Abstract
The ESO-ESSO-ESTRO Multidisciplinary Course in Oncology is intended to fill the gap of the undergraduate fragmented oncology education, to provide insight into all theoretical and practical aspects of oncology, and to encourage future professional choices towards an oncology discipline. Students are exposed to (a) preclinical cancer topics; (b) natural history of the disease; (c) laboratory diagnostic tests; (d) medical, radiation, surgical, and palliative treatment; and (e) direct or through multidisciplinary patients’ approach. Students are obliged to attend (i) all theoretical lectures, (ii) clinical case presentations, (iii) laboratories and ward visits, and (iv) to prepare and present a specific project under supervision. Participation is limited to 24 medical students who are selected through a competitive application process. Between 2016 and 2019, 96 students from 29 countries have attended. Data analysis derived from a given questionnaire demonstrates that most of the participants have declared that (1) they have achieved their expectations and objectives, (2) they have highly rated both clinical and non-clinical teaching oncological topics, and (3) they have been stimulated in developing a professional career in the field of oncology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although worldwide mortality of cancer remains high, oncology education is generally not well represented in medical schools’ curricula. Undergraduate teaching about cancer is often fragmented, and students are less confident in their knowledge, especially in cancer therapeutic management. There is strong evidence that students are not receiving adequate clinical rotation in oncology and have disproportionately fewer oncology didactics [1,2,3,4,5,6,7,8]. In developing countries, it has also been shown that students are a long way from reaching the standards of knowledge and skills required in cancer medicine [9,10,11,12,13]. There is no doubt that there is a pressing universal need to reform faculties’ oncology programs to increase oncology awareness among medical students.
During the last 20–25 years and to fill this defect, several European Universities or scientific bodies/societies have attempted to organize extra-curriculum activities to offer additional undergraduate oncology education. Elective oncology courses or summer schools dedicated to medical students have been organized in various European cities. Groningen University in the Netherlands, Vienna University in Austria, and Ioannina University in Greece were the first medical faculties that organized such courses [4, 14,15,16,17]. Subsequently, several oncological scientific organizations such as the Federation of European Cancer Societies (FECS), in 2007 transformed into the European Cancer Organization (ECCO), and the European School of Oncology (ESO) and the individual oncology societies, such as the European Society for Medical Oncology (ESMO), the European Society of Surgical Oncology (ESSO), and the European Society for Radiotherapy and Oncology (ESTRO), have provided cancer education to medical students [16,17,18,19].
The main purposes of these endeavors were to make the students familiar with (a) basic cancer knowledge, (b) cancer clinical presentations, (c) diagnostic approaches, (d) therapeutic management, and (e) value of inter- and multidisciplinary teamwork. Most of these courses have proven highly successful as reflected by the positive evaluation feedback received by the students. Courses have been rated with high scores regarding the event organization, the program composition, and the faculty teaching.
In this paper, we present the final data derived from the four multidisciplinary elective courses in oncology for medical students organized by ESO-ESSO-ESTRO.
Material and Methods
Goal and Design of the Course
The ESO-ESSO-ESTRO multidisciplinary course in oncology for medical students is a 2-week course intended to provide insight into all aspects of oncology with both theoretical and practical sessions and is a continuation of a concept that was originally set-up by four universities ((i) Antwerp University, Edegem, Belgium; (ii) Umea University, Umea, Sweden; (iii) Poznan University, Poznan, Poland; and (iv) Berlin Charite University, Berlin, Germany) within the framework of a SOCRATES/ERASMUS program within the European Union (EU).
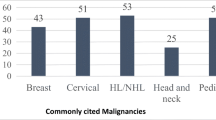
The course includes plenary sessions, case study presentations, daily special visits to various oncology departments, and group course projects that must be finalized and presented at the end of the course. Attention is given to the history of oncology, basic cancer research, epidemiology, prevention and screening, diagnostics, treatment principles, and therapeutic approaches in the frequently occurring tumor types. Besides, communication skills, alternative and complementary medicine, survivorship, and palliative care are brought into the discussion.
This 2-week event is offered to students who have completed their fourth year of studies, and participation is limited to 24 students selected through a competitive application process. The official language is English (students should be fluent in English). Here, it should be addressed that medical education in most European medical schools is officially provided in the local native language, except in those offering an English educational program, or in those that are exclusively English-spoken private universities. All students are required to stay until the end of the course.
