Abstract
A critical shortage of trained cancer specialists is one of the major challenges in addressing the increasing cancer burden in low- and middle-income countries. Inadequate undergraduate cancer education in oncology remains a major obstacle for both task shifting to general practitioners and for training of specialists. We provide the first report of cancer education in Rwanda’s undergraduate program to survey how new graduates are prepared to provide care for cancer patients. Anonymous online survey was sent January to June 2017 to medical students in their senior clinical years (years 5 and 6). Questions related to the demographics, medical curriculum, and general oncology exposure were included in the survey. Of 192 eligible students, 42% (n = 80) completed the survey and were analyzed. The majority were 25 to 29 years of age and 41% were female. Internal medicine was cited to provide the most exposure to cancer patients (50%) and cancer bedside teaching (55%). Close to a half (46%) have been taught oncology formally in addition to bedside teaching. A tenth (11%) of the participants felt comfortable in attending a cancer patient, and a fifth (21%) of the students felt comfortable while addressing multimodality treatment approach. The majority (99%) of the participants preferred having a formal oncology rotation. Of particular interest, 61% of the students are interested in pursuing an oncology career path. There is a need to modify the current oncology undergraduate curriculum to prepare future physicians for delivering cancer care in Rwanda. Raising the profile of oncology in undergraduate medical education will complement the on-going efforts to increase the country’s capacity in task shifting and in training of cancer specialists.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The burden of cancer is rapidly rising in low- and middle-income countries (LMICs), where over 70% of cancer deaths occur [1,2,3,4]. For low-income countries in particular, the many challenges of cancer care are often further compounded by severe shortages in health care practitioners at all levels, medical education that is not attuned to changing health threats, and insufficient health care infrastructure [2,3,4].
Throughout Africa, there is tremendous variability in basic oncology training for undergraduate medical students. Oncology is frequently taught under other medical disciplines, with minimal emphasis on current therapeutic modalities and direct clinical exposure to cancer patients [5,6,7]. As a result, these students are inadequately trained in cancer prevention, screening, and treatment. Many go on to become primary care providers after completion of their undergraduate studies, and their lack of oncologic training may eventually translate into sub-optimal management of cancer patients [5,6,7,8,9,10].
There is an emerging consensus that there is a critical shortage of trained oncology health practitioners in low-income countries. An oncology curriculum should ideally prepare trainees to make informed clinical decisions for when they ultimately take on the role of therapeutic decision-makers [11,12,13,14]. In addition, early exposure to oncology would facilitate acquisition of required knowledge and competencies to address cancer prevention, screening, early detection, and treatment.
Globally, there are several medical training initiatives focused on overcoming these educational deficits [14,15,16,17]. Efforts have included national educational programs, oncology-specific electives/clerkship programs, and organized curricular and extra-curricular activities [18,19,20]. These interventions have yielded encouraging results: they have provided additional motivation for trainees to further specialize in oncologic disciplines, and have led to an improvement in patient management [21, 22].
Rwanda’s population is a little over 12 million and has only two [2] practicing oncologists in different subspecialties (clinical and pediatric oncologists). As of 2018, the country does not have an oncology postgraduate program and depends on programs across Africa for training of their practitioners. National cancer figures are based on GLOBOCAN estimates, and existing, published numbers reflect the patients seeking care at the Butaro Cancer Center of Excellence [23].
The EDUCAN project was designed to understand the landscape of oncology training from both undergraduate (phase I) and postgraduate (phase II) students, and later expand to the faculty, in order to build an oncology curriculum suitable to the Rwandan cancer care needs.
The primary aim of this study was to identify the current status of cancer education in one of Rwanda’s two medical schools and to provide a basis for educational reforms that target improvements of cancer knowledge and management.
Methods
Study and Survey Design
We conducted an anonymous, cross-sectional survey of students at the University of Rwanda, School of Medicine. Participants were eligible if they were in year five or six (currently named levels VA and VB) of a 6-year program by the time of this study. School administration provided the current email addresses of all eligible participants; potential participants were sent an email detailing the study and providing a link to the online survey in January 2017. A letter of information and consent was provided before each participant can start the survey.
