Abstract
This study aimed to determine final year students’ core oncology and radiation oncology knowledge and attitudes about the quality of teaching in medical programmes delivered in Australia and New Zealand. Does the modern medical programme provide core oncology skills in this leading global cause of mortality and morbidity? An online survey was distributed between April and June 2018 and completed by 316 final year students across all 21 medical schools with final year cohorts in Australia and New Zealand. The survey examined teaching and clinical exposure, attitudes and core knowledge for oncology and radiation oncology. Several questions from a survey done of graduates in 2001 were repeated for comparison. We found that clinical exposure to oncology and its disciplines is low. Students rated oncology and haematology the worst taught medical specialties at medical school. Students reported the most confidence identifying when surgical management of cancer may be indicated and much lower levels of confidence identifying when systemic therapy and radiation therapy may be helpful. The majority of students had no formal course content on radiation therapy and more than one third of final year students erroneously believed that external beam radiation therapy turned patients radioactive. Exposure to oncology practice and the teaching of core oncology knowledge remains low for medical students in Australia and New Zealand. Many areas of oncology teaching and knowledge have worsened for medical students in Australia and New Zealand over the past 20 years. Well-established gaps in the core oncology knowledge of medical graduates must be urgently addressed given the increasing incidence of cancer and ongoing underutilisation of radiation therapy in particular.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer is a leading cause of mortality globally. In 2018, there was an estimated 18.1 million new cases of cancer worldwide and 9.6 million cancer deaths [1]. The lifetime risk of developing cancer varies from 33 to 50% across countries [1]. The increasing incidence of cancer and its ubiquity mean that doctors across all specialities including general practice require a sound understanding of the cancer continuum including prevention, screening, diagnosis, treatment modalities and survivorship. However, opportunities for oncology education remain limited outside of specialist oncologist training pathways, meaning that high-quality fundamental oncology learning needs to take place during medical school.
Medical schools have implemented significant changes across the structure and content of medical education in recent decades. Problem-based learning models, integrated content delivery and student-directed learning frameworks have grown alongside rapid advances in medical knowledge with an emphasis on other skill sets, such as research methods, communication, leadership, professionalism, ethics, social justice and public health [2, 3]. Around the world, medical curricula are crowded and subjects and learning opportunities face increasing competition for space and time. In Australia, many medical schools have replaced Bachelor of Medicine degrees with Doctor of Medicine programmes which includes larger research components, without changes to the duration of these programmes. This type of model may put further stress on attaining core clinical learning.
This is of particular concern for oncology education as studies have consistently detected gaps and deficits in students’ understanding of cancer and core oncology knowledge around the world [4,5,6,7,8,9,10,11]. Oncology knowledge and skills in Australian and New Zealand medical graduates were surveyed in 1990 and 2001 [8, 12] and showed some improvement in exposure to branches of oncology, declining competence in melanoma detection and Papanicolaou smears, and general dissatisfaction with teaching around managing patients with curable and incurable cancers [8]. The degree to which oncology knowledge and competence have changed over 18 years since the last survey of Australian and New Zealand medical students remains unknown.
Regarding various cancer treatment modalities, radiation oncology learning appears to be particularly neglected within medical schools [13]. A lack of exposure at medical school to a key treatment modality such as radiation therapy may have far-reaching consequences. For example, there is a well-established discrepancy between the number of patients who receive radiation therapy and the number of patients across many cancer sites that are estimated to benefit from it based on strongly evidence-based modelling for modern radiation therapy use [14, 15]. It is proposed that the lack of general and radiation oncology awareness amongst doctors, including general practitioners, contributes to the underuse of this effective therapy [16].
This study sets out to survey final year medical students in Australia and New Zealand to obtain a snapshot of oncology learning, radiation oncology and clinical exposure, and to compare these parameters based on similar questions asked of new graduates in 2001 [8].
Methods
Survey Development and Design
This survey was conducted as part of a larger project looking at radiation oncology teaching and learning across Australia and New Zealand and overseen by a core working group comprising radiation oncologists, registrars, junior doctors, medical students and staff at the Royal Australian and New Zealand College of Radiologists (RANZCR). Our survey followed on from studies investigating oncology (radiation oncology in particular) education as described by medical faculty and educators [Reference] and junior pre-vocational doctors (in prep). These studies also employed a survey methodology. The survey consisted of 29 items assessing student perceptions of oncology and radiation oncology curricula, and practical readiness to assess and manage oncology patients (Supplementary material). Domains included student demographics and degree structure, exposure to radiation oncology during medical school, confidence and understanding of oncology, and personal views about the oncology and radiation oncology curriculum. Questions were a mix of closed and open questions, multiple choice, free form, ranking and 5-point Likert scales.