Regarding the students selection criteria, all candidates should submit to ESO office: (i) an application form, (ii) a curriculum vitae, (iii) a letter of recommendation from an academic professor, (iv) a letter of intent written by the student explaining his/her reasons for wishing to attend the course as well as his/her expectations, and (v) the level of knowledge of English language.
Learning Outcomes
By the end of the course, participants should have (a) a comprehensive understanding of all aspects of oncology, (b) an understanding of the complexity and importance of the multidisciplinary approach to cancer treatment, and (c) be able to prepare a presentation in a combined effort with three other students and under the guidance of one of the teachers on a specific project to which they were appointed at the beginning of the course. This presentation is presented to the plenary audience and can be considered a training on how to prepare and present a scientific paper in a scientific meeting in the future.
Educational Methods
The course lasts ten working days and covers all aspects of oncology and includes the following: (a) theoretical plenary sessions of maximum 2 h, (b) multidisciplinary case presentations, (c) daily 2-h practical sessions in small groups (labs, ward visits, etc.), (d) preparation in small working groups of a presentation on a specific topic under the supervision of a teacher, and (e) project presentations delivered by the students on the last day. Faculty consists of distinguished academic members from European universities and/or European cancer centers.
Evaluation of Results
The evaluation of the course was performed (a) by answering a questionnaire consisting of 10 questions, which is related to the organization and the outcome of the event, and (b) by assessing the quality of teaching of each faculty member. The scoring system ranged from 0 to 10. The course chairs did take into account the evaluation from the preceding edition when organizing subsequent editions. It should be emphasized that the teaching evaluation data for the year 2016 are not available since it was not scheduled to provide students with the relevant form.
Social Activities
Three social activities were organized during the 2-week program: (i) a welcome reception organized by the host institute on the first day, (ii) a visit to the host city during the course, and (iii) a farewell reception at the end of the course.
Venues and Dates
The venues and the dates for the four courses were as follows: (i) Aug 24–Sept 4, 2016, in Poznan, (ii) Aug 28–Sept 8, 2017, in Antwerp, (iii) Aug 26–Sept 7, 2018, in Poznan; and (iv) Aug 26–Sept 6, 2019, in Turin.
Results
Demographics
In total, 399 applications were received from all over the world and 96 (24%) students were accepted, 24 for each course. Sixty-five percent were from Europe, 13% from Baltic and Eurasia countries, 12% from Middle East countries, 6% from Latin America, 3% from the USA, and 1% from China. The mean age was 23.5 years (range 21–30 years), 58% were women and 42% men. Most students (70%) belonged to the fourth year of medical studies (Table 1).
Results of the Questionnaire
Most questions for all four courses scored highly with mean values ranging from 7.8 to 9.0. Almost all students were satisfied in achieving their expectations and their objectives in both theoretical and practical knowledge. They also felt that the course helped them in choosing oncology for their future professional career. In addition, course organization and logistical arrangements were highly appreciated by the participants, as mirrored by the scoring. A small non-significant scoring decline was noticed in the 2018 event, especially on the structure of the course and on the allowed time for discussion and questions (6.1–6.6) (Table 2).
Teaching Evaluation
A short-term evaluation of alumni by completing a questionnaire was done at the end each event; however, no long-term follow-up was performed. The teaching evaluation data of 2017, 2018, and 2019 courses were divided into clinical and non-clinical topics. The clinical topics include the natural history, presentation, diagnosis, and treatment of the disease, while the non-clinical topics consist of a variety of lectures from epidemiology and research to principles of anti-cancer therapies.
In general, the overall mean values of both topics were highly rated (around 8.0 for clinical topics and from 7.0 to 9.0 for the non-clinical topics). However, some non-clinical topics, such as the history of oncology, epidemiology, carcinogenesis or genetics, did score somewhat lower in some years (5.7–6.0 in 2017 and 2018) (Table 3).