The 26 mixed format questions survey was designed in two general parts, the first is part gathering information related to the participants’ demographics. The second part included questions based on the occurrence of exposure of the medical students to commonly seen malignancies in Rwanda. The questionnaire involved 6-point Likert-scale questions to assess the level of knowledge and comfort in performing specified tasks. The survey was conducted in English, the language of medical instruction. It followed the format of knowledge, attitudes, and practices (KAP) survey and included questions on participants’ demographic information, current medical school curriculum, and exposure to oncology during training, and opinions regarding medical education and the inclusion of oncology and knowledge were self-reported. Additionally, the survey contained 86-point Likert-scale questions assessing participants’ personal level of comfort and knowledge regarding care of cancer patients. Exposure to different cancers was surveyed based on reported volumes estimates and gathered for ease of analysis.
Data Collection and Analysis
Each completed and submitted survey was automatically received through a secured Google DriveⓇ platform, and a Microsoft Excel database was generated at the end of the survey period (July 2017). Data was cleaned and analyzed using STATA version 13. Descriptive statistics were used to calculate the response rate of each survey question. Likert-scale responses were aggregated from the original six points to three. For level of comfort and level of knowledge, respectively, scores of 0–1 were reclassified as “not at all” or “none,” scores of 2–3 were reclassified as “somewhat” or “some,” and scores of 4–5 were reclassified as “very” or “adequate.”
Ethics Approval
Ethics approval was sought and obtained from the Kigali University Teaching Hospital Review Board. All participants provided electronically written informed consent prior to participation.
Results
One hundred ninety-two eligible students were emailed and 80 students responded and completed the survey, for a response rate of 42% which is line with response rates in other similar surveys. Of these 80 students, 47 (59%) were male, 50 (63%) were between 25 and 29 years of age, and 41 (51%) were in year VA (fifth year) (Table 1).
The majority of students were exposed to cancer patients an estimated 0–10 times [34 (43%) < 5 times; 35 (44%) 5–10 times] during their clinical training rotations, of approximately 32 weeks each over 4 years (third to sixth year). Internal medicine was cited by 40 (50%) to be the rotation with the most exposure to cancer, followed by pediatrics by 20 (25%) participants. Internal medicine was also the rotation with the most bedside cancer-related teaching for 44 (55%) participants (Table 2).
Forty-three (54%) participants stated there was an oncology-specific course during their medical training, and 15 (19%) reported there was a formal oncology curriculum at the School of Medicine. Regarding the manner in which oncology topics were taught, 37 (46%) participants stated they were taught during rotations as part of bedside teaching, and 19 (24%) stated they were taught during rotations as part of morning presentations; 8 (10%) participants were self-taught on oncology through reading. Further, 31 (39%) indicated there were recommended resources available for oncology-related topics (Table 2).
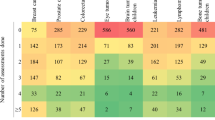
All students had seen at least one type of cancer during their medical education, and 21 (26%) had seen five types: breast, cervical, Hodgkin’s lymphoma/non-Hodgkin’s lymphoma (HL/NHL), head and neck, and pediatric. Among the cancers, HL/NHL was seen the most, followed by cervical and pediatric cancers (Fig. 1).
Likert-scale Questions
Participants were asked a series of Likert-scale questions regarding their comfort/confidence in or knowledge of key components of cancer care. In regard to their level of comfort or confidence, 9 (11%) participants felt comfortable in attending to a cancer patient; 4 (5%) felt confident in staging a cancer patient; 17 (21%) felt confident counseling a cancer patient and their family; and 30 (38%) felt confident managing cancer-related pain (Table 3). Concerning their level of knowledge, 5 (6%), 6 (8%), 13 (16%), and 17 (21%) participants felt they had adequate knowledge on the role of chemotherapy, radiotherapy, surgery, and multimodality, respectively, in managing cancer (Table 3).
