Abstract
Uterine carcinosarcomas are highly aggressive tumors of the uterus associated with a poor prognosis. Though initially classified as sarcomas, now these tumors are classified as carcinomas. The management approach of carcinosarcomas has also changed from those used for high grade sarcomas to that used for managing high grade endometrial carcinomas. The purpose of our study was to analyze the management and outcome of patients with uterine carcinosarcomas treated at our institution and also to attempt a brief review regarding the management of uterine carcinosarcomas. We did a retrospective analysis of all patients with a diagnosis of carcinosarcoma of the uterus treated at our Institution from January 2005 till December 2010. All Patients with a pathological diagnosis of carcinosacrcoma or malignant mixed mullerian tumours of the uterus were included. Data was obtained from the hospital electronic medical records and the hospital cancer registry. Data was analyzed using SPSS v.17. During this 6 year period we had 20 patients with carcinosarcoma of the uterus. 75 % of the patients belonged to Stage I and II. 95 % of the patients underwent Hysterectomy with Bilateral salpingo oophorectomy and 60 % had lymphadenectomy also along with hysterectomy.8 patients had disease recurrence . In patients who had gross extrauterine disease at the time of surgery , the survival was only 9 months whereas in patients who had complete staging with disease confined to the uterus , the survival was 36 months. Carcinosarcomas, accounts for more than 15 % of the uterine cancer associated deaths. Surgery remains the cornerstone of management for these tumors and surgery with pelvic and para aortic lymphadenectomy and peritoneal and omental biopsies is required for the correct staging of the disease and may also provide a survival advantage. Radiation therapy has been shown to provide only better local control without any survival advantage. Further studies are needed to assess whether chemotherapy offers a definite survival benefit in uterine carcinosarcomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Uterine carcinosarcomas are highly aggressive tumors of the uterus associated with a poor prognosis. They account for only 1–3 % of uterine tumors and have an incidence of less than 2 per 1, 00,000 women per year [1]. They carry a poor prognosis irrespective to the stage of diagnosis and even in early stage disease; survival is 50 % or less. Uterine carcinosarcomas were classified initially as uterine sarcomas and was termed malignant mixed mullerian tumors. But now, these tumors are classified as carcinomas since in vitro studies, immunohistochemistry and molecular studies have shown that they are derived from a monoclonal cancer cell which exhibits sarcomatous metaplasia [2, 3]. Also the epidemiology, risk factors and clinical behavior of these tumors points to an endometrial origin. Studies have also shown that the behaviors of these tumors are determined by the epithelial component. Epithelial elements invade the lymphatic and vascular spaces and metastasize, whereas the spindle cell component has a very limited metastatic potential [4, 5]. Figure 1 shows the microscopic appearance of a carcinosarcoma. The management approach of carcinosarcomas has also changed from those used for high grade sarcomas to that used for managing high grade endometrial carcinomas. The purpose of our study was to analyze the management and outcome of patients with uterine carcinosarcomas treated at our institution.
Materials and Methods
We did a retrospective analysis of all patients with a diagnosis of carcinosarcoma of the uterus or malignant mixed mullerian tumor as it was called earlier treated at our Institution from January 2005 till December 2010. Data was obtained from the hospital electronic medical records and the hospital cancer registry. All Patients with a pathological diagnosis of carcinosarcoma or malignant mixed mullerian tumors of the uterus were included. Demographic data included were—age at diagnosis, parity, menstrual status, family or personal history of malignancies, use of tamoxifen, estrogens or history of pelvic radiotherapy. Also the details of diagnosis, investigations and treatment including the surgical, chemotherapeutic and radiation details and present status of the patient were collected. Staging was according to the FIGO 1988 staging for the carcinoma of endometrium. In case of recurrences, the time of onset and type of recurrence, treatment taken and present status were noted. A senior oncopathologist without knowledge of the clinical outcome reviewed all the histopathology slides.
Data was analyzed in SPSS v.17. Survival was defined as the observed length of life from date of start of treatment to death, or in case of living patients, to the date of last contact.