Discussion
Undergraduate medical education is a term of students going from high school to medical schools in Europe and other countries, but not in the USA. Oncology undergraduate cancer education in Europe, the USA, Canada, and Australia is often underrepresented and fragmented. Most medical schools do not follow a common syllabus, and both didactic hours and clinical exposure to cancer patients are still limited. Medical students are less confident in their knowledge and skills concerning cancer treatment and have no adequate clinical rotations in either out-patients or patients’ clinics. They are not often involved in cancer diagnostics, in doctor-patient communication, in breaking bad news and in multidisciplinary teamwork [1,2,3,4,5,6,7,8,9,10, 12, 17]. There is no doubt that worldwide undergraduate curricula in oncology require an upgrade and re-evaluation
The new curriculum should raise awareness and increase undergraduate exposure to cancer patients concerning prevention, early detection, breaking bad news, communication skills, cancer treatment methods, and supportive and palliative management [20,21,22]. Whether the massed curriculum (teaching concentrated in one semester) is superior to the space-out curriculum (teaching spread out over 3 years), it remains to be proven [23]. Lately, some improvement in undergraduate oncology education has been introduced by various academic centers. In Poland, a new curriculum with increased teaching hours, the presence of an oncology education coordinator, and an examination after completion of the oncology training has been established [24, 25]. In the UK, a more robust clinical exposure of medical students to cancer patients has been proposed, with a formal teaching clinic under the supervision of a post-fellow trainee [26]. Other European countries, the USA, Canada, and Australia are also strongly supporting the development of a new model of the curriculum in oncology.
During the last two decades and to fill the already existing cancer undergraduate educational vacuum, some academic oncology departments (Groningen, Vienna, and Ioannina medical schools), cancer societies (ESMO, ESSO, ESTRO), and other scientific oncological bodies (ESO, FECS/ECCO) have established extra-curriculum summer elective courses in oncology [14,15,16,17,18].
Available evaluation data from two of these courses have demonstrated (a) that from the six ESO courses held in Ioannina University, Greece, between 2004 and 2009, the average rating score for the overall evaluation of the faculty members and the teaching topics ranged between 3.50 and 3.60 (score 1-4) [16] and (b) that from the Vienna Summer School on Oncology first held in 1999, the mean scores of the program organization, the program composition, and the faculty educators were 4.47, 4.68, and 4.36, respectively (scores 1–5) [4]. Similar experiences were obtained in the earlier mentioned SOCRATES/ERASMUS program for mobility activities in the EU that was executed in the universities of Antwerp, Berlin (Charite), and Poznan.
An average score of 4.9 on a scoring range of 1 to 5 in that course was provided to the question “Would you recommend the course to your colleagues” (Vermorken; personal communication). From these data, it is evident that these educational events were highly assessed by most medical students.
Since 2015, the ESO-ESMO courses held in Ioannina University, Greece, were transferred and annually continued in the University of Valencia, Spain, and since 2018 due to increased demand, an additional annual medical student course was initiated in the University of Naples [27, 28].
Between 2016 and 2019, ESO, ESSO, and ESTRO have organized a renewed collaborative 2-week medical student oncology course, offering both theoretical teaching and clinical exposure. A quarter of the applicants were accepted to attend the events. Courses have taken place in three different European cities. All four courses have been solicited and recommended by previous participants (54%), by departments’ directors (18%), by ESO (54%), ESSO (7%), and ESTRO (7%) websites as well as by social media.
Evaluation data of the four ESO-ESSO-ESTRO courses revealed that all questions from the provided questionnaire and most of the topics (especially the clinical ones) were highly scored. Nevertheless, some of the non-clinical topics received slightly lower scoring (5.7–6.9). It is also very interesting to emphasize the high positive score given by the medical students to question number 6 (mean 8.6, range 8.0–9.5) asking whether the course was able to influence their decision to choose oncology as their future specialty (Table 2).
In conclusion, between 2016 and 2019, ESO-ESSO-ESTRO successfully provided 2-week theoretical and practical multidisciplinary oncology courses, in which 94 European and non-European students have participated. Close to 90% of the students attended found that the courses met their expectations and their planned objectives. All four courses were highly scored. Based on these findings as well as on the high number of students’ applications, the organizers have decided to continue organizing this course in an annual basis.