Participant Opinions on Medical Training
Only 3 (4%) participants believed the amount of time allocated to oncology-related topics during their medical education was adequate. When asked if they believed a formal rotation in oncology would be useful, 78 (99%) responded “yes,” 65 (81%) respondents believed a standard curriculum for oncology would be suitable for medical students, and 70 (88%) believed an extra-curricular educative platform for oncology would be useful. Lastly, 49 (61%) student participants stated they would be interested in pursuing a career in oncology; 23 (29%) said it would depend on their interests at the time (Table 2).
Discussion
With the prevalence of cancer increasing globally, there is a growing concern around the shortage in physicians formally trained in oncology in LMICs. This is an issue that needs to be addressed: it is imperative that basic cancer knowledge be included as part of a structured undergraduate medical curriculum.
Rwandan medical schools, as is the case with many schools in African countries, lack a standardized oncology curriculum, and little is published on the current status of oncology education in undergraduate medical schools [6]. Our findings are based on a survey of medical students enrolled in their final 2 years of undergraduate education at one of the two medical schools in Rwanda. The students are distributed in four different teaching hospitals across the country, without a structured oncology-training curriculum, hence with differing levels of exposure to cancer patients. The results of this survey provide information on oncology education, exposure to cancer patients during undergraduate medical training, students’ levels of comfort in attending cancer patients, and self-reported levels of knowledge in domains of palliative care, chemotherapy, and radiation therapy.
The government of Rwanda together with multilateral partners embarked in the summer of 2012 on a 7-year collaboration to boost in numbers its output of qualified health care providers at different levels and specialties through the Human Resources for Health (HRH) program. The program saw a strong number of US-trained specialists teaching and mentoring both medical students and residents in their academic courses, extending to a twinning model of skill transferring between a US-trained faculty and a Rwandan faculty [24, 25]. Whether the presence of an increased number of specialists influenced medical students in their overall oncology knowledge is unknown and was not captured in the survey. Of note, the scope of the survey did not address the role of visiting HIC-based internal medicine residents in teaching Rwandan medical students so we did not add this to the paper for reasons related to space and lack of information. The role of such collaborations could be investigated further in the future.
At the time of the survey, radiotherapy facilities were in the procurement process and are currently running as of the final term of 2018; hence, the medical students who participated in this survey did not have exposure to radiation therapy principles.
The role of primary care physicians is of particular importance in LMICs given the shortage of trained oncologists. They are at the forefront of prevention, screening, diagnosis, and treatment management. In Rwanda, some of these physicians are trained to deliver specialized cancer care in a task-shifting model [26]. However, results of this survey clearly highlighted that there is a low level of confidence in managing and counseling cancer patients among senior medical students, majority of whom go on to become primary care physicians after 1 year of internship upon graduation from medical school. In order to provide patients with the highest standard of care, this confidence level needs to be strengthened through an established oncology curriculum with first-hand experience.
Similar projects across the globe have demonstrated the importance of a curriculum that puts an emphasis on teaching provided by oncology specialists during students’ different clinical rotations [11, 18, 19], thus allowing the students to be better taught and have more confidence in management of cancer patients. Our findings confirm the importance of bedside teaching in clinical rotations for undergraduate students. However, this continues to be a challenge in Rwanda, and in many LMICs, due to the paucity of oncologists and oncology practitioners that can serve as teachers and mentors [11].
The participants in this study expressed a preference of workplace instruction over traditional classroom-based oncology teaching. A European initiative allows medical students to participate in non-traditional instructional strategies in oncology. They report adequate oncology exposure and educational improvement overtime. This 3-year initiative focuses on commonly occurring and terminal malignant conditions in areas of comprehensive cancer care (surgery, radiation, medical oncology, and palliative care) and oncologic emergencies. More medical students reported aspiring to a career in oncology at the end of this educational initiative [15]. The channels for achieving this increased workplace exposure in LMICs could include team-based education, early patient and population exposure, different work-site training bases, and longitudinal relationships with patients and communities [27].