Questions about radiation oncology were developed by the core working group and/or adapted from our survey of medical faculties and junior doctors. Oncology awareness and general cancer knowledge were adapted with permission from the 2001 survey used by Barton et al. [8]. A draft survey was pilot tested with six final year medical students to ensure usability and comprehension and edits were made to the survey following feedback (see Supplementary material).
Survey Distribution and Participants
The survey (SurveyMonkey Inc., San Mateo, USA) was distributed to Australian and New Zealand medical students in their final year of study through a combination of social media (Facebook and Twitter) and email from April to June 2018. Initially, the medical student society at each medical school and three national societies were asked to promote the survey to their final year cohorts. Fifteen student associations cooperated in distributing the survey either via private Facebook pages or email. Follow-up promotion via the societies was undertaken at two time points over the data collection period. Part way through data collection curriculum leads at medical schools underrepresented in the participant pool were requested to promote the survey on learning platforms or via email. Participant responses were anonymous and voluntary, and no identifying data were collected. Data were collected from 27 April–24 June 2018.
Data Analysis
The SurveyMonkey data were exported into Excel where descriptive statistics were calculated. To compare responses to our survey with those from the 1990 and 2001 surveys, we compared unadjusted differences in proportions.
Results
Participant Characteristics
At the time of conducting our survey, there were 23 medical schools in Australia and New Zealand. Two schools did not yet have final year students, having recently opened. Across the remaining 21 medical schools, 18 medical student associations agreed to distribute a link to the electronic survey either via Facebook, newsletter or email.
In total, 316 respondents from 21 medical schools completed all or part of the survey. As recruitment was not targeted, we are unable to calculate a response rate; however, in 2018, there were an estimated 4339 final year students (Australia, 3803; New Zealand, 536) [17] yielding a response rate estimate of 7.3%. Fifty-nine percent of participants (n = 185) were female and 41% were male. Thirty-four percent were completing a MBBS (n = 109), 45% a MD (n = 142) and 21% a MBChB or BMed. There was good representation of undergraduate (53%, n = 166) and postgraduate (47%, n = 149) students and students enrolled in 4-year (44%, n = 138), 5-year (20%, n = 63) and 6-year (36%, n = 114) courses.
Exposure to Oncology Topics
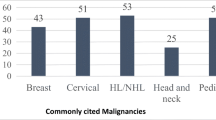
Approximately one in three respondents had no clinical exposure to medical oncology (35% of students) or palliative care (32%) (Table 1). Nearly three quarters of final year medical students had no clinical exposure to surgical oncology (74% of students). The cancer types of patients most commonly encountered across medical training were colorectal (11% of students with no exposure) and breast cancer (15% of students with no exposure); half of respondents had no contact with lymphoma (48%) or head and neck cancer (53%) patients (Table 1). Overall, 82% of students (207/254) indicated a desire for additional oncology teaching, particularly about cancer treatment options, mechanisms of therapy (89%) and oncological skills (60%).
Forty-seven percent of students (134/284) indicated that radiation oncology was not incorporated into their curriculum at all, and a further 16% (45/284) were unsure. Thirty percent of students reported no dedicated lecture or tutorial on the subject and a further 42% received only 1 to 2 h of content over the duration of their course (Table 1). Most students had contact with a patient requiring or receiving radiation therapy, but 76% of students had no experience with seeing radiation therapy delivery (Table 1). Eighty percent of students (205/255) indicated a desire for more formal radiation oncology teaching at medical school. The most desired topics were clinical indications for radiation therapy (90% of students), radiation oncology emergencies (87% of students), recognition and management of side effects (84% of students) and a better understanding of the mechanism of radiation therapy (68% of students).
Confidence and Training in Oncology
The majority of students self-reported average to high competence regarding smoking cessation counselling, performing a cervical swab, recognising a melanoma and breaking bad news (Table 2). Students felt less competent discussing death with a dying patient and 37% of students reported poor skills in this area (Table 2). Sixty-two percent of students reported no to low confidence recognising when radiation therapy is indicated, compared to 31% of students for systemic therapy and 17% for surgery. Overall, 45% of students indicated confidence in assessing patients with potential malignancy (Table 2).
When asked to rate the quality of their oncology training at medical school, final year students rated education around smoking cessation, cancer prevention and cancer screening more highly than teaching around the management of patients with curable cancer, incurable cancer and end-of-life management (Table 2). More than a third of respondents rated their training in cancer management (32% of students) and the management of dying patients (36% of students) as poor or very poor (Table 3).