Results
During this 6 year period we had1548 patients with gynecological cancers out of which 323 patients had cancer of the uterine corpus. There were 20 patients with carcinosarcoma of the uterus accounting to 6.2 % of all uterine malignancies. Clinicopathologic features are presented in Table 1. 95 % of our patients were post-menopausal. None of our patients had history of pelvic irradiation or history of use of tamoxifen or non-contraceptive estrogens. Median age at presentation was 61.5 years (range 46–79 years). 19 (95 %) patients underwent Hysterectomy with Bilateral salpingo oophorectomy and 12 (60 %) had pelvic and para aortic lymphadenectomy also along with hysterectomy. 7(35 %) patients had infracolic omentectomy done as a part of the staging. One patient had extensive disease on presentation and only partial debulking could be done.
Fifteen (75 %) patients belonged to Stage I and II. 4 (20 %) had stage III disease; there was one patient (5 %) with stage IV disease. For analyzing the data we have divided the patients into two major groups (Table 2) A. Patients with gross extrauterine disease at laparotomy(n = 4) and B. Patients who did not have gross extrauterine disease at laparotomy(n = 16). There were four patients (20 %) with gross extrauterine disease during laparotomy. Out of these, three were completely debulked. Adjuvant radiotherapy was given only for 2 patients as one patient refused adjuvant treatment. In this group the overall survival is 9 months. In the patient in whom complete debulking could not be achieved, only palliative surgery was done following which she had disease progression and she expired within 3 months.
The 16 patients who did not have any gross extrauterine disease at presentation, were divided further into two groups (Table 3)– 1.patients who had surgery with lymph node dissection (n = 11) and 2. patients who had surgery without lymph node dissection. (n = 5). Out of 11 patients who underwent lymphadenectomy, only one patient was node positive and she was assigned to Stage III due to the lymph node status. She received external pelvic radiation as adjuvant treatment, but presented with liver metastases after 34 months of treatment . She was given palliative chemotherapy but expired within 3 months of recurrence. The remaining 10 patients who had staging laparotomy including lymphadenectomy and was found to be node negative, adjuvant treatment was given in 6 patients. All six patients received radiation and 2 patients had chemotherapy with cisplatin and Ifosfamide along with radiotherapy. In the 4 patients who did not receive adjuvant treatment, 3 were Stage I a, with disease confined only to the endometrium with no myometrial invasion. The remaining patient had myometrial invasion, but she refused radiotherapy. Out of these 10 patients, only one had disease recurrence and it was a patient who had undergone pelvic and para aortic lymphadenectomy as a part of staging surgery and has received radiation ( EBRT + Brachytherapy ) as adjuvant treatment. She presented as lung metastases after 15 months and was given palliative chemotherapy, but the patient expired after 4 months. None of the four patients who did not receive adjuvant treatment recurred. Overall survival in the patients who had disease confined to the uterus, with proven node negative status is 36.3 months.
Five patients in this group had surgery without lymphnode dissection and none of them had adjuvant treatment. Two patients recurred in the vault within a year and were treated with radiotherapy. The overall survival in this group is 24 months.
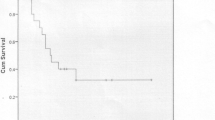
The overall survival of all patients is represented in Graph 1. Graph 2 compares the survival of patients with gross disease confined to the uterus with patients who had gross extrauterine disease during laparotomy.
Discussion
Carcinosarcoma of the uterus is a rare and highly aggressive tumor associated with a poor prognosis. This is one of the most malignant neoplasms known to occur in the uterus, accounting for more than 15 % of the uterine cancer associated deaths [6]. The 5 year survival is only about 33–39 % [7] and it has not markedly improved over the years despite the use of more aggressive adjuvant therapies.
Earlier, carcinosarcomas were described as the most common of the uterine sarcomas with an epithelial and stromal differentiation. Also, previously the sarcomatous component was subdivided into homologous viz. leiomyosarcoma, fibrosarcoma, malignant fibrous histiocytoma, or undifferentiated sarcoma and heterologous viz. rhabdomyosarcoma, chondrosarcoma, osteosarcoma, or liposarcoma. But now, these tumors are classified as carcinomas since the in vitro studies, immunohistochemistry and molecular studies have shown that they are derived from a monoclonal cancer cell which exhibits sarcomatous metaplasia [2, 3]. Studies have also shown that the behaviors of these tumors are determined by the epithelial component. Epithelial elements invade the lymphatic and vascular spaces and metastasize, whereas the spindle cell component has a very limited metastatic potential [4, 5]. This has got clinical relevance when planning the adjuvant treatment.