According to the World Health Organization, transformative scale-up of physician training consists of a process of both education and health systems reforms that address the quantity, quality, and relevance of health care providers, in order to contribute to universal access and improve population health outcomes [28]. To address the issue of quality, the ideal medical school curriculum should include both didactic teaching and workplace learning in oncology, so that students are exposed to all components of cancer management, prevention, and screening. The challenge of relevance, however, is that in many LMICs, the medical education may not match to the needed skills and epidemiology of the disease in their communities [26]. In order to address relevance, the curriculum must be context specific. Oncology education in LMICs should ideally focus on the relevant clinical challenges faced in these regions and the available essential medical therapies and technology [29].
Another challenge in Rwanda and other LMICs is the lack of available oncology specialists able to participate in medical education. Our survey indicates that most exposure to oncology occurs during other rotations, such as internal medicine. Medical students acquire a significant amount of knowledge from interactions with residents. A study conducted in a limited-resource setting established the role of mentors for surgery-focused medical students. The study showed an almost equal role of the residents and consultants for a bedside teaching to medical students [30]. This shift in residents-as-educators will persist for some time, and as such, it is important to investigate and enhance oncology knowledge in the postgraduate setting to optimize current oncology teaching. This could provide an additional resource that can help alleviate the impact of the shortage in oncology teaching faculty. We are currently conducting a similar investigation on oncology knowledge and exposure in the postgraduate setting. The objective is to identify challenges and opportunities to improve postgraduate learners’ competence in oncology and their ability to effectively engage in oncology teaching to undergraduate students.
Lastly, it is encouraging that more than half the medical students surveyed expressed an interest in a career in oncology despite the gaps in oncology curriculum in undergraduate education. This could be due to the fact there is an increasing awareness in LMICs of the magnitude of cancer as a vital public health issue. This interest in oncology as a career constitutes a highly conducive environment for innovative curricular interventions to improve oncology training in the undergraduate setting. There are several promising innovative interventions to improve medical students’ competencies and skills in cancer. These include increasing workplace exposure to oncology care, as well as improving oncology competencies and teaching skills in the postgraduate setting in order to harness the resources of residents-as-teachers to undergraduates.
With the increasing use of technology for effective knowledge sharing purposes in developing countries [31, 32], other possible interventions include incorporation of online modules and distance learning, inter-professional and team-based learning, sharing of curricula, collaboration among medical schools across the East African region, and adapting curricula from high-income countries to suit local disease burden and management resources. Fostering the engagement of undergraduate medical students in cancer research is also expected to increase knowledge, skills, and interest in this emerging public health threat. Further, raising the profile of oncology in undergraduate medical education will complement the on-going efforts to increase Rwanda’s capacity in cancer specialists training and task shifting with the ultimate goal of improving population health outcomes.
High-income countries (HIC) are also facing threats of shortages in the oncology work force. To this effect, the American Society of Clinical Oncology has developed several initiatives such as the formation of the ASCO Trainee Council comprised of medical students and residents. The council’s mission is to identify and support the unique early career development needs of medical students, residents, and fellows and to be their voice throughout ASCO [17]. The African Organization for Research and Training in Cancer (AORTIC) is currently establishing similar initiatives to support trainees across the spectrum at a continental level in order to make oncology an attractive and viable career choice for young physicians and other health professionals.
The study had a number of limitations including mainly being limited to medical students in the public National University and the non-direct control of participants’ response patterns and verification through the online survey design. Other limitations include the purely quantitative nature of the study and the non-inclusion of a potential HRH influence on medical students’ oncologic training in the survey. The study design grouped pediatric cancers together for ease of analysis, which did not allow assessment of potential individual childhood malignancy learning.