Data Availability
Yes
References
Arenas M, Sabater S, Biete A, Lara P, Calvo F (2018) Radiation oncology teaching programmes as part of the undergraduate degree in medicine in Spanish universities: the need for an update of the contents and structure. J Cancer Educ Off J Am Assoc Cancer Educ 33:352–358. https://doi.org/10.1007/s13187-016-1106-2
Ben Mustapha S, Meijnders P, Jansen N, Lakosi F, Coucke P (2019) The status of radiation oncology (RO) teaching to medical students in Europe. Clin Transl Radiat Oncol 17:40–46. https://doi.org/10.1016/j.ctro.2019.04.010
Gaffan J, Dacre J, Jones A (2006) Educating undergraduate medical students about oncology: a literature review. J Clin Oncol Off J Am Soc Clin Oncol 24:1932–1939. https://doi.org/10.1200/JCO.2005.02.6617
Lütgendorf-Caucig C, Kaiser PA, Machacek A, Waldstein C, Pötter R, Löffler-Stastka H (2017) Vienna Summer School on Oncology: how to teach clinical decision making in a multidisciplinary environment. BMC Med Educ 17:100. https://doi.org/10.1186/s12909-017-0922-3
McRae RJ (2016) Oncology education in medical schools: towards an approach that reflects Australia’s health care needs. J Cancer Educ Off J Am Assoc Cancer Educ 31:621–625. https://doi.org/10.1007/s13187-016-1088-0
Neeley BC, Golden DW, Brower JV, Braunstein SE, Hirsch AE, Mattes MD (2019) Student perspectives on oncology curricula at United States medical schools. J Cancer Educ Off J Am Assoc Cancer Educ 34:56–58. https://doi.org/10.1007/s13187-017-1265-9
Payne S, Burke D, Mansi J, Jones A, Norton A, Joffe J, Cunningham D, McVie G, Agarwal R (2013) Discordance between cancer prevalence and training: a need for an increase in oncology education. Clin Med 13:50–56. https://doi.org/10.7861/clinmedicine.13-1-50
Tam VC, Berry S, Hsu T, North S, Neville A, Chan K, Verma S (2014) Oncology education in Canadian undergraduate and postgraduate medical programs: a survey of educators and learners. Curr Oncol 21:e75–e88. https://doi.org/10.3747/co.21.1667
Amgad M, Shash E, Gaafar R (2012) Cancer education for medical students in developing countries: where do we stand and how to improve? Crit Rev Oncol Hematol 84:122–129. https://doi.org/10.1016/j.critrevonc.2012.01.003
Gaafar R, Shash E, El-Haddad A, Hady SA (2011) Teaching oncology to medical students is a must: the Egyptian NCI step on the road. J Cancer Educ Off J Am Assoc Cancer Educ 26:547–548. https://doi.org/10.1007/s13187-011-0214-2
Manirakiza A, Rubagumya F, Fehr AE, Triedman AS, Greenberg L, Mbabazi G, Ntacyabukura B, Nyagabona S, Maniragaba T, Longombe AN, Ndoli DA, Makori K, Kiugha M, Rulisa S, Hammad N (2020) Oncology training in Rwanda: challenges and opportunities for undergraduate medical students (The EDUCAN Project). J Cancer Educ Off J Am Assoc Cancer Educ 35:359–365. https://doi.org/10.1007/s13187-019-1473-6
Pavlidis N (1997) Undergraduate education in oncology in the Balkans and Middle East. The Metsovo Statement, April 4, 1997. Ann Oncol Off J Eur Soc Med Oncol 8:1281. https://doi.org/10.1023/a:1008299232223
Sharma DN, Rath GK, Parashar A, Singh P (2010) Survey of undergraduate medical students on their understanding and attitude towards the discipline of radiotherapy. J Cancer Res Ther 6:11–14. https://doi.org/10.4103/0973-1482.63556
De Vries J, Szabó BG, Sleijfer DT (2002) The educational yield of the international summer school “Oncology for Medical Students”. J Cancer Educ Off J Am Assoc Cancer Educ 17:115–120. https://doi.org/10.1080/08858190209528817
Haagedoorn EM, Oldhoff J, Bender W (1997) Report of an international summer school--oncology for medical students--in 1996 in Groningen, The Netherlands. J Cancer Educ Off J Am Assoc Cancer Educ 12:56–58. https://doi.org/10.1080/08858199709528452
Pavlidis N, Vermorken JB, Stahel R, Bernier J, Cervantes A, Pentheroudakis G, Audisio RA, Costa A (2012) Undergraduate training in oncology: an ESO continuing challenge for medical students. Surg Oncol 21:15–21. https://doi.org/10.1016/j.suronc.2010.07.003