Overall, the adequacy of training in cancer and haematology was the poorest amongst ten specialties surveyed (Table 4). Cardiovascular disease was deemed the most adequately taught across medical degrees.
Knowledge and Confidence in Radiation Oncology
The majority of students (79%) correctly identified that radiation therapy could have a curative role in the treatment of prostate cancer, but less than half of respondents identified its role in the treatment of tonsillar (48%), anal (44%) and cervical cancer (24%) (Table 5). Nearly all students (96%) correctly identified no role for radiation therapy in febrile neutropenia (96%), but 27% mistakenly stated a primary curative role for radiation therapy in early breast cancer, and 52% indicated a routine role for radiation therapy in malignant bowel obstruction. Over a third of students (37%) erroneously thought that patients are radioactive after external beam therapy (Table 5).
Students reported no or low confidence in being able to explain to patients how radiation therapy kills cancer, the process of radiation therapy planning and the differences between radiation therapy techniques (Table 6). Confidence was higher for identifying situations where radiation therapy may be urgently required, such as for spinal cord compression, bronchial obstruction and haemorrhage (Table 6).
Discussion
This is the first study in decades to assess oncology and radiation oncology education and knowledge in final year medical students across Australia and New Zealand. Since previous surveys the incidence of cancer has increased with the ageing population, the number of medical students has more than tripled, our understanding of the biology and treatment of cancer has grown exponentially, and medical programs have become more complex with no change to the duration of degrees. Our survey of students from 21 medical schools suggests that the state of oncology awareness amongst final year medical students remains of major concern and that this is consistent with international studies in comparable education and health systems.
Exposure to oncology is a mixed picture across our sample of final year students. Approximately, one in three students had no clinical learning experiences with medical oncology, three quarters had no experience with surgical oncology and three quarters had no experience with the provision of radiation therapy. Student contact with cancer patients does occur, but not in an oncological setting or placement. The more common cancers encountered by students are consistent with their prevalence. While students appear to be graduating with self-confidence in smoking cessation, melanoma detection and breaking bad news, discussing death with dying patients remains a source of low confidence for soon-to-be graduates. Within cancer treatment modalities, students are most confident in knowing when surgery is an appropriate therapy. Less than half of students feel confident assessing (history and examination) potential malignancies in patients.
For context, we asked students to rate the adequacy of their teaching across different diseases and specialties. Oncology and haematology were the lowest ranked subjects in terms of preparedness for practicing as a junior doctor. In Canada, oncology was similarly ranked by medical students and educators [6]. The majority of students desire additional oncology teaching before graduating, particularly around cancer treatments.
Alarmingly, exposure across all of oncology appears to have declined since the last surveys in 2001 and 1990 [8]. Over time, there has been a rise in the number of students with no exposure to medical oncology (46% in 2018, 20% in 2001 and 18% in 1990), radiation oncology (73% in 2018, 22% in 2001 and 42% in 1990), surgical oncology (75% in 2018, 3% in 2001 and 11% in 1990) and palliative care (32% in 2018, 18% in 2001 and 50% in 1990). Confidence in smoking cessation counselling (66% of students reported high or very high competence in 2018 vs 30–40% in 2001) and performing a cervical swab (57% high or very high competence in 2018 vs 14–18% in 2001) has improved since 2001; confidence recognising a melanoma (23% high or very high competence in 2018 vs 16–23% in 2001), breaking bad news (28% high or very high competence in 2018 vs 20–33% in 2001) and discussing death with a dying patient has declined (28% high or very high competence in 2018 vs 13–31% in 2001) [8]. Students in 2018 rated their training in cancer prevention (45% of students reported very good or good training in 2018 vs 34–37% in 2001) and screening more favourably than students in 2001 (53% of students reported very good or good training in 2018 vs 39–48% in 2001) [8]. The perception of the quality of training in managing patients with curable cancer declined (25% of students reported very good or good training in 2018 vs 29% in 2001). The perception of training in managing incurable cancer (20% of students reported very good or good training in 2018 vs 17–24% in 2001) and dying patients (27% of students reported very good or good training in 2018 vs 19–26% in 2001) remains poor and unchanged compared to ratings by students in 2001 [8].