Conclusion
In Rwanda, there are significant opportunities to improve undergraduate medical education in oncology. The hope is that improved educational opportunities will ultimately translate into improvements in cancer care and clinical outcomes. Impeding challenges include the shortage of cancer specialists in clinical rotations and the inadequate infrastructure relating to both cancer care and resources needed for curricular redesign. In this paper, we have proposed several strategies to address challenges and broker opportunities to improve undergraduate medical education in Rwanda and other African countries. Future studies should include both quantitative and qualitative methods to investigate the implementation and the impact of these innovative interventions in teaching oncology in the undergraduate setting.
References
Torre LA, Bray F, Siegel RL et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Pervaiz R, Faisal F (2017) Cancer incidence and mortality are associated with human development index and health setups in Africa. J Egypt Natl Cancer Inst 29(3):123–126
Curado MP et al (2015) Cancer burden in Latin America and the Caribbean. Ann Glob Health 80(5):370–377
Knaul F, Horton S, Yerramilli P, Gelband H, Atun R (2015) Financing cancer care in low-resource settings. In: Gelband H, Jha P, Sankaranarayanan R et al (eds) Cancer: disease control priorities, third edition (volume 3). The International Bank for Reconstruction and Development / The World Bank, Washington (DC) Chapter 17
Seyoum N, Biluts H, Bekele A et al (2014) Medical Students’ choice of specialty and factors determining their choice: a cross-sectional survey at the Addis Ababa University, School of Medicine, Ethiopia. Ethiop Med J 52(3):129–135
Soliman AS, Nasser SS et al (2003) Cancer education in medical, nursing, and pharmacy schools in Egypt: features applicable to other countries. J Cancer Educ 18(1):12–14
Cecilio-Fernandes D, Aalders WS, Bremers AJ, Tio RA, de Vries J (2017) The impact of curriculum design in the acquisition of knowledge of oncology: comparison among four medical schools. J Cancer Educ 33(5):1110–1114. https://doi.org/10.1007/s13187-017-1219-2
Hsairi M, Gobrane HB, Alaya NB et al (2007) Knowledge and attitudes of medical students at the end of their curriculum, towards breast and cervical cancer screening. Santepublique (Vandoeuvre-les-Nancy, France) 19(2):119–132
Morhason-Bello IO, Odedina F, Rebbeck TR et al (2013) Challenges and opportunities in cancer control in Africa: a perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol 14(4):e142–e151
Amgad M, Shash E, Gaafar R (2012) Cancer education for medical students in developing countries: where do we stand and how to improve? Crit Rev Oncol Hematol 84(1):122–129
Gaafar R, Shash E, El-Haddad A, Hady SA (2011) Teaching oncology to medical students is a must: the Egyptian NCI step on the road. J Cancer Educ 26(3):547–548
Kapoor N, Haagedoorn EML, de Vries J (2006) The UICC/WHO-CCCE cancer education project: an Indian experience. J Cancer Educ 21(3):182–185
Shulman LN, Mpunga T, Tapela N, Wagner CM, Fadelu T, Binagwaho A (2014) Bringing cancer care to the poor: experiences from Rwanda. Nat Rev Cancer 14(12):815–821
Hamadeh GN, Adib SM (2001) Changes in attitudes regarding cancer disclosure among medical students at the American University of Beirut. J Med Ethics 27(5):354–354
Karamouzis MV, Ifanti AA et al (2006) Medical students’ views of undergraduate oncology education: a comparative study. Educ Health (Abingdon, England) 19(1):61–70
De Vries J, Szabo BG, ThSleijfer D (2002) The educational yield of the international summer school “Oncology for Medical Students”. J Cancer Educ 17(3):115–120
Gaffan J, Dacre J, Jones A (2006) Educating undergraduate medical students about oncology: a literature review. J Clin Oncol 24(12):1932–1939