In our series the carcinomatous component was endometrioid type in 70 % of the cases. Only 40 % of the epithelial components had Grade III histology on presentation. The sarcomatous component was homologous in 65 %, heterologous in 25 % and undifferentiated in 10 % of the patients.
Several risk factors have been associated with uterine carcinosarcomas including post-menopausal age, long term use of non-contraceptive estrogens, tamoxifen use and also a history of previous pelvic irradiation. Most of our patients were postmenopausal with a mean age of 61.5 years but none had history of use of hormones or tamoxifen and none had received previous pelvic irradiation. The most important prognostic factor is said to be the extent of tumor at the time of diagnosis. Survival is very poor if the tumor is extending beyond the uterus at the time of diagnosis [8]. In our series, the overall survival for patients who had tumor extending beyond uterus was 9 months versus 31 months in patients who had gross disease confined to the uterus.
The primary treatment modality for a carcinosarcomas is surgery. A comprehensive staging has its value as a diagnostic procedure and will also be a determinant for adjuvant therapy. According to the Gynecologic Oncology Group (GOG) surgical staging data of 301 patients with carcinosarcomas of the uterus, 20 % of the patients with disease clinically confined to the uterus had surgically documented metastasis. Also there was 18 % lymph node positivity in an otherwise Stage I-II disease [9]. In our series the lymphnode positivity in otherwise Stage I-II disease was 9 % (1 out of 11). The frequency and pattern of lymph node metastases in carcinosarcoma is similar to that of high risk endometrial adenocarcinoma [10]. As sampling of the pelvic or para aortic lymph nodes may miss microscopic or occult lymph node metastasis, systematic lymph node dissection is recommended [11]. Because the surgical removal is the most important aspect of treatment, the removal of occult lymph node metastases may also improve prognosis and may render women more susceptible to cure by adjuvant therapy [11]. Like any high grade endometrial cancer, carcinosarcomas has a propensity for transperitoneal spread causing positive peritoneal cytology, adnexal, omental and peritoneal metastasis . In the GOG series, 20 % of the carcinosarcomas were reclassified as stage III-IV from stage I-II after a comprehensive surgical staging [9]. Positive peritoneal washings have been reported in 19–44 % of women with carcinosarcoma and 29 % in women with apparently early stage disease [11]. Although the role of omentectomy and multiple peritoneal biopsies are unclear, as they are a recommended staging procedure in high risk endometrial cancers, it should also be done in women with early stage carcinosarcomas [11]. Hence a surgical staging with peritoneal washing cytology, removal of the adnexal structures, systematic pelvic, common iliac and para-aortic lymphadenectomies, and omentectomy is recommended to know the correct extent of these tumors. If there is extensive extrauterine disease on laparotomy, debulking surgery similar to that of epithelial ovarian cancer is recommended [11]. In a recent series, cytoreductive surgery with the goal of achieving a complete gross resection was found to be associated with an improved overall survival in patients with advanced carcinosarcoma [12]. Lymphadenectomy was done in 60 % (12 out of 20) of our patients and infracolic omentectomy for 35 %(7 out of 20). Lymph node involvement was found in 16.7 % (2 out of 12) of the patients who underwent lymphadenectomy. At diagnosis only about 65 % of the carcinosarcomas are confined to the uterus [13]. In our series 75 % of the patients had disease confined to the uterus on presentation.
The poor prognosis of women with carcinosarcomas, shows that adjuvant therapies need to be improved. The 2012 National comprehensice Cancer Network ( NCCN) guidelines recommends adjuvant treatment for all stages of carcinosarcoma except stage IA without myometrial invasion. In GOG 150, a Phase III trial comparing Whole abdominal radiation with three cycles of Ifosfamide with cisplatin as adjuvant therapy for completely resected Stage I – IV uterine carcinosarcoma, the recurrence rate was 21 % lower and death rate 29 % lower in the chemotherapy arm [14] but the results were not statistically significant. Sutton et al. showed that in advanced carcinosarcoma, higher response rates were seen with the combination of Ifosfamide and cisplatin compared with that of Ifosfamide(54%vs 36 %) alone [15]. Paclitaxel with Ifosfamide achieved higher response rates in a phase III trial when compared with Ifosfamide, [16] establishing this as a reasonable first line option for advanced carcinosarcoma. Paclitaxel with carboplatin has shown a response rate of 54 % in women with no prior chemotherapy, making this another reasonable first line treatment [17].
