2, 7, 13]. Four patients received adjuvant radiotherapy, 3 cases of carcinosarcoma and 1 leiomyosarcoma. Stage for stage, leiomyosarcoma has a worse prognosis than carcinosarcoma. Disease recurrence in our study was 47 % and mortality 26 %. The low mortality rate in our study may be attributed to the large number of ESS in stage I and the low incidence of leiomyosarcoma which has the worst prognosis.
Conclusion
Uterine sarcoma is a rare tumours with high malignant potential and poor prognosis. The only prognostic factor that correlated with survival was the stage of disease at diagnosis. Adjuvant therapies do not have much benefit and does not alter survival.


References
Sharma DN, Rath GK, Kumar S, Kumar L, Bhatla N, Gandhi AK, Hariprasad R (2011) Clinical outcome of patients with uterine sarcomas. J Cancer Res Ther 7:270–274
Naaman Y, Shveiky D, Ben-Shachar I, Shushan A, Mejia-Gomez J, Benshushan A (2011) Uterine sarcoma: prognostic factors and treatment evaluation. IMAJ 13:76–79
Durnali A, Tokluoğlu S, Özdemir N, Inanç M, Alkiş N, Zengin N, Sönmez ÖU, Küçüköner M (2012) Prognostic factors and treatment outcomes in 93 patients with uterine sarcoma from 4 centers in Turkey. Asian Pac J Cancer Prev 13(5):1935–1941
Nassar OA, Abdul Moaty SB, Khalil e-SA, El-Taher MM, El Najjar M (2010) Outcome and prognostic factors of uterine sarcoma in 59 patients: single institutional results. J Egypt Natl Canc Inst 22(2):113–122
Prat J (2009) FIGO staging for uterine sarcomas. Int J Gynaecol Obstet 104(3):177–178
Shah JP, Bryant CS, Kumar S et al (2008) Lymphadenectomy and ovarian preservation in low-grade endometrial stromal sarcoma. Obstet Gynecol 112:1102
Wright JD, Seshan VE, Shah M et al (2008) The role of radiation in improving survival for early-stage carcinosarcoma and leiomyosarcoma. Am J Obstet Gynecol 199(5):536.e1–536.e8
Puliyath G, Krishnan Nair M (2012) Endometrial stromal sarcoma: a review of the literature. Indian J Med Paediatr Oncol 33(1):1–6
D’Angelo E, Prat J (2010) Uterine sarcomas: a review. Gynecol Oncol 116(1):131–139
Naaman Y, Shveiky D, Ben-Shachar I, et al (2011) Uterine sarcoma: prognostic factors and treatment evaluation. IMAJ 13(2):76–79
Barakat RR. Principles and practice of gynecological oncology
Homesley HD, Filiaci V, Markman M, Gynecologic Oncology Group et al (2007) Phase III trial of ifosfamide with or without paclitaxel in advanced uterine carcinosarcoma: a gynecologic oncology group study. J Clin Oncol 25:526–531
Anupama R, Kuriakose S et al (2013) Carcinosarcoma of the uterus—a single institution retrospective analysis of the management and outcome and a brief review of literature. Indian J Surg Oncol 4(3):222–228
Conflict of Interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sivakumari, S., Rajaraman, R. & Subbiah, S. Uterine Sarcoma: The Indian Scenario. Indian J Surg Oncol 6, 232–236 (2015). https://doi.org/10.1007/s13193-015-0433-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0433-9