Pavlidis N, Vermorken JB, Stahel R, Bernier J, Cervantes A, Audisio R, Pentheroudakis G, Costa A (2007) Oncology for medical students: a European School of Oncology contribution to undergraduate cancer education. Cancer Treat Rev 33:419–426. https://doi.org/10.1016/j.ctrv.2007.02.005
Eriksen JG, Leech M, Benstead K, Verfaillie C (2016) Perspectives on medical education in radiation oncology and the role of the ESTRO School. Clin Transl Radiat Oncol 1:15–18. https://doi.org/10.1016/j.ctro.2016.10.001
ESMO ESMO-ESO courses on medical oncology for medical students. https://www.esmo.org/meetings/esmo-eso-courses-on-medical-oncology-for-medical-students. Accessed 6 Apr 2020
DeNunzio NJ, Joseph L, Handal R et al (2013) Devising the optimal preclinical oncology curriculum for undergraduate medical students in the United States. J Cancer Educ Off J Am Assoc Cancer Educ 28:228–236. https://doi.org/10.1007/s13187-012-0442-0
Ha FJ, Parakh S (2018) Novel approaches to undergraduate oncology education. J Cancer Educ Off J Am Assoc Cancer Educ 33:500–504. https://doi.org/10.1007/s13187-016-1109-z
Sherwood M, Rioux D, Knight R, LeBlanc M, Betsch T, Giuliani M, Caissie A (2019) Increasing undergraduate exposure to oncology: the role of oncology interest groups. J Cancer Educ Off J Am Assoc Cancer Educ. 35:997–1001. https://doi.org/10.1007/s13187-019-01554-x
Cecilio-Fernandes D, Aalders WS, de Vries J, Tio RA (2018) The impact of massed and spaced-out curriculum in oncology knowledge acquisition. J Cancer Educ Off J Am Assoc Cancer Educ 33:922–925. https://doi.org/10.1007/s13187-017-1190-y
Matkowski R, Szelachowska J, Szewczyk K, Staszek-Szewczyk U, Kornafel J (2014) Improvements in undergraduate oncology education introduced at Polish medical universities between 2004 and 2010 under Poland’s “National Program for Combating Neoplastic Diseases”. J Cancer Educ 29:428–433. https://doi.org/10.1007/s13187-014-0633-y
Wawryka J, Ziobro P, Tyszko M (2017) Cancer education in Poland: current status and suggestions for improvement. J Cancer Educ Off J Am Assoc Cancer Educ 32:669–675. https://doi.org/10.1007/s13187-016-1033-2
Fackrell D (2017) Medical student-led outpatient clinics: Improving undergraduate oncology education. Clin Oncol R Coll Radiol G B 29:e140. https://doi.org/10.1016/j.clon.2017.02.001
Medical Student Course 2020 | Naples. https://www.esmo.org/meetings/medical-students-course-2020-naples. Accessed 6 Apr 2020
Medical Student Course 2020 | Valencia. https://www.esmo.org/meetings/medical-student-course-2020-valencia. Accessed 6 Apr 2020
Acknowledgments
We would like to thank all event organizers Mrs. Christine Verfaillie, Arta Leci, Alessandra Nappa (ESTRO), Carine Lecoq, Ana Galan (ESSO) and Dolores Knupfer (ESO) for their valuable support.
Author information
Authors and Affiliations
Consortia
Contributions
All authors participated in data collection, analysis and interpretation, drafting, and final approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Not applicable
Consent to Participate
All participants that answered the survey were considered to have consented to participate.
Consent for Publication
Not applicable
Research Involving Human Participants
This is an observational study. The European School of Oncology has confirmed that no ethical approval is required.
Informed Consent
All participants that answered the survey were considered to have consented to participate in the study.
Code Availability
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pavlidis, N., Madry, R., Peeters, M. et al. ESO-ESSO-ESTRO Multidisciplinary Course in Oncology for Medical Students: 4 Years of Experience (2016–2019). J Canc Educ 37, 1239–1244 (2022). https://doi.org/10.1007/s13187-020-01947-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-020-01947-3