Reviews by Smith et al. and Nemani et al. analyzing the data from the SEER database has shown no survival benefit for Stage I- III carcinosarcomas with adjuvant RT. Smith et al. has shown an overall survival benefit with adjuvant RT in stage IV disease [18, 19]. In a study by Sampath et al. of 3,650 women, radiation did not seem to be predictive of overall survival [20]. The GOG 150 trial comparing WAI with chemotherapy did not show any statistically significant survival benefit or disease free survival benefit for radiation. There was a decline in vaginal failures (4 % vs. 10 %), but no difference was noted in the pelvic failure rate(13 %). There was higher rate of abdominal relapse in the radiation arm (28%vs19%). A phase III trial conducted by EORTC- GCG evaluating the role of adjuvant Radiation in uterine sarcomas found that there is increased local control for carcinosarcoma patients receiving radiation which does not translate into a survival benefit. In the irradiated carcinosarcoma group there is a greater likelihood of developing a first relapse at a distant site despite better local control. They have concluded that radiation therapy when used as adjuvant improves local control, but the additional morbidity and failure to impact on survival makes its inclusion not routinely acceptable. Extrapolating from the use in epithelial endometrial carcinomas, use of radiotherapy as a salvage treatment is recommended. They have also supported the use of adjuvant chemotherapy as a part of initial treatment for carcinosarcoma and tailored radiation only for the high risk groups [21].
Forty-five percent (9 out of 20) of our patients received adjuvant treatment. 2 patients had a combination of chemotherapy and radiation as a part of adjuvant treatment. A total of 8 patients received radiation as a part of adjuvant treatment and 3 received chemotherapy.
Carcinosarcoma has a very poor overall outcome with 5 year survival ranging from 33 to 39 %. The EORTC group showed 14 % relapse in the adjuvantly treated group and 24 % in the observation group [21]. The GOG study reported 112 recurrences for the 197 patients in the study. 60 were in the radiotherapy group and 52 in the chemotherapy group. Although not statistically significant, there were more vaginal recurrences in the chemotherapy group and abdominal recurrences in the radiation group [14]. In our series 7 patients (35 %) had disease recurrence and one patient with advanced disease in whom complete debulking could not be achieved had progressive disease. Two patients recurred in the vault and the remaining five had distant recurrences. Both the vault recurrences were in patients who had stage I disease, but node dissection was not done in these patients as a part of staging and had not received any adjuvant therapy. In the five patients with distant recurrences, four were Stage III and one patient was stage I who had received adjuvant radiation after the surgery. The vault recurrences were treated with radiotherapy and patients with distant recurrences had palliative treatment including chemotherapy
We acknowledge that this study is limited by the fact that this is a retrospective analysis and the patient numbers are small. But the two vault recurrences out of five stage I patients who did not have lymphadenectomy as a part of staging, shows the need for a thorough staging including lymphadenctomy in all patient suspected with carcinosarcoma uterus. Although there were no local recurrences in the six Stage I and II patients treated with adjuvant Radiotherapy, one distant recurrence occurred in this group, indicating the need for a better adjuvant therapy including chemotherapy in these patients also. But this being a small series, no statistically significant conclusions can be made.
Conclusion
Carcinosarcomas are highly aggressive malignant tumors of the uterus associated with a poor prognosis. Though earlier classified as sarcomas, recent evidence shows that these are high grade endometrial carcinomas with sarcomatous metaplasia. Surgery remains the cornerstone of management for these tumors and surgery with pelvic and para aortic lymphadenectomy and peritoneal and omental biopsies required for the correct staging of the disease. From the available evidence, radiation therapy has been shown to provide only better local control without any survival advantage. Chemotherapy is recommended as a standard adjuvant treatment in completely resected tumors and also after debulking in metastatic disease. But further studies are needed to assess whether chemotherapy offers a definite survival benefit for the patients with carcinosarcomas.