Pavlidis N, Vermorken JB, Stahel R et al (2012) Undergraduate training in oncology: an ESO continuing challenge for medical students. Surg Oncol 21(1):15–21
Bayomy H, El Awadi M, El Araby E, Abed HA (2016) Computer-based medical education in Benha University, Egypt: knowledge, attitude, limitations, and suggestions. J Egypt Public Health Assoc 91(4):179–184
Aboshady OA, Radwan AE, Eltaweel AR, Azzam A, Aboelnaga AA, Hashem HA, Darwish SY, Salah R, Kotb ON, Afifi AM, Noaman AM (2015) Perception and use of massive open online courses among medical students in a developing country: multicentre cross-sectional study. BMJ Open 5(1):e006804
Matkowski R, Szelachowska J, Szewczyk K et al (2014) Improvements in undergraduate oncology education introduced at Polish Medical Universities between 2004 and 2010 under Poland’s “National Program for Combating Neoplastic Diseases”. J Cancer Educ 29(3):428–433
Agarwal A, Shah A, Byler S, Hirsch AE (2017) Cultivating interest in oncology through a medical student oncology society. J Cancer Educ 32(1):31–34
Lara P, Calvo FA, Guedea F et al (2013) Undergraduate cancer education in Spain: the debate, the opportunities and the initiatives of the University Forum of the Spanish Society of Radiation Oncology (SEOR). Rep Pract Oncol Radiother 18(6):405–413
Agarwal A, De Nunzio NJ, Ahuja D et al (2014) Beyond the standard curriculum: a review of available opportunities for medical students to prepare for a career in radiation oncology. Int J Radiat Oncol Biol Phys 88(1):39–44
Liu J-E, Mok E, Wong T (2005) Perceptions of supportive communication in Chinese patients with cancer: experiences and expectations. J Adv Nurs 52(3):262–270
Binagwaho A, Kyamanywa P, Farmer PE, Nuthulaganti T, Umubyeyi B, Nyemazi JP, Mugeni SD, Asiimwe A, Ndagijimana U, Lamphere McPherson H, Ngirabega JDD (2013) The human resources for health program in Rwanda—a new partnership. N Engl J Med 369(21):2054–2059
Ndenga E, Uwizeye G, Thomson DR, Uwitonze E, Mubiligi J, Hedt-Gauthier BL, Wilkes M, Binagwaho A (2016) Assessing the twinning model in the Rwandan Human Resources for Health Program: goal setting, satisfaction and perceived skill transfer. Glob Health 12(1):4
Rubagumya F, Greenberg L, Manirakiza A et al (2017) Increasing global access to cancer care: models of care with non-oncologists as primary providers. Lancet Oncol 18(8):1000–1002
Bhutta ZA, Chen L, Cohen J, Crisp N, Evans T, Fineberg H, Frenk J, Garcia P, Horton R, Ke Y, Kelley P, Kistnasamy B, Meleis A, Naylor D, Pablos-Mendez A, Reddy S, Scrimshaw S, Sepulveda J, Serwadda D, Zurayk H (2010) Education of health professionals for the 21st century: a global independent commission. Lancet 375(9721):1137–1138
World Health Organization, 2011. Transformative scale up of health professional education: an effort to increase the numbers of health professionals and to strengthen their impact on population health. http://apps.who.int/iris/bitstream/10665/70573/1/WHO_HSS_HRH_HEP2011.01_eng.pdf ) accessed September 9th, 2017)
African Organization for Research and Education in Cancer (AORTIC): education and training committee strategic plan. http://www.aorticafrica.org/images/uploads/AORTIC_Education_and_Training_StrategicPlan.pdf. Accessed 15 Oct 2018
Manirakiza A, Hrdy M, Ginwalla R et al (2016) Mentorship role in the choice of surgery as a career among medical students in Rwanda. Rwanda Med J 73(3):17–20
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval was sought and obtained from the Kigali University Teaching Hospital Review Board. All participants provided electronically written informed consent prior to participation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manirakiza, A., Rubagumya, F., Fehr, A.E. et al. Oncology Training in Rwanda: Challenges and Opportunities for Undergraduate Medical Students (The EDUCAN Project). J Canc Educ 35, 359–365 (2020). https://doi.org/10.1007/s13187-019-1473-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-1473-6