A more detailed examination of awareness and knowledge of radiation oncology revealed some confusion around the role of radiation therapy in particular cancers and oncological presentations, perhaps unsurprising given its relative absence from most medical curricula [13] and the fact that half of respondents in our survey were unaware of it in their curricula. Knowledge of radiation therapy is limited to specific cancers such as prostate and symptoms such as malignant bone pain. Outside of these applications, a significant proportion of students are unaware of other applications or the role of radiation therapy in an estimated 50% of cancer patients [15, 18]. Indeed, some fundamental aspects of this common treatment modality are misunderstood by medical students. Students express a strong desire for more education about radiation therapy, as there is a lack of formal teaching, and poor self-reported confidence in understanding different radiation treatments. It is therefore unsurprising that a not insignificant proportion believe external beam therapy leads to a patient becoming radioactive. Underuse of radiation therapy in cancer patients remains an ongoing problem [14, 15] and is a situation not helped by medical graduates with little clinical exposure and teaching in radiation oncology [13]. There is a clear need to develop more learning experiences in outpatient clinics and services where the majority of medical and radiation oncology is performed.
The identification of limited oncology teaching and learning in medical education programmes is common across educational and health system contexts. Of concern is a persistent pattern of low clinical oncology exposure, oncology teaching and poor self-confidence for cancer content and skills amongst final year medical students, which in some areas appears worse compared to studies conducted in the same region decades ago. The detailed look at radiation oncology performed here is the first to sample the awareness of this important treatment modality amongst final year medical students in Australia and New Zealand. A lack of exposure, understanding and confidence in radiation oncology mirrors the broader pattern affecting general oncology teaching and learning.
Oncology education continues to suffer from neglect and fragmentation [4, 19], and despite historical acknowledgement of the need for a standardised set of learning objectives, this remains elusive [19, 20]. Debate as to whether oncology should be integrated into curricula or taught as blocks also persists [20, 21]. Further, education in oncology may be suffering because of pressures on the modern and crowded medical curriculum. International evaluations of oncology teaching and learning consistently raise concerns around students’ understanding of cancer and core oncology knowledge. A study of UK medical graduates found that only 61% had undergone a clinical module or attachment in oncology and less than half of graduates (41%) felt prepared to care for patients with cancer [9]. Oncology was rated the most poorly taught medical specialty by Canadian final year students [6], and in the USA, deficits in cancer prevention knowledge and cancer history-taking have been identified in medical students [4].
This evident, and perhaps worsening, problem facing oncology teaching means that evidence-based curriculum reform is overdue but is not being addressed by medical faculties, at least for radiation oncology [13]. Alternative models for teaching oncology include e-learning modules [22], brief clinical modules [23], research programmes hosted by cancer centres [24] and summer schools [18]. While lectures remain the dominant form of teaching at medical school, other modes are being trialled. Even the adoption and promotion of an oncology textbook would help focus learning by medical students, and studies in other education contexts indicate a strong desire for a resource aligned to learning objectives [6].
Limitations
The proliferation of medical student online surveys and feedback collection (course content, placements, end of semester etc.) mean that many final year students report survey and feedback fatigue (personal communication). While we did collect from responses from all 21 medical schools with final year cohorts but the number of medical graduates per year has more than tripled since the last survey of this nature and a larger sample would allow for more robust conclusions. Responder bias amongst self-selected participants may have either over-estimated the knowledge and confidence of students. Alternatively, we may have underestimated oncology content and practice because we surveyed students several months before fully completing their training.
Conclusion
The inflation of medical degrees may have come at a cost in terms of core knowledge and clinical exposure. Exposure to oncology at medical school as at 2018 remains low and appears to have fallen in the past decades. Oncology and haematology were rated the poorest taught medical disciplines over the course of medical degrees and the teaching of cancer management, breaking bad news and end-of-life care remain low and unchanged over the last two decades. Given the rapidly increasing incidence of cancer, treatment combinations and number of cancer survivors requiring cross-disciplinary care, improvements in core oncology teaching at medical school are urgently required. Our work confirms that exposure to, and knowledge of, radiation oncology in particular are lower than for other areas of oncology and specific efforts and attention are needed to address identified gaps within core oncology teaching.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Dotters-Katz SK (2018) Medical education: how are we doing? Med Educ 52(1):5–7