References
Cantrell LA, Havrilesky L, Moore DT et al (2012) A multi-institutional cohort study of adjuvant therapy in stage I-II uterine carcinosarcoma. Gynecol Oncol 127:22–26
Amant F, Moerman P, Neven P et al (2005) Endometrial cancer. Lancet 366(9484):491–505
McCluggage WG (2002) Uterine carcinosarcomas (malignant mixed mullerian tumors) are metaplastic carcinomas. Int J Gynecol Cancer 12:687–690
Bitterman P, Chun B, Kurman RJ (1990) The significance of epithelial differentiation in mixed mesodermal tumors of the uterus. A clinicopathologic and immunohistochemical study. Am J Surg Pathol 14:317–328
Silverberg SG, Major FJ, Blessing JA et al (1990) Carcinosarcoma (malignant mixed mesodermal tumor) of the uterus. A Gynecologic Oncology Group pathologic study of 203 cases. Int J Gynecol Pathol 9:1–19
El-Nashar SA, Mairani A (2011) Uterine carcinosarcoma. Clin Obstet Gynecol 54:292–304
Raspollini MR, Tommano S, Amunni G et al (2005) COX-2, c-KIT and HER-2/ neu expression in uterine carcinosarcomas: prognostic factors or potential markers for targeted therapies? Gynecol Oncol 96(1):159–167
Gonzalez Bosquet J, Terstriep SA, Cliby WA et al (2010) The impact of multi-modal therapy on survival for uterine carcinosarcomas. Gynecol Oncol 116:419–423
Major FJ, Blessing JA, Sliverberg SG et al (1993) Prognostic factors in early stage uterine sarcomas. A Gynaecologic Oncology Group Study. Cancer 71(4 Suppl):1702–1709
Creasman WT, Odicino F, Maisonneuve P et al (2006) Carcinoma of the corpus uteri. FIGO 26th annual report on the results of treatment in Gynecological Cancer. Int J Gynaecol Obstet 95(Suppl 1):S105–S143
Nam JH (2011) Surgical treatment of uterine sarcoma. Best Pract Res Clin Obstet Gynaecol 25:751–760
Tanner EJ, Leitao MM Jr, Garg K et al (2011) The role of cytoreductive surgery for newly diagnosed advanced-stage uterine carcinosarcoma. Gynecol Oncol 123:548–552
Gadducci A, Sartori E, Landoni F et al (2002) The prognostic relevance of histological type in uterine sarcomas: a Cooperation Task Force (CTF) multivariate analysis of 249 cases. Eur J Gynaecol Oncol 23:295–299
Wolfson AH, Brady MF, Rocereto T et al (2007) A gynecologic oncology group randomized phase III trial of whole abdominal irradiation (WAI) vs. cisplatin-ifosfamide and mesna (CIM) as post-surgical therapy in stage I-IV carcinosarcoma (CS) of the uterus. Gynecol Oncol 107:177–185
Sutton G, Brunetto VL, Kilgore L et al (2000) A phase III trial of ifosfamide with or without cisplatin in carcinosarcoma of the uterus: a Gynecologic Oncology Group Study. Gynecol Oncol 79:147–153
Homesley HD, Filiaci V, Markman M et al (2007) Phase III trial of ifosfamide with or without paclitaxel in advanced uterine carcinosarcoma: a Gynecologic Oncology Group Study. J Clin Oncol 25:526–531
Powell MA, Filiaci VL, Rose PG et al (2010) Phase II evaluation of paclitaxel and carboplatin in the treatment of carcinosarcoma of the uterus: a Gynecologic Oncology Group study. J Clin Oncol 28:2727–2731
Smith CD, Macdonald OK, Gaffney DK (2008) The impact of adjuvant radiation therapy on survival in women with uterine carcinosarcoma. Radiother Oncol 88:227–232
Nemani D, Mitra N, Guo M et al (2008) Assessing the effects of lymphadenectomy and radiation therapy in patients with uterine carcinosarcoma: a SEER analysis. Gynecol Oncol 111:82–88
Sampath S, Schultheiss TE, Ryu JK et al (2010) The role of adjuvant radiation in uterine sarcomas. Int J Radiat Oncol Biol Phys 76:728–734
Reed NS, Mangioni C, Malmstrom H et al (2008) Phase III randomized study to evaluate the role of adjuvant pelvic radiotherapy in the treatment of uterine sarcomas stages I and II: an EORTC Gynaecological Cancer Group study (protocol 55874). Eur J Cancer 44:808–818
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anupama, R., Kuriakose, S., Vijaykumar, D.K. et al. Carcinosarcoma of the Uterus—A Single Institution Retrospective Analysis of the Management and Outcome and a Brief Review of Literature. Indian J Surg Oncol 4, 222–228 (2013). https://doi.org/10.1007/s13193-012-0206-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-012-0206-7