Cusano R, Busche K, Coderre S, Woloschuk W, Chadbolt K, McLaughlin K (2017) Weighing the cost of educational inflation in undergraduate medical education. Adv Health Sci Educ Theory Pract 22(3):789–796
DeNunzio NJ, Joseph L, Handal R, Agarwal A, Ahuja D, Hirsch AE (2013) Devising the optimal preclinical oncology curriculum for undergraduate medical students in the United States. J Cancer Educ 28(2):228–236
Matkowski R, Szelachowska J, Szewczyk K, Staszek-Szewczyk U, Kornafel J (2014) Improvements in undergraduate oncology education introduced at Polish medical universities between 2004 and 2010 under Poland’s “National program for combating neoplastic diseases”. J Cancer Educ 29(3):428–433
Tam VC, Berry S, Hsu T, North S, Neville A, Chan K, Verma S (2014) Oncology education in Canadian undergraduate and postgraduate medical programs: a survey of educators and learners. Curr Oncol 21(1):e75–e88
Zumberg M, Broudy V, Bengston E, Gitlin S (2015) Preclinical medical student hematology/oncology education environment. J Cancer Educ 30:711–718
Barton M, Tattersall M, Butow P, Crossing S, Jamrozik K, Jalaludin B, Atkinson CH, Miles SE (2003) Cancer knowledge and skills of interns in Australia and New Zealand in 2001: comparison with 1990, and between course types. Med J Aust 178:285–289
Cave J, Woolf K, Dacre J, Potts H, Jones A (2007) Medical student teaching in the UK: how well are newly qualified doctors prepared for their role caring for patients with cancer in hospital? Br J Cancer 97:472–478
Kujan O, Abuderman A, Azzegahiby S, Alenzi FQ, Idrees M (2013) Assessing oral cancer knowledge among Saudi medical undergraduates. J Cancer Educ 28(4):717–721
Deng L, Na FF, Wang JW, Meng MB, He HY, Yang JJ, Jian YS, Wu JJ, Ding J, Xie D, Liu Y, Mu XM, Li YF, Chen Y, Lu Y (2011) Insufficient screening knowledge in Chinese interns: a survey in ten leading medical schools. Asian Pac J Cancer Prev 12(10):2801–2806
Barton M, Bell P, Koczwara B (2006) What should doctors know about cancer? Undergraduate medical education from a societal perspective. Lancet 7:596–603
Nicholls L, Bravery B, Chelvarajah R, Shi K, Tieu MT, Turner S, Windsor A (2018) The status of radiation oncology teaching in Australian and New Zealand medical schools. J Med Imaging Radiat Oncol. https://doi.org/10.1111/1754-9485.12788
Morgan G (2011) Why has radiotherapy utilisation not improved since 1999? J Med Imaging Radiat Oncol 117(2):386–389
Delaney GP, Barton MB (2015) Evidence-based estimates of the demand for radiotherapy. Clin Oncol (R Coll Radiol) 27(2):70–76
Morris L, Gorayski P, Turner S (2018) Targeting general practitioners: prospective outcomes of a national education program in radiation oncology. J Med Imaging Radiat Oncol 62(2):270–275
Medical Deans Australia and New Zealand. (2017). Workforce data report 2017. Retrieved from http://www.medicaldeans.org.au/wp-content/uploads/2017_Snapshot_Data_Report.pdf
Baskar R, Lee KA, Yeo R, Yeoh KW (2012) Cancer and radiation therapy: current advances and future directions. Int J Med Sci 9(3):193–199
Pavlidis N, Vermorken JB, Stahel R, Bernier J, Cervantes A, Audisio R, Pentheroudakis G, Costa A (2007) Oncology for medical students. Cancer Treat Rev 33(5):419–426
Hughes-Davies L, Barrett J (2011) Training the oncologists of the future. Clin Oncol 23(9):565–568
Agarwal A, Koottappillil B, Shah B, Ahuja D, Hirsch AE (2015) Medical student-reported outcomes of a radiation oncologist-led preclinical course in oncology: a five-year analysis. Int J Radiat Oncol Biol Phys 92(4):735–739
da Costa Vieira RA LA, Sarri AJ, Benedetti ZC, de Oliveira CZ (2016). Oncology e-learning for undergraduate. A prospective randomized controlled trial. J Cancer Educ 32(2):344–351. https://doi.org/10.1007/s13187-015-0979-9
Auret K, Starmer D (2008) Using structured clinical instruction modules (SCIM) in teaching palliative care to undergraduate medical students. J Cancer Educ 23:149–155
Fernando E, Jusko-Friedman A, Catton P, Nyhof-Young J (2015) Celebrating 10 years of undergraduate medical education: a student-centered evaluation of the Princess Margaret Cancer Centre—determinants of Community Health year 2 program. J Cancer Educ 30(2):225–230
Acknowledgements
We thank the medical student societies and medical faculties that helped distribute this survey. RANZCR provided access to SurveyMonkey.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study was approved by Human Research Ethics Committee, Central Coast Local Health District. Data were collected from 27 April–24 June 2018.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 491 kb).
Rights and permissions
About this article
Cite this article
Bravery, B.D., Shi, K., Nicholls, L. et al. Oncology and Radiation Oncology Awareness in Final Year Medical Students in Australia and New Zealand. J Canc Educ 35, 1227–1236 (2020). https://doi.org/10.1007/s13187-019-01586-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-01586-3